Abstract
Background:
Knee pain, is one of the most common causes of patients’ referring to physiatric clinics, and several factors, are involved in its creation. One of these factors is pes anserine bursitis (PAB) for which various treatment methods are used. This study aims to investigate the effect of this method on reducing chronic pain in these patients.
Materials and Methods:
This clinical trial was conducted in 2013- 2014 on patients with PAB referring to academic, physical medicine clinics. The patients with chronic PAB (pain duration more than 3 months), who were refractory to conservative treatments, were randomly divided into two 20-member experimental groups (extracorporeal shock wave therapy [ESWT] and sham ESWT). Pain scores of all patients were measured using the Visual Analog Scale (VAS) and McGill Pain Questionnaire (MPQ) (total and present pain indexes [TPIs and PPIs]) before intervention, immediately after intervention (3rd week), and after 8 weeks. The pain scores were then compared and statistically analyzed.
Results:
In the ESWT group, the mean patient pain score of the VAS and TPI in MPQ were significantly lower than in the sham ESWT group immediately after intervention (3rd week): P =0.02, P = 0.04 respectively; and 8 weeks after the end of treatment: P =0.01, P = 0.000. Moreover, the PPI in both groups had significantly decreased over time, although in ESWT group this decrement was significantly more than sham ESWT group (P < 0.001).
Conclusion:
The results showed that ESWT could be effective in reducing the pain and treating PAB.
Keywords: Extracorporeal shock wave therapy, McGill pain questionnaire, Pes Anserine Bursitis, Visual analog scale
Introduction
Knee pain is one of the most common causes of patients’ referring to physical medicine treatment centers, and several factors are involved in its creation. Different types of bursitis, including ischiogluteal, greater trochanter, pes anserine, prepatellar, popliteal, and retrocalcaneal bursitis are the causes of pain in lower extremities of patients referring to treatment centers. Most of these patients recover spontaneously, by conservative treatments and activity modification.[1] Inflammation of a bursa located below pes anserine tendon (at the junction of semitendinosus, Sartorius, and gracilis muscle tendons with the anteromedial proximal tibia) is called pes anserine bursitis (PAB). In most cases, the occurrence of PAB in patients, cannot be proved;[2,3] so the diagnosis of PAB syndrome is frequently base on clinical features.[4] Ultrasonography can facilitate the diagnosis of PAB.[5,6] However, in most suspected cases ultrasound findings are lacking.[7] In a study, only 2.5% of these patients showed radiologic signs of PAB in magnetic resonance imaging (MRI);[3,8] therefore the diagnosis of PAB cannot be based solely on MRI findings, but it is helpful for ruling out other structural causes of proximal tibial pain such as stress fracture and bone cysts.[9,10] Common biomechanical deficiencies that may occur along with this disease include weakness of core muscles, weakness of medial hamstring muscles, and weakness of hip adductors. Initial treatment includes ice, acetaminophen or nonsteroidal anti-inflammatory drug (NSAID) to reduce inflammation and pain.[2] Furthermore, using short-term knee orthosis is very important to reduce the pain.[8,11,12] Rehabilitation of such patients includes increasing the flexibility, stretching, and endurance of pes anserine muscles; however, the kinetic chain must be considered.[2] Use of phonophoresis and iontophoresis may be suitable for treatment.[13] In cases where conservative treatments fail or when severe pain causes functional limitations, local corticosteroid injection is used.[2,8] There has been recently a strong tendency toward using extracorporeal shock wave therapy (ESWT) in tendon pathologies. The success rate of ESWT in treating epicondylitis, plantar fasciitis, rotator cuff tendinitis, Achilles tendinitis, and jumper's knee is reported to be 60–80%.[14] Because the studies on treating PAB with ESWT are very limited, we decided to investigate the effect of this method on reducing the pain in chronic PAB so that if this method is proved to be effective, we can recommend it as a treatment for PAB.
