Abstract
The activPAL™ (AP) monitor is well established for distinguishing sitting, standing and stepping time. However, its validity in predicting time in physical activity intensity categories in a free-living environment has not been determined.
Purpose
To determine the validity of the AP in estimating time spent in sedentary, light and moderate-to-vigorous physical activity (MVPA) in a free-living environment.
Methods
Thirteen participants (mean (SD) age 24.8 y (5.2), BMI 23.8 kg.m2 (1.9)) were directly observed (DO) for three 10-hr periods wearing an AP. A custom R program was developed and used to summarize detailed active and sedentary behavior variables from the AP. AP estimates were compared to DO.
Results
The AP accurately and precisely estimated time in activity intensity categories (bias (95% CI) sedentary = 0.8 min (−2.9, 4.5), light = 1.7 min (2.2, 5.7) and −2.6 min (−5.8, 0.7)). The overall accuracy rate for time in intensity categories was 96.2%. The AP also accurately estimated guideline minutes, guideline bouts, prolonged sitting minutes and prolonged sitting bouts.
Conclusion
The AP can be used to accurately capture individualized estimates of active and sedentary behavior variables in free-living settings.
Keywords: physical activity and sedentary behavior measurement, validity, accelerometers
Introduction
The activPAL™ (AP) activity monitor is a small device worn on the thigh that uses information about static and dynamic acceleration to 1) distinguish body posture as sitting/lying, standing and stepping and 2) estimate energy expenditure (EE) (expressed as metabolic equivalents (METs)) (34). A unique feature of the AP is that it is worn on the anterior midline of the thigh versus the hip or wrist like most other accelerometry-based activity monitors. The thigh sensor location provides rich information about body posture and transitions between postures. This allows the AP to summarize behavior in terms of “events” (i.e., changes in posture). Numerous validation studies report the accuracy of the AP to distinguish sitting/lying, standing and stepping and features of sedentary behavior (SB) including time-spent sitting/lying and breaks from sitting/lying (2, 6, 16, 18, 27, 30, 36). These reports include both laboratory and free-living settings and diverse samples (e.g. toddlers to the elderly, men and women, lean and overweight, healthy and diseased, able-bodied and physical handicapped). However little work has been done to test the validity of the AP to estimate METs. If the AP can accurately estimate METs, it could be used to determine time spent in different physical activity intensity categories (i.e., sedentary, light, moderate-to-vigorous) and combined with its events-based measurement approach, will provide more detailed information about patterns of both active and sedentary behaviors over the entire 24-hour activity/sleep cycle (5, 7, 9, 12, 17).
To our knowledge, no study has tested the validity of EE outputs from the activPAL™ activity monitor to categorize behavior as sedentary, light or moderate-to-vigorous (MVPA) and only one study has tested the validity of the AP to produce point estimates of EE. In a young (15–25 years old), healthy sample of females, Harrington et al. (2011) used indirect calorimetry and a standard treadmill protocol (3.2 to 7.0 km.h−1) to test the validity of the AP point estimates of METs during stepping (20). The authors reported a significant overestimation of METs during lower intensity stepping (3.2 and 4.8 km.h−1) and a significant underestimation of METs during higher intensity stepping (jogging) (5.6, 6.4 and 7.0 km.h−1). These results suggest the AP is not ideal for estimating METs during free-living physical activity. However, the validity of the AP and its associated software to categorize activity intensity as sedentary (<1.5 METs), light (1.5–2.99 METs) or MVPA (≥ 3 METs) has not been tested. Given that: 1) most other accelerometer-based activity monitors do not produce accurate point estimates of EE across a range of activities, but do perform reasonably well at estimating EE within a given range (e.g. moderate-to-vigorous intensity) and 2) most intervention and surveillance researchers are primarily interested in estimating time spent in physical activity intensity categories, it is beneficial to test the validity of the AP to categorize activity as sedentary, light or MVPA. If the AP accurately estimates physical activity intensity categories, this would allow researchers to use one device to accurately measure both active and sedentary behaviors in the field.
