Abstract
Objective:
Angiographic assessment of stenosis has limited predictive value for functionally significant lesions compared with fractional flow reserve (FFR). The recently developed angiographic DILEMMA score, which consists of minimal lumen diameter (MLD), lesion length (LL) and Bypass Angioplasty Revascularization Investigation (BARI) Myocardial Jeopardy Index (MJI) was found to have diagnostic value in predicting FFR ≤0.80. The present study was an investigation of prediction of FFR ≤0.80 using DILEMMA score and its relationship to resting distal coronary artery pressure/aortic pressure (Pd/Pa).
Methods:
Records of consecutive patients who underwent coronary angiography and FFR were retrospectively analyzed. Assessment of MLD and LL was performed using quantitative coronary angiography. BARI MJI was calculated using angiographic calculation index.
Results:
A total of 185 pressure wire analysis data sets from 150 patients were analyzed retrospectively. There were 82 lesions in FFR >0.80 group and 103 lesions in FFR ≤0.80 group. Negative correlation was found between FFR and DILEMMA score (r=-0.494; p<0.001), FFR and BARI-MJI (r=-0.378; p<0.001), and between FFR and LL (r=-0.314; p<0.001). Positive correlation was found between FFR and baseline Pd/Pa (r=0.713; p<0.001), and between FFR and MLD (r=0.415; p<0.001). DILEMMA score had negative correlation with resting Pd/Pa (r=-0.389; p<0.001). In receiver operating characteristic analysis for diagnosing FFR≤0.80, area under curve values of resting Pd/Pa, DILEMMA score, MLD, BARI-MJI, and LL were 0.862, 0.793, 0.780, 0.728, and 0.686, respectively.
Conclusion:
DILEMMA score had moderately strong correlation with FFR and good accuracy in diagnosing significant FFR, but it had weak correlation with resting Pd/Pa. (Anatol J Cardiol 2017; 17: 285-92)
Keywords: DILEMMA score, fractional flow reserve, pressure wire analyses, resting Pd/Pa
Introduction
Revascularization of ischemia-producing coronary lesions is widely used in management of coronary artery disease (CAD) (1). Invasive coronary angiography (CAG) continues to be the basic method for diagnosing coronary artery stenosis. However, CAG has very limited ability to diagnose lesions responsible for inducing myocardial ischemia, and especially for lesions with intermediate diameter of stenosis (2–4). Fractional flow reserve (FFR) has become standard tool for assessment of functional significance of coronary stenosis severity in the catheterization laboratory (1–4). FFR-guided percutaneous coronary intervention (PCI) has been shown to be related to lower rate of composite endpoints of nonfatal myocardial infarction (MI), repeat revascularization, and death at 1 year, compared with angiography-guided PCI (2). However, utility of FFR before revascularization remains underused (5–7). Dattilo et al. (5) analyzed data of 61,874 attempted coronary interventions of intermediate coronary stenosis from the National Cardiovascular Data Registry CathPCI Registry and demonstrated that FFR was used for 6.1% patients, intravascular ultrasound (IVUS) was used for 20.3% patients, and only angiographic appearance assessment for 73.6% patients. An electronic survey study of 1089 interventionalists revealed that 57% of them used FFR measurement in less than one-third of cases, and 15% never used it (6). In the International Survey on Interventional Strategy, which investigated personal strategies for evaluating angiographically intermediate stenosis in the catheterization laboratory, 495 interventional cardiologists were asked to provide their decision according to angiographic appearance for 4421 lesions evaluated by FFR (7). In 71% of lesions, participants relied on angiographic appearance that was discordant in 47% with known FFR, using 0.80 as cut-off value (7). FFR was requested in only 21% of lesions (7).
Primary reasons for FFR underuse cited in another survey were lack of availability, problems with reimbursement due to high cost, and that it was a time-consuming procedure (6). Apart from operator or patient-related reasons, FFR has limitations in several conditions such as (i) presence of serial stenosis, (ii) FFR in collateral donor artery to artery with chronic total occlusion, (ii) presence of diffuse CAD, (iii) presence of microvascular disease, (iv) presence of elevated right atrial pressure, (v) presence of excellent flow capacity (may lead to reduced FFR across moderate stenosis), and (vi) technical difficulties in presence of inadequate vasodilator response to adenosine (8, 9). In light of these considerations, and because they reduce procedural time and refrain from patient discomfort due to hyperemia, emerging non-hyperemic (adenosine-free) physiological indices such as instantaneous wave-free ratio and ratio of resting (or baseline) distal coronary artery (distal to target lesion) pressure to aortic pressure ratio (Pd/Pa) over entire cardiac cycle have been evaluated with increasing interest (10, 11). Resting Pd/Pa values ≤0.85 were found to have positive predictive value (PPV) of 95% for predicting FFR with cut-off of ≤0.80 (significant FFR), and values ≥0.93 were found to have negative predictive value (NPV) of 96% for predicting significant FFR (11).
Visual estimation by CAG continues to dominate physicians’ treatment decision for intermediate stenosis despite advances in intravascular imaging technology (7). Quantitative coronary angiography (QCA)-derived minimal lumen diameter (MLD) and percent diameter stenosis (DS) have been used to assess lesion significance for a long time (12). However, previous studies reported that QCA-derived MLD had modest diagnostic accuracy for predicting significant FFR (12). More recently, a novel coronary angiography index known as DILEMMA score was developed to predict significant FFR. It combines MLD, lesion length (LL), and Bypass Angioplasty Revascularization Investigation (BARI) Myocardial Jeopardy Index (MJI) (13). DILEMMA score was found to be better predictor of significant FFR compared with MLD, LL, and BARI MJI in patients with intermediate lesions (13). Since then, there has been no reported clinical study in the literature comparing DILEMMA score and FFR in patients with intermediate lesions.
The aim of this study was to test clinical usefulness of DILEMMA score in prediction of significant FFR and its relationship with resting Pd/Pa.
