Abstract
Intestinal epithelial cells are the targets for transmissible gastroenteritis (TGE) virus (TGEV) infection. It is urgent to develop a novel candidate against TGEV entry. Bacillus subtilis is a probiotic with excellent anti-microorganism properties and one of its secretions, surfactin, has been regarded as a versatile weapon for most plant pathogens, especially for the enveloped virus. We demonstrate for the first time that B. subtilis OKB105 and its surfactin can effectively inhibit one animal coronavirus, TGEV, entering the intestinal porcine epithelial cell line (IPEC-J2). Then, several different experiments were performed to seek the might mechanisms. The plaque assays showed that surfactant could reduce the plaque generation of TGEV in a dose-dependent manner. Meanwhile, after incubation with TGEV for 1.5 h, B. subtilis could attach TGEV particles to their surface so that the number of virus to bind to the host cells was declined. Furthermore, our data showed that the inhibition of B. subtilis was closely related to the competition with TGEV for the viral entry receptors, including epidermal growth factor receptor (EGFR) and aminopeptidase N (APN) protein. In addition, Western blotting and apoptosis analysis indicated that B. subtilis could enhance the resistance of IPEC-J2 cells by up-regulating the expression of toll-like receptor (TLR)-6 and reducing the percentage of apoptotic cells. Taken together, our results suggest that B. subtilis OKB105 and its surfactin can antagonize TGEV entry in vitro and may serve as promising new candidates for TGEV prevention.
Keywords: antiviral, Bacillus subtilis OKB105, entry, surfactin, TGEV
Introduction
Transmissible gastroenteritis (TGE) virus (TGEV) is an enveloped virus that belongs to the coronaviridae family within the coronavirus genus [1,2]. It is the causative agent of porcine TGE, leading to vomiting, acute diarrhoea, dehydration and a nearly 100% mortality in suckling piglets [3]. Current vaccines, neither inactivated nor attenuated, cannot provide full protection to pigs [4]. Therefore, it is urgent to discover and develop a novel anti-TGEV candidate to reduce the economic losses caused by TGE.
Surfactin is a cyclic lipopeptide antibiotic and biosurfactant synthesized by Bacillus subtilis [5]. It consists of an anionic seven-membered peptide cyclo and a mixture of several hydrophobic β-hydroxy fatty acids with chain lengths of 13–15 carbon atoms [6]. By this amphiphilic structure, surfactin is one of the strongest biosurfactants. Studies on surfactin are focused on properties against phytopathogenic microorganisms, such as antibacterial [7], antifungal [8], inhibition of fibre clot formation [9] and antiviral [10,11] ability. Some reports showed that surfactin could inactivate various enveloped virus, like vesicular stomatitis virus (VSV, rhabdoviridae) and suid herpes virus type 1 (SHV-1, pseudorabies virus) , by inserting into the outer layer of lipid membrane bilayer so that the envelope disintegrates [12]. But whether surfactin has the activity against TGEV, an animal enveloped virus from coronaviridae family, remains poorly understood. Moreover, our colleagues had reported that B. subtilis could antagonize enteropathogenic Escherichia coli (ETEC) infection [13]. In the present study, we investigated the antiviral effects of B. subtilis OKB105 and its surfactin against TGEV entry in the intestinal porcine epithelial cell line (IPEC-J2) cells.
To explore the possible mechanisms, the effects of B. subtilis OKB105 and surfactin on viral infectivity as well as the impact on the receptors of TGEV, epidermal growth factor receptor (EGFR) and aminopeptidase N (APN), were investigated. Additionally, the toll-like receptors (TLRs) and the apoptosis of IPEC-J2 cells were also detected. Our results reveal that both the B. subtilis OKB105 and surfactin exhibit the suppressive activity against TGEV entry and may possibly serve as potential candidates to reduce the economic loss caused by TGE.
Materials and methods
Cells and virus
The IPEC-J2 cell lines (Guangzhou Jennio Biotech Co, Ltd., China) were maintained in Dulbecco’s modified Eagle’s medium nutrient (DMEM from Life Technologies, Shanghai, China) supplemented with 10% FBS (Gibco), 1% penicillin/streptomycin (Life Technologies) and 16 mM Hepes (Life Technologies) in a 37°C, 5% CO2 incubator. The TGEV strain SHXB (108 plaque forming units (pfu) per ml (pfu/ml)) was kindly provided by the Jiangsu Academy of Agricultural Sciences. All infections were performed at a multiplicity of infection (MOI) of 0.01.
Bacteria and surfactin
Inhibition of B. subtilis or surfactin
B. subtilis 168 and OKB105 (donated by Prof Xuewen Gao from College of Plant Protection in Nanjing Agricultural University) were cultivated in Luria broth (LB), then after centrifugation, the bacteria were washed three times to remove excess LB. Finally, the viable B. subtilis were resuspended in DMEM to the designed concentration from 1.00E + 07 to 1.00E + 10 colony forming units (cfu) per ml (cfu/ml). B. subtilis OKB105 was a surfactin producer transformed from B. subtilis 168 [14,15].
Surfactin used in the present study was extracted from B. subtilis OKB105 according to the procedures of Xue-wen et al. [16]. The concentration of surfactin is over 95% detected by HPLC.
