Abstract
Background:
Allergists commonly perform intradermal skin testing (IDST) after negative skin-prick testing (SPT) to comprehensively diagnose environmental allergic sensitization. However, with the availability of modern methods to detect serum-specific immunoglobulin E (ssIgE), it is unclear if ssIgE testing could substitute for IDST.
Objective:
To determine the efficacy of ssIgE testing and IDST when added to SPT in diagnosing environmental allergic sensitizations.
Methods:
SPT, IDST, and ssIgE testing to nine common environmental allergens were analyzed in 75 patients with oculonasal symptoms who presented to our allergy clinics in the Bronx, New York, between January 2014 and May 2015.
Results:
A total of 651 SPT and 499 ssIgE tests were independently performed and revealed 162 (25%) and 127 (25%) sensitizations, respectively. When SPT results were negative, IDST results revealed 108 of 452 additional sensitizations (24%). In contrast, when SPT results were negative, ssIgE test results only revealed 9% additional sensitizations. When both SPT and IDST results were negative, ssIgE testing only detected 3% of additional sensitizations, and ssIgE levels were typically low in these cases (median, 1.25 kU/L; range, 0.357–4.47 kU/L). When both SPT and ssIgE test results were negative, IDST results detected 15% additional sensitizations.
Conclusion:
IDST detected more additional environmental sensitizations compared with ssIgE testing. IDST, therefore, may be useful when the SPT and/or ssIgE testing results were negative, but the exposure history indicated relevant allergic sensitization. Serology added only a little more information if both SPT and IDST results were negative but may be useful in combination with SPT if IDST cannot be performed.
Keywords: Skin prick testing, intradermal skin testing, serum-specific immunoglobulin E, additional environmental allergen sensitizations
Establishing a diagnosis of immunoglobulin E (IgE) mediated environmental allergy is one of the most common tasks in allergy practice. Skin-prick testing (SPT) is traditionally favored by most allergists because it is relatively simple to apply, provides fast results, is highly predictive of clinical allergy, and is safe.1,2 Accordingly, the 2008 Practice Parameter3 states that SPT is the preferred method of diagnosing environmental allergies, notwithstanding the fact that today's widely commercially available serum-specific IgE (ssIgE) testing methods (e.g., ImmunoCap [Phadia, Uppsala, Sweden] and Immulite [Siemens Health Care Diagnostics, Tarrytown, NY]) have been shown to be as sensitive as SPT.1–7 Hence, the American Academy of Pediatrics8 and Asthma Management guidelines set forth by the National Asthma Education and Prevention Program5 in 2007 recommend either SPT or ssIgE testing to establish a diagnosis of environmental allergies.
However, the diagnostic yield of SPT and ssIgE testing can differ substantially, depending on the specific allergen.8 For example, Bousquet et al.4 showed, in a multicenter study, that, among 3140 patients sensitized to dust mite, SPT alone or ssIgE (ImmunoCap) testing alone would have missed 13 and 29% of sensitizations, respectively, compared with a combination of ssIgE testing and SPT. These findings indicated that the combination of SPT and ssIgE is more comprehensive than either test alone in diagnosing environmental sensitizations. Nevertheless, instead of ssIgE testing, many allergists in the United States use intradermal skin testing (IDST) to detect additional sensitizations when clinical suspicion of specific sensitizations persists despite negative SPT results. This is not unreasonable because it has been shown that IDST may pick up 10–30% additional sensitizations, and, if higher concentrations are used, even >50% of additional sensitizations are found compared with SPT alone.2,9–11 However, it is not well established how much information is gained through IDST compared with ssIgE testing when the SPT result is negative. As of yet, studies to determine the yield of ssIgE and IDST in diagnosing multiple allergen sensitizations in daily allergy practice have not been performed. In our study, we aimed to determine the yield of IDST in comparison with ssIgE testing when added to SPT in diagnosing environmental allergic sensitizations to nine common allergens in northeastern United States.