Methods
Study population
We retrospectively examined records of 156 consecutive patients who underwent coronary angiography and FFR assessment at tertiary referral university hospital (Department of Cardiology, Heart Center, Cumhuriyet University, Sivas, Turkey) between January 2008 and December 2012. All patients who had at least 1 target coronary artery with between 50% and 70% angiographic DS on QCA assessment were included in the study. Exclusion criteria included bypass graft lesions, left main stenosis, recent ST-segment elevation myocardial infarction (STEMI), and culprit coronary arteries that collateralized other vessels. According to those criteria, 2 patients with bypass graft lesion FFR assessment, 1 patient with left main lesion FFR assessment, 2 patients with recent STEMI, and 1 patient with culprit coronary artery collateralizing other vessels were excluded. Remaining 150 patients with 185 FFR-assessed lesions were included in the present study. None of the lesions were tandem with another intermediate or severe lesion in same coronary artery. This retrospective study was conducted in accordance with the Helsinki Declaration.
Coronary angiography, QCA analyses, and intracoronary pressure measurements
Invasive coronary angiography was performed using standard techniques with transradial, transbrachial, or transfemoral approach. At least 4 different projection views of left coronary system and at least 2 different projection views of right coronary artery (RCA) were obtained for angiographic assessment (XPER Allura FD10; Philips Medical Systems Nederland B.V, Best, Netherlands). QCA analyses were performed for all visually estimated intermediate coronary artery stenoses. For further assessment, coronary artery lesions with DS of ≥50% and <70% in QCA analyses underwent physiological study using sensor-tipped 0.014-inch guidewire (PressureWire, St. Jude Medical, St. Paul, MN, USA). Pressure wire was advanced through guiding catheter, calibrated, and positioned just distal to stenosis. Resting hemodynamic parameters including heart rate, Pa, and Pd were measured, and resting (or baseline) Pa/Pd was calculated. After recording resting hemodynamic parameters, intracoronary adenosine bolus starting at a dose of 40 µg for the RCA and 40–80 µg for the left coronary artery system was administered. An incremental dose approach (up to maximum dose of 210 µg) was applied in patients with FFR ≥0.75 to achieve maximum hyperemia (14). FFR was calculated as ratio of mean Pd measured with pressure wire divided by mean Pa measured with guiding catheter during maximal hyperemia. Coronary stenosis with FFR value ≤0.80 was considered functionally significant (2).
DILEMMA score calculation
DILEMMA score, which has been described in detail elsewhere (11), was calculated using 3 parameters: QCA-derived MLD, QCA-derived LL, and BARI MJI. QCA-derived MLD is classified into 3 groups: (i) <1.1 mm receives score of 4 points, (ii) 1.1–1.5 mm receives score of 1, and (iii) >1.5 mm receives score of 0. QCA-derived LL is also classified into 3 groups: (i) >18 mm is awarded 3 points, (ii) 9–18 mm receives score of 1, and (iii) <9 mm is scores 0. BARI MJI is classified into 3 groups as well: (i) >35% receives a score of 5, (ii) 18–35% receives score of 1 point, and (iii) <18% receives score of 0. DILEMMA score of lesion was calculated as sum of scores obtained from these 3 parameters. Calculated DILEMMA score is between 0 and 12 (Fig. 1).
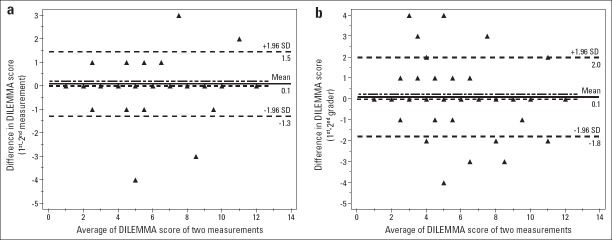
Figure 1.
Representative example of intermediate stenosis in the left anterior descending artery with a DILEMMA score of 6, a resting Pd/Pa of 0.94 and a FFR of 0.87. (a) BARI MJI score of 3 was assigned to the right posterior descending artery, and 3 in the right posterior lateral artery with a side branch; (b) BARI MJI score of 3 in the left anterior descending artery, and 2 in the second diagonal artery; (c) BARI MJI score of 4 was assigned to the left circumflex artery with a side branch, 2 in the second obtuse marginal artery, 2 in the first obtuse marginal artery, 2 in the second septal artery, and 1 in the third septal artery. MLD and LL were derived from QCA; (d) Calculation of DILEMMA score and BARI MJI
BARI - bypass angioplasty revascularization investigation; FFR - fractional flow reserve; LL - lesion length; LV - left ventricle; MJI - myocardial jeopardy index; MLD - minimal lumen diameter; Pd/Pa - distal coronary artery pressure/aortic pressure; QCA - quantitative coronary angiography.
BARI MJI was calculated using methods as initially described from left ventricular (LV) myocardium at risk (LV myocardium jeopardized by lesion), depending on size and location (15–17). According to BARI MJI, percentage of LV myocardium jeopardized by lesion was based on extent of distribution of the 3 main coronary arteries and all major branches (15–17). Native coronary artery distribution was based on observer grading of distal terminating arteries (the ramus intermedius, 0–3 diagonal branches, 0–3 obtuse marginal branches, sub-branches for each of these, 0 to 3 septal arteries, posterior-lateral artery, posterior descending, as well as distal terminal portion of left anterior descending artery, left circumflex artery, and RCA), limited to those approximately ≥1.5 mm in diameter (15–17). This system assigns numerical LV score corresponding to relative size of all of these terminal arteries (15–17). This LV score reflects size of LV territory supplied by each vessel and is based on ratio of length of terminating artery to LV base to apex distance (and to a lesser extent circumferential spread of smaller branches). Numerical LV score for each terminating artery was assigned based on LV distribution: (i) ratio <1/5 receives value of 0, (ii) ratio 1/5 to 1/3 receives value of 1, (iii) ratio 1/3 to 2/3 receives value of 3. Right ventricular marginal and posterior descending artery septal branches were not included in this index. Total score of septal branches is maximum of 3. Overall score of all arteries supplying LV (overall LV score) is calculated by adding together LV score of each terminal artery. Final BARI MJI was obtained by dividing sum of scores of terminal arteries subtended distal to lesion by overall LV score, which finally permits estimation of percentage of myocardium at risk (Fig. 1) (15–17).