Cellular toxicity assessment
Toxic effects of the B. subtilis and surfactin on IPEC-J2 cells were determined using the MTT viability assay [17]. Suspensions of 100 μl containing different amounts of B. subtilis ranging from 1.00E + 06 to 1.00E + 09 cfu/ml and concentrations of surfactin ranging from 2.00E – 06 to 2.00E – 01 mg/ml were added to IPEC-J2 cell monolayers in a 96-well plate (Corning Costar) for 2 h before washing away. Then 20 μl of MTT (1 mg/ml, Sigma) was added to the cells per well and incubated for 4 h at 37°C, the reaction was stopped by adding an equal volume of lysis buffer (50% DMSO and 20% SDS, pH 7.4). The absorbance was read at 570 nm. The cell survival rate was determined as the stimulatory index (SI) calculated according to the following equation: SI = (ODinfected well − ODbank control)/(ODnegative well − ODbank well). Mock-treated cells served as control. Each experiment was performed in triplicate.
Three setups focused on the suppressive effect against TGEV entry varying the treatment period. Briefly, monolayers of IPEC-J2 cells were treated with B. subtilis 168, OKB105 and surfactin for 1.5 h respectively, which was washed away before infection with TGEV for 1.5 h (pre-treatment assay), TGEV was added to the cell layer together with B. subtilis 168, OKB105 and surfactin respectively, during the 1.5 h infection period (co-treatment assay), virus was mixed with B. subtilis 168, OKB105 and surfactin respectively and incubated for 1.5 h at 37°C, aliquots were removed and diluted 1:10 with DMEM supplemented with 5% FBS to stop the effect of the surfactin and then sterile filtered through a 0.22 μm filter. Then the filtrate were added to the cell layer and incubated for 1.5 h (out-treatment assay). For the indicated time points, cells were washed three times and kept in medium containing 1% penicillin/streptomycin for 0.5 h to kill any viable bacteria that were left. After incubation, cells were washed three times, then re-suspended in TRIzol (Sigma) and stored at –80°C until analyses. As for the Western blotting, nuclear and cytoplasmic proteins were extracted and isolated using the Nuclear and Cytoplasmic Protein Extraction Kit (Beyotime, Jiangsu, China) [18] .
Plaque assays
To assess the direct effects of B. subtilis or surfactin on TGEV, we performed a plaque formation assay [19]. Briefly, the virus was mixed with different concentrations of B. subtilis or surfactin and incubated for 1.5 h at 37°C, after exorcizing the surfactin effect and probiotics as described above. Two hundred fifty microlitres of filtrate were added to confluent monolayers of ST cells (the susceptible cell) grown in six-well tissue culture plates (1–2 × 106 per well) and incubated for 1.5 h at 37°C. After washing, the cells were overlaid with 1640 medium containing 0.7% Sea-Plague agarose, 2% FBS and 1% penicillin/streptomycin. The plates were incubated at 4°C for 30 min to solidify the overlay medium. Cells were then grown at 37°C and 5% CO2 to allow plaque formation. Viral plaques were visualized by staining with 0.8% (w/v) Crystal Violet dye after 2-day incubation. Virus titres were calculated according to the following formula: Titre (pfu/ml) = number of plaques/volume of diluted virus added to the well × dilution factor of the virus used to infect the well in which plaques were enumerated. Virus without any treatment served as control and ST cells without addition of TGEV served as mock.
Binding effects of B. subtilis
In order to examine the possible direct binding of virus by B. subtilis, we mixed B. subtilis 168 or OKB105 with TGEV (1.00E + 07 cfu/ml bacterial cells with different MOIs: 0.01, 0.1, 0.2) for 1.5 h. After centrifugation, the bacterial cells were washed and re-suspended in 30 μl PBS. Viral nucleocapsid protein (N) (TGEV-N) was detected by Western blotting. PBS used in this test served as a native control, bacteria without virus served as a mock and TGEV served as the positive control.
The impact of B. subtilis or surfactin treatments on IPEC-J2 cells
Some studies reported that probiotic bacteria might also indirectly interfere with virus by altering the state of cells, stimulating innate and adaptive immunity. To find out how the B. subtilis or surfactin treatments mediate the state of cells, we made a single-treatment assay. Cells were treated with 1.00E + 07 cfu/ml B. subtilis or 0.002 mg/ml surfactin for 1.5 h, then the p-EGFR, APN and TLR-6 proteins were detected by Western blotting.
RNA extraction and qRT-PCR
For quantitative reverse transcription-PCR (qRT-PCR), total RNA from IPEC-J2 cells was extracted using a TRIzol reagent (Life Technologies) and subjected to reverse transcription with Prime Script qRT-PCR Kit (Takara, Dalian, CA). qPCR reactions were performed in ABI 7500 instrument (Applied Biosystems, U.S.A.). Gene expression was calculated with the comparative Ct method and normalized to the endogeneous levels of GAPDH. Primers sequences used for qRT-PCR are listed in Table 1. The data were analysed using the ABI PRISM 7500 software tool (Applied Biosystems).
Table 1.
Primer sequences used for qRT-PCR
| Gene | Type | Primer pairs (5′-3′) |
|---|---|---|
| GAPDH-for | Forward | TCATCATCTCTGCCCCTTCT |
| GAPDH-rev | Reverse | GTCATGAGTCCCTCCACGAT |
| TGEV-for | Forward | CAATTCCCGTGGTCGGAAGA |
| TGEV-rev | Reverse | TTTACGTTGGCCCTTCACCA |
| TLR-6-for | Forward | CTTTGCCCACCACAACCTCT |
| TLR-6-rev | Reverse | TTCACATCATCCTCTTCAGCGAC |
Western blotting
For immunodetection of the TGEV-N, p-EGFR, APN and TLR-6 proteins by Western blotting [20], rabbit anti-TGEV (VMRD, Hangzhou, China), rabbit anti-p-EGFR (CST) and rabbit anti-TLR6 (Bioss), followed by HRP–conjugated goat anti-mouse IgG and HRP–conjugated goat anti-rabbit IgG (Sigma) were used. The signal was detected using Super Signal West Pico lit (Thermo Scientific) and subjected to Image Reader LAS-4000 imaging system (FUJIFILM, Japan). The intensity of the bands in terms of density was measured and normalized against GAPDH expression. Three independent experiments and appropriate gel exposures yielded very similar results for each treatment modality.
