Abstract
IMPORTANCE
Patients with facial paralysis are perceived negatively by society in a number of domains. Society’s perception of the health utility of varying degrees of facial paralysis and the value society places on reconstructive surgery for facial reanimation need to be quantified.
OBJECTIVE
To measure health state utility of varying degrees of facial paralysis, willingness to pay (WTP) for a repair, and the subsequent value of facial reanimation surgery as perceived by society.
DESIGN, SETTING, AND PARTICIPANTS
This prospective observational study conducted in an academic tertiary referral center evaluated a group of 348 casual observers who viewed images of faces with unilateral facial paralysis of 3 severity levels (low, medium, and high) categorized by House-Brackmann grade. Structural equation modeling was performed to understand associations among health utility metrics, WTP, and facial perception domains. Data were collected from July 16 to September 26, 2015.
MAIN OUTCOMES AND MEASURES
Observer-rated (1) quality of life (QOL) using established health utility metrics (standard gamble, time trade-off, and a visual analog scale) and (2) their WTP for surgical repair.
RESULTS
Among the 348 observers (248 women [71.3%]; 100 men [28.7%]; mean [SD] age, 29.3 [11.6] years), mixed-effects linear regression showed that WTP increased nonlinearly with increasing severity of paralysis. Participants were willing to pay $3487 (95% CI, $2362–$4961) to repair low-grade paralysis, $8571 (95% CI, $6401–$11 234) for medium-grade paralysis, and $20 431 (95% CI, $16 273–$25 317) for high-grade paralysis. The dominant factor affecting the participants’ WTP was perceived QOL. Modeling showed that perceived QOL decreased with paralysis severity (regression coefficient, −0.004; 95% CI, −0.005 to −0.004; P < .001) and increased with attractiveness (regression coefficient, 0.002; 95% CI, 0.002 to 0.003; P < .001). Mean (SD) health utility scores calculated by the standard gamble metric for low- and high-grade paralysis were 0.98 (0.09) and 0.77 (0.25), respectively. Time trade-off and visual analog scale measures were highly correlated. We calculated mean (SD) WTP per quality-adjusted life-year, which ranged from $10 167 ($14 565) to $17 008 ($38 288) for low- to high-grade paralysis, respectively.
CONCLUSIONS AND RELEVANCE
Society perceives the repair of facial paralysis to be a high-value intervention. Societal WTP increases and perceived health state utility decreases with increasing House-Brackmann grade. This study demonstrates the usefulness of WTP as an objective measure to inform dimensions of disease severity and signal the value society places on proper facial function.
LEVEL OF EVIDENCE
NA.
Patients with facial paralysis have negative psychosocial consequences, including difficulty emoting and diminished quality of life (QOL).1–4 The current treatment for permanent facial paralysis is facial reanimation surgery, which encompasses a broad range of procedures that restore form and function to the paralyzed face.5,6 As the practice of facial plastics moves toward objective quality measurements,7 the importance of understanding the health utility of facial paralysis and the value of facial reanimation surgery increases.
To understand these measures, 2 perspectives offer key insights—those of the patient and societal members—with recognition that neither is a substitute for the other. The investigation of society’s perspective calls on the age-old economic principle of the “wisdom of crowds,” which asserts that society at large is better at aggregating information and estimating the true value of goods than discrete individuals alone.8 For facial paralysis, the assessment of the layperson has been said to be one of the most important yet elusive measurements to obtain.9 We sought to quantify the value society places on a fully functioning face by measuring the perceived health utility of individuals with facial paralysis and valuation of surgical repair, with the understanding that societal willingness to pay (WTP) represents the hypothetical limit of resources that individuals are willing to allocate to medical interventions.10
Furthermore, previous studies have demonstrated the usefulness of the ratio of WTP per quality-adjusted life-year (QALY) in understanding societal valuations of expenditures for medical interventions.10,11 This ratio is generated using a contingent valuation method in which a population states their WTP for an intervention. Zillich et al12 showed that WTP for an asthma cure is highly related to objective and subjective measures of disease severity. The denominator of the ratio, health utility, refers to societal members’ rating of the QOL with a given health state derived from standard gamble (SG),13 time trade-off (TTO),14 and visual analog scale (VAS)15 methods.
The WTP:QALY ratio has been used to understand the societal value of repairing knee osteoarthritis16 and cutaneous facial lesions.17 Sinno et al18 measured the perceived health utility of facial paralysis. Other studies have shown that facial reanimation surgery restores affect display (the expression of emotion through facial expression), improves attractiveness, and decreases negative facial perception.19–21 To our knowledge, the societal WTP to repair varying degrees of facial paralysis, the perceived health utility of varying degrees of facial paralysis, and the subsequent societal valuation of facial reanimation surgery remain unstudied. We had the following major aims for this study: (1) to measure the value society places on repairing facial paralysis (through measurement of societal WTP and perceived health utility of patients with facial paralysis); (2) to understand facial perception domains that influence this societal perspective; and (3) to demonstrate WTP as a marker for studying facial perception and the severity of facial deformity.