Despite the AP capturing rich accelerometer data, its corresponding software is limited. Currently, it does not provide a mechanism to perform batch processing of multiple participant files, nor does it allow extraction of all of the detailed information about behavior that is captured by the device. When data are downloaded from the device and processed in the AP software, informative illustrations of participant behavior and some summary statistics are displayed. However, more information can be extracted from the continuous activity logs (i.e. 15-second epoch and events files) that are automatically generated by the software. These files can be exported as .csv files and further processed in an independent statistical environment, such as R, to provide more information about the pattern and duration of behaviors.
The primary purpose of this study was to address these limitations by first testing the validity of the EE outputs from the AP to classify behavior into sedentary (<1.5 METs), light (1.5–2.99 METs) and MVPA (≥ 3 METs) intensity categories during free-living behavior. Second, we provide a custom R package to extract detailed features of sedentary and active behavior from the AP “events” file (32).
Methods
Recruitment and Eligibility
Thirteen participants (5 males, 8 females) were recruited from the surrounding community. Eligible participants were 18–60 years of age and in good physical health (no diagnosed cardiovascular, pulmonary, metabolic, joint, or chronic diseases). All participants completed a health history questionnaire and an informed consent document approved by the University of Massachusetts Institutional Review Board. Following the consenting process, height (to the nearest 0.1 cm) and weight (to the nearest 0.1kg) were measured using a floor scale/stadiometer (Detecto; Webb City, MO).
Experimental Procedures
Direct observation (DO) served as the criterion. DO allowed for the criterion validation of sedentary, standing and total activity time and concurrent validation of time spent in activity intensity categories.
Participants were directly observed in their free-living environment on three separate days. Each day the observation period lasted for approximately ten consecutive hours, resulting in ~30 hours of observation for each participant. Participants were met by a trained observer in their natural environment (e.g. home, place of work, school) and observed for approximately ten consecutive hours. Observers worked in 2–4 hour shifts and a total of three different observers completed all of the observation sessions. A hand-held personal digital assistant (PDA) (Noldus Information Technology; Netherlands) was used to record participant behavior (activity type, intensity and duration). Every time behavior changed (e.g. sitting to standing) the observer recorded the new activity type and intensity in the PDA. Each entry was time stamped and the length of each behavior bout was automatically recorded in the PDA. During the ten hour observation time, subjects were allowed to have “private time” when needed and these data were removed from the AP file. Reasons for “private time” included behaviors such as using the restroom and changing clothes. A log of the start and stop of each behavior was exported to a text file from the PDA using custom software (Noldus: Observer 9.0). These data were used to determine criterion measures of all variables.
The development of our DO method has been described in detail previously and has been validated compared to indirect calorimetry (27, 28, 31). A study from our laboratory showed that DO estimates of activity intensity were highly correlated with indirect calorimetry (low intensity: intraclass correlation (ICC) = 0.99, MVPA: ICC = 0.99) and had a small bias (low intensity: percent bias = 2.1%, MVPA: percent bias = −4.9 %) (29).
Three observers completed extensive verbal, written and video training and testing before observing participants in a free-living environment. Upon completion of training, each observer was tested in the identification of activity type (e.g. sit, stand, walk) and intensity (e.g. 3 METs) using a ~15 minute video of free-living behavior. The video was first coded by a group of experienced observers. Study observer responses (activity type and MET value) were compared with the experienced observers’ responses using a Cohen’s kappa coefficient (κ). To be considered “in agreement” study observers needed to correctly identify both the type and intensity of the activity. There was a very high level of agreement between the study observer responses and the experienced observer responses (mean κ = 0.92).
Participants wore the AP on the midline of their right thigh, one-third of the way between the hip and knee. The AP was programmed to collect data according to manufacturer settings, however before processing we used the advanced options feature within the AP software to adjust the MET value assigned to standing events from 1.4 (default value) to 1.5 METs. According to the Compendium of Physical Activities the standing MET value is 1.3 METs, standing and fidgeting is 1.8 METs and standing during household activities (e.g., ironing, washing dishes, laundry) ≥ 1.8 METs (1). In the current study, we observed that most standing events included minimal movement of the upper body and/or shuffling steps, thus we increased the standing MET value only slightly from 1.4 to 1.5 METs. The AP default MET values for sitting/lying and stepping events were used. METs for sitting/lying were 1.2 and for stepping events, the internal AP algorithm, which is a cadence-based linear regression (34), was used to estimate METs. The time-stamped “event” data file from the AP software (version 5.8.5) was then exported as a .csv file for further cleaning and analysis in R.