Apoptosis assay
At indicated times in the three different treatment assays (the pre-, co-, out-treatment assays), cell apoptosis was further analysed with FITC Annexin V/propidium iodide (PI) staining assay (Miltenyi Biotec, Shanghai, China) as described recently [21].
Statistical analysis
Results are expressed as means ± S.D. or S.E.M.. One-way ANOVA and Student’s t test were employed to determine statistical differences among multiple groups. A P value of <0.05 was considered to be significant (*P<0.05, **P<0.01).
Results
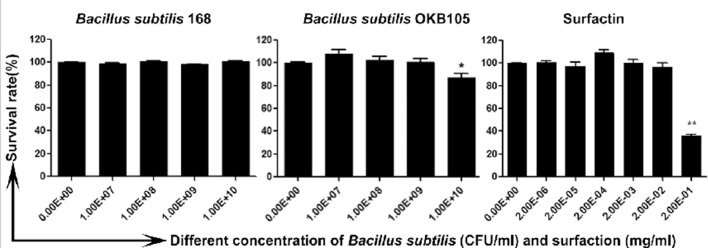
The safe dose of B. subtilis or surfactin
It was necessary to ensure that the doses added to cells were non-toxic. As shown in Figure 1, B. subtilis 168 was non-toxic in the used doses, B. subtilis OKB105 was non-toxic up to 1.00E + 09 cfu/ml, and the safe dose of surfactin was up to 0.02 mg/ml. Therefore, the safe dose of B. subtilis (1.00E + 07 cfu/ml) and surfactin (0.002 mg/ml) were used in the next study.
Figure 1. The cytotoxicity of Bacillus subtilis or surfactin in IPEC-J2 cells.
B. subtilis or surfactin were added to confluent cells in a 96-well plate, which were then incubated at 37°C for 2 h. Cell viability was measured by MTT and normalized to the value of non-treated control cells (set at 100%). The cell survival rates at different concentrations are given and 50% above the cell survival rate is regarded as a safe dose. Data are expressed as the S.E.M. from three independent experiments.
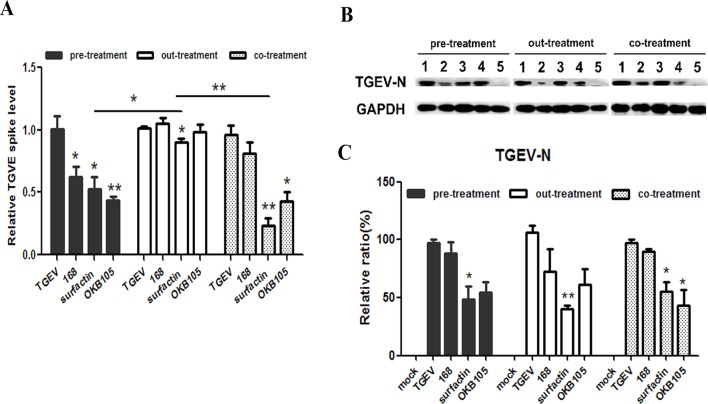
B. subtilis or surfactin inhibit the entry of TGEV
After different treatments, we detected the levels of TGEV-N mRNA and protein expression. First, for different ‘drugs’, our results showed that the relative amounts of viral RNAs in the surfactin-treated IPEC-J2 cells decreased in all treatments. On the other side, OKB105 reduced the relative amounts of viral RNAs in the pre-treatment and co-treatment, where cells existed. While B. subtilis 168 could only decrease the relative amounts of viral RNAs in the pre-treatment (Figure 2A). Second, for different ‘drugs’ in the same treatment, B. subtilis OKB105 showed the best suppression activity in the pre-treatment, where it had enough time of interacting with the cells. However, in the out-treatment, where the cells were not present, B. subtilis did not show significant inhibition, while surfactin did. Similar results were obtained in the Western blotting analysis (Figure 2B). Taken together, these data indicated that there might be a hidden association between B. subtilis and IPEC-J2 cells, while the surfactin might function on both the virus and the cells, and B. subtilis and the surfactin might show synergetic effect to some extent.
Figure 2. Suppress activity of B.subtilis or surfactin.
Cells were exposed to B. subtilis 168, OKB105 and surfactin in different treatments as described above. For the indicated time points, cells were collected and the yield of virus was determined by qRT-PCR (A) and Western blotting (B). (B) Lane 1, TGEV control; lane 2, virus from cells treated with 0.002 mg/ml surfactin; lane 3, virus from cells treated with 1.00E + 07 cfu/ml B. subtilis 168; lane 4, virus from cells treated with 1.00E + 07 cfu/ml B. subtilis OKB105; lane 5, mock. (C) Mean relative protein ratio of TGEV-N. Blots were reported with antibody to GAPDH as a loading control. The mean ± S.D. from three independent experiments are shown. Significance levels for the differences between B. subtilis and surfactin treatments and virus control from untreated cells are given above the bar: *P<0.05, **P<0.01.