Methods
Participants
Participants were casual observers recruited via surveys posted on public access websites. Individuals were excluded if they were younger than 18 years or had schizophrenia or autism spectrum disorders because of differences in the ways individuals with these disorders perceive faces.22,23 Twenty-one participants were excluded based on these criteria. Complete surveys were collected from 348 participants. Demographic profiles of the participants are presented in Table 1. The Johns Hopkins Medicine institutional review board approved this study and waived the need for informed consent.
Table 1.
Demographic Characteristics of Study Participants
| Characteristic | No. (%) of Participants (N = 348)a |
|---|---|
| Age, mean (SD), y | 29.3 (11.6) |
| Sex | |
| Female | 248 (71.3) |
| Male | 100 (28.7) |
| Race | |
| Asian | 95 (27.3) |
| African American | 31 (8.9) |
| White | 197 (56.6) |
| American Indian | 5 (1.4) |
| Pacific Islander | 3 (1.2) |
| Other | 17 (4.9) |
| Hispanic/Latinob | 22 (6.3) |
| Educational level | |
| Some high school | 2 (0.6) |
| High school or GED | 23 (6.6) |
| Some college | 52 (14.9) |
| Associate degree | 10 (2.9) |
| Bachelor’s degree | 176 (50.6) |
| Master’s degree | 72 (20.7) |
| Doctoral degree | 13 (3.7) |
| Annual household income, $1000 | |
| <25 | 106 (30.5) |
| 25–49 | 72 (20.7) |
| 50–74 | 45 (12.9) |
| 75–99 | 35 (10.1) |
| 100–149 | 32 (9.2) |
| 150–199 | 22 (6.3) |
| ≥200 | 25 (7.2) |
| NA | 11 (3.2) |
| Facial paralysis experience | |
| Personal | 8 (2.3) |
| Relatives with facial paralysis | 24 (6.9) |
Abbreviations: GED, General Educational Development; NA, not available.
Percentages have been rounded and may not total 100.
Participants may identify in addition to other race.
Survey Instrument
Photographs of 16 individuals (4 individuals without paralysis serving as controls and 12 individuals with unilateral facial paralysis) were queried from the Johns Hopkins facial plastic surgery image archive. Of the 12 individuals with facial paralysis, 4 were included in each of 3 categories of facial paralysis (low, medium, and high). We categorized low-grade paralysis as House-Brackmann grade 2, medium-grade paralysis as House-Brackmann grades 3 to 4, and high-grade paralysis as House-Brackmann grades 5 to 6. Four unique surveys were then generated with 8 photographs each. The composition of each survey included 2 photographs in each of the following 4 categories: normal and low-grade, medium-grade, and high-grade paralysis. We included 1 smiling and 1 reposed photograph for each of the 4 categories. Each individual was shown only once within a survey, and no photograph was duplicated among the 4 surveys. The survey collected the following 3 vital pieces of information: (1) facial perception metrics, (2) metrics to calculate perceived health utility, and (3) the participant’s WTP for a repair.
Facial Perception
Participants were asked to rate facial perception domains, including the attractiveness, affect display, and paralysis severity of each face they were shown. Attractiveness and severity were measured on a scale of 0 to 100, with higher scores corresponding to greater attractiveness and severity. Affect display was assessed with a scale of 0 to 100 informed by the Derogatis Affects Balance Scale core affects (hostile, depressed, guilty, joyful, content, vigorous), with 0 being defined as a negative affect (ie, face appears hostile, depressed, or guilty) and 100 as a positive affect (ie, joyful, content, or vigorous).24
Health Utility
Health utility was measured using 3 established methods described in cost-effectiveness analysis literature as SG,13 TTO,14 and VAS.15 Standard gamble is measured by giving participants a choice between living with a medical condition or accepting treatment that carries a specified risk for death.10,16 Participants were asked to imagine the photograph shown as their own face and choose between living with that face and electing for facial reanimation surgery with a risk for immediate death. Depending on the participant’s choice, a bisecting algorithm generated up to 6 iterations of risk percentages until an inflection point of acceptable risk was assumed.13,18
Time trade-off is measured by giving participants the choice between living with a medical condition and trading years of life in exchange for an immediate cure.16 We used 40 years as the maximum number of additional years one can live without trading off years of life. This value was obtained by estimating a life expectancy of 80 years and subtracting 40 years, the median age of diagnosis for Bell palsy.25 Participants were thus asked to choose between living 40 years with the face in the image shown and living for fewer years without facial paralysis. Finally, using the VAS method, participants imagined each face as their own and rated perceived health utility with a slider bar with 1-point increments anchored from 0 (death) to 100 (perfect health or no paralysis).
Willingness to Pay
Finally, we assessed WTP using an iterative closed-ended bidding method. Participants were asked whether they were willing to pay to repair the facial paralysis they saw and offered an out-of-pocket cost for the intervention. Participants indicated whether they would be willing to pay more than that value (no or yes). As described by Dey et al,17 a bisection algorithm with 6 iterations was used before obtaining a final WTP value. Inputs into this algorithm (starting WTP value and lower and upper bound values) were assessed using a pilot study that asked 22 individuals their WTP to correct varying grades of facial paralysis.