Data Cleaning and Reduction
For an observation to be included in the analyses valid DO and AP data were required. Additionally, behavior coded as “private” by the observer along with the corresponding AP data were eliminated from analyses. To determine total time spent in activity intensity categories, we used a customized R program to first extrapolate AP events files to a second-by-second (i.e. 1-second epochs) data file. We then summed sitting/lying epochs less than 1.5 METs (sedentary), standing and stepping epochs 1.5–2.99 (light) and stepping epochs greater than 2.99 (MVPA). In recent years, the research community has become increasingly interested in understanding how patterns of active and sedentary behavior are associated with health, thus we also estimated and validated guideline minutes, guideline bouts, and prolonged sedentary bouts. In the current paper, guideline minutes and bouts are based on the US Department of Health and Human Services physical activity guidelines recommendations and are defined as the duration and number of MVPA bouts that last at least ten consecutive minutes, respectively. Prolonged sedentary bouts are defined as uninterrupted sedentary time that lasted at least 30 or 60 minutes in duration.
R Package
R is an open-source computing language and statistics package available at www.r-project.org (38). A custom R package was developed to extract the following PA and SB variables from the events file (32). The package contains 19 functions created to help those interested in PA and SB data process and interpret data from the AP events files. Eighteen of the functions provided can be used independently (according to the user manual) and provide the user the flexibility of processing data sets as deemed appropriate for specific needs. The function process.AP uses all other functions in the package and was designed to automate AP processing for a complete data set. The function process.AP and the instruction material provided in this manuscript were designed to make processing AP data as quick and easy as possible. process.AP can be used to batch process all files within a user specified directory and produce three .csv files that summarize 1) sleep/wake time and wear/non-wear time, 2) PA and SB variables per day and 3) PA and SB variables by visit. To use process.AP, minimal R code is needed, but several data management steps are required including creating a log of subject ID’s that correspond to the AP events files to be processed. See R script (SDC 1, example code to apply R package) and Appendix I (see Document, SDC 2, R package instructions) for a complete description and step-by-step instructions.
Statistical Evaluation
Statistical evaluation was done using R software programs. To account for the lack of independence within subject, repeated measures linear mixed models were used to compare AP estimates to DO. Bias (95% CI), root mean squared error (rMSE) and intraclass correlation (ICC) two-way analysis of variance model were used to evaluate AP performance. Bland-Altman analyses were also performed.
Results
Thirteen participants (5 males, 8 females) completed the study. Participants were relatively young (mean (SD) age 24.8 y (5.2)) and lean (BMI 23.8 kg.m2 (1.9)). The AP did not record data on one occasion, resulting in a total of 360.4 h of direct observation with corresponding AP data over 38 separate sessions. Mean observed time per session was 9.5 h (0.5).
Table 1 shows the mean (95% CI) for DO and AP estimates of time in physical activity intensity categories, guideline minutes, guideline bouts, prolonged sitting minutes and prolonged sitting bouts. According to DO, participants spent 356.8 min (351.3, 362.3) sedentary, 143.8 min (139.4, 148.3) in light intensity and 68.3 min (66.2, 70.4) in MVPA per observation. The AP accurately and precisely estimated time in intensity categories (bias (95% CI) sedentary = 0.8 min (−2.9, 4.5), light = 1.7 min (2.2, 5.7) and MVPA = −2.6 min (−5.8, 0.7)) (Table 1). The AP also accurately estimated guideline minutes, guideline bouts, prolonged sitting minutes and prolonged sitting bouts (Table 1). The Bland-Altman analyses did not reveal a significant heterogeneous bias for any of the variables tested (see SDC 3–11, Bland-Altman plots; activPAL vs. Direct Observation).