Intraobserver and interobserver variability
Two experienced cardiologists (first grader [HK] and second grader [OOT]), who were blinded to baseline Pd/Pa and FFR values, measured DILEMMA score of 185 lesions. In addition, first grader repeated DILEMMA score calculation of 185 lesions 5 weeks after initial measurement in order to assess intragrader variability.
Statistical analyses
Variables were examined using analytical method (one-sample Kolmogorov-Smirnov test) to determine whether or not they were normally distributed. Continuous variables were expressed as mean±standard deviation, or median (interquartile range, 25th–75th percentile) in presence of abnormal distribution, and categorical variables were provided as percentages. Comparisons between groups of patients were made with chi-square test for categorical variables, independent samples t-test for normally distributed continuous variables, and Mann-Whitney U test when distribution was skewed. While investigating associations between normally distributed variables, correlation coefficients and their significance were calculated using Pearson test. In case of non-normally distributed variables and/or ordinal variables, correlation coefficients and their significance were calculated using Spearman test. Receiver operating characteristic (ROC) curve analysis was used to compare diagnostic performance (sensitivity and specificity) of resting Pd/Pa, DILEMMA score, MLD, BARI-MJI, and LL.
Intragrader and intergrader variability and agreement for assessing DILEMMA score were evaluated using absolute agreement model of intraclass correlation coefficient (ICC) and Bland-Altman plot analyses (18–20). ICC values between 0.81 and 1.00 indicated almost perfect agreement, values between 0.61 and 0.80 signified good agreement, values between 0.41 and 0.60 denoted moderate agreement, values between 0.21 and 0.40 indicated poor agreement, and values less than 0.20 indicated poor agreement (18–20). In Bland-Altman plot analyses, 95% limits of agreement (LOA) were defined as mean difference±1.96 x standard deviation. In Bland-Altman plots, difference between 2 measurements was plotted against average of 2 measurements. Mean difference value was compared with 0 value of difference using one-sample test to investigate presence of any systemic (fixed) bias. Diagnostic accuracy, PPV, and NPV of resting Pd/Pa, DILEMMA score, and MLD for predicting FFR≤0.80 were calculated using Bayesian analysis model. Statistical procedures were performed using SPSS software, version 16.0 (SPSS Inc., Chicago, IL, USA) and MedCalc for Windows, version 9.5.1.0 (MedCalc Software, Mariakerke, Belgium; personal license of MBY). P value of 0.05 was considered statistically significant.
Results
Patient demographics and angiographic characteristics of lesions
A total of 185 pressure wire data sets from 150 patients were analyzed retrospectively. Baseline characteristics of study population are provided in Table 1. Mean age was 59±9 years and 116 (77.3%) patients were male. Seventy-one patients (47.3%) had diabetes mellitus, 92 (61.3%) patients had hypertension, 81 (54.0%) patients had dyslipidemia, and 68 (45.3%) patients were active, current smokers. Patients had undergone CAG with indications for stable angina (68.7%), unstable angina (16.0%), non-STEMI (4.0%), and for other reasons (11.3%) including structural heart disease, atypical chest pain, and silent ischemia.
Table 1.
Baseline characteristics of study population (n=150)
| Age, years | 59±9 |
| Male, n (%) | 116 (77.3) |
| Diabetes mellitus, n (%) | 71 (47.3) |
| Hypertension, n (%) | 92 (61.3) |
| Active smoker, n (%) | 68 (45.3) |
| Dyslipidemia, n (%) | 81 (54.0) |
| Obesity, n (%) | 42 (28.0) |
| Family history, n (%) | 38 (25.3) |
| Previous MI-remote area, n (%) | 35 (23.3) |
| Previous ACS, n (%) | 48 (32.0) |
| Previous PCI, n (%) | 58 (38.7) |
| Previous CABG, n (%) | 18 (12.0) |
| Acetylsalicylic acid, n (%) | 123 (82.0) |
| Clopidogrel, n (%) | 104 (69.3) |
| Beta-blockers, n (%) | 107 (71.3) |
| RAAS antagonist, n (%) | 115 (76.7) |
| CaCB, n (%) | 21 (14.0) |
| Statins, n (%) | 77 (51.3) |
| Nitrates, n (%) | 13 (8.7) |
| Current CAG indications | |
| Stable angina pectoris, n (%) | 103 (68.7) |
| Unstable angina pectoris, n (%) | 24 (16.0) |
| NSTEMI, n (%) | 6 (4.0) |
| Other reasons, n (%) | 17 (11.3) |
ACS - acute coronary syndrome; CABG - coronary artery by-pass grafting; CaCB - calcium-channel blockers; CAG - coronary angiography; CMI - myocardial infraction; NSTEMI - non-ST-elevation acute myocardial infarction; PCI - percutaneous coronary intervention; RAAS - renin-angiotensin-aldosterone system
Characteristics of FFR-assessed lesions are presented in Table 2. There were 82 lesions in FFR >0.80 group and 103 lesions in FFR ≤0.80 group. Distribution of lesions according to coronary arteries and their locations were similar between FFR ≤0.80 and FFR >0.80 groups. Median value of LL was higher in FFR ≤80 group compared with FFR >0.80 group (14 mm vs. 10 mm, respectively; p<0.001). Median value of MLD was lower in FFR ≤0.80 group compared with >0.80 group (1.45 mm vs. 1.49 mm; p=0.005). BARI-MJI was statistically higher in FFR ≤0.80 group compared with FFR >0.80 group (36 vs. 30; p<0.001). FFR ≤0.80 group had higher DILEMMA score compared with FFR >0.80 group (7 vs. 4; p<0.001). Median value of baseline Pd/Pa was 0.87 in FFR ≤0.80 group and 0.93 in FFR >0.80 group (p<0.001).