Materials and Methods
This single-blind randomized, clinical controlled trial was conducted in 2013–2014 on patients with chronic PAB referred to Out Patients Department Clinics of Physical Medicine Department of Isfahan University of Medical Sciences. Patients with a clinical diagnosis of chronic PAB (pain for at least 3 months and point tenderness at the insertion of pes anserine tendon on anteromedial, proximal aspect of tibia), who were refractory to conservative treatments such as ice, acetaminophen, NSAID or physiotherapy were included. The patients were randomly divided into two 20-member experimental groups (ESWT and sham ESWT) after diagnosis by a physical medicine specialist and differentiating from other causes of pain on medial side of knee such as medial collateral ligament injury according to history and clinical examination. Patients with degenerative or non degenerative neurological diseases (change of patient's perception), history of coagulopathy, cancer, cardiac pacemaker, pregnancy, fractures below the knee during the past year, history of corticosteroid injection during the past month, knee effusion, and taking anticoagulants were not included. Considering type I error (alpha) =0.05 and study power = 80%, the sample size was calculated for at least 20 patients in each group. The study protocol was approved by the Ethics Committee of Isfahan University of Medical Sciences, and informed consent was obtained from all patients. First, the mean pain score in each group was measured using the visual analog scale (VAS) and McGill pain questionnaire (MPQ) before the intervention. Then the intervention consisting of one session of ESWT per week (using focus probe, 4 Hz frequency, 1500 pulses and 0.15 mj/mm2 energy per se ssion) that was performed during three consecutive weeks. For the placebo group sham treatment was done where standard contact of focus probe with the skin was provided. The machine makes a noise with every shock wave delivered and, in order to enhance the sham design, minimal energy pulses (0.04 mJ/mm2) were generated. In both groups, the patients could use hot water bags or 400 mg gelofen BID to reduce their pain. They also were trained in hamstring stretching exercises (3 times a day, 3 times each, and each time for 30 s). The patients started exercising since the beginning of the study and continued it up to the end of the study. Pain scores of all patients were again measured using VAS and MPQ (total pain index, present pain index [PPI]) immediately after the intervention (at the end of 3rd week) and after 8 weeks. Using SPSS (version 19.0, SPSS Inc., Chicago, Illinois, USA), the independent t-test, repeated measures analysis of variance (ANOVA), Mann–Whitney tests, and Friedman test, the pain scores of patients were statistically analyzed and compared to the two groups and to each other (in terms of time and intra-group comparison). P < 0.05 was considered as the significance level.
Results
Forty patients (aged 35–65 years) were enrolled in this study and were randomly divided into two groups. The ESWT group consisted of 4 (20%) males and 16 (80%) females with a mean age of 49.4 ± 7.8 years. The sham ESWT group consisted of 5 (25%) males and 15 (75%) females with a mean age of 50.2 ± 8.1 years. There was no significant difference between the mean ages of patients in both groups. Both groups were similar in terms of age (P = 0.738).
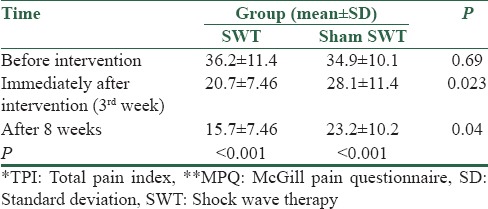
There were no significant differences between both groups in terms of gender distribution (P = 0.705). The intra-group comparisons were performed using repeated measures ANOVA. The results showed a significant difference between the average scores of pain in both groups before, immediately after and 8 weeks after treatment based on VAS and MPQ indices (P < 0.001). The inter-group comparisons showed that there were no significant differences between two groups before intervention based on VAS and MPQ (P = 0.17, P = 0.69, respectively), but the average score of pain immediately after intervention (3rd week), (P = 0.04, P = 0.02, respectively), and 8 weeks after treatment (P = 0.001, P= 0.04) was significantly lower in the ESWT group than that in the sham group. Tables 1 and 2 show the changes.
Table 1.
Mean of VAS* in two groups before and after treatment
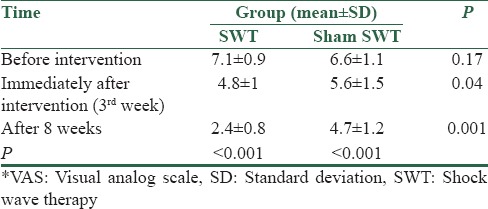
Table 2.