Table 1.
activPAL™ performance compared to direct observation (mean (95% CI)).
| DO | AP | |
|---|---|---|
|
| ||
| MVPA (min) | 68.3 (66.2, 70.4) | 65.8 (63.9, 67.7) |
| Bias | - | −2.6 (−5.8, 0.7) |
| rMSE | - | 8.4 |
| ICC | - | 0.98 (0.95, 0.99)* |
|
| ||
| Light (min) | 143.8 (139.4, 148.3) | 145.6 (141.2, 150.0) |
| Bias | - | 1.7 (2.2, 5.7) |
| rMSE | - | 12.3 |
| ICC | - | 0.99 (0.98, 0.99)* |
|
| ||
| Sedentary (min) | 356.8 (351.3, 362.3) | 357.6 (352.1, 363.1) |
| Bias | - | 0.8 (−2.9, 4.5) |
| rMSE | - | 11.5 |
| ICC | - | 0.99 (0.99, 1.00)* |
|
| ||
| Guideline Minutes | 41.3 (39.2, 43.5) | 35.9 (33.8, 37.9) |
| Bias | - | −5.4 (−11.9, 1.0) |
| rMSE | - | 17.3 |
| ICC | - | 0.91 (0.83, 0.95)* |
|
| ||
| Guideline Bouts | 1.8 (1.8, 1.9) | 1.6 (1.5, 1.7) |
| Bias | - | −0.3 (−0.6, 0.0) |
| rMSE | - | 0.7 |
| ICC | - | 0.92 (0.84, 0.96)* |
|
| ||
| Number sedentary bouts > 30 min | 3.0 (2.9, 3.1) | 3.3 (3.2, 3.4) |
| Bias | - | 0.3 (0.0, 0.7) |
| rMSE | - | 1.0 |
| ICC | - | 0.86 (0.73, 0.93)* |
|
| ||
| Number sedentary bouts > 60 min | 0.9 (0.8, 0.9) | 0.9 (0.9, 1.0) |
| Bias | - | 0.0 (−0.3, 0.3) |
| rMSE | - | 0.6 |
| ICC | - | 0.80 (0.64, 0.89)* |
|
| ||
| Minutes sedentary bouts > 30 min | 169.6 (163.8, 175.4) | 188.8 (182.8, 194.8) |
| Bias | - | 18.0 (−9.8, 45.9) |
| rMSE | - | 65.1 |
| ICC | - | 0.84 (0.71, 0.91)* |
|
| ||
| Minutes sedentary bouts > 60 min | 79.4 (74.8, 84.1) | 86.3 (81.7, 90.9) |
| Bias | - | 5.6 (−20.9, 32.1) |
| rMSE | - | 60.2 |
| ICC | - | 0.78 (0.61, 0.88)* |
rMSE = root mean squared error, ICC = intraclass correlation coefficient.
ICC analysis revealed significant (p<0.05) agreements between DO and all AP estimates (range ICC: 0.78–0.99) (Table 1). Figures 1–3 plot AP estimates of time in sedentary, light and MVPA against DO. For all intensity categories the points (observations, N=38) fall very close to the line of identity, illustrating the high degree of accuracy.
Figure 1.
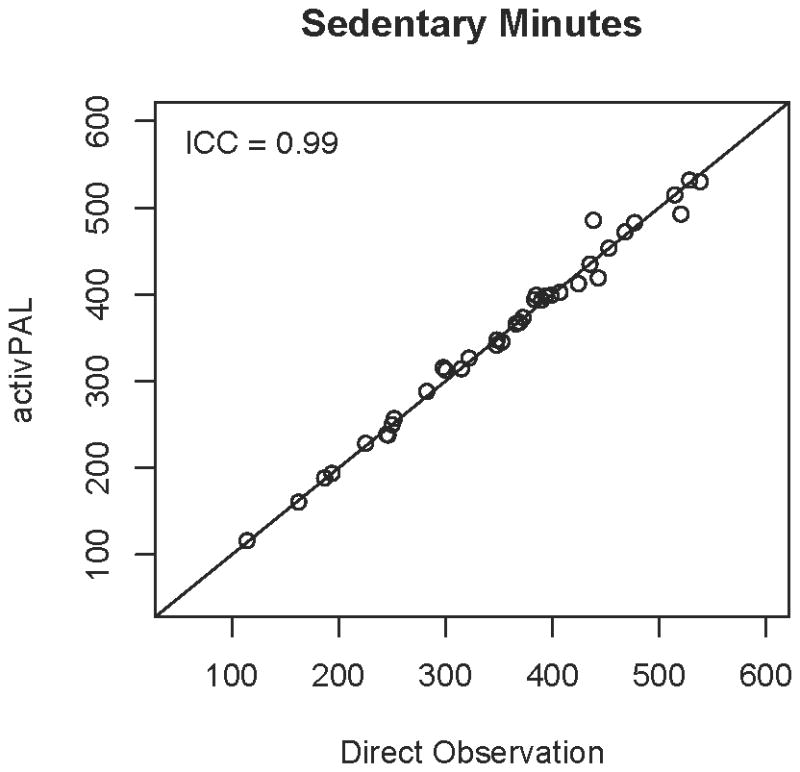
AP estimates of sedentary minutes compared to DO. Each point represents a separate DO observation session (e.g., 3 per participant). The line of identity represents the truth, thus the closer the point falls to the line, the closer the AP estimate was to DO.
