Abstract
Background
We probe the adolescent gender difference in depression, asking two critical questions. First, most longitudinal studies of gender differences in adolescent depression date from the 1980s and 1990s, raising the need for a body of evidence on whether the developmental pattern is similar or different today.
Second, despite the importance of chronicity to depression, we do not know whether there is a gender difference in the chronicity burden of the disorder.
Methods
In a contemporary longitudinal sample of U.S. adolescents, depression symptoms were assessed at ages 11, 13, 15, and 18, and depression diagnoses were assessed at age 20. To capture the chronicity burden of clinical depression, we assessed for every depressive episode in an individual’s lifetime and summed the total number of days spent in episode.
Results
A gender difference emerged at age 13 for depression symptoms and at age 13–14 for diagnoses. These findings are similar to those in the 1980s and 1990s despite many social changes that have occurred. However, the magnitude of the gender difference in symptoms at ages 13 and 15 may be larger than those documented previously. Latent growth curve modeling of depression symptoms indicated that girls’ symptoms accelerated early in adolescence whereas boys’ symptoms accelerated later. Although more girls (24%) than boys (15%) experienced major depression or dysthymia by age 20, the chronicity burden among those with depression showed gender similarities (median = 2.6% days depressed for boys and 2.4% for girls).
Limitations
Depression diagnoses were assessed retrospectively; however, symptom data were assessed prospectively, and symptom and diagnostic data converged. The sample was also predominantly White, limiting generalizability.
Conclusions
In a contemporary adolescent sample we observed gender differences in depression symptoms and diagnoses beginning at age 13. We documented distinct developmental trajectories of depression for adolescent girls and boys, suggesting different developmental windows for depression prevention programs. We also discovered a gender similarity in the chronicity burden of clinical depression.
Keywords: Gender, depression, longitudinal, adolescence, chronicity
The gender difference in depression (with twice as many females experiencing depression as males) was first underscored by Myrna Weissman in the 1970s among adults (Weissman & Klerman, 1977). Subsequent research revealed that the gender difference emerges during adolescence (as reviewed by Nolen-Hoeksema & Girgus, 1994). Several large longitudinal studies have documented the emergence and pattern of gender differences in depression diagnoses and symptoms from childhood through adolescence (e.g., Essau et al., 2010; Garber et al., 2002; Ge et al., 2001; Hankin et al., 1998; Marmorstein, 2009; Angold et al., 1998); however, none of these studies comprise contemporary samples. The individuals in these samples experienced adolescence in the 1980s and 1990s. Much about gender relations and society has changed since then. For example, the emergence of media such as Facebook and texting has created a different social environment for today’s adolescents, as well as new ways to engage in peer harassment (Jose et al., 2011). Media viewed by adolescents has become increasingly sexualized, and conveys a sexual script for girls that they can attain status by sexually objectifying themselves (American Psychological Association, 2010; Graff et al., 2013). Many have also suggested that lifestyle changes (e.g., greater sugar consumption, pro-inflammatory diets, increased self-focus) have increased rates of depression (e.g., Haroon et al., 2012; Hidaka, 2012; Lopresti et al., 2013). Forces such as these might well change patterns of depression for adolescent girls and boys. Indeed, a recent review concluded that internalizing problems for girls increased from the late 20th century to the 21st century; however, findings for boys were mixed (Bor et al., 2014). Given the current context of forces promoting depression, it is especially interesting and of great public health significance to continue monitoring trends in gender differences in depression among youth.
Longitudinal studies of adolescents in the 1980s and 1990s documented that the gender difference in depression symptoms and diagnoses emerges between ages 12 and 15 (Angold et al., 1998; Ge et al., 2001; Hankin et al., 1998; Marmorstein, 2009). Girls experience greater increases than boys in both depression symptoms and diagnoses throughout adolescence (Garber et al., 2002; Ge et al., 2001; Hankin et al., 1998). One study found that girls experience increases in depression symptoms in early adolescence while boys experience increases in depression symptoms in later adolescence (Ge et al., 2001). Other research suggests that the trajectory of adolescent depression symptoms may be curvilinear or even cubic, and does not differ by gender (Marmorstein, 2009; Rawana & Morgan, 2014).
Cross-sectional studies of adolescents in the 2000s have confirmed that the adolescent gender difference in depression still exists. Among 13 to 18 year-olds in the National Comorbidity Survey-Adolescent Supplement, the lifetime prevalence of major depressive disorder or dysthymia was 15.9% for females and 7.7% for males (Merikangas et al., 2010). Girls also reported higher levels of depression symptoms in a recent population-based study of middle school and high school adolescents in the U.S. (Lampard et al., 2014). Although cross-sectional studies are informative, they do not provide a clear picture of the developmental course of the gender difference in depression. Among a sample of adolescents in the 2000s, at what age do gender differences in depression emerge? Does the gender difference in depression persist across adolescence or is it greater during certain developmental periods? Do girls and boys have similar trajectories of depression across adolescence? Hankin et al. (1998) clearly delineated the developmental pathways of gender differences in depression among New Zealand adolescents who experienced adolescence in the 1980s and early 1990s. A comparable study among contemporary adolescents in the 2000s is needed.
Although researchers documented the gender difference in adolescent depression in the 1980s and 1990s, they did not assess gender differences in the burden of the disorder. Chronicity is a crucial component of the depression burden (i.e., individual suffering, cost to society). Researchers in the 1970s shifted the conceptualization of depression as an acute disorder to a recurrent and chronic disorder (Zis & Goodwin, 1979). The longer lasting the depression, the greater the burden (i.e., the more days an individual spends depressed, the more suffering the individual experiences and the greater burden endured by society). However, the extant approaches to quantifying depression do not fully capture its chronicity. Thus, we do not know if males or females are more burdened by depression chronicity.
