Introduction
Key Teaching Points.
-
•
Permanent His bundle pacing offers an alternative method of cardiac resynchronization in the setting of multiple comorbidities, including renal failure.
-
•
The QRS morphology alone may not always clearly reflect loss of His capture when checking capture thresholds with a permanent His bundle lead. A multipolar catheter positioned at the His position would help discern an accurate His capture threshold.
-
•
An atrioventricular junction ablation can be safely performed without impacting the capture threshold of a newly implanted permanent His bundle lead with the aid of 3-dimensional mapping.
Cardiac resynchronization therapy (CRT) has shown a significant clinical benefit over right ventricular pacing in patients with left ventricular dysfunction and a high ventricular pacing requirement.1 Traditionally, CRT has relied on coronary sinus (CS) lead placement through the use of fluoroscopy and venography. Three-dimensional (3D) electroanatomic mapping has been used as an alternative technique for CS lead placement.2 Recently, permanent His bundle pacing has emerged as another technique to achieve CRT via near physiologic activation of both ventricles through the native His-Purkinje system. We report a novel technique for permanent His bundle lead placement followed by atrioventricular (AV) junction ablation using 3D mapping.
Case report
An otherwise healthy 92-year-old man was admitted with respiratory distress and rapid atrial fibrillation. Despite aggressive attempts at rate and rhythm control, recurrent hemodynamically significant atrial fibrillation resulted in acute liver and kidney injury. A transthoracic echocardiogram showed an ejection fraction of 45%. The decision was made to pursue atrioventricular node ablation and pacemaker implantation. Owing to the patient’s advanced age, severe renal dysfunction, and ventricular dysfunction, permanent His bundle pacing, rather than biventricular pacing, was favored as a method to achieve cardiac resynchronization and avoid the use of intravenous contrast. We report a novel method for safe, accurate, and effective His bundle lead implantation using a 3D mapping system (NavX; St. Jude Medical, St. Paul, MN).
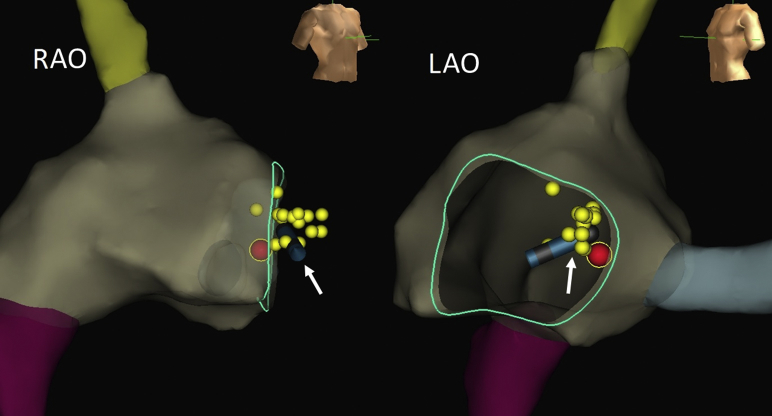
A 4-mm ablation catheter was used via a femoral venous approach to create a 3D geometry of the superior and inferior venae cavae, right atrium, His bundle region, and CS (Figure 1). An octapolar catheter was used to map both proximal and distal His bundle recordings (yellow dots). Pacing with this catheter from a His bundle location, distal to where AV node ablation would routinely be performed, resulted in parahisian capture.
Figure 1.
Three dimensional map of the His cloud, final permanent His bundle lead position, and site of AV node ablation: 3D map showing final permanent His bundle lead location (white arrow). The yellow dots represent His points collected during electroanatomic mapping. The red dot represents the site of AV node ablation at a more proximal location relative to the His bundle lead. LAO = left anterior oblique; RAO = right anterior oblique.