Figure 3.
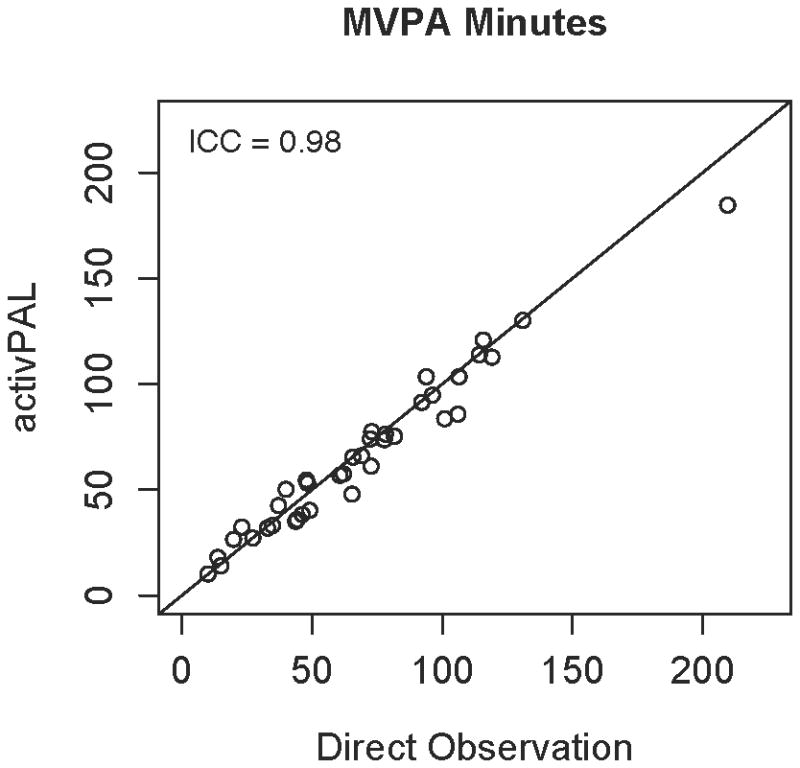
AP estimates of MVPA minutes compared to DO. Each point represents a separate DO observation session (e.g., 3 per participant). The line of identity represents the truth, thus the closer the point falls to the line, the closer the AP estimate was to DO.
Discussion
The primary finding of this study is that EE outputs from the activPAL™ activity monitor, accurately and precisely categorized behavior as sedentary, light and MVPA intensity categories in a free-living setting. This is the first study in healthy adults to demonstrate the validity of the AP to estimate time in physical activity intensity categories and to estimate novel PA and SB metrics that are important to health. Further, we observed a very high degree of accuracy across all participants and intensity categories combined (96.2%). These findings are of particular importance given that wearable accelerometers historically do not accurately estimate PA and SB across a wide range of types and intensities (3, 4, 10, 11, 29, 35, 37). Given the accumulating evidence that prolonged sedentary time is associated with adverse health risks, even among those meeting current physical activity guidelines recommendations (8, 15, 21–23, 33), it is important that a device accurately and precisely categorize both active and sedentary behaviors.
Other groups have shown interest in exploiting AP outputs for physical activity variables in addition to the sedentary and posture variables provided (13, 20, 25). One previous study tested the validity of the AP’s cadence based linear regression to produce point estimates of METs during treadmill walking and running (20). Like other commercially available accelerometers, the AP overestimated slow walking and underestimated running, however the validity of the AP to categorize intensity as sedentary, light and MVPA was not tested. Researchers from the same group then performed a calibration study to determine if AP activity counts (rather than cadence) could be used to distinguish moderate and vigorous physical activity in adolescent girls (13). These data showed that the AP could be used to classify activity intensity and researchers concluded that the AP was a valid objective monitoring device for sedentary and physical activity variables.