Statistical Analysis
Data were collected using the Qualtrics Online Survey Software26 from July 16 to September 26, 2015, and analyzed using STATA statistical software (version 13 SE; StataCorp). We derived health utility values from SG, TTO, and VAS metrics using standard methods.16 With measured health utility and WTP values, we calculated WTP:QALY ratios with the method described by King et al.10 Because WTP has been shown to be highly skewed for reflecting diverse individual preferences, we applied a Box-Cox transformation to normality on WTP data with a lambda factor of 0.2696841.10 We used a 3% discount rate to calculate the present value of future health benefits10 and the National Vital Statistics database to estimate life expectancies adjusted by participant demographic profiles.27
We applied structural equation modeling (SEM) to analyze the significance and directionality of associations between facial perception metrics (attractiveness, affect, and severity), a latent variable we defined as perceived QOL (P-QOL), and health utility metrics (derived from SG, TTO, and VAS). We used SEM for its ability to fit networks of constructs to data and account for sources of variance. We used a multivariate probit model to elucidate when participants identified paralysis and when they accepted TTO or SG. This probability model was used to mix normal and paralysis models when analyzing WTP as a function of paralysis severity.
Results
Completed surveys were analyzed from 348 participants (248 women [71.3%]; 100 men [28.7%]; mean [SD] age, 29.3 [11.6] years). The income distribution of participants is representative of that of the US population.28 The demographic distribution exhibits a skew toward younger individuals, individuals with higher levels of education, and women. The 3 main categories of information that were collected and/or calculated included (1) WTP to reanimate a face, (2) health utility, and (3) value calculated as a ratio of the former 2 variables (ie, WTP:QALY).
Structural Equation Modeling
Figure 1 is a conceptual network diagram of the SEM generated from participant response data. The diagram demonstrates that paralysis severity as defined by House-Brackmann grade has a direct association with observer-perceived severity. If the shown face was smiling, perceived severity increased, perceived affect display was rated more positively, and attractiveness ratings decreased. In addition, perception of greater severity of paralysis decreased attractiveness and affect ratings, and positive affect scores increased attractiveness ratings. We hypothesized that if a participant perceived a face as having higher QOL, he or she would be willing to trade less time off their lives (decreased TTO), assume a lower risk for death (decreased SG), and pay less money to repair the facial paralysis (decreased WTP). To demonstrate this, we included a latent P-QOL variable to connect concepts of paralysis severity and facial perception domains to calculated health utility values and WTP. If a participant rated attractiveness as high, the P-QOL variable increased; if a participant rated the severity of paralysis as high, the P-QOL variable decreased. The model confirmed our hypothesis that as P-QOL increased, SG, TTO, and WTP all decreased. In addition, if a participant identified a face as having paralysis, this effect independently increased WTP for a repair. Magnitude of influence and statistical significance of each SEM association are detailed in Table 2. We also found an inflection point of QOL under which participants did not accept TTO or SG. The inflection point for SG was lower than that for TTO (ie, participants would sooner risk a chance of immediate death than trade time off their lives) (probit model in Table 2).
Figure 1. Structural Equation Model Network Diagram.
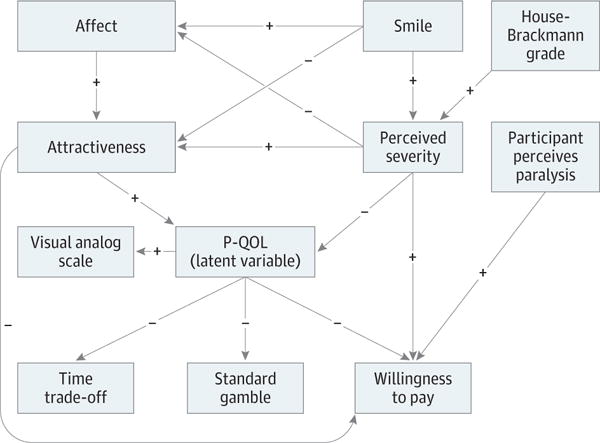
The structural equation model reflects associations among perceived facial characteristics, the perceived quality-of-life (P-QOL) latent variable, measures of health state utility, and willingness to pay (WTP). Each arrow represents a statistically significant association, and the arrow direction indicates the flow. A positive sign represents a positive association (eg, as the affect rating increases, the attractiveness rating increases), and a negative sign represents an inverse association (eg, if perceived QOL is high, WTP for a repair decreases).
Table 2.