Table 2.
Characteristics of FFR-assessed lesions
| Variables | All lesions (n=185) | FFR >0.8 (n=82) | FFR ≤0.8 (n=103) | P |
|---|---|---|---|---|
| Lesion location | ||||
| LAD, n (%) | 125 (67.6) | 52 (63.4) | 73 (70.9) | 0.282 |
| LCX, n (%) | 32 (17.3) | 17 (20.7) | 15 (14.6) | 0.365 |
| RCA, n (%) | 23 (12.4) | 10 (12.2) | 13 (12.6) | 1.0 |
| Other (diagonal, OM, PDA), n (%) | 5 (2.7) | 3 (3.7) | 2 (1.9) | 0.657 |
| Lesion location in coronary arteries | ||||
| Proximal, n (%) | 84 (45.4) | 32 (39.0) | 52 (50.5) | 0.120 |
| Mid, n (%) | 94 (50.8) | 45 (54.9) | 49 (47.6) | 0.323 |
| Distal, n (%) | 7 (3.8) | 5 (6.1) | 2 (1.9) | 0.244 |
| QCA analysis | ||||
| Percent diameter stenosis, % | 54.4±4.1 | 53.7±4.0 | 54.9±4.1 | 0.053 |
| MLD, mm | 1.49 (1.09–1.49) | 1.45 (1.01–1.55) | 1.49 (1.09–1.49) | 0.005 |
| MLD <1.1 mm, n (%) | 35 (18.9) | 11 (13.4) | 24 (23.3) | 0.088 |
| MLD 1.1–1.5 mm, n (%) | 107 (57.8) | 30 (36.6) | 77 (74.8) | <0.001 |
| MLD >1.5 mm, n (%) | 43 (23.2) | 41 (50.0) | 2 (1.9) | <0.001 |
| LL, mm | 14 (9–19) | 10 (8–15) | 14 (11–20) | <0.001 |
| LL >18 mm, n (%) | 53 (28.6) | 15 (18.3) | 38 (36.9) | 0.005 |
| LL 9–18 mm, n (%) | 89 (48.1) | 33 (40.2) | 56 (54.4) | 0.056 |
| LL <9 mm, n (%) | 43 (23.2) | 34 (41.5) | 9 (8.7) | <0.001 |
| BARI MJI, % | 34.0 (25.5–38.0) | 30.0 (20.0–37.0) | 36.0 (30.0–38.0) | <0.001 |
| BARI MJI >35%, n (%) | 88 (47.6) | 24 (29.3) | 64 (62.1) | <0.001 |
| BARI MJI 18–35%, n (%) | 94 (50.8) | 56 (68.3) | 38 (36.9) | <0.001 |
| BARI MJI <18%, n (%) | 3 (1.6) | 2 (2.4) | 1 (1.0) | 0.585 |
| DILEMMA score | 5 (3–7) | 4 (2–5) | 7 (4–12) | <0.001 |
| DILEMMA score ≥9, n (%) | 42 (22.7) | 5 (6.1) | 37 (35.9) | <0.001 |
| DILEMMA score 3–8, n (%) | 107 (57.8) | 44 (53.7) | 63 (61.2) | 0.304 |
| DILEMMA score ≤2, n (%) | 36 (19.5) | 33 (40.2) | 3 (2.9) | <0.001 |
| Pressure analyses | ||||
| Resting Pd/Pa | 0.90 (0.87–0.94) | 0.93 (0.91–0.95) | 0.87 (0.85–0.90) | <0.001 |
BARI - bypass angioplasty revascularization investigation; FFR - fractional flow reserve; LAD - left anterior descending artery; LCX - left circumflex artery; LL - lesion length; MJI - myocardial jeopardy index; MLD - minimal lumen diameter; OM - obtuse marginal artery; PDA - posterior descending artery; Pd/Pa - distal coronary artery pressure/aortic pressure; QCA - quantitative coronary angiography; RCA - right coronary artery. Results were expressed as mean±standard deviation or median (interquartile range, 25th-75th percentile) in presence of abnormal distribution, and categorical variables as percentages. Comparisons were made using chi-square test for categorical variables, independent samples t-test for normally distributed variables, and Mann-Whitney U test for continuous variables not normally distributed
Relationship between pressure-derived and QCA-derived parameters
Range of resting Pd/Pa values was 0.81 to 1.0, and range of FFR values was 0.55 to 0.94. Correlation analyses of FFR are presented in Table 3. A positive correlation was found between FFR and resting Pd/Pa (r=0.713; p<0.001), and between FFR and MLD (r=0.415; p<0.001). Negative correlation was demonstrated between FFR and DILEMMA score (r=-0.494; p<0.001), between FFR and BARI-MJI (r=-0.378; p<0.001), and between FFR and LL (r=-0.314; p<0.001). Relationship was poor between FFR and DS (r=-0.102; p=0.058) (Table 3). DILEMMA score had negative correlation with resting Pd/Pa (r=-0.389; p<0.001).
Table 3.