Specifically, approaches to quantifying the gender difference in depression have included examining gender differences in symptoms, diagnoses, maximum duration of an episode, and recurrence. Although informative, these metrics do not fully capture the chronicity burden of depression. For example, recurrence does not accurately reflect chronicity in the case of individuals with relatively short recurrent episodes (who might experience fewer days depressed than individuals with a single chronic major depressive episode or dysthymia). With respect to clinically diagnosed depression, it is the combination of number of episodes and the length of each episode (i.e., the total number of days spent in depressive episodes) that fully captures the chronicity associated with clinical depression. Despite extensive research on gender differences in depression, we do not know if, among depressed individuals, females spend more days of their lives suffering from depression compared to males.
The purpose of the current study was to answer two critical questions about gender differences in depression throughout adolescence using data from a longitudinal sample of U.S. adolescents, the Wisconsin Study of Families and Work (Hyde et al., 1995). First, what is the developmental pattern of the emergence of the gender difference in depression in adolescence in a contemporary sample in the 2000s? In particular, we examined at what age the gender difference emerges, the magnitude of the gender difference, and whether the developmental trajectory of depression differs by gender. We used two methods of assessment (depression symptoms and depression diagnoses) to provide converging information about the pattern of the development of gender differences in depression across adolescence. Second, among adolescents with clinical depression, is there a gender difference in the chronicity burden by age 20 (i.e., do girls or boys spend more days clinically depressed)?
Methods
Participants
Participants were adolescents who have participated in a longitudinal study of child development since birth, the Wisconsin Study of Families and Work (WSFW; Hyde et al., 1995). From 1990 to 1991, a total of 570 pregnant women were recruited from the Madison and Milwaukee, Wisconsin areas for participation in the study. At one month postpartum, 548 mothers and their infants were participating in the study. The present study focuses on the adolescent assessments taken at ages 11, 13, 15, and 18 for depression symptoms and the young adult assessment at age 20 for depression diagnoses.
Of the original 548 child participants, 416 (76%) completed at least one of the adolescent assessments. These 416 participants (51% female) comprise the sample used for the analyses with depression symptoms. Of the 416 participants, 89% were White, 8% biracial, 2% African American, and 1% American Indian. Data were collected during the summers following Grade 5 (N = 311; mean age = 11.5, SD = .32; summers of 2002 and 2003), Grade 7 (N = 376; M = 13.5, SD = .33), Grade 9 (N = 337; M = 15.5, SD = .33), and Grade 12 (N = 325; M = 18.5, SD = .33; summers of 2009 and 2010). The 416 adolescent participants did not differ from the 132 participants no longer participating in adolescence on the following variables assessed in infancy: family income2, maternal and paternal depression symptoms. The 416 adolescent participants had significantly higher maternal education3 at the start of the study (p <.05, d = 0.34) and marginally higher paternal education (p = .08, d = 0.20) than the 132 participants no longer participating in adolescence.
For the analyses with depression diagnoses, participants were 267 WSFW participants (58% female) who completed a diagnostic interview at the age 20 assessment (M = 20.5, SD = .31; summers 2011 and 2012). Of these 267 participants, 92% had attended college or technical school after high school and 84% indicated that they would be attending college in the upcoming fall. Of these participants, 90% were White, 8% biracial or multiracial, and 2% African American. Out of the 416 participants with adolescent data, there were no significant differences between the 267 participants with diagnostic data and the 149 participants without diagnostic data on measures of depression symptoms at ages 11 through 18 (all p values > 0.14).
Procedure
Participants completed questionnaires administered on a laptop computer during in-home visits during the age 11, 13, and 15 assessments. At age 18 participants completed the questionnaires online (using Qualtrics software) or paper questionnaires if requested. Diagnostic interviews were conducted by phone at the age 20 assessment. The University of Wisconsin Institutional Review Board approved the study. Parents provided consent and children provided assent for their participation until age 18, when participants provided consent. At each wave of data collection participants received monetary compensation (e.g., participants received $50 for the diagnostic interview at age 20).
Measures
Depression symptoms
Depression symptoms were assessed at ages 11, 13, 15, and 18 with the short version of the Children’s Depression Inventory (CDI; Kovacs, 1985). The short form of the CDI is a 10-item self-report scale designed for use with 8 to 17-year-olds (Kovacs, 1985). The CDI measures the presence of affective, behavioral, and cognitive symptoms of depression, with higher scores indicating more depression. For each item, participants identified one of three statements (rated 0–2) that best described themselves in the previous 2 weeks (e.g., “I was sad”). Scale scores represent total scores, with a theoretical range from 0 to 20. Internal consistencies were 0.69 at age 11, 0.77 at age 13, 0.78 at age 15, and 0.77 at age 18.
Depression diagnoses
Trained doctoral students in clinical psychology conducted diagnostic interviews using the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID; First et al., 2002) when participants were 20 years old. The interview provides Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association, 2000) diagnoses of a wide range of psychiatric disorders. However, the bereavement exclusion criterion for depression diagnoses was not applied, making these diagnoses consistent with DSM-5. Dr. Lyn Abramson provided training in administration of the SCID for the two diagnostic interviewers. Interviews covered lifetime history of psychopathology, and assessed symptoms and duration for every possible episode of depression in an individual’s life, including Major Depressive Disorder (MDD), Dysthymia, and Depressive Disorder- Not Otherwise Specified (DNOS). We included the DNOS category given that adolescents with subthreshold depression (high levels of depression that do not meet criteria for major depression or dysthymia) still experience significant impairment (e.g., Lewinsohn et al., 2000) and are at elevated risk for later development of major depression and suicidal behaviors (Fergusson et al., 2005; Klein et al., 2009).