SEM and Probit Model Findings
| Dependent Variable and Covariate | Structural Equation Model, Regression Coefficient (SE) [95% CI] | P Value |
|---|---|---|
| Fixed Effects | ||
| QOL VAS | ||
| P-QOL | 1 [Reference] | NA |
| Constant | 0.76 (0.01) [0.73 to 0.78] | <.001 |
| Severitya | ||
| Low-grade paralysisb | 7.50 (0.95) [5.65 to 9.36] | <.001 |
| Medium-grade paralysisc | 26.90 (0.95) [25.04 to 28.76] | <.001 |
| High-grade paralysisd | 64.52 (0.95) [62.67 to 66.38] | <.001 |
| Smilinge | 14.91 (0.67) [13.59 to 16.22] | <.001 |
| Observer variance | 1 [Reference] | NA |
| Constant | −3.58 (0.84) [−5.23 to −1.92] | <.001 |
| Attractivenessf | ||
| Severity | −0.28 (0.01) [−0.30 to −0.26] | <.001 |
| Affect | 0.50 (0.02) [0.47 to 0.53] | <.001 |
| Smilinge | −6.20 (0.65) [−7.48 to −4.92] | <.001 |
| Observer variance | 1 [Reference] | NA |
| Constant | 57.64 (0.60) [56.47 to 58.82] | <.001 |
| Affecta | ||
| Severity | −0.270 (0.01) [−0.29 to −0.25] | <.001 |
| Smiling | 23.77 (0.72) [22.36 to 25.20] | <.001 |
| Constant | 2.28 (0.55) [1.20 to 3.36] | <.001 |
| P-QOLg | ||
| Severity | −0.004 (0.000) [−0.005 to −0.004] | <.001 |
| Attractiveness | 0.002 (0.000) [0.002 to 0.003] | <.001 |
| TTOg | ||
| Willing TTO | −0.04 (0.02) [−0.08 to −0.01] | .01 |
| P-QOL | −1.00 (0.01) [−1.02 to −0.98] | <.001 |
| Unwilling TTO × P-QOLh | 1 [Reference] | NA |
| Willing TTO × P-QOLh | 2.45 (0.06) [2.32 to 2.57] | <.001 |
| Constant | 1.00 (0.00) [0.10 to 1.00] | <.001 |
| SGg | ||
| Willing SG | −0.09 (0.01) [−0.11 to −0.07] | <.001 |
| QOL | −1.00 (0.02) [−1.04 to −0.96] | <.001 |
| Unwilling SG × P-QOLh | 1 [Reference] | NA |
| Willing SG × P-QOLh | 1.71 (0.04) [1.64 to 1.79] | <.001 |
| Constant | 1.00 (0.00) [0.99 to 1.01] | <.001 |
| BC-WTP | ||
| Severity | 0.19 (0.01) [0.17 to 0.22] | <.001 |
| Attractiveness | −0.06 (0.01) [−0.08 to −0.03] | <.001 |
| Observer not perceiving paralysis | −23.17 (0.77) [−24.67 to −21.67] | <.001 |
| P-QOL | −20.07 (1.95) [−23.88 to −16.26] | <.001 |
| Constant | 31.59 (1.00) [29.63 to 33.56] | <.001 |
| Random Effectsi | ||
| Observer variance | ||
| Severity | 53.98 (6.81) [42.16 to 69.12] | NA |
| Attractiveness | 64.88 (5.14) [55.55 to 75.79] | NA |
| Residual variance | ||
| P-QOL | 0.02 (0.00) [0.02 to 0.02] | NA |
| QOL VAS | 0.03 (0.00) [(0.03 to 0.03] | NA |
| TTO | 0.004 (0.000) [0.004 to 0.004] | NA |
| SG | 0.014 (0.000) [0.013 to 0.015] | NA |
| WTP | 127.35 (3.51) [120.66 to 134.42] | NA |
| Severity | 310.35 (8.93) [293.32 to 328.36] | NA |
| Attractiveness | 188.95 (5.37) [178.71 to 199.78] | NA |
| Affect | 344.07 (9.26) [326.40 to 362.71] | NA |
| Probit Model | ||
| Observer not perceiving paralysis | ||
| Severity | −0.36 (0.03) [−0.42 to −0.29] | <.001 |
| Constant | 2.70 (0.17) [2.37 to 3.03] | <.001 |
| TTO observer willingnessf | ||
| Severity | 0.03 (0.00) [0.03 to 0.04] | <.001 |
| Constant | −1.92 (0.06) [−2.03 to −1.81] | <.001 |
| SG observer willingnessf | ||
| Severity | 0.04 (0.00) [0.04 to 0.05] | <.001 |
| Constant | −1.54 (−0.05)[−1.64 to −1.45] | <.001 |
| Tetrachoric correlation | ||
| Willing TTO, perceiving paralysis | −0.79 (0.06) [−0.88 to −0.64] | <.001 |
| Willing SG, perceiving paralysis | −0.83 (0.05) [−0.90 to −0.71] | <.001 |
| Willing SG, willing TTO | 0.63 (0.34) [0.56 to 0.69] | <.001 |
Abbreviations: BC-WTP, Box-Cox willingness to pay; NA, not applicable; P-QOL, perceived quality of life latent variable; SG, standard gamble; TTO, time trade-off; VAS, visual analog scale; WTP, willingness to pay.
Scored on a fixed-effects scale ranging from 0 to 100, with higher scores indicating greater severity.
Defined as House-Brackmann grade 2.
Defined as House-Brackmann grades 3 and 4.
Defined as House-Brackmann grades 5 and 6.
Facial photograph portrays individual smiling vs in repose.
Scored on a fixed-effects scale ranging from 0 to 100, with higher scores indicating greater attractiveness.
Scored on a fixed-effects scale ranging from 0 to 1.00, with higher scores indicating better health or no paralysis.
Represents interaction between covariates (ie, participants not willing and willing to trade time off their lives and their perception of the photographed individual’s QOL).
Data are expressed as estimates.
Willingness-to-Pay
Figure 2 plots the mixed-effects regression equation for societal WTP to restore a face to normal as a function of perceived severity, with corresponding House-Brackmann categories marked on the severity scale. The WTP to repair facial paralysis increases nonlinearly with severity (P = .005), ranging from $3487 (95% CI, $2362–$4961) to repair low-grade paralysis to $8571 (95% CI, $6401–$11 234) to repair medium-grade paralysis and $20 431 (95% CI, $16 273–$25 317) to repair high-grade paralysis.