Mean of TPI* (MPQ)** in two groups before and after treatment
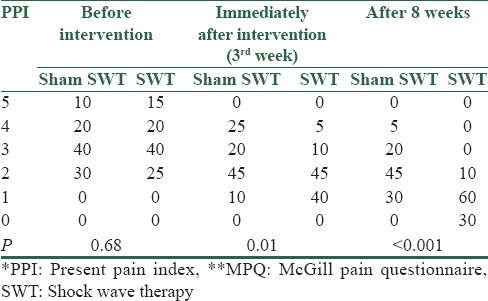
According to the Mann–Whitney test, there were no significant differences between two groups in terms of PPI before the intervention. However, PPI was significantly lower in the ESWT group than the control group [Table 3] immediately (P = 0.01) and 8 weeks after treatment (P = 0.000). Friedman test revealed a significant reduction in PPI in both groups over the time.
Table 3.
PPI* frequency (MPQ)** in both groups before and after treatment
Discussion
Anserine bursitis is one of the causes of knee pain leading to pain and tenderness in anteromedial of the knee. There are various options for the treatment of PAB (rest, ice, NSIAD, physical therapy, injection), but a lot of them are not satisfactory effective, and some of them are associated with risks. For example, glucocorticoid injections can provide temporary pain relief, but care should be taken to avoid injecting any of the three tendons converging at the pes anserinus; injection within the tendons themselves can weaken these structures and intensify the patient's pain.[15] One of the new methods to reduce the tendon injuries is using shock waves. There is a growing tendency to use the ESWT and to determine its mechanism in tendon pathology; which done with electromagnetic stimulation and producing low level energy wave which may be effective on increasing blood flow in the treated area. Nowadays, various procedures are used for treatment that we can point to improving muscles movement by means of decreasing passive muscle tone and increase muscle movement range. Experimental results show that ESWT increases neovascularization along with increased angiogenic growth index in the tendon, bone, and tendon-bone junction. Neovascularization may play an important role in blood circulation improvement and tendon repair. There is a close clinical relationship between decreased substance P concentration and pain treatment in ESWT on the tendon. Moreover, it seems that nitric oxide plays a fundamental role in the molecular mechanism of ESWT. Changes in the concentration of internal mediators support the anti-inflammatory effects of this treatment.[14] According to our results, although the pain intensity in both groups was significantly reduced over the experimental period, the average score of pain in the ESWT group immediately after intervention (3rd week) and 8 weeks after treatment was significantly lower than the Sham group based on VAS and MPQ indices. Other treatment methods such as ice, acetaminophen or massage may have little effect on reducing the pain, and some of them are associated with risks. For example injection within the tendons themselves can weaken these structures and intensify the patient's pain. Moreover; we cannot use NSAIDs in chronic renal failure or glucocorticoid injections in patients with diabetes. Hence, according to other available researches about the efficacy of ESWT on bursitis and tendinitis and also based on our results, we can recommend ESWT as an effective and safe method. The results of a study by Zhao et al. on the treatment of knee osteoarthritis showed that ESWT reduces pain and improves knee function during the 12 weeks of treatment as compared with placebo.[16] In a systematic review, the effects of focus-ESWT and radial pulse therapy on musculoskeletal diseases of the soft tissue have been compared. The results showed that focus-ESWT is an effective in the treatment of plantar fasciitis and calcific tendinitis while radial pulse therapy is an effective in the treatment of plantar fasciitis. It appears that the focus-ESWT is dose-dependent. There is some low-value evidence indicating that low dose focus-ESWT, and radial pulse therapy are ineffective in the treatment of rotator cuff diseases. There are mixed results on the lateral epicondylitis.[17] Furia et al. found that low-energy radial ESWT is effective in the treatment of chronic patellar tendinopathy.[18]
In another study, the impact of ESWT with platelet rich plasma (PRP) injection on the chronic patellar tendinopathy in athletes was investigated. During the 12 months follow-up, both groups showed significant improvement. Although the group that received PRP showed higher improvement at 6 and 12 months, both groups were similar in early follow-up.[19] In a study by Henk et al., the therapeutic effects of focus and radial ESWT in the treatment of patellar tendinopathy were compared. The patients in each group were treated during three sessions (1 session/week). In each group, a specific exercise program (eccentric decline squat training) began 2 weeks after the last treatment session and continued until the end of the study period (12 weeks). No significant differences were observed between the effects of both methods.[20] A placebo-controlled trial of ESWT by Vahdatpour et al., in subjects with chronic plantar fasciitis indicated a superior improvement in the active treatment than the placebo group.[21] In another placebo-controlled trial by Vahdatpour et al., it seems that ESWT have positive effects on treatment, quicker return to daily activities, and quality-of-life improvement on frozen shoulder.[22] Furthermore, a placebo-controlled trial confirmed that ESWT is a safe and effective method in patients with chronic pelvic pain syndrome in short-term.[23]
Regarding PAB, there are very limited studies, and we found only one study published in the literature[24] in which the therapeutic effect of ESWT on PAB in 28 patients was investigated. In that study, shock wave therapy was performed on patients after a local anesthetic with focus probe. The results, 180 days after treatment, were as follows: Excellent (44%), good (38.2%), fair (2.9%), and poor (14.7%). They concluded that, ESWT was found to be a noninvasive and safe treatment for PAB in patients not responding to other conservative treatments. Hence, their findings are as compatible with our results in this research.