Interviewers used calendars to aid accurate reporting from participants
Onset dates for depression diagnoses were operationalized as a participant meeting full diagnostic criteria. Likewise, offset dates were operationalized as a participant no longer meeting full criteria. Dr. Abramson provided continued supervision based on audio-recordings of interviews. To ensure the reliability of the diagnostic interviewers, all interviewers participated in a weekly group meeting with Dr. Abramson where all diagnoses were reviewed and confirmed. An inter-rater reliability study on a randomly chosen subset of 30 audio-recorded interviews yielded kappas >0.90 for all depression diagnoses.
Chronicity burden
The LDI (Lifetime Depression Index; Rose et al., 1994) measures the chronicity burden of clinically significant depression. Rose and colleagues (1994) introduced the LDI in a study of depressed inpatients. However, to our knowledge, it has not been used since. The LDI is calculated by summing the total number of days spent in depressive episodes in an individual’s life and dividing that number by the total number of days lived (using participants’ birthdates and assessment dates). For an individual who is 20.5 years old (the average age of participants at the diagnostic interview), an LDI of 5% represents roughly a total of one year clinically depressed across the lifetime. Separate LDI scores were calculated for major depression and/or dysthymia, DNOS, and all depression diagnoses combined. Inter-rater reliability for LDI (percentage of days spent depressed) for all depression diagnoses on the subset of 30 interviews yielded a correlation coefficient of r = 0.99.
Data-Analytic Plan for Symptom Measures
We calculated descriptive statistics as means ± SD for depression symptoms. We tested for gender differences in depression at each age using independent samples t-tests. To protect the type I error rate, we should first test the between-subjects effect of gender in a repeated measures MANOVA; however, formulas for pooling F-tests of analysis of variance for multiply imputed data sets (which would be necessary with our longitudinal data) are still in development (van Ginkel & Kroonenbeg, 2014). Nonetheless, we ran a repeated measures MANOVA with multiple imputation in SPSS to determine if the pattern of results across the five imputed data sets supported the analysis of independent samples t-tests at each age.
Latent growth curve models were used to answer additional questions about the developmental pattern of the emergence of the gender difference in depression. Specifically, we tested whether the developmental trajectory of depression differs by gender. All proposed models were estimated with Mplus software (Version 5.21, Muthén & Muthén, 2007) using full information maximum likelihood (FIML) for missing data. Model fit was measured with the chi square goodness-of-fit test, the comparative fit index (CFI), and RMSEA. The chi square value tests the hypothesis that there is no difference between the modeled data and the observed data, and is said to indicate a good fit when the chi square is not significant. However, when sample sizes are large the chi square test frequently rejects correctly specified models (Hoyle, 1995). Therefore, we used the CFI and RMSEA in conjunction with the chi square test to examine practical fit. Acceptable fit is typically reflected by a CFI > 0.90 (Marsh et al., 2005). RMSEAs less than 0.05, 0.08, and 0.10 reflect a close, reasonable, and mediocre fit, respectively (Browne & Cudeck, 1993).
Measurement models
In order to determine that the depression symptom measure (CDI) was comparable for boys and girls at ages 11, 13, 15, and 18, we computed models to test for measurement invariance. Measurement invariance is established when sequential constraints for factor loadings and intercepts across gender do not produce significant change in model fit. We began with a model with no equality constraints on factor loadings or intercepts across gender at any time point (Model 1), then constrained factor loadings to equality across gender (Model 2), and finally constrained both factor loadings and intercepts across gender (Model 3). We compared nested models with a chi square difference test to determine whether gender constraints affected model fit, i.e. whether measures of depression were comparable across gender. Chi square difference tests are very strict and are sensitive to sample size; thus Little (1997) recommends comparing change in the practical fit indices, with a change of less than 0.05 indicating model similarity. Models used maximum likelihood estimation with robust standard errors (MLR estimation) because CDI items were not normally distributed.
Latent growth curve models
Latent growth curve models were used to describe the developmental trajectory of depression symptoms across adolescence, and to determine whether this trajectory differs by gender. Latent growth modeling uses repeated measures of a single variable to estimate two latent factors: the initial level (i.e., the intercept) and a measure of change over time (i.e., the slope). Factor loadings were set to pre-specified values such that the intercept represented depression at age 11 and the slope represented annual change in depression from age 11 to age 18. We specified a linear slope by fixing the slope factor loadings to 0, 2, 4, and 7 at ages 11, 13, 15, and 18, respectively. Thus, the interpretation of the linear slope corresponded to change in depression across one year. A quadratic slope was also added to the model with factor loadings of 0, 4, 16, and 49, to capture nonlinear trends. Maximum likelihood estimation was used for all latent growth curve models.
To determine whether latent growth trajectories differed by gender, we conducted a multi-group latent growth analysis (Bollen & Curran, 2006). We began by constraining the means and variances of the intercepts and slopes to equality across gender for both the linear and quadratic latent growth models. Then we released this constraint, allowing the means and variances of the slopes and intercepts to be freely estimated for boys and girls. A chi square difference test was used to determine whether developmental trajectories in depression differed by gender.
Data-Analytic Plan for Gender Differences in Depression Diagnoses and the Lifetime Depression Index
To examine the developmental pattern of gender differences in depression diagnoses, we computed depression prevalence for each 2-year period from age 11 to age 20: 11–12, 13–14, 15–16, 17–18, and 19–20. We then calculated odds ratios (OR) and conducted Fisher’s exact tests for gender differences (given that some analyses had cell counts less than 5). We hypothesized that more girls than boys would experience an episode of clinical depression throughout adolescence. These hypotheses support the use of one-tailed Fisher’s tests.