Figure 2. Willingness to Pay (WTP) vs Paralysis Severity Scale.
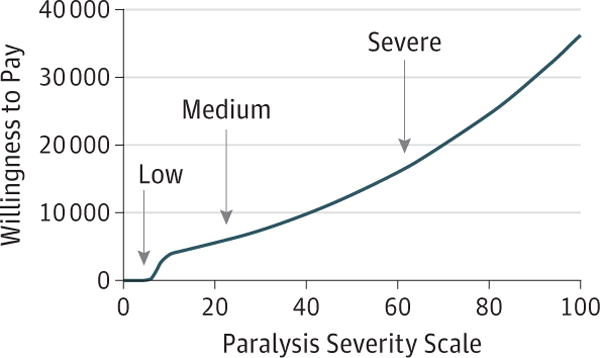
Graph represents the mean WTP to repair facial paralysis by increasing perceived severity scores. Mean perceived severity scores of reposed faces with low-, medium-, and high-grade paralysis are marked accordingly on the scale (low-grade paralysis, 3.92; medium-grade paralysis, 23.32; and high-grade paralysis, 60.95).
Health Utility
The mean (SD) of health utility values by paralysis severity and by the calculation method (SG, TTO, and VAS) are shown in Table 3. By all 3 methods, health utility values decreased with increasing House-Brackmann severity grade. A health utility value of 0 is defined as death and 1.00 is defined as perfect health or no facial paralysis. From low- to high-grade paralysis, health utility values ranged from 0.98 to 0.77, 0.98 to 0.74, and 0.92 to 0.43 using the SG, TTO, and VAS methods, respectively.
Table 3.
WTP, Health State Utility, and WTP:QALY Ratios by Facial Paralysis Severity
| Measurement | Normala | Grade of Paralysis | ||
|---|---|---|---|---|
| Lowb | Mediumc | Highd | ||
| WTP, Mean (95% CI), $ | 1980 (1233–3014) |
3487 (2362–4961) |
8571 (6401–11 234) |
20 431 (16 273–25 317) |
| Health utility value, mean (SD) | ||||
| SG | 1.00 (0.19) | 0.98 (0.09) | 0.93 (0.15) | 0.77 (0.25) |
| TTO | 1.00 (0.03) | 0.98 (0.11) | 0.92 (0.21) | 0.74 (0.30) |
| VAS | 0.99 (0.18) | 0.92 (0.18) | 0.76 (0.21) | 0.43 (0.21) |
| WTP:QALY, mean (SD), $ | ||||
| SG | 6353 (5479) | 10 167 (14 565) | 16 277 (28 327) | 17 008 (38 288) |
| TTO | 7822 (7388) | 14 988 (28 396) | 12 680 (31 732) | 13 065 (41 953) |
| VAS | 1458 (1877) | 1349 (2055) | 2072 (3553) | 2266 (2890) |
Abbreviations: SG, standard gamble; TTO, time trade-off; VAS, visual analog scale; WTP, willingness to pay; WTP:QALY, WTP per quality-adjusted life-year.
Indicates values for normal faces that participants mistook as having mild paralysis. Actual normal faces were cost averaged to near zero, as seen in Figure 2.
Defined as House-Brackmann grade 2.
Defined as House-Brackmann grades 3 and 4.
Defined as House-Brackmann grades 5 and 6.
Valuation
Using the health utility values calculated, we derived WTP: QALY ratios for normal faces and faces with varying degrees of paralysis severity. The WTP:QALY values are shown in Table 3. Mean (SD) WTP:QALY ratios calculated from SG ranged from $10 167 ($14 565) to $17 008 ($38 288) for low- to high-grade paralysis.
Discussion
This study is the first, to our knowledge, to measure (1) WTP to repair varying degrees of facial paralysis, (2) the health utility of varying degrees of facial paralysis, and (3) the subsequent value of facial reanimation surgery, all as perceived by society. We measured WTP to repair different degrees of facial paralysis and found that WTP increased nonlinearly with perceived severity and House-Brackmann grade (Figure 2). This finding suggests that individuals with high-grade paralysis endure a much greater perception penalty than those with low-grade paralysis. This finding has important implications for the effective use of health care resources, demonstrating that societal members are willing to reserve a much greater proportion of resources for the most severe paralyses.
In addition, some participants mistook normal faces to have paralysis, and the mean WTP for those faces was measured at $1980 (95% CI, $1233–$3014) (Table 3). This mistake may be attributable to the phenomenon that a specific level of facial asymmetry must exist before one can accurately identify paralysis, and observers may find it difficult to perceive differences between a normal face (House-Brackmann grade 1) and low-grade facial paralysis (House-Brackmann grade 2).29
This study also highlights the importance of WTP as a measure of the association between societal perception and intrinsic characteristics of a disease state. Economists have argued for the equivalence of economic benefit with WTP, stating that WTP is actually a measure of human preference.30 We posit that, with respect to disease states, WTP can be used as an indication of the importance to society of repairing a condition and thus a signal of the intrinsic severity of the condition. We hope that this study lays groundwork for future investigations to use WTP as an objective scale of facial perception and highlights the importance of the wisdom of crowds in understanding value.