Among the limitations of this study, we can point to failure to complete the process of the patients and using several unreported self-treatments by the patients simultaneously.
Conclusions
According to the results of the present study, ESWT could be an effective and safe method of treatment and reducing the pain in chronic anserine bursitis. However, more extensive studies are needed to obtain more reliable results, and confirm whether there is any superiority over other available modalities or not.
Financial support and sponsorship
The Isfahan University of Medical Sciences (Research Project Number 393191).
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study was supported by the Isfahan University of Medical Sciences (Research Project Number 393191). The authors thank to Mr. Akbar Hassanzadeh as a statistician for his consulting and personnel of Kashani Medical Educational Center for their assistance. Authors also appreciate the cooperation of the patients.
References
- 1.Butcher JD, Salzman KL, Lillegard WA. Lower extremity bursitis. Am Fam Physician. 1996;53:2317–24. [PubMed] [Google Scholar]
- 2.Hansen PA, Willick SE. Musculoskeletal disorders of the lower limb. In: Braddom RL, editor. Physical Medicine Rehabilitation & Rehabilitation. 4th ed. Vol. 843. Philadeiphia, PA: Saunders; 2011. p. 59. [Google Scholar]
- 3.Rennie WJ, Saifuddin A. Pes anserine bursitis: Incidence in symptomatic knees and clinical presentation. Skeletal Radiol. 2005;34:395–8. doi: 10.1007/s00256-005-0918-7. [DOI] [PubMed] [Google Scholar]
- 4.Helfenstein M, Jr, Kuromoto J. Anserine syndrome. Rev Bras Reumatol. 2010;50:313–27. [PubMed] [Google Scholar]
- 5.Voorneveld C, Arenson AM, Fam AG. Anserine bursal distention: Diagnosis by ultrasonography and computed tomography. Arthritis Rheum. 1989;32:1335–8. doi: 10.1002/anr.1780321025. [DOI] [PubMed] [Google Scholar]
- 6.Yoon HS, Kim SE, Suh YR, Seo YI, Kim HA. Correlation between ultrasonographic findings and the response to corticosteroid injection in pes anserinus tendinobursitis syndrome in knee osteoarthritis patients. J Korean Med Sci. 2005;20:109–12. doi: 10.3346/jkms.2005.20.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uson J, Aguado P, Bernad M, Mayordomo L, Naredo E, Balsa A, et al. Pes anserinus tendino-bursitis: What are we talking about? Scand J Rheumatol. 2000;29:184–6. doi: 10.1080/030097400750002076. [DOI] [PubMed] [Google Scholar]
- 8.Hanada ED, Keplinger FS, Gupta N. Knee bursitis. In: Forontera WR, Silver JK, Rizzo TD, editors. Essentials of Physical Medicine and Rehabilitation. 7th ed. Philadeiphia, PA: Saunders; 2008. pp. 355–8. [Google Scholar]
- 9.Forbes JR, Helms CA, Janzen DL. Acute pes anserine bursitis: MR imaging. Radiology. 1995;194:525–7. doi: 10.1148/radiology.194.2.7824735. [DOI] [PubMed] [Google Scholar]
- 10.Marra MD, Crema MD, Chung M, Roemer FW, Hunter DJ, Zaim S, et al. MRI features of cystic lesions around the knee. Knee. 2008;15:423–38. doi: 10.1016/j.knee.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Alvarez-Nemegyei J, Canoso JJ. Evidence-based soft tissue rheumatology IV: Anserine bursitis. J Clin Rheumatol. 2004;10:205–6. doi: 10.1097/01.rhu.0000135561.41660.b0. [DOI] [PubMed] [Google Scholar]