We calculated descriptive statistics for the LDI as means ± SD. Given the positive skew with the LDI we also present median data. We tested gender differences using independent samples t-tests.
Results
Gender Differences in Depression Symptoms
Descriptive statistics
Descriptive statistics for depression symptoms are presented in Table 1. Multiple imputation in SPSS and FIML in Mplus produced similar results for all descriptive statistics. Across all five multiply imputed data sets, the between-subjects effect of gender in the repeated measures MANOVA was significant, supporting analysis by independent samples t-tests at each age.
Table 1.
Descriptive statistics for depression symptoms.
| Females | Males | Gender Difference | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Symptoms | M | SD | M | SD | t | p-value | d | 95% CI for d |
| Age 11, CDI | 1.11 | 1.85 | 0.97 | 1.52 | 0.742 | 0.458 | 0.08 | [−0.14, 0.31] |
| Age 13, CDI | 1.64 | 2.29 | 0.93 | 1.62 | 3.468 | 0.001 | 0.36 | [0.15, 0.56] |
| Age 15, CDI | 2.03 | 2.57 | 1.04 | 1.76 | 4.177 | 0.000 | 0.45 | [0.23, 0.66] |
| Age 18, CDI | 1.93 | 2.26 | 1.62 | 2.41 | 1.232 | 0.219 | 0.14 | [−0.08, 0.36] |
Data presented for all participants at each time point (n = 311, 376, 337, and 325 at ages 11, 13, 15, and 18, respectively). P-values are associated with independent samples t-tests for gender differences at each age. d = (Mf−Mm) /sw. Mf = mean for females, Mm = mean for males, and sw = pooled within gender standard deviation. Positive d values indicate that females reported more depression symptoms than males. At ages 13 and 15 the data violated the equal variance assumption (females had significantly more variance), resulting in use of Welch’s t-test and the associated p-value. All of the models examining gender differences in depression symptoms violated the General Linear Model (GLM) assumption of normality; however, the coefficients are still the best, unbiased, efficient estimators among linear solutions (Cohen et al., 2003).
There was no gender difference in depression symptoms at age 11 (d = .08); a gender difference emerged by age 13 (d = 0.36) persisted through age 15 (d = 0.45) but then narrowed and became nonsignificant at age 18 (d = 0.14).
Measurement models
With increasing equality constraints across gender, the chi square difference test was significant; however, the change in practical fit indices was well below the 0.05 standard set by Little (1997). Therefore, we concluded that scalar invariance was met and measures of depression do not differ across gender at any time point. That is, factor scores can be meaningfully compared across gender. Data are available upon request.
Latent growth curve models
Table 2 displays the results of all latent growth analyses. For the linear model with means and variances constrained to be equal across gender, the average initial level at age 11 corresponded to an average rating of “one” (on a 0–20 scale) for depression symptoms and increased by about 0.11 each year until age 18. The quadratic model with means and variances constrained to be equal across gender had a significantly better fit than the constrained linear model (Δχ2(6) = 43.16), indicating that the data displayed a quadratic trend across time. The data showed a slight curve in the trajectory for boys and girls combined, with depression symptoms increasing in early adolescence and then decreasing in middle to late adolescence.
Table 2.
Fit statistics for latent growth curve models.
| χ2 | d.f. | RMSEA | CFI | Intercept Mean (Var) | Linear Slope Mean (Var) | Quadratic Slope Mean (Var) | |
|---|---|---|---|---|---|---|---|
| Means and Variance Constrained Across Gender | |||||||
| Linear | 73.43* | 14 | .14 | .70 | 1.03* (1.38*) | 0.11* (.03) | |
| Quadratic | 30.27* | 8 | .12 | .89 | 0.96* (1.38*) | 0.08 (.32) | 0.01 (.01) |
| Means and Variances Estimated Freely Across Gender | |||||||
| Linear | 46.17* | 10 | .13 | .82 | F = 1.21* (2.32*) | F = 0.13* (0.05) | |
| M = 0.83* (0.59*) | M = 0.08* (0.01) | ||||||
| Quadratic | 0.54 | 2 | .00 | 1.00 | F = 1.07* (1.18) | F = 0.36* (0.42) | F = −0.03* (0.01*) |
| M = 0.96* (1.76*) | M = −0.07 (0.30) | M = 0.02* (0.00) | |||||
Note.
denotes significantly different from zero (p < .05). F = females, M = males.
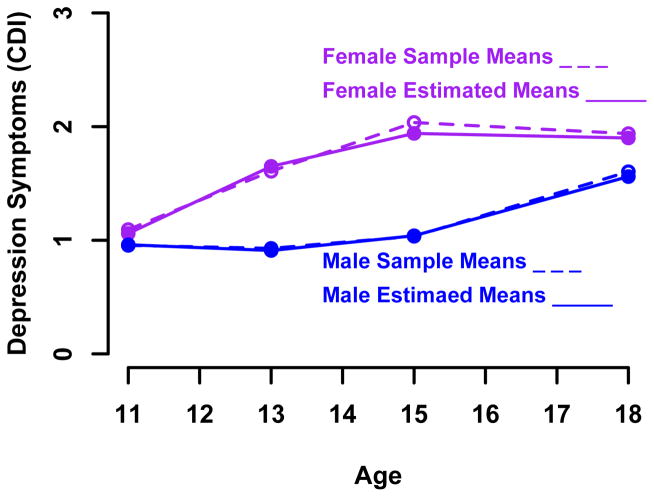
When the equality constraints were relaxed and the models were estimated freely across gender, both the linear model (Δχ2(4) = 27.26, p < 0.05) and the quadratic model (Δχ2(6) = 29.73, p < 0.05) improved model fit. When comparing the freely estimated models, the quadratic model fit significantly better than the linear model (Δχ2(8) = 45.63, p < 0.05). In fact, the quadratic model with freely estimated means and variances provided an excellent fit to the data (see Table 2). Girls showed slightly higher levels of depression than boys at age 11, but the difference was small. The linear factor suggests that depression increased more for girls than for boys. The quadratic trend (which represents the slope of the tangent line to the curve) indicated a negative trajectory for girls and a positive trajectory for boys. Over time girls’ depression scores increased, but then leveled off, whereas boys’ depression was low initially, but then increased more rapidly at later ages. See Figure 1.