Previous literature showed that, depending on the health utility method used (SG, TTO, or VAS), the resultant QALY and thus WTP:QALY ratio calculated for the same condition may differ.16 Owing to the lack of a criterion standard, we calculated health utilities using all 3 methods. Our results demonstrated results similar to those of previous research, in which SG and TTO health utility values were extremely comparable and in which VAS exaggerated a decrease in health utility with increasing severity of paralysis.10 This result is likely owing to an alteration in risk-taking behavior when years of life and the risk for death are at stake. Regardless of the method used, perceived health utility measurements decreased with increasing paralysis grade. These data show that society believes facial paralysis decreases QOL. Because one’s health utility state is strongly influenced by a community’s response to one’s appearance, this objective measurement of society’s perception of health utility may explain why patients with facial paralysis live with significant QOL morbidity.1,31
The WTP:QALY ratios for low-, medium-, and high-grade paralysis demonstrated society’s perceived value of repairing facial paralysis. The WTP:QALY ratios ranged from $10 167 to $17 008 from low- to high-grade paralysis using the SG method. In health care economics, various thresholds are used to determine whether interventions are cost-effective, and WTP:QALY ratios have been shown to be an even more conservative estimation of value than these thresholds.10
Although this study was not a formal cost-effectiveness analysis, comparing the WTP:QALY values we derived with formal cost-effectiveness analysis thresholds yields interesting insights. For example, a widely cited cost-effectiveness threshold value is less than $50 000 per QALY proposed by Kaplan and Bush32 in 1982, although this value is not adjusted for inflation. Laupacis et al33 have since proposed 3 tiers of threshold values to rank whether an intervention has strong, moderate, or weak evidence for adoption. After adjusting for inflation and currency exchange rates in 2003 US dollars, these values are less than $23 400 per QALY (strong evidence), $23 400 per QALY to $116 800 per QALY (medium evidence), and greater than $116 800 per QALY (weak evidence).10 The calculated societal perceived WTP:QALY values in this study were well below all of these cost-effectiveness thresholds, indicating that society perceives facial reanimation surgery to be a high-value intervention.
Finally, we used an SEM to analyze the nuanced associations among the domains of facial perception, perceived QOL, and health utility and economic values. The association between facial perception domains and the resultant WTP and health utility values is directly mediated through a latent variable of P-QOL. This process is significant because although P-QOL is a theoretical variable that cannot be measured directly, we hope to have laid groundwork for future studies to use other metrics as a proxy for how societal members regard a disease state. The association between facial perception domains and P-QOL is supported by previous studies,34–36 which have shown that attractive individuals are more likely to have higher self-esteem, be perceived as more intellectual and competent, and achieve higher measures of psychological well-being. Conversely, individuals with facial disfigurement endure societal discrimination, higher rates of depression, and long-term negative psychological effects.37,38
Limitations
This study explored WTP, health utility, and value from a societal perspective, but we have yet to explore these metrics from a patient perspective. Societal perception of the disease state of facial paralysis could contrast with patient self-ratings of QOL and the actual costs of reanimation surgery. Therefore, this study cannot be used as a formal cost-effectiveness analysis. Depending on the illness, casual observers may underestimate or overestimate the effect of an illness.16
Static images were used in the surveys, which may not allow participants to appreciate the full limitations of facial paralysis. The use of videos may be helpful for viewers to understand the effect facial paralysis has on speech and facial motion.
The measurement of societal WTP also carries some important considerations. First, the existence of a third-party payer system in the United States means that individuals rarely recognize the full cost of interventions. Even if they do, insured individuals often do not pay the full cost of health care services out of pocket, which would influence their WTP for repairing a hypothetical disease state. As such, this study may instead reflect individuals’ willingness to co-pay.39 Finally, although income data were included in our demographic survey, income strata were not included in the SEM owing to the large magnitude of tested variables; previous studies have shown that participants’ income levels influence WTP for repair of medical conditions.10
Conclusions
Society perceives facial reanimation surgery to be a high-value intervention in repairing facial paralysis. Facial paralysis is perceived to decrease QOL, with the greatest penalties associated with the most severe grades of paralysis. Societal WTP also increases nonlinearly with increasing House-Brackmann grade, which may guide the pursuit of high-value care in the field of facial plastics. This study also begins to establish WTP as an objective measure of facial perception and intrinsic disease severity.
Key Points.
Question
What value does society place on reconstructive surgery for facial paralysis?
Findings
In this prospective observational study of 348 naive participants, reconstructive surgery for facial paralysis was found to be of high value, with willingness to pay for reconstructive surgery increasing as House-Brackmann grade of severity of paralysis increased.
Meaning
Willingness to pay may be a useful objective measure to inform questions of disease severity and the value of normal facial function.
Footnotes
Author Contributions: Ms Su and Dr M. Ishii had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Su, L. E. Ishii, Joseph, Nellis, Dey, Bater, Boahene, M. Ishii.
Acquisition, analysis, or interpretation of data: Su, L. E. Ishii, Joseph, Nellis, Dey, Byrne, M. Ishii.
Drafting of the manuscript: Su, L. E. Ishii, Joseph, Boahene, M. Ishii.