Correlation coefficients for FFR
| Correlation coefficients | P | |
|---|---|---|
| Resting Pd/Pa | 0.713 | <0.001 |
| DILEMMA score | -0.494 | <0.001 |
| MLD, mm | 0.415 | <0.001 |
| BARI MJI, % | -0.378 | <0.001 |
| LL, mm | -0.314 | <0.001 |
| DS, % | -0.102 | 0.058 |
BARI - bypass angioplasty revascularization investigation; DS - percent diameter stenosis; FFR - fractional flow reserve; LL - lesion length; MJI - myocardial jeopardy index; MLD - minimal lumen diameter; Pd/Pa - distal coronary artery pressure/aortic pressure. Correlation coefficients and significance were calculated using Pearson test for normally distributed variables, and Spearman test for non-normally distributed variables and/or ordinal variables
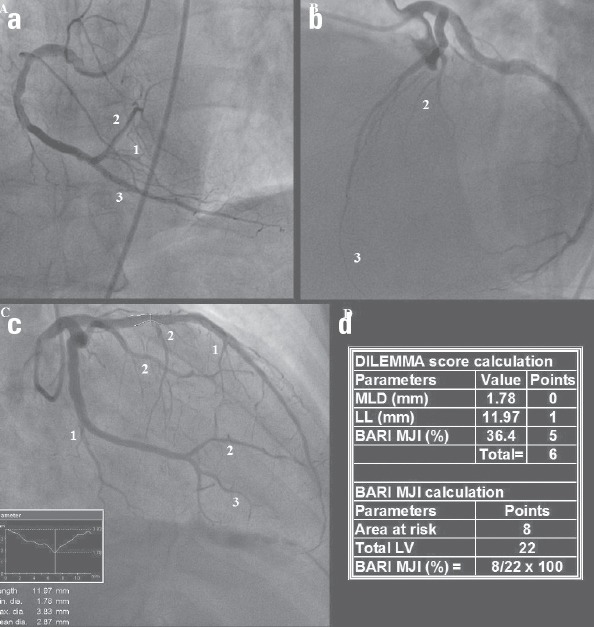
Comparison of ROC curves of resting Pd/Pa, DILEMMA score, MLD, BARI-MJI, and LL for diagnosing FFR ≤0.80 is presented in Figure 2. Area under curve (AUC) values were 0.862 (95% CI: 0.804–0.908; p<0.001) for resting Pd/Pa, 0.793 (95%CI: 0.727–0.849; p<0.001) for DILEMMA score, 0.780 (95% CI: 0.713–0.837; p<0.001) for MLD, 0.728 (95% CI: 0.658–0.791; p<0.001 for BARI-MJI, and 0.686 (95%CI: 0.614–0.753; p<0.001) for LL.
Figure 2.
Receiver operator characteristic curve. Resting Pd/Pa (AUC=0.862, 95% CI: 0.804–0.908, P<0.001), DILEMMA score (AUC=0.793, 95% CI: 0.727–0.849, P<0.001), MLD (AUC=0.780, 95% CI: 0.713–0.837, P<0.001), BARI-MJI (AUC=0.728, 95% CI: 0.658–0.791, P<0.001), and LL (AUC=0.686, 95% CI:0.614–0.753, P<0.001)
Resting Pd/Pa ≤0.90, DILEMMA score >6, and MLD ≤1.3 mm were associated with diagnostic accuracies of 81.6%, 75.3%, and 72.4% for predicting FFR≤0.80, respectively. Resting Pd/Pa of ≤0.85 was associated with ≥98% specificity and 97% PPV for predicting FFR ≤0.80, whereas a resting Pd/Pa of ≥0.95 was associated with sensitivity of ≥99% and NPV of 94%. DILEMMA score ≥9 was associated with 100% specificity and 100% PPV for predicting FFR ≤0.80, while DILEMMA score ≤2 was associated with sensitivity of ≥97% and NPV of 91%. MLD ≤0.8 mm was associated with ≥98% specificity and 97% PPV for predicting FFR ≤0.80, whereas MLD of ≥1.3 mm was associated with sensitivity of ≥98% and NPV of 95%.
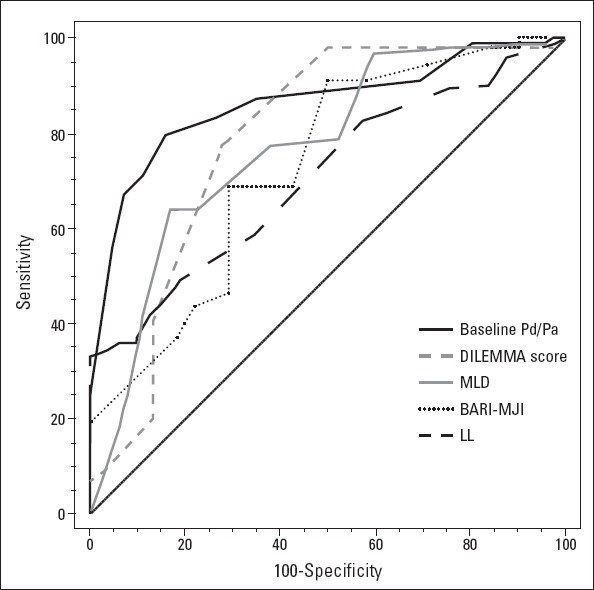
Intragrader measurements of DILEMMA score revealed ICC value of 0.98 which indicates almost perfect agreement (Table 4). Bland-Altman plot analyses for DILEMMA score intragrader variability are provided in Figure 3a, which shows 95% LOA of -1.29 to 1.45 with mean difference of 0.08. Intergrader measurements of DILEMMA score had ICC value of 0.97 which denotes almost perfect agreement (Table 4). Bland-Altman plot analyses for DILEMMA score intergrader variability are provided in Figure 3b, which shows 95% LOA of -0.96 to 2.80 with mean difference of 0.92.
Table 4.
Intra- and intergrader variability analyses of DILEMMA score
| ICC (95% CI) | Mean difference | Bland-Altman 95% LOA | P* | |
|---|---|---|---|---|
| Intra-grader** | 0.98 (0.98–0.99) | 0.08 | -1.29,1.45 | 0.116 |
| Inter-grader*** | 0.97 (0.97–0.98) | 0.92 | -0.96,2.80 | 0.194 |
P value of one-sample t-test (comparing between mean difference and zero value) to indicate presence of systemic bias.
Mean difference was determined from 1st time measurement minus 2nd time measurement.