METHODS
Study Participants
A retrospective chart review was conducted of all the patients who presented for evaluation of perennial or seasonal oculonasal symptoms in the allergy clinic at Jacobi Medical Center and one clinic at Montefiore Medical Center between January 2014 and May 2015. The protocol was approved by the institutional review board of Albert Einstein College of Medicine. Seventy-five subjects had SPT, IDST, and ssIgE testing performed.
SPTs
SPT was performed to nine common allergens in northeastern United States (Greer Laboratories, Inc., Lenoir, NC): tree pollen, grass pollen, ragweed pollen, mugwort pollen, cat, dog, mouse, dust mite, and cockroach (Table 1). All allergen extracts were applied by using the ComforTen applicator (Hollister-Stier Laboratories, Spokane, WA) and were read at 15–20 minutes. Histamine dihydrochloride 10 mg/mL (Hollister-Stier Laboratories) was used as a positive control, and 50% glycerol saline solution was used as negative control. A “grade 1” positive SPT result was defined as a wheal diameter 2–4 mm larger than the negative control, “grade 2” was 4–7 mm larger, “grade 3” was 7–10 mm larger, and “grade 4” was >10 mm larger or pseudopods were present. If the SPT result was negative, then the IDST to that environmental allergen was performed if the patient was considered to be a candidate for allergy immunotherapy or if his or her history indicated additional environmental allergies despite a negative SPT result.
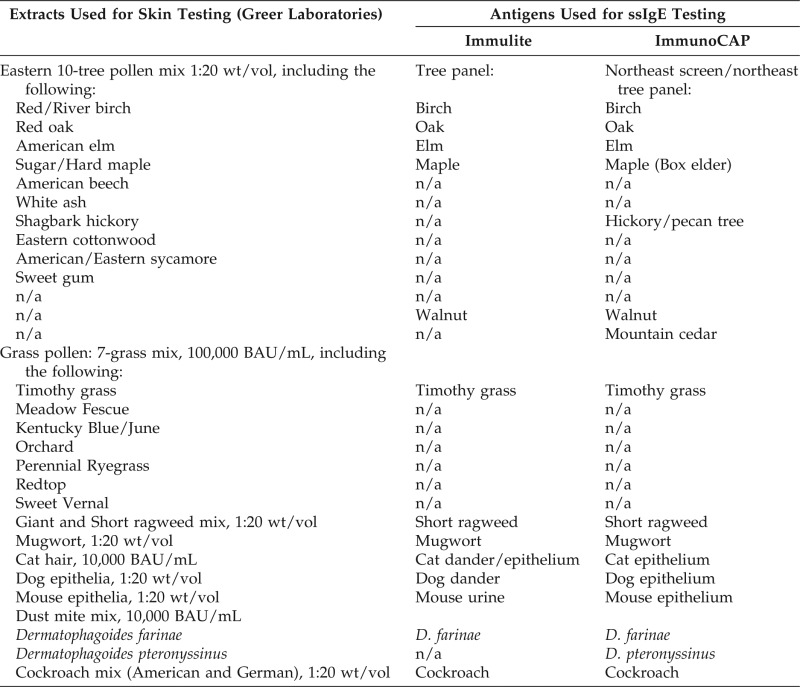
Table 1.
Environmental allergens used for skin testing and serologic testing
ssIgE = serum-specific immunoglobulin E; n/a = not available.