Figure 1.
Quadratic latent growth curve model freely estimated across gender.
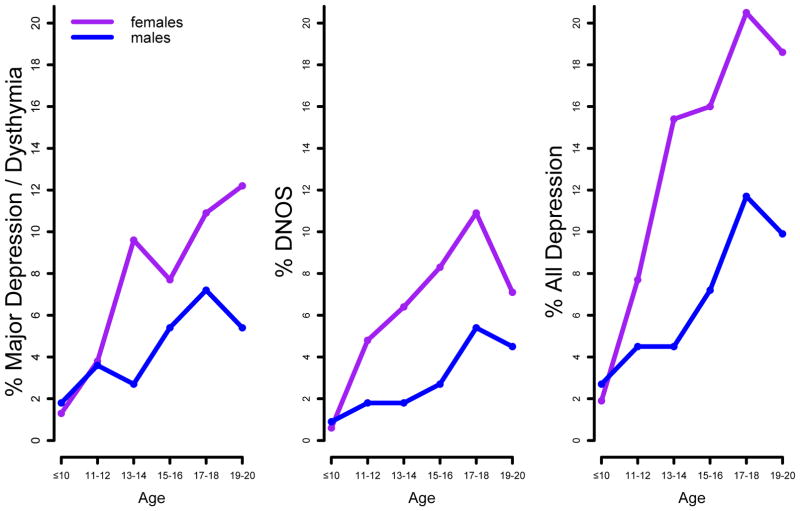
Gender Differences in Depression Diagnoses and the LDI
Descriptive statistics for each 2-year prevalence of depression diagnoses across adolescence are presented in Table 3. By age 20, 38 females (24%) had experienced at least one episode of major depression or dysthymia, compared to 16 males (15%). There was a significant association between gender and depression diagnosis by age 20, p = .032, Fisher’s exact test, OR = 1.91, 95% CI [1.00, 3.63]. There was not a significant difference in age at first onset of major depression/dysthymia between males (M = 14.94, SD= 3.71) and females (M = 15.86, SD= 3.34, p = 0.39). By age 20, 10 females (6%) and 2 males (2%) had experienced an episode of recurrent major depression/ dysthymia. The gender difference in major depression/dysthymia appeared during the age 13–14 interval (see Table 3, Figure 2).
Table 3.
Descriptive statistics for 2-year prevalence of depression diagnoses.
| Females n = 156 | Males n = 111 | Gender Difference | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Depression Diagnoses | n | % | n | % | p-value | OR |
| Major & Dysthymia | ||||||
| By age 10 | 2 | 1.3 | 2 | 1.8 | .553 | 0.71 |
| Ages 11, 12 | 6 | 3.8 | 4 | 3.6 | .594 | 1.07 |
| Ages 13, 14 | 15 | 9.6 | 3 | 2.7 | .021* | 3.83 |
| Ages 15, 16 | 12 | 7.7 | 6 | 5.4 | .317 | 1.46 |
| Ages 17, 18 | 17 | 10.9 | 8 | 7.2 | .211 | 1.57 |
| Ages 19, 20 | 19 | 12.2 | 6 | 5.4 | .046* | 2.43 |
| DNOS | ||||||
| By age 10 | 1 | 0.6 | 1 | 0.9 | .660 | 0.71 |
| Ages 11, 12 | 6 | 4.8 | 2 | 1.8 | .280 | 2.18 |
| Ages 13, 14 | 10 | 6.4 | 2 | 1.8 | .064 | 3.73 |
| Ages 15, 16 | 13 | 8.3 | 3 | 2.7 | .046* | 3.27 |
| Ages 17, 18 | 17 | 10.9 | 6 | 5.4 | .086 | 2.14 |
| Ages 19, 20 | 11 | 7.1 | 5 | 4.5 | .277 | 1.61 |
| All Diagnoses | ||||||
| By age 10 | 3 | 1.9 | 3 | 2.7 | .489 | 0.71 |
| Ages 11, 12 | 12 | 7.7 | 5 | 4.5 | .215 | 1.77 |
| Ages 13, 14 | 24 | 15.4 | 5 | 4.5 | .003* | 3.85 |
| Ages 15, 16 | 25 | 16.0 | 8 | 7.2 | .022* | 2.46 |
| Ages 17, 18 | 32 | 20.5 | 13 | 11.7 | .040* | 1.95 |
| Ages 19, 20 | 29 | 18.6 | 11 | 9.9 | .035* | 2.08 |
p <.05.
Figure 2.
Development of overall rates of depression (2-year prevalence combining new cases and recurrences) by age, gender, and type of depression.
By age 20, 36 females (23%) had experienced at least one episode of DNOS, compared to 12 males (11%). There was a significant association between gender and DNOS diagnosis by age 20, p = .007, Fisher’s exact test, OR = 2.48, 95% CI [1.22, 5.01]. There was not a significant difference between males (M = 16.08, SD= 3.32) and females (M = 15.33, SD= 2.66) in age at first onset of DNOS (p = 0.49). By age 20, 8 females (5%) and 3 males (3%) had experienced an episode of recurrent DNOS. The gender difference in DNOS emerged during the age 15–16 interval (see Table 3, Figure 2).