Mean difference was determined from 1st grader measurement minus 2nd grader measurement. CI - confidence interval; ICC - intraclass correlation coefficient; LOA - limits of agreement. Intragrader and intergrader variability and agreement were evaluated using absolute agreement model of ICC and Bland–Altman plot analyses
Figure 3.
Bland- Altman plots of intragrader (a) and intergrader (b) measurements of lesions
AUC - area under curve; BARI - bypass angioplasty revascularization investigation; CI - confidence interval; MJI - myocardial jeopardy index; MLD - minimal lumen diameter; LL - lesion length; Pd/Pa distal coronary artery pressure/aortic pressure.
Discussion
The present study demonstrated that there is a strong correlation between pressure-derived resting Pd/Pa and FFR, and a moderately strong correlation between QCA-derived DILEMMA score and FFR. DILEMMA score was weakly correlated with resting Pd/Pa. ROC curve analyses indicated that resting Pd/Pa has very good accuracy as diagnostic test in predicting FFR ≤0.80, whereas QCA-derived DILEMMA score and MLD have good accuracy. When a hybrid approach was used to improve diagnostic accuracy, resting Pd/Pa of ≤0.85 had PPV of ≥97% in predicting FFR ≤0.80, and resting Pd/Pa of ≥0.95 had ≥94% NPV. DILEMMA score ≥9 had 100% PPV in predicting FFR≤0.80, and DILEMMA score ≤2 had ≥91% NPV.
In the DEFER trial, QCA-derived DS results were found to be no different from both PCI and medical therapy groups over the full range of stenosis encountered (30–70%) (21). Similar findings were demonstrated in recent meta-analyses reporting that QCA-derived DS only accounted for 31% variance in FFR (22). Although it is clear that FFR assessment of coronary artery stenosis severity results in improved clinical outcomes in comparison with that of decision-making based on angiographic severity of disease (8, 22), FFR-guided revascularization is still only used in 6–7% of all PCI procedures (5). Consistent with these studies, we found very poor relationship between FFR and DS.
Mamas et al. (11) found significant linear correlation (r=0.74; p<0.001) between resting Pd/Pa and FFR in 483 patients. They used hybrid approach in order to improve accuracy of resting Pd/Pa in predicting FFR ≤0.80 (11). According to this approach, when resting Pd/Pa was ≤0.85, PPV was 95%, and when resting Pd/Pa was ≥0.93, NPV was 96% (11). Also, 66% of their cohort had ≤0.85 or ≥0.93 resting Pd/Pa values, which means that FFR with adenosine would only be necessary in 34% lesions (11). The RESOLVE study demonstrated that resting Pd/Pa ≤0.92 has 76.3% sensitivity, 88.1% specificity, 89.2% PPV, 74.4% NPV, and 81.5% overall diagnostic accuracy for FFR≤0.80 (AUC=0.82; 95% confidence interval: 0.80–0.84) (10). Park et al. (23) reported that resting Pd/Pa cut-off of 0.91 had diagnostic accuracy of 82% (AUC=0.9) for FFR ≤0.80. In the present study, we found similar degree of correlation between resting Pd/Pa and FFR. In addition, comparable results were found when we proposed hybrid approach to predict FFR ≤0.80, as in study of Mamas et al. (11) Also, similar to results reported by Mamas et al. (11), 58.7% of our cohort had ≤0.85 or ≥0.95 resting Pd/Pa, indicating that FFR would be needed in 41.3% lesions.
QCA has several advantages over physiological imaging technologies such as being non-invasive, time- and money-saving, simple (utilization and interpretation), and not causing increment in radiation dose exposure, QCA-derived anatomical parameters have modest diagnostic accuracy for FFR ≤0.80 (12). It is well known that QCA-derived anatomical parameters such as MLD, DS, and LL, influence physiological significance of coronary lesions (24). Park et al. (12) reported weak correlation (r=0.414) between QCA-derived MLD and FFR, which was similar to our findings (r=0.415). Brosh et al. (25) demonstrated weak inverse correlation (r=-0.31) between QCA-derived LL and FFR, which was also comparable to present study. Three well-known known myocardial jeopardy scores (MJS): the Duke Jeopardy Score, BARI MJI, and the Alberta Provincial Project of Outcome Assessment in Coronary Heart Disease (APPROACH) score, were compared in a cohort of 20,067 patients and each was found to be predictive of 1-year mortality in patients treated with PCI or medically (26). Shiono et al. (27) reported that FFR is correlated with MLD (r=0.584), DS (r=-0.565), LL (r=-0.306), and modified APPROACH MJS (r=-0.504). In our study, we found weak correlation between FFR and BARI MJI.
More recently, Wong et al. (13) developed a simple technique called DILEMMA scoring system and used it in a derivation cohort consisting of 196 patients. It was then tested on validation cohort of 100 patients. Derivation cohort findings were similar to validation cohort results (13). In validation cohort, c-statistic of DILEMMA score, MLD, LL, and BARI MJI in predicting FFR ≤0.80 was 0.88, 0.72, 0.81, and 0.77, respectively (13). They demonstrated that AUC values of DILEMMA score, BARI MJI, MLD, and LL were 0.88, 0.77, 0.77, and 0.81, respectively for FFR ≤0.80 in validation cohort (13). In both derivation and validation cohorts, they found that DILEMMA score of ≤2 was associated with >95% sensitivity of FFR >0.8, and DILEMMA score of ≥9 was associated with specificity of >95% (13). It was underlined that 51% of lesions had DILEMMA scores of ≤2 or ≥9 in validation cohort (13). In our study, 42.2% (n=76) of lesions had DILEMMA scores of ≤2 or ≥9.