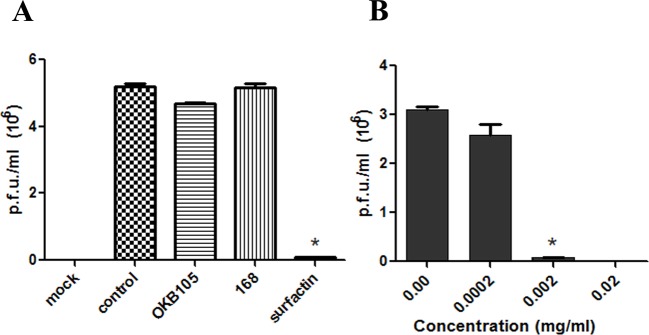
The reduction in the virus infectivity by the surfactin
To detect whether surfactin could directly reduce the infectivity of TGEV, a plaque assay was performed. The results showed significant (P<0.01) reduction in the TGEV load after treating with 0.002 mg/ml surfactin, but B. subtilis 168 or OKB105 did not (Figure 3A). Subsequently, the inhibitory effect of surfactin was further examined by mixing TGEV with different doses of surfactin, and the result showed that the reduction was in a dose-dependent manner (Figure 3B).
Figure 3. Evaluation of the B. subtilis or surfactin antiviral activities using plaque formation assay.
(A) Virus load expressed as pfu/ml was significantly reduced after treatment with surfactin compared with untreated virus. (B) The inhibitory effect of surfactin on TGEV was dose dependent (independent-samples T test, P<0.01).
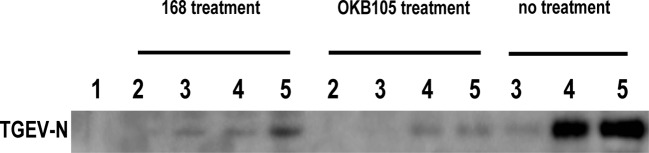
Attachment of TGEV particles to B. subtilis
A cell-free assay was performed to survey the attachment of TGEV to the B. subtilis. As shown in Figure 4, virus particles were bound by B. subtilis 168 and OKB105. And when mixed with TGEV at MOI 0.01, B. subtilis 168 could attach much more virus than OKB105.
Figure 4. Attachment of TGEV particles to B. subtilis 168 and OKB105.
After incubation with different concentration of TGEV ( MOI=0.01, 0.1, 0.2) for 1.5h, B.subtilis 168 and OKB105 were washed and detected by the TGEV-N in the western blotting analysis. Lane 1, negative control, the PBS used to re-suspend the bacterial cells; lane 2, mock, that bacterial cells without virus; lane 3 to lane 5, treatment with different concentration of TGEV (MOI=0.01, 0.1, 0.2).. No treatment: positive control, TGEV without bacterial treatment.
B. subtilis suppresses the TGEV entry by competing with virus for its receptors and improving the state of the IPEC-J2 cells
B. subtilis competes with TGEV for the viral-entry receptors
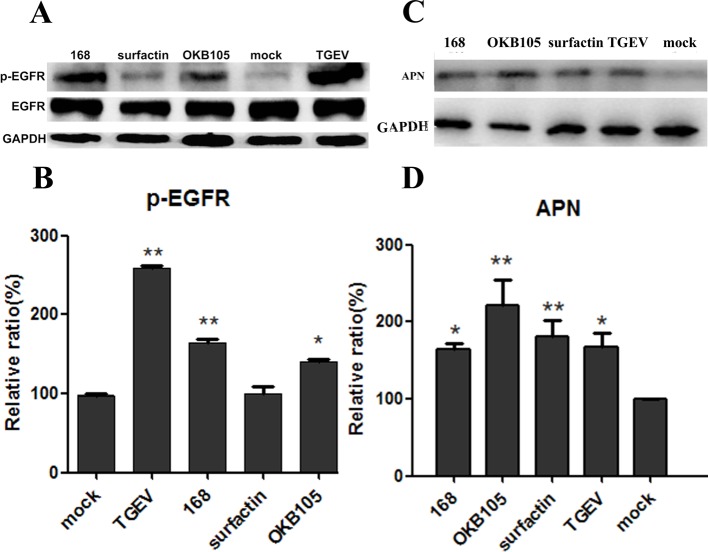
Binding to the cellular receptor is the first step of CoV entry process [22,23]. To test whether our ‘drugs’ could attach to the viral-entry receptors, we performed a single-treatment experiment. Interestingly, results showed that after stimulation with B. subtilis, both 168 and OKB105, the expression of both APN protein (Figure 5C) and p-EGFR (Figure 5A) were increased, which was the similar effect with the TGEV treatment. However, the surfactin stimulus did not change the two receptors expression.
Figure 5. B. subtilis 168 and OKB105 enhance the expression of APN protein and p-EGFR in IPEC-J2 cells.
IPEC-J2 cells were treated with B. subtilis or surfactin respectively, for 1.5 h and cell lysates were analysed for the expression of p-EGFR and APN protein. Both the TGEV and B. subtilis 168 and OKB105 enhanced the EGFR activation, and increased the expression of APN. Blots were reported with antibody to GAPDH as a loading control. (A) Expression of p-EGFR at IPEC-J2 in the protein level. (C) Expression of APN at IPEC-J2 in the protein level. (B) Mean relative protein ratio of p-EGFR. (D) Mean relative protein ratio of APN.