IDSTs
IDSTs were done independently of ssIgE results. Intradermal allergen extracts were prepared from the same source products as for SPT. The protocol for IDST differed by provider and clinic site. The first protocol (protocol 1) used IDST in two steps: first, patients underwent IDST at low concentrations (tree, 200 PNU/mL; grass, 500 AU/mL; ragweed, Amb A1 0.4 μg/mL; mugwort, 200 PNU/mL; cat, 50 BAU/mL; dog, 100 PNU/mL; mouse, 200 PNU/mL; dust mite, 500 PNU/mL; and cockroach, 250 PNU/mL). If the results were negative but the provider believed that further testing was clinically indicated, then a second step, at 10-fold higher concentrations, was performed at a third visit. Another provider tested patients directly with higher concentrations (protocol 2) (one step): tree, 1000 PNU/mL; grass, 1000 AU/mL; ragweed, Amb A1 1.4 μg/mL; mugwort, 1000 PNU/mL; cat, 100 BAU/mL; dog, 1000 PNU/mL; mouse, 1000 PNU/mL; dust mite, 1000 BAU/mL; and cockroach, 1000 PNU/mL. For simplification of the analysis, the IDST results were based on the higher concentrations only, in addition to IDST results at lower concentrations in patients who did not proceed with the higher concentrations (e.g., because of missed visits or because further testing was not deemed clinically necessary by the provider).
Detection of ssIgE Levels
The ssIgE levels to environmental allergens were tested by using the ImmunoCAP method or Immulite method, independent of the SPT results. Levels of <0.35 kU/L were considered negative and ≥0.35 kU/L was considered positive. The allergens used for ssIgE testing differed slightly from those used for skin testing (Table 1). For example, a mixture of 10 tree pollens was used for SPT and IDST, whereas the ssIgE levels were tested to 5–7 tree pollens (all found in the skin-testing mix), based on what the laboratory offered at each clinical site. If at least one of the tests of individual trees had ssIgE levels of ≥0.35 kU/L, then the tree testing was considered positive.
Statistical Methods
Descriptive statistics were applied to all the variables. Continuous variables of nonparametric distribution were described as the median and range, and parametrically distributed variables were described as the mean and standard deviation. The data were analyzed by using Microsoft Office Excel 2010 (Microsoft Inc, Redmond, WA) and STATA SE11 statistical software (StataCorp, College Station, TX).
RESULTS
Baseline characteristics of the patients included in the study are summarized in Table 2. Women and Hispanic ethnicity were predominant in our study population.
Table 2.
Demographic and clinical characteristics of the study population

IgE = Immunoglobulin E.
*Three patients were <18 years old.
§Included only patients in whom seasonality of symptoms was clear based on a chart review; patients with symptoms that overlapped three seasons were not included; patients in whom the symptoms seasonality was not mentioned in the chart were not included.
#The percentage is of the total number of patients for whom symptom seasonality was recorded (n = 51).
¶Two patients had total serum-specific IgE reported as >2000 kU/L (the levels were converted to 2001 kU/L for analysis purpose).
Overview of Study Flow
The 75 patients underwent a total of 651 SPTs (Fig. 1). Because mugwort pollen skin testing was only introduced after the timeline for inclusion in this study, the first 24 patients had missing data on mugwort SPTs. Fifty-seven patients had at least one positive SPT result, with a median of two positive SPT results for each patient (range, 1–8). A total of 499 ssIgE tests were performed, and 44 patients had at least one positive ssIgE test result, which resulted in 127 of 499 positive test results (25%). In most subjects who had negative SPT results, IDST was performed. In total, results of 108 of 452 IDSTs (24%) were positive.
Figure 1.
Decision tree regarding the use of skin-prick testing (SPT), intradermal skin prick testing (IDST), and serum-specific immunoglobulin E (ssIgE).* If the SPT result was negative, then the IDST to that environmental allergen was performed if the patients were considered to be candidates for allergy immunotherapy or if the history indicated additional allergies despite negative SPT results. IDSTs were performed independently of ssIgE results.** The ssIgE testings were performed independently of skin testing results.
Comparison of SPT with ssIgE Testing
A total of 499 SPT–ssIgE pairs were available for analysis; 115 SPT results (23%) were positive and 127 ssIgE levels (25%) were positive (Fig. 1). Overall, ssIgE results revealed 9% additional sensitizations when the corresponding SPT results were negative. Similarly, SPT results revealed 7% additional sensitizations when the corresponding ssIgE results were negative (Figs. 2 and 3 A). For grass and ragweed, ssIgE testing detected additional sensitizations that were not shown by SPT. For the other tested allergens, ssIgE testing detected some additional sensitizations that were not found by SPT and vice versa (Fig. 3 A).