Results from the current study confirm that, in healthy adults, the AP is a valid tool for categorizing activity intensity across a range of activity types and intensities. Further, our results were observed in a free-living setting, where AP estimates were compared to the criterion of direct observation. This is important because other studies have shown that the validity of wearable accelerometers (and their associated data processing methods) in estimating meaningful PA and SB metrics is significantly reduced when tested in free-living environments where a range of activity types and intensities are performed in natural settings (3, 14, 19, 24, 28).
In this study we did not test the validity of the AP to distinguish moderate (3–5.99 METs) from vigorous (≥ 6 METs) intensity. The AP uses a cadence-based linear regression to estimate METs. Briefly, the model (described in detail in the AP User’s Manual) assigns a value of 4 METs to cadences of 120 steps per minute and all other cadences are scaled linearly from quiet standing (1.4 METs). Using this approach, a minimum cadence of 240 steps per minute is required for a stepping event to be categorized as vigorous. Although several individualized factors (e.g., anthropometric, gait mechanics) influence cadence, recreational runners generally select a cadence between 160–170 steps per minute, while elite runners typically select a cadence ~180–200 steps per minute. Since it is rare for even elite athletes to maintain a cadence much greater than 200 steps per minute, it is clear that the current approach is not appropriate for precisely measuring vigorous intensity activity.
We have also provided an easy to use custom R package to estimate detailed PA and SB variables (https://cran.r-project.org/web/packages/activpalProcessing/index.html) (32). The package contains 18 flexible functions that can be used on data in various forms (e.g. epoch settings). The package also contains one function that is specifically designed to process AP events files that have been converted to second-by-second data files. This function, process.AP, uses the other functions within the package to batch process all AP files within a given data set. To execute this function several data management steps must be followed, but minimal experience coding in R is required. Detailed instructions to use process.AP are provided in SDC 1 and SDC 2 (see SDC 1, example code to apply R package and SDC 2, Appendix I R package instructions). Because standard methods are not available to handle non-wear time and time spent sleeping, we have provided the user the option to use logs that identify wear/non-wear and wake/sleep periods. These logs are then used to eliminate non-wear and sleep periods from the analysis. To be used with process.AP the logs must be in a precise format and thus we provide example logs within the R package. Example logs within the R package can be exported and used as a template to create new logs (see SDC 1, example code to apply R package).
The user-friendly R package, along with the detailed instructions (see SDC 2, Appendix I R package instructions) and templates provided will be a significant contribution to the physical activity measurement community. Over the past few years measurement researchers have developed promising new methods to process accelerometer data. These methods often improve PA and SB estimates, however, their complex nature and dependence on expensive statistical software render them impractical for use by applied researchers. As a result, traditional, simple regression approaches and methods provided within device software remain the predominant choice for data processing. The AP’s wearing position on the front of the thigh combined with its events-based monitoring approach enables rich information about posture, behavior and movement to be captured by the device. These data however are currently not optimized by the AP software. The customized R package provided summarizes the postural data provided by the AP software and provides an easy method for applied researchers to extract additional data from the AP events file and summarize several important PA and SB variables. For example, the package provides more detailed information about active time (e.g., guideline minutes) and sedentary time (e.g., minutes in sedentary bouts > 30 min). These data can be used to supplement the rich postural data currently provided by the AP software, allowing for a more comprehensive analysis of active and sedentary behavior in free-living settings. Additionally, the flexible nature of R programming allows for published packages to be updated regularly, which will for additional variables and increased functionality to be incorporated into the package as the science advances.