By age 20, combining all depression diagnoses, 62 females (40%) and 25 males (23%) had experienced at least one episode of clinically diagnosable depression. This gender difference was statistically significant, p = .002, Fisher’s exact test, OR = 2.27, 95% CI [1.31–3.92]. Across all depression diagnoses, there was not a significant difference between males (M = 15.30, SD= 3.56) and females (M = 15.11, SD= 2.96) in age at first onset (p = 0.70). By age 20, 26 females (17%) and 5 males (5%) had experienced a recurrent episode of depression. The gender difference in all depression diagnoses emerged during the age 13–14 interval (see Table 3, Figure 2).
Overall then, significantly more females than males experienced clinical depression by age 20. Combining across all depression diagnoses, the gender difference emerged during the age 13–14 interval. The developmental pattern of the gender difference in depression suggests that girls experienced increases in diagnoses in early adolescence while boys experienced increases in diagnoses in later adolescence (see Figure 2).
Descriptive statistics for the LDI are presented in Table 4. There were no significant gender differences in the LDI. Thus, among those with clinical depression, boys and girls spent a similar percentage of their days clinically depressed.
Table 4.
Descriptive statistics for Lifetime Depression Index.
| Females | Males | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| LDI | n | Mean | Median | Range | n | Mean | Median | Range | p-value |
| Major and/or Dysthymiaa | 38 | 5.26% | 2.40% | 0.18 - 34.57% | 16 | 7.40% | 2.55% | 0.19 –44.98% | .42 |
| DNOS | 36 | 2.96% | 1.30% | 0.09 – 18.32% | 12 | 3.62% | 2.20% | 0.11 – 16.37% | .63 |
| All Depressiona | 62 | 4.94% | 2.86% | 0.18 –34.57% | 25 | 6.48% | 2.10% | 0.13 –44.98% | .40 |
All of the models examining gender differences in the LDI violated the General Linear Model (GLM) assumption of normality; however, the coefficients are still the best, unbiased, efficient estimators among linear solutions.
These models violated the GLM assumption of constant variance. Log transforming the data corrected the violations, and no gender differences remained in the LDI among the log-transformed data.
Discussion
We set out to answer two questions. First, what is the developmental pattern of the emergence of the gender difference in depression in adolescence in a contemporary sample? Second, among those adolescents who experience depression, is there a gender difference in the chronicity burden of the disorder (i.e., do girls or boys spend more days of their lives clinically depressed)? We observed gender differences in depression symptoms and diagnoses beginning at age 13. We also discovered a gender similarity in the chronicity burden of clinical depression.
Developmental Patterns of Gender Differences in Depression
Depression symptoms and diagnoses provided converging evidence for the pattern of gender differences in depression throughout adolescence in our sample. The gender difference emerged at age 13 for depression symptoms and at the age 13–14 interval for diagnoses. The age at which a gender difference in depression symptoms and diagnoses appears is similar to findings from the 1980s and 1990s (Angold et al., 1998; Hankin et al., 1998; Twenge & Nolen-Hoeksema, 2002), despite many social changes that have occurred in the intervening period.
It is important to note that the gender difference in depression diagnoses was found at the age 13–14 interval in our sample, in contrast to the age 14–15 interval in the study by Hankin and colleagues (1998). However, Hankin et al. (1998) did not assess for depression at the age 13–14 interval; they only assessed from 12–13 when there was no gender difference and 14–15 when there was a gender difference. Repeated depression assessments over shorter follow-up periods may allow for a more refined understanding of the timing of the emergence of the gender difference depression. For example, in an accelerated longitudinal cohort design, Hankin et al. (2015) recently reported that the gender difference in clinical depression emerges at age 12.5, slightly younger than the findings from the current study.
Although the age at which a gender difference emerged in our sample of adolescents from the 2000s is similar to the findings from the 1980s and 1990s, the magnitude of the gender difference in depression symptoms was larger in our sample compared to previous findings. In a meta-analysis on gender differences in depression symptoms covering cohorts born from 1964 to 1988 (and therefore reaching adolescence in the 1970s through 1990s), Twenge and Nolen-Hoeksema (2002) reported an effect size of .08 at age 13, and roughly .20 at ages 14 through 16. In our sample, the effect size for the gender difference in depression symptoms was roughly .40 at ages 13 and 15.
We also documented distinct developmental trajectories of depression symptoms across adolescence for boys and girls. Latent growth curve modeling of depression symptoms indicated a positive quadratic trajectory for girls and a negative quadratic trajectory for boys. Girls’ depression symptoms accelerated early in adolescence and boys’ depression symptoms accelerated later in adolescence. The pattern of results from the current analysis is similar to the developmental trajectories documented among adolescents in the 1980s and 1990s by Ge and colleagues (2001).
Consistent with the symptom data, in our sample, girls’ rates of depression diagnoses increased from ages 11 through 14, whereas boys’ rates of depression diagnoses increased from ages 15 through 18. Thus, based on both the symptom and diagnostic data, a picture emerges in which contemporary adolescent girls experience increases in depression in early adolescence and boys experience increases in depression in late adolescence. If this finding is replicated, an important area for future research will be identifying risk factors for depression for boys and girls in these different developmental periods. Do boys and girls have different risk factors for depression, or similar risk factors that increase for girls in early adolescence and for boys in late adolescence? These results also suggest different developmental windows for depression prevention programs for girls and boys in adolescence. Given the developmental trends in our data, one possibility is that as these youth become adults, the gender gap may disappear (i.e., the boys will catch up to the girls). We observed this trend at age 18 for depression symptoms in our dataset. Due to boys’ acceleration from ages 15 to 18, the gender difference in depression at age 18 was not significant.