Figure 2.

The proportion of additional sensitizations detected through serum-specific immunoglobulin E (ssIgE) and intradermal skin prick testing (IDST) when skin-prick testing (SPT) results were negative, through SPT and IDST (done in cases of negative SPT results) when ssIgE levels were negative, and through ssIgE testing when IDST (done in cases of negative SPT results) were negative.
Figure 3.
Concordance and discordance of the following: (A) Skin-prick testing (SPT) and serum-specific immunoglobulin E (ssIgE) test results. (B) Intradermal skin prick testing (IDST) results and ssIgE levels (in 362 SPTs with negative results for which all three tests were done; the percentage is of the total number of patients who had all three tests done).
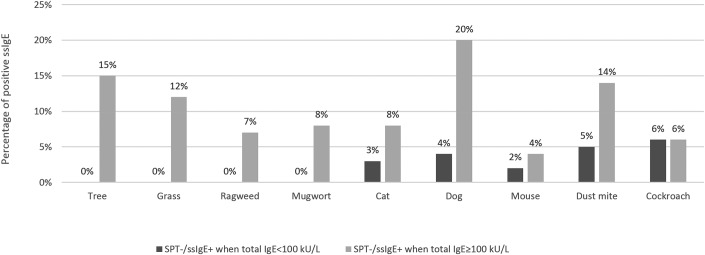
Environmental sensitizations detected through serologic testing in allergens with corresponding negative SPT results were more likely in patients with a total serum IgE level of ≥100 kU/L (Fig. 4). In this group, the rate of positive ssIgE results ranged from 4 to 20% for each allergen tested (highest for dog and trees), whereas, for patients with a total IgE level of <100 kU/L and a negative SPT result, the rate of positive ssIgE results ranged from 0 to 6% (percentages are of all patients who had SPT, ssIgE, and total IgE performed for each allergen tested). Among the 35 positive SPT results with corresponding negative ssIgE levels, the SPT wheal diameters were not always small (e.g., to cat and dust mite) (Table 3). Similarly, there were some high ssIgE levels despite negative corresponding SPT results (e.g., to trees and dog) (Table 4). Among 18 patients who had completely negative SPT results for all nine allergens tested, only 1 patient showed one positive serologic sensitization (dust-mite ssIgE level, 4.41 kU/L) (data not shown).
Figure 4.
The rate of positive serum-specific immunoglobulin E (ssIgE) results in patients with negative corresponding skin-prick testing (SPT) results based on total immunoglobulin E (IgE) levels (total IgE of <100 kU/L versus total IgE level of ≥100 kU/L, respectively).
Table 3.
Grades of positive skin-prick test results when the corresponding ssIgE was negative (35 test pairs)

ssIgE = Serum-specific immunoglobulin E; SPT = skin-prick test.
Table 4.
The level of ssIgE for allergens with negative corresponding skin test results
ssIgE = Serum-specific immunoglobulin E; SPT = skin-prick test; IDST = intradermal skin prick testing.
Comparison of IDST with ssIgE when SPT Result Was Negative
The ssIgE testing and IDST were performed in 362 negative SPT. Overall, IDST results revealed more sensitizations when compared with ssIgE testing (Fig. 3 B). The majority of negative SPT results (74% [269/362]) were confirmed through both IDST and ssIgE testing. However, IDST results revealed 23% additional sensitizations (82/362) when corresponding SPT results were negative. Of these 82 positive IDST results, only 29 (35%) could also be detected serologically. The number of additional sensitizations and the concordance or discordance between IDST and ssIgE varied among allergens. For tree and ragweed, IDST alone revealed many additional sensitizations, whereas ssIgE alone did not reveal any. For most of the other allergens (grass, dust mite, cat, dog, cockroach, and mouse), IDST alone revealed many more additional sensitizations than did ssIgE alone.