Critical revision of the manuscript for important intellectual content: Su, L. E. Ishii, Joseph, Nellis, Dey, Bater, Byrne.
Statistical analysis: Su, L. E. Ishii, Joseph, Bater, M. Ishii.
Administrative, technical, or material support: Su, Joseph, Nellis, Dey, Bater, Byrne, M. Ishii.
Study supervision: Su, L. E. Ishii, Byrne, Boahene, M. Ishii.
Conflict of Interest Disclosures: None reported.
Previous Presentation: This paper was presented at the American Academy of Facial Plastic and Reconstructive Surgery meeting; May 20, 2016; Chicago, Illinois.
References
- 1.Coulson SE, O’Dwyer NJ, Adams RD, Croxson GR. Expression of emotion and quality of life after facial nerve paralysis. Otol Neurotol. 2004;25(6):1014–1019. doi: 10.1097/00129492-200411000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Ishii L, Godoy A, Encarnacion CO, Byrne PJ, Boahene KD, Ishii M. Not just another face in the crowd: society’s perceptions of facial paralysis. Laryngoscope. 2012;122(3):533–538. doi: 10.1002/lary.22481. [DOI] [PubMed] [Google Scholar]
- 3.Kleiss IJ, Hohman MH, Susarla SM, Marres HA, Hadlock TA. Health-related quality of life in 794 patients with a peripheral facial palsy using the FaCE Scale: a retrospective cohort study. Clin Otolaryngol. 2015;40(6):651–656. doi: 10.1111/coa.12434. [DOI] [PubMed] [Google Scholar]
- 4.Godoy A, Ishii M, Dey J, Boahene KD, Byrne PJ, Ishii LE. Facial lesions negatively impact affect display. Otolaryngol Head Neck Surg. 2013;149(3):377–383. doi: 10.1177/0194599813490887. [DOI] [PubMed] [Google Scholar]
- 5.Bhama PK, Hadlock TA. Contemporary facial reanimation. Facial Plast Surg. 2014;30(2):145–151. doi: 10.1055/s-0034-1371900. [DOI] [PubMed] [Google Scholar]
- 6.Chan JY, Byrne PJ. Management of facial paralysis in the 21st century. Facial Plast Surg. 2011;27(4):346–357. doi: 10.1055/s-0031-1283053. [DOI] [PubMed] [Google Scholar]
- 7.Ishii LE. Moving toward objective measurement of facial deformities: exploring a third domain of social perception. JAMA Facial Plast Surg. 2015;17(3):189–190. doi: 10.1001/jamafacial.2015.36. [DOI] [PubMed] [Google Scholar]
- 8.Surowiecki J. The Wisdom of Crowds. New York, NY: Anchor Books; 2004. [Google Scholar]
- 9.Hadlock T. Standard outcome measures in facial paralysis: getting on the same page. JAMA Facial Plast Surg. 2016;18(2):85–86. doi: 10.1001/jamafacial.2015.2095. [DOI] [PubMed] [Google Scholar]
- 10.King JT, Jr, Tsevat J, Lave JR, Roberts MS. Willingness to pay for a quality-adjusted life year: implications for societal health care resource allocation. Med Decis Making. 2005;25(6):667–677. doi: 10.1177/0272989X05282640. [DOI] [PubMed] [Google Scholar]
- 11.Hirth RA, Chernew ME, Miller E, Fendrick AM, Weissert WG. Willingness to pay for a quality-adjusted life year: in search of a standard. Med Decis Making. 2000;20(3):332–342. doi: 10.1177/0272989X0002000310. [DOI] [PubMed] [Google Scholar]
- 12.Zillich AJ, Blumenschein K, Johannesson M, Freeman P. Assessment of the relationship between measures of disease severity, quality of life, and willingness to pay in asthma. Pharmacoeconomics. 2002;20(4):257–265. doi: 10.2165/00019053-200220040-00004. [DOI] [PubMed] [Google Scholar]
- 13.Von Neumann J, Morgenstern O. Theory of Games and Economic behavior. 3rd. Princeton, NJ: Princeton University Press; 1953. [Google Scholar]
- 14.Torrance GW, Thomas WH, Sackett DL. A utility maximization model for evaluation of health care programs. Health Serv Res. 1972;7(2):118–133. [PMC free article] [PubMed] [Google Scholar]
- 15.Streiner D, Norman G. Health Measurement Scales: A Practical Guide to Their Development and Use. New York, NY: Oxford University Press; 1989. [Google Scholar]
- 16.Byrne MM, O’malley K, Suarez-Almazor ME. Willingness to pay per quality-adjusted life year in a study of knee osteoarthritis. Med Decis Making. 2005;25(6):655–666. doi: 10.1177/0272989X05282638. [DOI] [PubMed] [Google Scholar]
- 17.Dey JK, Ishii LE, Joseph AW, et al. The cost of facial deformity: a health utility and valuation study. JAMA Facial Plast Surg. 2016;18(4):241–249. doi: 10.1001/jamafacial.2015.2365. [DOI] [PubMed] [Google Scholar]
- 18.Sinno H, Thibaudeau S, Izadpanah A, et al. Utility outcome scores for unilateral facial paralysis. Ann Plast Surg. 2012;69(4):435–438. doi: 10.1097/SAP.0b013e318246e698. [DOI] [PubMed] [Google Scholar]