Chronicity Burden
Although we observed gender differences in depression symptoms and diagnoses, we found a gender similarity in the chronicity burden of adolescent depression. Almost twice as many girls (24%) had experienced major depression/ dysthymia by age 20 compared to boys (15%); however, adolescent girls and boys who obtained depression diagnoses spent a similar number of days clinically depressed by age 20. To our knowledge, this is the first study to examine gender differences in depression chronicity.
Often a strong emphasis is placed on the impairment associated with female depression, which is important given that females are more likely to become depressed compared to males. However, our results suggest that we should not overlook the chronicity burden associated with males’ depression. It will be important to determine if this gender similarity in the LDI replicates and remains throughout adulthood. An additional agenda for future research should be identifying factors that place individuals at risk for experiencing a high LDI by age 20. Fortunately, most adolescents in our community sample did not spend more than one year depressed by the age of 20, but that still represents a substantial burden.
Strengths and Limitations
A major strength of the current study is its longitudinal design and prospective assessment of depression symptoms. Emphasizing the importance of symptom measures, a recent meta-analysis concluded that dimensional measures of psychopathology are reliable and valid (Markon et al., 2011). The examination of both depression symptoms and diagnoses provided converging evidence regarding gender differences in depression across adolescence. Another major strength is the examination of chronicity burden and the identification of different trajectories of depression symptoms for boys compared with girls. In addition, the youth in our sample experienced adolescence recently, between 2002 and 2012.
This study cannot be generalized to ethnic groups other than Whites. We encourage future research in ethnic minority populations. Although the detailed assessment of lifetime history of depression diagnoses is also noteworthy, the retrospective report of depression diagnoses is a limitation (Moffitt et al., 2010). However, given that the average age of depression onset was 15 in this sample, most participants were recalling symptoms from only the past 5.5 years. Additionally, individuals who had experienced any depressive episode by age 20 had significantly more depression symptoms (measured prospectively) at ages 13, 15, and 18, providing validation for the diagnoses. The LDI for all depression diagnoses also correlated significantly with adolescent depression symptoms at all four ages. Lastly, the sample size for the diagnostic interviews was relatively small; however, the sample size for symptom data was larger and conclusions from the symptom and diagnostic data converged.
Conclusions
In a contemporary sample of U.S. adolescents, girls experienced increases in depression symptoms and diagnoses in early adolescence while boys did not develop higher levels of symptoms and diagnoses until late adolescence. Although girls were more likely than boys to develop depression diagnoses by age 20, those boys who did develop clinical depression experienced the same chronicity burden as girls who developed clinical depression. Given changes in recent decades in the social environment for adolescents in the U.S., the findings of somewhat larger gender differences in depression symptoms at ages 13 and 15 (compared to those documented in the 1980s and 1990s) are critical to continue monitoring. Future research should seek to identify cultural changes that may influence depression in adolescent girls and boys.
Highlights.
Gender differences in depression in a contemporary sample emerged at age 13.
Girls’ depression symptoms accelerated early in adolescence.
Boys’ depression symptoms accelerated later in adolescence.
The chronicity burden of clinical depression is similar for boys and girls.
Acknowledgments
We thank Mollie N. Moore, Dominika Swistun, Holly Flores, Samantha Anderson, and Samantha Prust for help with data collection. We thank the families of the Wisconsin Study of Families and Work for their continued loyalty and participation over many years.
Footnotes
This material is based upon work supported by the National Science Foundation Graduate Research Fellowship (DGE- 071823 to Rachel Salk); the National Institute of Mental Health (R01MH44340 to Janet Shibley Hyde); the Graduate School and the Office of the Vice Chancellor for Research and Graduate Education at the University of Wisconsin-Madison with funding from the Wisconsin Alumni Research Foundation (University Fellowship to Salk); and a University of Wisconsin Graduate School grant to Janet Shibley Hyde. The content is solely the responsibility of the authors, and any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Science Foundation or National Institute of Mental Health.
Average annual family income at the beginning of the study (1990–1991; at which time all women were living with a husband or partner and 81.5% of the women were employed) was $49,500 (median = $45,000; range = $2000–$200,000). In 1991, the median income of married couple families with the wife in the paid labor force was $48,169 (U.S. Department of Labor, 1993). Therefore, the sample matches the national figure well.