- 12.Kang I, Han SW. Anserine bursitis in patients with osteoarthritis of the knee. South Med J. 2000;93:207–9. [PubMed] [Google Scholar]
- 13.Basford J. Physical agents. In: Delisa J, Gans B, editors. Rehabilatien Medicine: Principles and Practice. 3rd ed. Philadelphia: JP Lippincott; 1998. pp. 812–25. [Google Scholar]
- 14.Notarnicola A, Moretti B. The biological effects of extracorporeal shock wave therapy (ESWT) on tendon tissue. Muscles Ligaments Tendons J. 2012;2:33–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Glencross PM, Consuelo TL. Pes Anserine Bursitis Treatment & Management. [Last accessed on 2014 Feb 12]. Available from: http://www.google.com/
- 16.Zhao Z, Jing R, Shi Z, Zhao B, Ai Q, Xing G. Efficacy of extracorporeal shockwave therapy for knee osteoarthritis: A randomized controlled trial. J Surg Res. 2013;185:661–6. doi: 10.1016/j.jss.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Speed C. A systematic review of shockwave therapies in soft tissue conditions: Focusing on the evidence. Br J Sports Med. 2014;48:1538–42. doi: 10.1136/bjsports-2012-091961. [DOI] [PubMed] [Google Scholar]
- 18.Furia JP, Rompe JD, Cacchio A, Del Buono A, Maffulli N. A single application of low-energy radial extracorporeal shock wave therapy is effective for the management of chronic patellar tendinopathy. Knee Surg Sports Traumatol Arthrosc. 2013;21:346–50. doi: 10.1007/s00167-012-2057-8. [DOI] [PubMed] [Google Scholar]
- 19.Smith J, Sellon JL. Comparing PRP injections with ESWT for athletes with chronic patellar tendinopathy. Clin J Sport Med. 2014;24:88–9. doi: 10.1097/JSM.0000000000000063. [DOI] [PubMed] [Google Scholar]
- 20.Henk VD, Johannes Z, Inge VA, Ron LD. The TOPSHOCK Study: Effectiveness of radial shock wave therapy compared to focused shock wave therapy for treating pattelar tendinopath design of a randomized controlled trial. BMC Musculoskelet Disord. 2012;12:229–36. doi: 10.1186/1471-2474-12-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vahdatpour B, Sajadieh S, Bateni V, Karami M, Sajjadieh H. Extracorporeal shock wave therapy in patients with plantar fasciitis. A randomized, placebo-controlled trial with ultrasonographic and subjective outcome assessments. J Res Med Sci. 2012;17:834–8. [PMC free article] [PubMed] [Google Scholar]
- 22.Vahdatpour B, Taheri P, Zade AZ, Moradian S. Efficacy of extracorporeal shockwave therapy in frozen shoulder. Int J Prev Med. 2014;5:875–81. [PMC free article] [PubMed] [Google Scholar]
- 23.Vahdatpour B, Alizadeh F, Moayednia A, Emadi M, Khorami MH, Haghdani S. Efficacy of extracorporeal shock wave therapy for the treatment of chronic pelvic pain syndrome: A randomized, controlled trial. ISRN Urol. 2013;2013:972601. doi: 10.1155/2013/972601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pires PR, Lui M. Effectiveness of Shock Wave Therapy in Patients with Pes Anserine Bursitis. IN: ISMST. 2009. [Last accessed on 2014 Jul 30]. Available from: http://www.Scholar.google.com/