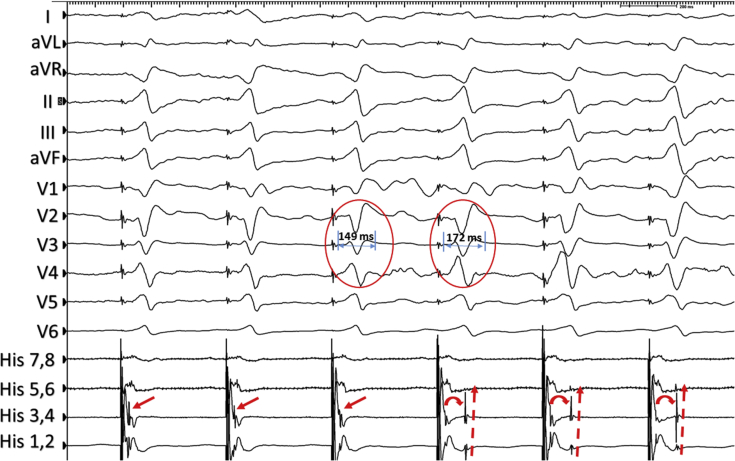
A preshaped sheath (C315 His; Medtronic, Inc, St. Paul, MN) was used to guide the active fixation pacing lead (3830 SelectSecure; Medtronic, Inc, St. Paul, MN) to a distal His bundle location under direct visualization with the 3D mapping system. Figure 2 shows the intracardiac recordings from the octapolar catheter during pacing from the permanent His bundle lead. Parahisian capture (solid red arrow) is shown at higher outputs with loss of His capture (curved red arrow) and retrograde His activation (dashed red arrows) at lower outputs despite a minimal change in QRS morphology (red circles). Though the change in QRS morphology is subtle, the increase in QRS duration reflects a change from parahisian to septal capture. The lead was secured at its final location (Figure 1, white arrow) with a parahisian capture threshold of 1.75 V at 1.0 ms and right ventricular septal capture threshold of 0.5 V at 1.0 ms. After connection to the pulse generator and pocket closure, radiofrequency catheter ablation of the AV node was performed at a location proximal to the His bundle lead (Figure 1, red dot). The parahisian capture threshold remained stable the following morning, and the patient was discharged home. He was unexpectedly readmitted 2 weeks later with acute respiratory failure secondary to health care–associated pneumonia. The pacemaker was functioning normally at this time. Owing to prior patient wishes regarding intubation and intensive care unit–level care, his family elected to pursue comfort care. The patient died owing to respiratory failure during the hospitalization.
Figure 2.
Intracardiac electrograms during permanent His bundle lead threshold testing: With decreasing outputs during threshold testing of the permanent His bundle lead, loss of his capture and retrograde His activation are shown on the octopolar mapping catheter (curved red arrows and dashed arrows). This is accompanied by a subtle change in QRS morphology, but a clear increase in QRS duration (red circles).
Discussion
To our knowledge, this is the first report of the use of 3D mapping to guide permanent His bundle lead implantation. His bundle pacing has emerged as an alternative technique to achieve electrical resynchronization.3, 4, 5 In this case, 3D mapping allowed lead placement at a location that resulted in His bundle capture without any compromise from AV node ablation. Further studies are needed with regard to the long-term efficacy and durability of this technique, as well as its potential to reduce procedure and fluoroscopy times.
Footnotes
Dr Knight has received consulting fees and speaker honoraria for Medtronic, Inc.
References
- 1.Curtis A.B., Worley S.J., Adamson P.B., Chung E.S., Niazi I., Sherfesee L., Shinn T., Sutton M.S. Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med. 2013;368(17):1585–1593. doi: 10.1056/NEJMoa1210356. [DOI] [PubMed] [Google Scholar]
- 2.Del Greco M., Maines M., Marini M. Three-dimensional electroanatomic mapping system-enhanced cardiac resynchronization therapy device implantation: results from a multicenter registry. J Cardiovasc Electrophysiol. 2017;28(1):85–93. doi: 10.1111/jce.13120. [DOI] [PubMed] [Google Scholar]
- 3.Lustgarten D.L., Calame S., Crespo E.M., Calame J., Lobel R., Spector P.S. Electrical resynchronization induced by direct His-bundle pacing. Heart Rhythm. 2010;7:15–21. doi: 10.1016/j.hrthm.2009.09.066. [DOI] [PubMed] [Google Scholar]
- 4.Deshmukh P., Casavant D.A., Romanyshyn M., Anderson K. Permanent, direct His-bundle pacing: a novel approach to cardiac pacing in patients with normal His-Purkinje activation. Circulation. 2000;101:869–877. doi: 10.1161/01.cir.101.8.869. [DOI] [PubMed] [Google Scholar]
- 5.Sharma P.S., Dandamudi G., Naperkowski A., Oren J.W., Storm R.H., Ellenbogen K.A., Vijayaraman P. Permanent His-bundle pacing is feasible, safe, and superior to right ventricular pacing in routine clinical practice. Heart Rhythm. 2015;12(2):305–312. doi: 10.1016/j.hrthm.2014.10.021. [DOI] [PubMed] [Google Scholar]