Pathophysiological relationship between DILEMMA score and FFR hypothetically depends on the Hagen-Poiseuille law of fluid dynamics. According to Poiseuille’s law, pressure gradient is influenced by coronary blood flow and viscosity, minimum radius, and LL (28). Pressure drop across epicardial coronary arteries is affected not only by stenosis, but also by coronary blood flow volume (CBFV) (29). Therefore, FFR value is influenced by both epicardial artery resistance and CBFV through stenosis. As CBFV increases, pressure gradient across stenosis also increases (30). Amount of CBFV correlates with volume of regional myocardial mass supplied by coronary artery (31), which may explain the relationship between FFR and BARI MJI. Epicardial artery resistance also provides insight: resistance is affected by blood viscosity, minimum radius (MLD), and LL (28). According to Poiseuille’s law, gradient across coronary stenosis is inversely proportional to fourth power of lesion radius (r4) and is proportional to LL (28). Consequently, DILEMMA score may represent nearly all determinants of the pressure gradient, including coronary blood flow (estimated by BARI MJI), minimum radius (estimated by QCA-derived MLD), and LL (estimated by QCA-derived LL).
Proposed hybrid approach of applying derived DILEMMA scores of ≤2 and ≥9 may help extract clinical implications from our results and lead to savings of both time and costs. FFR could potentially have been deferred in 42.2% (n=78) lesions that had DILEMMA scores of ≤2 or ≥9. Furthermore, when derived resting Pd/Pa values of ≤0.85 and ≥0.95 were applied to remaining 57.8% (n=107) of lesions as a second step, this could have led to deferral of adenosine application in 36 remaining lesions. Consequently, FFR with adenosine would only have been necessary in the remaining 71 (38.4%) lesions. This stepwise approach may save time and expense, but further clinical trials (especially trials testing clinical outcomes) are needed to test DILEMMA score before clinical application.
Study limitations
Several limitations of this study should be acknowledged. First, it was a retrospective analysis, which is susceptible to bias in data selection. Second, it was a single-center study, and volume at the center where present study was conducted was not enough to draw definitive conclusions. Third, we included patients with intermediate coronary stenosis on QCA and FFR measurement. Lesions with ≥50% to <70% DS were included in the present study. Lesion selection for FFR represents our institutional clinical practice, and may not represent clinical practice of other institutions. Fourth, we did not use 3-D angiography, intravascular ultrasound, or optic coherence tomography, which can provide more accurate morphology of coronary arteries in comparison with QCA. Fifth, BARI MJI does not include right ventricle territory. Myocardial supply area of RCA might be underestimated. Consequently, large-scale, randomized, prospective trials are needed to confirm diagnostic accuracy of DILEMMA score and test its clinical significance.
Conclusion
Angiographically derived DILEMMA score had moderately strong correlation with FFR and good accuracy in diagnosing significant FFR, but it had weak correlation with resting Pd/Pa. DILEMMA score would have been useful for deferring FFR in 42.2% lesions that had DILEMMA scores of ≤2 or ≥9. DILEMMA score may lead to savings of time and costs by preventing unnecessary FFR assessment.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept – O.B., H.K., O.O.T., M.B.Y.; Design – O.B., H.K., M.B.Y.; Supervision – O.B., H.K., O.O.T., M.B.Y.; Funding – O.B., H.K., O.O.T., M.B.Y.; Data collection &/or processing – O.B., H.K., O.O.T., M.B.Y.; Analysis and/or interpretation – O.B., H.K., O.O.T., M.B.Y.; Literature review – O.B., H.K., O.O.T., M.B.Y.; Writing – O.B.; Critical review – O.B., H.K., O.O.T., M.B.Y.
References
- 1.Fearon WF. Invasive coronary physiology for assessing intermediate lesions. Circ Cardiovasc Interv. 2015;8:e001942. doi: 10.1161/CIRCINTERVENTIONS.114.001942. [DOI] [PubMed] [Google Scholar]
- 2.Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van't Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–24. doi: 10.1056/NEJMoa0807611. [DOI] [PubMed] [Google Scholar]
- 3.Tonino PA, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816–21. doi: 10.1016/j.jacc.2009.11.096. [DOI] [PubMed] [Google Scholar]
- 4.Gould KL, Johnson NP, Bateman TM, Beanlands RS, Bengel FM, Bober R, et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol. 2013;62:1639–53. doi: 10.1016/j.jacc.2013.07.076. [DOI] [PubMed] [Google Scholar]
- 5.Dattilo PB, Prasad A, Honeycutt E, Wang TY, Messenger JC. Contemporary patterns of fractional flow reserve and intravascular ultrasound use among patients undergoing percutaneous coronary intervention in the United States: insights from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2012;60:2337–9. doi: 10.1016/j.jacc.2012.08.990. [DOI] [PubMed] [Google Scholar]
- 6.Hannawi B, Lam WW, Wang S, Younis GA. Current use of fractional flow reserve: a nationwide survey. Tex Heart Inst J. 2014;41:579–84. doi: 10.14503/THIJ-13-3917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toth GG, Toth B, Johnson NP, De Vroey F, Di Serafino L, Pyxaras S, et al. Revascularization decisions in patients with stable angina and intermediate lesions: results of the international survey on interventional strategy. Circ Cardiovasc Interv. 2014;7:751–9. doi: 10.1161/CIRCINTERVENTIONS.114.001608. [DOI] [PubMed] [Google Scholar]
- 8.Gewirtz H. Functional versus anatomic imaging of CAD: lessons learned from recent clinical trials. Curr Cardiol Rep. 2016;18:4. doi: 10.1007/s11886-015-0686-5. [DOI] [PubMed] [Google Scholar]