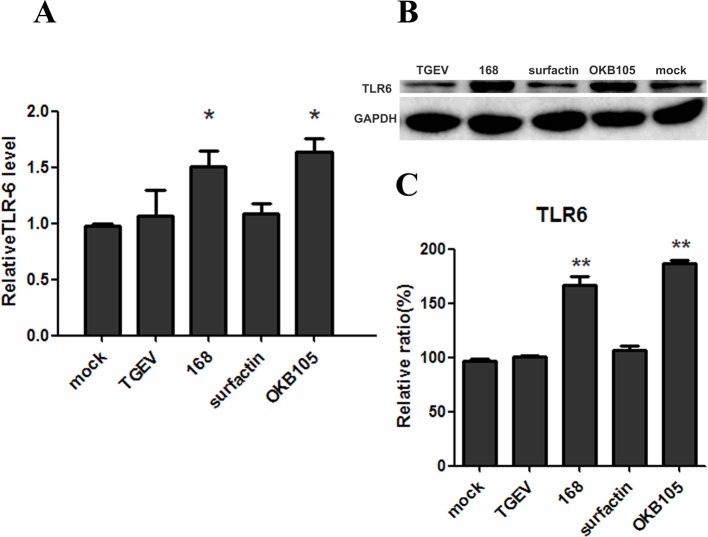
B. subtilis up regulate the expression of TLR-6 in IPEC-J2 cells
The state of cells is important to resist the pathogens. As the data shown in Figure 6, stimulation with with B. subtilis 168 or OKB105 could significantly up-regulate the TLR-6 mRNA expression in IPEC-J2 cells (Figure 6A). This could be demonstrated by Western blot on the protein level (Figure 6B).
Figure 6. Expression and regulation of TLR-6 at IPEC-J2 cells in the mRNA (A) and protein (B) level.
IPEC-J2 cells were left either non-stimulated (mock) or were stimulated with B. subtilis or surfactin. (A) RT-PCR was employed to determine TLR-6 mRNA expression. Data are shown as mean TLR-6/GAPDH ratio. (B) Mean relative protein ratio of TLR-6.
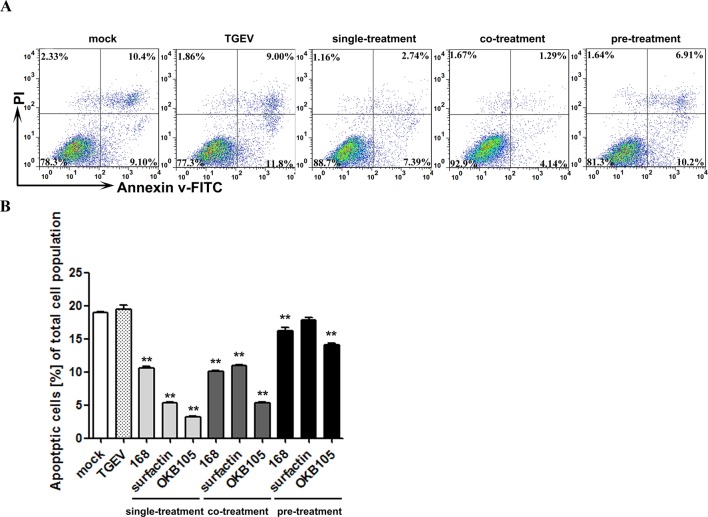
B. subtilis and the surfactin decreased the percentage of apoptotic cells
To explore the protective effect of B. subtilis and surfactin, the apoptosis of IPEC-J2 cells was assessed. As shown in Figure 7, TGEV could increase the apoptosis level of IPEC-J2 cells to some extent, while B. subtilis and surfactin could significantly reduce the apoptotic cells number (P<0.01). Although the ‘drugs’ displayed the same effect in the co-treatment, but the reduction extent was less than that in the single treatment. We owned this phonmenon to that the apoptosis caused by TGEV, which means when TGEV existed, the apoptosis level of IPEC-J2 was higher, and the reduction extent of apoptpsis our ‘drugs' caused was ease..
Figure 7. The inhibitory effect of B. subtilis or surfactin on IPEC-J2 cells apoptosis.
(A) Scatter plots of the annexin V-FITC/PI flow cytometry results of a representative experiment are presented below the graphs. The lower right quadrants represent cells in the early stage of apoptosis. The upper right quadrants represent cells in the later stage of apoptosis or necrotic cells. (B) The are expressed as the percentage of Annexin V-FITC-positive cells (apoptotic cells) in different treatments (*P<0.05, **P<0.01, compared with the data from mock-infected cells).
Discussion
TGEV enters epithelial cells by binding to the cellular receptor and then mediates membrane fusion at the plasma membrane or by endosomal uptake [24,25]. Previous studies have proven that APN protein is the receptor of TGEV [26]. Recently, Hu et al. [24] determined that EGFR was another receptor for TGEV entering IPEC-J2 cells. In order to interrupt TGEV infection in the origination stage, we detected the inhibition effect of B. subtilis OKB105 and the surfactin on TGEV entry process in vitro.
Different experimental protocols were applied in the present study, the pre-, co- and out-treatment assays. The cells were challenged with TGEV at MOI 0.01, as this more closely reflects the natural infection [27]. The results showed that surfactin could reduce the virus yields in all processes, no matter whether the host cells existed or not, while B. subtilis OKB105 only had the antiviral activity when the cells existed (Figure 2A) . We conjectured that surfactin could both affect the virus and the cells, while B. subtilis might alter the state of cells, eventually leading to an antiviral response. This hypothesis was confirmed in the sequential analysis.