The only exception was mugwort, for which ssIgE testing alone revealed some additional sensitizations, whereas IDST alone did not. The results of all three types of testing are shown in Table 5. Serologic testing alone only revealed 3% of additional sensitizations (11/362) when SPT and IDST results were negative, whereas IDST detected 15% additional sensitizations (53/362) when SPT and ssIgE results were negative (Fig. 2, Table 5). As expected, detectable ssIgE levels were generally low when the corresponding IDST was negative (Table 4). Among the 18 patients with negative SPT results to all nine allergens tested, 9 patients showed sensitizations on IDST.
Table 5.
IDST and ssIgE results for each aeroallergen
IDST = Intradermal skin prick testing; ssIgE = serum-specific immunoglobulin E.
*Percentage of IDST–ssIgE pairs.
#Percentage of positive IDST results.
§Percentage of negative IDST results.
¶Percentage of positive ssIgE results.
‖Percentage of negative ssIgE results.
SPT–ssIgE Pairs in Patients with Symptoms in the Spring-Summer (trees and grass pollens were analyzed) or Perennial Symptoms (dust mite, cockroach, mouse, and cat were analyzed)
In patients who reported seasonal allergic rhinoconjunctivitis, 9 of 12 (75%) had positive ssIgE levels to trees and 6 of 8 (75%) to grass, whereas 13 of 30 (43%) had positive SPT to trees, and 7 of 30 (23%) had positive SPT results to grass. When SPT results were negative and ssIgE testings were performed, ssIgE results revealed 17 and 38% additional sensitizations for tree pollen and grass pollen, respectively. (Fig. 5 A) Of patients who had perennial symptoms and who had both SPT and ssIgE testing done, no additional serologic sensitizations were found for dust mite, roach, and mouse when the corresponding SPT result was negative, whereas SPT revealed additional sensitizations when the ssIgE test result was negative for all perennial allergens analyzed (Fig. 5 B). All perennial serologic sensitizations were confirmed by SPT. IDST results were not analyzed because of the low number of tests performed in these groups.
Figure 5.
Pairs of skin-prick testing (SPT) and serum-specific immunoglobulin E (ssIgE) results in patients symptomatic in (A) Spring-Summer (tree, grass) and (B) perennial (dust mite, cockroach, mouse, cat).
DISCUSSION
The aim of this study was to determine the yield of ssIgE testing and IDST when added to SPT in diagnosing multiple environmental allergic sensitizations. Both, IDST and ssIgE testing diagnosed additional sensitizations after negative SPT results, with IDST detecting more than twice additional sensitizations compared with ssIgE testing (23 versus 9%). When both SPT and IDST results were negative, only 3% additional sensitizations were revealed through serologic testing. In this study, we did not aim to determine clinical relevance of allergic sensitizations. A positive SPT, ssIgE level, or IDST result reflected that the patient was immunologically sensitized to that specific allergen, but it did not guarantee that the patient would develop allergic symptoms when exposed to the allergen in question. Even though allergen provocation tests are used in some research settings as the criterion standard to diagnose clinical environmental allergies, they are impractical in the everyday allergy office.12 Moreover, provocation tests do not take into account multiple and chronic allergen exposures because they occur in real life and, therefore, may underestimate the clinical relevance of sensitizations. Because of this uncertainty, most allergists in the United States prescribe allergy immunotherapy based on a comprehensive diagnosis of allergen sensitization in combination with a thorough allergen exposure history.