- 9.Motwani M, Motlagh M, Gupta A, Berman DS, Slomka PJ. Reasons and implications of agreements and disagreements between coronary flow reserve, fractional flow reserve, and myocardial perfusion imaging. J Nucl Cardiol. 2015 Dec 29; doi: 10.1007/s12350-015-0375-1. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 10.Jeremias A, Maehara A, Généreux P, Asrress KN, Berry C, De Bruyne B, et al. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting Pd/Pa with fractional flow reserve: the RESOLVE study. J Am Coll Cardiol. 2014;63:1253–61. doi: 10.1016/j.jacc.2013.09.060. [DOI] [PubMed] [Google Scholar]
- 11.Mamas MA, Horner S, Welch E, Ashworth A, Millington S, Fraser D, et al. Resting Pd/Pa measured with intracoronary pressure wire strongly predicts fractional flow reserve. J Invasive Cardiol. 2010;22:260–5. [PubMed] [Google Scholar]
- 12.Park SJ, Kang SJ, Ahn JM, Shim EB, Kim YT, Yun SC, et al. Visual-functional mismatch between coronary angiography and fractional flow reserve. JACC Cardiovasc Interv. 2012;5:1029–36. doi: 10.1016/j.jcin.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 13.Wong DT, Narayan O, Ko BS, Leong DP, Seneviratne S, Potter EL, et al. A novel coronary angiography index (DILEMMA score) for prediction of functionally significant coronary artery stenoses assessed by fractional flow reserve: A novel coronary angiography index. Am Heart J. 2015;169:564–71. doi: 10.1016/j.ahj.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 14.Lopez-Palop R, Saura D, Pinar E, Lozano I, Perez-Lorente F, Pico F, et al. Adequate intracoronary adenosine doses to achieve maximum hyperaemia in coronary functional studies by pressure derived fractional flow reserve: a dose response study. Heart. 2004;90:95–6. doi: 10.1136/heart.90.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alderman EL, Stadius MD. The angiographie definitions of the Bypass Angioplasty Revascularization Investigation. Coron Artery Dis. 1992;3:1189–207. [Google Scholar]
- 16.Alderman EL, Kip KE, Whitlow PL, Bashore T, Fortin D, Bourassa MG, et al. Native coronary disease progression exceeds failed revascularization as cause of angina after five years in the Bypass Angioplasty Revascularization Investigation (BARI) J Am Coll Cardiol. 2004;44:766–74. doi: 10.1016/j.jacc.2004.05.041. [DOI] [PubMed] [Google Scholar]
- 17.Moral S, Rodríguez-Palomares JF, Descalzo M, Martí G, Pineda V, Otaegui I, et al. Quantification of myocardial area at risk: validation of coronary angiographic scores with cardiovascular magnetic resonance methods. Rev Esp Cardiol. 2012;65:1010–7. doi: 10.1016/j.recesp.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 18.Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas. 1973;33:613–9. [Google Scholar]
- 19.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 20.Bland JM, Altman DG. Agreed statistics: measurement method comparison. Anesthesiology. 2012;116:182–5. doi: 10.1097/ALN.0b013e31823d7784. [DOI] [PubMed] [Google Scholar]
- 21.Pijls NH, van Schaardenburgh P, Manoharan G, Boersma E, Bech JW, van't Veer M, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis:5-year follow-up of the DEFER Study. J Am Coll Cardiol. 2007;49:2105–11. doi: 10.1016/j.jacc.2007.01.087. [DOI] [PubMed] [Google Scholar]
- 22.Johnson NP, Tóth GG, Lai D, Zhu H, Açar G, Agostoni P, et al. Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol. 2014;64:1641–54. doi: 10.1016/j.jacc.2014.07.973. [DOI] [PubMed] [Google Scholar]
- 23.Park JJ, Petraco R, Nam CW, Doh JH, Davies J, Escaned J, et al. Clinical validation of the resting pressure parameters in the assessment of functionally significant coronary stenosis;results of an independent, blinded comparison with fractional flow reserve. Int J Cardiol. 2013;168:4070–5. doi: 10.1016/j.ijcard.2013.07.030. [DOI] [PubMed] [Google Scholar]
- 24.Kern MJ, Lerman A, Bech JW, De Bruyne B, Eeckhout E, Fearon WF, et al. Physiological assessment of coronary artery disease in the cardiac catheterization laboratory: a scientific statement from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Circulation. 2006;114:1321–41. doi: 10.1161/CIRCULATIONAHA.106.177276. [DOI] [PubMed] [Google Scholar]
- 25.Brosh D, Higano ST, Lennon RJ, Holmes DR, Jr, Lerman A. Effect of lesion length on fractional flow reserve in intermediate coronary lesions. Am Heart J. 2005;150:338–43. doi: 10.1016/j.ahj.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Graham MM, Faris PD, Ghali WA, Galbraith PD, Norris CM, Badry JT, et al. Validation of three myocardial jeopardy scores in a population-based cardiac catheterization cohort. Am Heart J. 2001;142:254–61. doi: 10.1067/mhj.2001.116481. [DOI] [PubMed] [Google Scholar]
- 27.Shiono Y, Kubo T, Tanaka A, Kitabata H, Ino Y, Tanimoto T, et al. Impact of myocardial supply area on the transstenotic hemodynamics as determined by fractional flow reserve. Catheter Cardiovasc Interv. 2014;84:406–13. doi: 10.1002/ccd.25300. [DOI] [PubMed] [Google Scholar]
- 28.Kimball BP, Dafopoulos N, LiPreti V. Comparative evaluation of coronary stenoses using fluid dynamic equations and standard quantitative coronary arteriography. Am J Cardiol. 1989;64:6–10. doi: 10.1016/0002-9149(89)90644-9. [DOI] [PubMed] [Google Scholar]
- 29.Bache RJ, Schwartz JS. Effect of perfusion pressure distal to a coronary stenosis on transmural myocardial blood flow. Circulation. 1982;65:928–35. doi: 10.1161/01.cir.65.5.928. [DOI] [PubMed] [Google Scholar]
- 30.Gould KL, Kelley KO. Physiological significance of coronary flow velocity and changing stenosis geometry during coronary vasodilation in awake dogs. Circ Res. 1982;50:695–704. doi: 10.1161/01.res.50.5.695. [DOI] [PubMed] [Google Scholar]
- 31.Choy JS, Kassab GS. Scaling of myocardial mass to flow and morphometry of coronary arteries. J Appl Physiol. 2008;104:1281–6. doi: 10.1152/japplphysiol.01261.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]