Many reports showed that the probiotics could trap the virus by drop in virus titres [27,28]. Our results were consistent with these observations, after incubating with different titres of TGEV, B. subtilis 168 and OKB105 could trap most of TGEV on their surface (Figure 4). And an interesting phenomenon was that the attachment ability of B. subtilis 168 was better than B. subtilis OKB105, for there was much virus on the B. subtilis 168 surface when mixed with TGEV at MOI 0.01, which might indicate that the surfactin secreted by B. subtilis OKB105 had destroyed the trapped virion so that could not be detected by the Western blotting. This hypothesis was confirmed in the plaque assay, and we also confirmed that the inactivity of surfactin was dose dependent (Figure 3). Similar results had been observed in previous studies, by using EM, Dirk Vollenbroich et al. detected that the lipid membrane of SHV-1 was disintegrated after incubated with surfactin at 37°C for 1 h, Kracht et al. [12] also reported that surfactin could inactivate VSV.
Evidence have shown that probiotics could block viral attachment by competitive inhibition if they were able to bind viral receptors at the surface of cells [29,30]. Basbaum et al. [31] demonstrated that Gram-positive bacteria could active the EGFR by their lipoteichoic acid. Similarly, in the present study, we found that after stimulating with B. subtilis 168 and OKB105 for 1.5 h, the phosphorylation of EGFR and the expression of APN protein were both increased (Figure 6), which indicated that B. subtilis might compete with TGEV for binding to the receptors at the surface of IPEC-J2 cells.
The states of cells are critical for keeping healthy, including the response ability and the balance between intestinal cell proliferation and apoptosis, and TLRs play an important role in the sensing the viruses and in the initiation of antiviral host-defence response [32,33]. Since our study was focused on the TGEV entry process, the TLRs at the cells’ surface were investigated. To our knowledge, IPEC-J2 cells can express TLR1, TLR2, TLR3, TLR4, TLR6, TLR8, TLR9 and TLR10, but only TLR1, TLR2, TLR4 and TLR6 were expressed at the cells’ surface [34,35]. Regretfully, the TLR-2 was not detected in our IPEC-J2 cells (results not shown). Surprisingly, our results showed that the expression of TLR-6 was up-regulated after incubation with B. subtilis 168 and OKB105 (Figure 6). The results were supported by the fact that TLR-6 was a TLR that could identify the lipoproteins of Gram-positive bacteria [36]. TLR-6 was reported as a novel member of TLRs by Takeuchi et al. [37] in 1999, and it consisted of the signalling pathway of TLR2–TLR6–MyD88, MDA-5–IPS-1 and NALP3 inflammasome pathways [38].
Several clinical studies had demonstrated that TGEV could induce the apoptosis of some kinds of cells like porcine kidney (PK-15) cells [39,40] and ST cells [41]. Additionally, studies have reported that apoptosis was an important regulatory mechanism in intestine maturation [42]. In the present study, after a short-time incubation, all the three treatments could depress the percentage of apoptotic cells (Figure 7). And the depression of the percentage of apoptotic cells was better in the single treatment, where the TGEV did not exist, which might indicate that the TGEV could induce the apoptosis of this IPEC-J2 cells to some extent. Interestingly, Kim et al. [43] determined that surfactin could induce pro-apoptotic of LoVo cells, a human colon carcinoma cell line, when treated for 24 h. While in our study, we found that after treating with 0.002 μg/ml surfactin for 1.5 h, the percentage of apoptotic cells was depressed, which indicted that a safe dose and for a safe time, surfactin could display a positive effect on cells. But how surfactin affect the cells, especially animal cells needs more penetrating study.
Conclusion
The results of the present study demonstrate that B. subtilis OKB105 and the surfactin have antiviral activity against TGEV entering IPEC-J2 cells. And that possibly overlapping mechanisms lead to the antiviral activity: might by competing with TGEV in combining to the receptors, adsorptive trapping, inactivation of virus particles of surfactin, improvement of the cell state through activating the innate immunity and induce the apoptosis level. This finding suggests that B. subtilis OKB105 and the surfactin could serve as potential candidates against TGEV entry in vitro.
Abbreviations
- APN
aminopeptidase N
- cfu
colony forming unit
- CoV
coronavirus
- CST
Cell Signaling Technology
- DMEM
Dulbecco’s modified Eagle’s medium
- EGFR
epidermal growth factor receptor
- for
forward
- GAPDH
glyceraldehyde-3-phosphate dehydrogenase
- HRP
Horseradish Peroxidase
- IPEC-J2
intestinal porcine epithelial cell line
- IPS-1
interferon beta promoter stimulator 1
- LB
Luria broth
- LoVo
human colon cancer cell line LoVo
- MDA-5
melanoma differentiation associated gene 5
- MOI
multiplicity of infection
- MyD88
myeloid differentiation factor 88
- NALP3
NACHT, LRR and domains-containing protein 3
- pfu
plaque forming units
- PI
propidium iodide
- qPCR
quantitative real-time PCR
- qRT-PCR
quantitative reverse transcription-PCR
- rev
reverse
- SHV-1
suid herpes virus type 1
- SI
stimulatory index
- ST
swine testis
- TGE
transmissible gastroenteritis
- TGEV
transmissible gastroenteritis virus
- TLR
toll-like receptor
- T test
student's t test
- VMRD
Veterinary Medical Research & Dev
- VSV
vesicular stomatitis virus
- 1640 medium
culture medium for ST cells
Competing interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China [grant number 31372465]; and the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author contribution
W.H. helped in part of the experimental design and L.Z. provided excellent technical assistance. Qian Yang conceived and designed the experiment and modified the article. Xiaoqing Wang performed the experiment and wrote the article.