Similar to other studies,4,13 when considering only patients who are sensitized, the proportions of mismatched SPT–ssIgE results were much larger, with a median of 27% (range, 13–60%) of sensitizations missed by SPT testing alone (e.g., to grass, ragweed, and dog) and 17% (range, 0–39%) of sensitizations missed by ssIgE testing alone (e.g., to cockroach) (Fig. 3 A, upper 3 boxes of the bars). Consistent with our results, Calabria et al.1 showed that, among 78 individuals sensitized to cockroach, 46% would have been missed by ssIgE testing (ImmunoCap) alone and 29% would have been missed by SPT alone. The same study found that, among patients sensitized to birch pollen, ssIgE testing alone would have missed 18% of sensitizations and SPT alone would have missed 32% of sensitizations compared with combined SPT and ssIgE testing.1 These findings indicate that a combination of SPT and ssIgE testing yields substantially higher positive results than either testing method alone in patients who are sensitized. In agreement with other studies,1,13 serologic sensitization in patients with negative SPT results was more likely in individuals with high total IgE levels.
We found that a relatively large number of negative SPT results (74%) were confirmed as negative by both ssIgE testing and IDST. In 18 patients with completely negative SPT results for all allergens tested, only one additional serologic sensitization was found in one patient, but nine sensitizations were found by IDST. These findings indicated that ssIgE testing rarely revealed additional information for allergens that were already negative by both SPT and IDST or in patients in whom all SPT results were negative. Likewise, in the subgroup of patients with perennial symptoms, no additional serologic sensitizations were depicted when SPT results were negative. In addition, we found that the median ssIgE levels for allergens with negative SPT and negative IDST results were generally low (median, 1.25 kU/L; range, 0.357–4.47 kU/L).
Previous studies done to determine predictive values of clinical allergy showed that low levels of ssIgE are less likely to predict clinical allergy for some allergens, such as cat or Alternaria.12,14 However, for other allergens, such as mouse and dust mite, ssIgE levels have been shown to be highly predictive of clinical allergy, even at very low levels.15,16 Similarly, the predictive values of IDST for clinical allergy (i.e., to produce symptoms after experimental exposure) are largely variable. The positive predictive values generally increase by wheal diameter and decrease with increasing concentrations of testing extracts and vary based on the allergen tested.12,14,15 Although, for dust mite, there is evidence that IDST does not have a good positive predictive value,17 for cat and Alternaria, the IDST positive predictive values for allergic symptoms are high.12,14,15 Therefore, the potential predictive value of clinical allergy has to be considered separately for each allergen.
Compared with ssIgE testing, the highest proportion of additional allergen sensitizations detected through IDST was found for tree pollen (35%). One of the reasons could be differences in the composition of allergens used for skin and serum testing. Such discrepancies are common in daily allergy practice and must carefully be considered when prescribing immunotherapy based on a combination of skin and serum tests. Nevertheless, our study showed that, even for allergens that used highly homologous or identical allergen sources (e.g., ragweed, northern grasses, dust mite, cat, and dog), IDST was more effective in detecting additional allergen sensitization (15–30%) than ssIgE testing (7–26%). The only exception was IDST to mugwort, which did not reveal any additional sensitizations, whereas the ssIgE testing detected a few additional sensitizations compared with SPT alone. Although interpretation of this finding was limited by a relatively smaller sample size for mugwort (n = 24), it was possible that mugwort skin extract was particularly potent and that most sensitizations, therefore, had already been detected by SPT. These results emphasized again the variability of SPT, ssIgE testing, and IDST results, depending on the specific allergen tested, which has to be considered in practice.
Other studies demonstrated that, the higher the concentrations used for IDST, the more likely it is to diagnose sensitizations.2,9,10,12,15 In our retrospective study, we combined the results of patients treated at different hospitals, which used different protocols for IDST. Even though this may be considered a bias or a lack of standardization, different allergen concentrations used for IDST are widely used in the clinical practice: e.g., in case of standardized allergens, the range of starting IDST is reported to be between 10 and 100 BAU,18,19 and most physicians use 100- to 1000-fold dilutions of the concentrated extracts used for SPT19 As such, 163 of 452 of all IDSTs (36%) in this study were done by using protocol 1 (two steps), of which 100 negative results never proceeded to IDST at higher concentrations.