At the beginning of the study, 1.8% of women had achieved less than a high school education; 15.4% graduated from high school; 9.6% received some technical training beyond high school; 19.8% had some college; 34.9% had earned a college degree; 7.5% received some education beyond the college degrees; and 10.9% had completed a masters, doctoral, or professional degree.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. American Psychiatric Association; Washington, DC: 2000. text rev. [Google Scholar]
- American Psychological Association. Report of the APA Task Force on the Sexualization of Girls. Washington, DC: American Psychological Association; 2010. American Psychological Association, Task Force on the Sexualization of Girls. Retrieved from http://www.apa.org/pi/women/programs/girls/report-full.pdf. [Google Scholar]
- Angold A, Costello EJ, Worthman CM. Puberty and depression: The roles of age, pubertal status, and pubertal timing. Psychol Med. 1998;28:51–61. doi: 10.1017/s003329179700593x. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Hoboken, NJ: Wiley; 1993. [Google Scholar]
- Bor W, Dean AJ, Najman J, Hayatbakhsh R. Are child and adolescent mental health problems increasing in the 21st century? A systematic review. Aust N Z J Psychiatry. 2014;48:606–616. doi: 10.1177/0004867414533834. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage Publications; 1993. pp. 136–162. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/ correlation analysis for the behavioral sciences. 3. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- Essau CA, Lewinsohn PM, Seeley JR, Sasagawa S. Gender differences in the developmental course of depression. J Affect Disorders. 2010;127:185–190. doi: 10.1016/j.jad.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psyciat. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P, 1/2007 revision) New York: Biometrics Research, New York State Psychiatric Institute; Nov, 2002. [Google Scholar]
- Garber J, Keily MK, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. J Consult Clin Psychol. 2002;70:79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Ge X, Conger RD, Elder JH., Jr Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Dev Psychol. 2001;37(3):404–417. doi: 10.1037//0012-1649.37.3.404. [DOI] [PubMed] [Google Scholar]
- Graff KA, Murnen SK, Krause AK. Low-cut shirts and high-heeled shoes: Increased sexualization across time in magazine depictions of girls. Sex Roles. 2013;69(11–12):571–582. [Google Scholar]
- Hankin BL, Abramson L, Moffitt T, Silva P, McGee R, Angell K. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Young JF, Abela JR, Smolen A, Jenness JL, Gulley LD, Technow JR, Gottlieb AB, Cohen JR, Oppenheimer CW. Depression from childhood into late adolescence: Influence of gender, development, genetic susceptibility, and peer stress. J Abnorm Psychol. 2015;124:803–816. doi: 10.1037/abn0000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haroon E, Raison CL, Miller AH. Psychoneuroimmunology meets neuropsychopharmacology: Transitional implications of the impact of inflammation on behavior. Neuropsychopharmacology. 2012;37:137–162. doi: 10.1038/npp.2011.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hidaka BH. Depression as a disease of modernity: Explanations for increasing prevalence. J Affect Disorders. 2012;140:205–214. doi: 10.1016/j.jad.2011.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyle RH, editor. Structural equation modeling: Concepts, issues, and applications. Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- Hyde J, Klein M, Essex M, Clark R. Maternity leave and women’s mental health. Psychol Women Q. 1995;19:257–285. [Google Scholar]
- Jose PE, Kljakovic M, Scheib E, Notter O. The joint development of traditional bullying and victimization with cyber bullying and victimization in adolescence. J Res Adolesc. 2011;22:301–309. [Google Scholar]
- Klein DN, Shankman SA, Lewinsohn PM, Seeley JR. Subthreshold depression in adolescents: Predictors of escalation to full syndrome depressive disorders. J Am Acad Child Adolesc Psychiatry. 2009;48:703–710. doi: 10.1097/CHI.0b013e3181a56606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacol Bull. 1985;21:995–998. [PubMed] [Google Scholar]
- Lampard AM, MacLehose RF, Eisenberg ME, Neumark-Sztainer D, Davison KK. Weight-related teasing in the school environment: Associations with psychosocial health and weight control practices among adolescent boys and girls. J Youth Adolesc. 2014;43:1770–1780. doi: 10.1007/s10964-013-0086-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. J Abnorm Psychol. 2000;109:345–351. [PubMed] [Google Scholar]
- Little TD. Mean and covariance structures (MACS) analyses of cross-cultural data: Practical and theoretical issues. Multivariate Behav Res. 1997;32:53–76. doi: 10.1207/s15327906mbr3201_3. [DOI] [PubMed] [Google Scholar]
- Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep, and exercise. J Affect Disorders. 2012;148:12–27. doi: 10.1016/j.jad.2013.01.014. [DOI] [PubMed] [Google Scholar]
- Markon KE, Chmielewski, Miller CJ. The reliability and validity of discrete and continuous measures of psychopathology: A quantitative review. Psychol Bull. 2011;137:856–879. doi: 10.1037/a0023678. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR. Longitudinal associations between alcohol problems and depressive symptoms: Early adolescence through early adulthood. Alcoholism: Clinical and Experimental Research. 2009;33(1):49–59. doi: 10.1111/j.1530-0277.2008.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh HW, Hau K-T, Grayson D. Goodness of fit evaluation in structural equation modeling. In: Maydeu-Olivares A, McCardle J, editors. Contemporary psychometrics: A Festschrift to Roderick P. McDonald. Mahwah, NJ: Lawrence Erlbaum Associates; 2005. pp. 275–340. [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, … Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCSA) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40:899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5. Los Angeles: Muthén & Muthén; 2007. [Google Scholar]
- Nolen-Hoeksema S, Girgus J. The emergence of gender differences in depression during adolescence. Psychol Bull. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Rawana JS, Morgan AS. Trajectories of depressive symptoms from adolescence to young adulthood: The role of self-esteem and body-related predictors. J Youth Adolesc 2014. 2014;43:597–611. doi: 10.1007/s10964-013-9995-4. [DOI] [PubMed] [Google Scholar]
- Rose DT, Abramson LY, Hodulik CJ, Halberstadt L, Leff G. Heterogeneity of cognitive style among depressed inpatients. J Abnorm Psychol. 1994;103:419–429. doi: 10.1037//0021-843x.103.3.419. [DOI] [PubMed] [Google Scholar]
- Twenge J, Nolen-Hoeksema S. Age, gender, race, socioeconomic status, and birth cohort differences in the Children’s Depression Inventory: A meta-analysis. J Abnorm Psychol. 2002;111:578–588. doi: 10.1037//0021-843x.111.4.578. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Labor. 20 facts on women workers. Washington, DC: U.S. Government Printing Office; 1995. [Google Scholar]
- van Ginkel JR, Kroonenberg PM. Analysis of variance of multiply imputed data. Multivariate Behav Res. 2014;49(1):78–91. doi: 10.1080/00273171.2013.855890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL. Sex differences and the epidemiology of depression. Arch Gen Psyciat. 1977;34:98–111. doi: 10.1001/archpsyc.1977.01770130100011. [DOI] [PubMed] [Google Scholar]
- Zis AP, Goodwin FK. Major affective disorder as a recurrent illness: a critical review. Arch Gen Psyciat. 1979;36:835–839. doi: 10.1001/archpsyc.1979.01780080009002. [DOI] [PubMed] [Google Scholar]