References
- 1.Carstens E.B. (2010) Ratification vote on taxonomic proposals to the International Committee on Taxonomy of Viruses (2009). Arch. Virol. 155, 133–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pratelli A. (2011) The evolutionary processes of canine coronaviruses. Adv. Virol. 2011, 562831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zou H., Zarlenga D.S., Sestak K., Suo S. and Ren X. (2013) Transmissible gastroenteritis virus: identification of M protein-binding peptide ligands with antiviral and diagnostic potential. Antiviral Res. 99, 3, 383–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwegmann-Wessels C. and Herrler G. (2006) Sialic acids as receptor determinants for coronaviruses. Glycoconj. J. 23, 51–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sen R. (2010) Surfactin: biosynthesis, genetics and potential applications. Adv. Exp. Med. Biol. 672, 316–323 [DOI] [PubMed] [Google Scholar]
- 6.Kowall M., Vater J., Kluge B., Stein T., Franke P. and Ziessow D. (1998) Separation and characterization of surfactin isoforms produced by Bacillus subtilis OKB 105. J. Colloid Interface Sci. 204, 1–8 [DOI] [PubMed] [Google Scholar]
- 7.Cawoy H., Mariutto M., Henry G., Fisher C., Vasilyeva N., Thonart P. et al. (2014) Plant defense stimulation by natural isolates of Bacillus depends on efficient surfactin production. Molecular Plant-Microbe Interation. 27, 2, 87–100 [DOI] [PubMed] [Google Scholar]
- 8.Płaza G.A., Turek A., Król E. and Szczgłowska R. (2013) Antifungal and antibacterial properties of surfactin isolated from Bacillus subtilis growing on molasses. Afr. J. Microbiol. Res. 7, 3165–3170 [Google Scholar]
- 9.Aleti G., Lehner S., Bacher M., Compant S., Nikolic B., Pleasko M. et al. (2016) Surfactin variants mediate species-specific biofilm formation and root colonization in Bacillus. Environ. Microbiol. 18, 2634–2645 [DOI] [PubMed] [Google Scholar]
- 10.Vilà S., Badosa E., Montesinos E., Planas M. and Feliu L. (2016) Synthetic cyclolipopeptides selective against microbial, plant and animal cell targets by incorporation of D-amino acids or histidine. PLoS ONE 11, e0151639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vollenbroich D., Özel M., Vater J., Kamp R.M. and Pauli G. (1997) Mechanism of inactivation of enveloped viruses by the biosurfactant surfactin from Bacillus subtilis. Biologicals 25, 289–297 [DOI] [PubMed] [Google Scholar]
- 12.Kracht M., Rokos H., Ozel M., Kowall M., Pauli G. and Vater J. (1999) Antiviral and hemolytic activities of surfactin isoforms and their methyl ester derivatives. J. Antibiot. (Tokyo), 52, 7, 613–619 [DOI] [PubMed] [Google Scholar]
- 13.Ye X.L., Li P.C., Yu Q.H. and Yang Q. (2013) Bacillus subtilis inhibition of enterotoxic Escherichia coli-induced activation of MAPK signaling pathways in Caco-2 cells. Ann. Microbiol. 63, 577–581 [Google Scholar]
- 14.Nakano M.M., Marahiel M. and Zuber P. (1988) Identification of a genetic locus required for biosynthesis of the lipopeptide antibiotic surfactin in Bacillus subtilis. J. Bacteriol. 170, 5662–5668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang Y., Wu H.J., Lin L., Zhu Q.Q., Borriss R., Gao X.W. (2015) A plasmid-born Rap-Phr system regulates surfactin production, sporulation and genetic competence in the heterologous host, Bacillus subtilis OKB105. Appl. Microbiol. Biotechnol. 99, 7241–7252 [DOI] [PubMed] [Google Scholar]
- 16.Xue-wen G., Shiyi Y., Pham H., Vater J. and Jin-sheng W. (2004) Lipopeptide antibiotics produced by the engineered strain Bacillus subtilis GEB3 and detection of its bioactivity. Agricultural Sciences in China 3, 3, 192–197 [Google Scholar]
- 17.Denizot F. and Lang R. (1986) Rapid colorimetric assay for cell growth and survival: modifications to the tetrazolium dye procedure giving improved sensitivity and reliability. J. Immunol. Methods 89, 271–277 [DOI] [PubMed] [Google Scholar]
- 18.Wang J., Du X.-X., Jiang H. and Xie J.-X. (2009) Curcumin attenuates 6-hydroxydopamine-induced cytotoxicity by anti-oxidation and nuclear factor-kappa B modulation in MES23. 5 cells. Biochem. Pharmacol. 78, 178–183 [DOI] [PubMed] [Google Scholar]
- 19.Zhang Y., Wei Y., Li J. and Li J. (2012) Development and optimization of a direct plaque assay for human and avian metapneumoviruses. J. Virol. Methods 185, 61–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Z., Yu Q., Gao J. and Yang Q. (2012) Mucosal and systemic immune responses induced by recombinant Lactobacillus spp. expressing the hemagglutinin of the avian influenza virus H5N1. Clin. Vaccine Immunol. 19, 174–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhu L.Q., Mou C.X., Yang X., Lin J. and Yang Q. (2016) Mitophagy in TGEV infection counteracts oxidative stress and apoptosis. Oncotarget 7, 27122–27141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iyengar S., Hildreth J.E.K. and Schwartz D.H. (1998) Actin-dependent receptor colocalization required for human immunodeficiency virus entry into host cells. J. Virol. 