Nevertheless, of the other 96 negative results of IDSTs performed according to protocol 1, 20% revealed positive results at higher IDST concentrations. However, the rate of sensitization depicted through IDSTs based on protocol 2 (one step) was 16.7%, similar to the rate of positive results found when using protocol 1. It is likely that, if all negative results of IDST performed at lower concentrations based on protocol 1 had been done at high concentrations, the discrepancy between the diagnostic yield of ssIgE and IDST would have been even larger than what we described. Even though we used two different methods of detection for ssIgE (Immulite and ImmunoCAP), both tests agreed in distinguishing between negative and positive ssIgE results.13,20,21 Our intention was not to evaluate the performance of these tests against each other or to use data generated by one assay to predict the outcomes with another assay.
Based on the subanalysis of seasonality symptoms of our patients, SPT may be more sensitive in diagnosing environmental allergies to perennial aeroallergens, whereas ssIgE testing performed better for tree and grass pollens. The number of patients included in this subanalysis was small, but there is a trend that SPT performs better in studies in which experimental exposure to indoor allergens is used, especially for mouse, cat, and Alternaria.12,14,15 Similar experimental exposure data regarding true allergic sensitization to pollens is lacking.
CONCLUSION
This study found that, in general, IDST detected an average of 23% additional sensitizations after negative SPT results. Overall, IDST was more than twice as effective in detecting allergic sensitizations than ssIgE testing when the SPT result was negative, and ssIgE added little additional information when both SPT and IDST results were negative. Therefore, it might be prudent to offer IDST to patients with negative SPT results to further detect additional environmental allergen sensitizations when the exposure history is suggestive. The combination of SPT and ssIgE testing seems to be insufficient for diagnosing all environmental sensitizations in patients who are truly sensitized for most allergens but may be useful if IDST cannot be performed.
Footnotes
No funding sources supported research
The authors have no conflicts of interest to declare pertaining to this article
This work is published and licensed by OceanSide Publications, Inc. The full terms of this license are available at https://www.allergyandrhinology.com/terms and incorporate the Creative Commons License Deed: Attribution – Non-Commercial – NoDerivs 4.0 Unported (CC BY-NC-ND 4.0). By accessing the work you hereby accept the terms. Non-commercial uses of the work are permitted without any further permission from OceanSide Publications, Inc., provided the work is properly attributed. Any use of the work other then as authorized under this license or copyright law is prohibited.
REFERENCES
- 1. Calabria CW, Dietrich J, Hagan L. Comparison of serum-specific IgE (ImmunoCAP) and skin-prick test results for 53 inhalant allergens in patients with chronic rhinitis. Allergy Asthma Proc 30:386–396, 2009. [DOI] [PubMed] [Google Scholar]
- 2. Larrabee YC, Reisacher W. Intradermal testing after negative skin prick testing for patients with high suspicion of allergy. Int Forum Allergy Rhinol 5:547–550, 2015. [DOI] [PubMed] [Google Scholar]
- 3. Bernstein IL, Li JT, Bernstein DI, et al. Allergy diagnostic testing: An updated practice parameter. Ann Allergy Asthma Immunol 100(suppl. 3):S1–S148, 2008. [DOI] [PubMed] [Google Scholar]
- 4. Bousquet PJ, Chatzi L, Jarvis D, Burney P. Assessing skin prick tests reliability in ECRHS-I. Allergy 63:341–346, 2008. [DOI] [PubMed] [Google Scholar]
- 5. National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma—Summary Report 2007. J Allergy Clin Immunol 120(suppl.):S94–S138, 2007. [DOI] [PubMed] [Google Scholar]