- 19.Dey JK, Ishii LE, Byrne PJ, Boahene KD, Ishii M. Seeing is believing: objectively evaluating the impact of facial reanimation surgery on social perception. Laryngoscope. 2014;124(11):2489–2497. doi: 10.1002/lary.24801. [DOI] [PubMed] [Google Scholar]
- 20.Dey JK, Ishii M, Boahene KD, Byrne PJ, Ishii LE. Facial reanimation surgery restores affect display. Otol Neurotol. 2014;35(1):182–187. doi: 10.1097/MAO.0b013e3182a1ea8a. [DOI] [PubMed] [Google Scholar]
- 21.Dey JK, Ishii M, Boahene KD, Byrne PJ, Ishii LE. Changing perception: facial reanimation surgery improves attractiveness and decreases negative facial perception. Laryngoscope. 2014;124(1):84–90. doi: 10.1002/lary.24262. [DOI] [PubMed] [Google Scholar]
- 22.Nakano T, Tanaka K, Endo Y, et al. Atypical gaze patterns in children and adults with autism spectrum disorders dissociated from developmental changes in gaze behaviour. Proc Biol Sci. 2010;277(1696):2935–2943. doi: 10.1098/rspb.2010.0587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Manor BR, Gordon E, Williams LM, et al. Eye movements reflect impaired face processing in patients with schizophrenia. Biol Psychiatry. 1999;46(7):963–969. doi: 10.1016/s0006-3223(99)00038-4. [DOI] [PubMed] [Google Scholar]
- 24.Derogatis LR, Rutigliano PJ. The Derogatis Affects Balance Scale DABS. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia, PA: Lippincott-Raven; 1996. pp. 107–118. [Google Scholar]
- 25.Murthy JM, Saxena AB. Bell’s palsy: treatment guidelines. Ann Indian Acad Neurol. 2011;14(suppl 1):S70–S72. doi: 10.4103/0972-2327.83092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qualtrics [computer program] Provo, UT: Qualtrics; 2015. [Google Scholar]
- 27.Arias E. United States life tables, 2010. Natl Vital Stat Rep. 2014;63(7):1–63. [PubMed] [Google Scholar]
- 28.DeNavas-Walt C, Protor BD. Income and poverty in the United States. 2014 http://www.census.gov/content/dam/Census/library/publications/2015/demo/p60-252.pdf. Issued September 2015. Accessed November 1, 2015.
- 29.Chu EA, Farrag TY, Ishii LE, Byrne PJ. Threshold of visual perception of facial asymmetry in a facial paralysis model. Arch Facial Plast Surg. 2011;13(1):14–19. doi: 10.1001/archfacial.2010.101. [DOI] [PubMed] [Google Scholar]
- 30.Pearce D. Cost-benefit analysis and environmental policy. Oxf Rev Econ Policy. 1998;14(4):84–106. [Google Scholar]
- 31.Ryzenman JM, Pensak ML, Tew JM., Jr Facial paralysis and surgical rehabilitation: a quality of life analysis in a cohort of 1,595 patients after acoustic neuroma surgery. Otol Neurotol. 2005;26(3):516–521. doi: 10.1097/01.mao.0000169786.22707.12. [DOI] [PubMed] [Google Scholar]
- 32.Kaplan RM, Bush JW. Health-related quality of life measurement for evaluation research and policy analysis. Health Psychol. 1982;1(1):61–80. [Google Scholar]
- 33.Laupacis A, Feeny D, Detsky AS, Tugwell PX. How attractive does a new technology have to be to warrant adoption and utilization? tentative guidelines for using clinical and economic evaluations. CMAJ. 1992;146(4):473–481. [PMC free article] [PubMed] [Google Scholar]
- 34.Jackson LA. Physical attractiveness: a sociocultural perspective. In: Cash TF, Pruzinsky T, editors. Body Image: A Handbook of Theory, Research, and Clinical Practice. New York, NY: Guilford Press; 2002. pp. 13–21. [Google Scholar]
- 35.Jackson LA, Hunter JE, Hodge CN. Physical attractiveness and intellectual competence: a meta-analytic review. Soc Psychol Q. 1995;58(2):108–122. [Google Scholar]
- 36.Umberson D, Hughes M. The impact of physical attractiveness on achievement and psychological well-being. Soc Psychol Q. 1987;50(3):227–236. [Google Scholar]
- 37.Valente SM. Visual disfigurement and depression. Plast Surg Nurs. 2009;29(1):10–16. doi: 10.1097/01.PSN.0000347718.75285.23. [DOI] [PubMed] [Google Scholar]
- 38.Versnel SL, Plomp RG, Passchier J, Duivenvoorden HJ, Mathijssen IM. Long-term psychological functioning of adults with severe congenital facial disfigurement. Plast Reconstr Surg. 2012;129(1):110–117. doi: 10.1097/PRS.0b013e3182361f64. [DOI] [PubMed] [Google Scholar]
- 39.Brenner MJ. What cost-utility analysis can teach us about facial deformity: gambles, trade-offs, and willingness to pay. JAMA Facial Plast Surg. 2016;18(4):249–250. doi: 10.1001/jamafacial.2016.0044. [DOI] [PubMed] [Google Scholar]