72, 5251–5255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clement C., Tiwari V., Scanlan P.M., Valyi-Nagy T., Yue B.Y. and Shukla D. (2006) A novel role for phagocytosis-like uptake in herpes simplex virus entry. J. Cell Biol. 174, 1009–1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu W., Zhu L., Yang X., Lin J. and Yang Q. (2016) The epidermal growth factor receptor regulates cofilin activity and promotes transmissible gastroenteritis virus entry into intestinal epithelial cells. Oncotarget 7, 12206–12221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guo L., Yu H., Gu W., Luo X., Li R., Zhang J. et al. (2016) Autophagy negatively regulates transmissible gastroenteritis virus replication. Sci. Rep. 6, 23864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Delmas B., Gelfi J., L’Haridon R., Vogel L.K., Sjöström H., Norén O. et al. (1992) Aminopeptidase N is a major receptor for the enteropathogenic coronavirus TGEV. Nature, 357, 417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chai W., Burwinkel M., Wang Z., Palissa C., Esch B., Twardziok S. et al. (2013) Antiviral effects of a probiotic Enterococcus faecium strain against transmissible gastroenteritis coronavirus. Arch. Virol. 158, 799–807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takeuchi O. and Akira S. (2007) Recognition of viruses by innate immunity. Immunol. Rev. 220, 214–224 [DOI] [PubMed] [Google Scholar]
- 29.Freitas M., Tavan E., Cayuela C., Diop L., Sapin C. and Trugnan G. (2003) Host-pathogens cross-talk. Indigenous bacteria and probiotics also play the game. Biol. Cell 95, 503–506 [DOI] [PubMed] [Google Scholar]
- 30.Freitas M., Cayuela C., Antoine J.M., Piller F., Sapin C. and Trugnan G. (2001) A heat labile soluble factor from Bacteroides thetaiotaomicron VPI‐5482 specifically increases the galactosylation pattern of HT29-MTX cells. Cell. Microbiol. 3, 289–300 [DOI] [PubMed] [Google Scholar]
- 31.Basbaum C., Li D., Gensch E., Gallup M. and Lemjabbar H. (2003) Mechanisms by which gram-positive bacteria and tobacco smoke stimulate mucin induction through the epidermal growth factor receptor (EGFR). Novartis Found. Symp 171–176 [PubMed] [Google Scholar]
- 32.Pichlmair A. and Reis e Sousa C. (2007) Innate recognition of viruses. Immunity 27, 370–383 [DOI] [PubMed] [Google Scholar]
- 33.Kawai T. and Akira S. (2011) Toll-like receptors and their crosstalk with other innate receptors in infection and immunity. Immunity 34, 637–650 [DOI] [PubMed] [Google Scholar]
- 34.Finberg R.W., Wang J.P. and Kurt-Jones E.A. (2007) Toll like receptors and viruses. Rev. Med. Virol. 17, 35–43 [DOI] [PubMed] [Google Scholar]
- 35.Lan D., Tang C., Yue H., Sun H., Cui L., Hua X. et al. (2013) Microarray analysis of differentially expressed transcripts in porcine intestinal epithelial cells (IPEC-J2) infected with porcine sapelovirus as a model to study innate immune responses to enteric viruses. Arch. Virol. 158, 1467–1475 [DOI] [PubMed] [Google Scholar]
- 36.Takeuchi O., Kawai T., Mühlradt P.F., Morr M., Radolf J.D., Zychlinsky A. et al. (2001) Discrimination of bacterial lipoproteins by toll-like receptor 6. Int. Immunol. 13, 933–940 [DOI] [PubMed] [Google Scholar]
- 37.Takeuchi O., Kawai T., Sanjo H., Copeland N.G., Gilbert D.J., Jenkins N.A. et al. (1999) TLR6: a novel member of an expanding Toll-like receptor family. Gene 231, 59–65 [DOI] [PubMed] [Google Scholar]
- 38.Delaloye J., Roger T., Steiner-Tardivel Q.G., Le Roy D., Knaup Reymond M., Akira S. et al. (2009) Innate immune sensing of modified vaccinia virus ankara (MVA) is mediated by TLR2-TLR6, MDA-5 and the NALP3 inflammasome. PLoS Pathog. 5, 6, e1000480. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 39.Huang Y., Ding L., Li Z.C., Dai M.L., Zhao X.M., Li W. et al. (2013) Transmissible gastroenteritis virus infection induces cell apoptosis via activation of p53 signalling. J. Gen. Virol. 94, 1807–1817 [DOI] [PubMed] [Google Scholar]
- 40.Ding L., Xu X.G., Huang Y., Li Z.C., Zhang K., Chen G.D. et al. (2012) Transmissible gastroenteritis virus infection induces apoptosis through FasL- and mitochondria-mediated pathways. Vet. Microbiol. 158, 12–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sirinarumitr T., Kluge J. and Paul P. (1998) Transmissible gastroenteritis virus induced apoptosis in swine testes cell cultures. Arch. Virol. 143, 2471–2485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vachon P.H., Cardin E., Harnois C., Reed J.C. and Vézina A. (2000) Early establishment of epithelial apoptosis in the devel-oping human small intestine. Int. J. Dev. Biol. 44, 891–898 [PubMed] [Google Scholar]
- 43.Kim S.-Y., Kim J.Y., Kim S.-H., Bae H.J., Yi H., Yoon S.H. et al. (2007) Surfactin from Bacillus subtilis displays anti-proliferative effect via apoptosis induction, cell cycle arrest and survival signaling suppression. FEBS Lett. 581, 865–871 [DOI] [PubMed] [Google Scholar]