- 6. Cobbaert CM, Jonker GJ. Allergy testing on the IMMULITE 2000 Random-Access immunoanalyzer—A clinical evaluation study. Clin Chem Lab Med 43:772–781, 2005. [DOI] [PubMed] [Google Scholar]
- 7. Gleeson M, Cripps AW, Hensley MJ, et al. A clinical evaluation in children of the Pharmacia ImmunoCAP system for inhalant allergens. Clin Exp Allergy 26:697–702, 1996. [PubMed] [Google Scholar]
- 8. de Vos G. Skin testing versus serum-specific IgE testing: Which is better for diagnosing aeroallergen sensitization and predicting clinical allergy? Curr Allergy Asthma Rep 14:430, 2014. [DOI] [PubMed] [Google Scholar]
- 9. McKay SP, Meslemani D, Stachler RJ, Krouse JH. Intradermal positivity after negative prick testing for inhalants. Otolaryngol Head Neck Surg 135:232–235, 2006. [DOI] [PubMed] [Google Scholar]
- 10. Wood RA, Phipatanakul W, Hamilton RG, Eggleston PA. A comparison of skin prick tests, intradermal skin tests, and RASTs in the diagnosis of cat allergy. J Allergy Clin Immunol 103(pt. 1):773–779, 1999. [DOI] [PubMed] [Google Scholar]
- 11. Peltier J, Ryan MW. Comparison of intradermal dilutional testing, skin prick testing, and modified quantitative testing for common allergens. Otolaryngol Head Neck Surg 137:246–249, 2007. [DOI] [PubMed] [Google Scholar]
- 12. Fernández C, Bevilacqua E, Fernández N, et al. Asthma related to Alternaria sensitization: An analysis of skin-test and serum-specific IgE efficiency based on the bronchial provocation test. Clin Exp Allergy 41:649–656, 2011. [DOI] [PubMed] [Google Scholar]
- 13. de Vos G, Nazari R, Ferastraoaru D, et al. Discordance between aeroallergen specific serum IgE and skin testing in children younger than 4 years. Ann Allergy Asthma Immunol 110:438–443, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fernandez C, Cardenas R, Martin D, et al. Analysis of skin testing and serum-specific immunoglobulin E to predict airway reactivity to cat allergens. Clin Exp Allergy 37:391–399, 2007. [DOI] [PubMed] [Google Scholar]
- 15. Sharma HP, Wood RA, Bravo AR, Matsui EC. A comparison of skin prick tests, intradermal skin tests, and specific IgE in the diagnosis of mouse allergy. J Allergy Clin Immunol 121:933–939, 2008. [DOI] [PubMed] [Google Scholar]
- 16. King MJ, Tamulis T, Lockey RF. Prick puncture skin tests and serum specific IgE as predictors of nasal challenge response to Dermatophagoides pteronyssinus in older adults. Ann Allergy Asthma Immunol 101:12–17, 2008. [DOI] [PubMed] [Google Scholar]
- 17. Haxel BR, Huppertz T, Boessert P, et al. Correlation of skin test results and specific immunoglobulin E blood levels with nasal provocation testing for house-dust mite allergies. Am J Rhinol Allergy 30:60–64, 2016. [DOI] [PubMed] [Google Scholar]
- 18. Nelson HS, Oppenheimer J, Buchmeier A, et al. An assessment of the role of intradermal skin testing in the diagnosis of clinically relevant allergy to timothy grass. J Allergy Clin Immunol 97:1193–1201, 1996. [DOI] [PubMed] [Google Scholar]
- 19. Niemeijer NR, Goedewaagen B, Kauffman HF, de Monchy JG. Optimization of skin testing. I. Choosing allergen concentrations and cutoff values by factorial design. Allergy 48:491–497, 1993. [DOI] [PubMed] [Google Scholar]
- 20. Bulat Lokas S, Plavec D, Rikić Pišković J, et al. Allergen-specific IgE measurement: Intermethod comparison of two assay systems in diagnosing clinical allergy. J Clin Lab Anal 2016. (Epub ahead of print September 8, 2016.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee YW, Sohn JH, Lee JH, et al. Allergen-specific IgE measurement with the IMMULITE 2000 system: Intermethod comparison of detection performance for allergen-specific IgE antibodies from Korean allergic patients. Clin Chim Acta 401:25–32, 2009. [DOI] [PubMed] [Google Scholar]