Limitations
This study is has some limitations. First, the DO method relies on extensively trained observers to estimate intensity, rather than a direct measure such as indirect calorimetry. Thus, the validation of sedentary, standing and total activity using DO is considered criterion validity, while DO classification of intensity is convergent validity (26). However, the DO method has been shown to accurately estimate METs compared to indirect calorimetry and has the advantage of estimating immediate transitions between intensities rather than requiring time-lagged steady state estimates. The validation of our DO method was performed in a laboratory where it is impossible to capture the infinite number of activities (e.g., driving) that can be performed in truly free-living environments. Other criterion methods are possible (e.g., portable indirect calorimetry, video analysis, doubly labeled water) however each possess a unique set of limitations that must be considered when performing validations in free-living settings. Second, our validation was performed on relatively young, lean and healthy adult population. Because the AP relies on cadence to estimate EE, it is possible that the current results are not generalizable to other populations, including children and youth, older adults and clinical populations. Future research should test the validity of the AP to categorized EE outputs into sedentary and active behavior categories in these populations. Thus, researchers studying these groups should take caution when using the R package provided, as the body posture variables (i.e., sitting/lying, standing and stepping) produced have been validated in these groups but activity classification as light or MVPA has not. Third, the current manuscript does not contain a comprehensive validation of the custom R package provided. This type of validation is beyond the scope of this paper but future research should address this concern as well as continue to identify additional variables that are important to health outcomes.
Supplementary Material
Supplemental Digital Content 1: R Source (example R script)
Supplemental Digital Content 10: Bland-Altman Figure – Minutes of Sedentary Bouts >30 Minutes
Supplemental Digital Content 11: Bland-Altman Figure – Number of Sedentary Bouts >60 Minutes
Supplemental Digital Content 2: Appendix I – Step-by-step instructions on use of R package.
Supplemental Digital Content 3: Bland-Altman Figure – Sedentary Minutes
Supplemental Digital Content 4: Bland-Altman Figure – Light Minutes
Supplemental Digital Content 5: Bland-Altman Figure – MVPA Minutes
Supplemental Digital Content 6: Bland-Altman Figure – Guideline Minutes
Supplemental Digital Content 7: Bland-Altman Figure – Guideline Bouts
Supplemental Digital Content 8: Bland-Altman Figure – Number of Sedentary Bouts >30 Minutes
Supplemental Digital Content 9: Bland-Altman Figure – Number of Sedentary Bouts >60 Minutes
Figure 2.
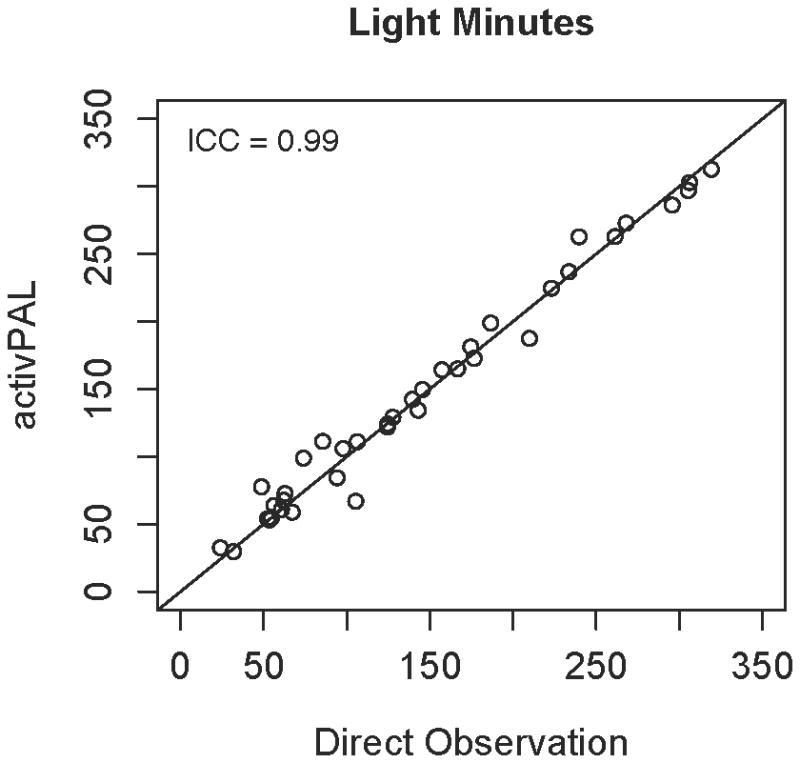
AP estimates of light minutes compared to DO. Each point represents a separate DO observation session (e.g., 3 per participant). The line of identity represents the truth, thus the closer the point falls to the line, the closer the AP estimate was to DO.
Acknowledgments
Funded by: NIH RC1HL099557 and R01 CA 121005
The authors thank Natalia Petruski and Amanda Libertine for their assistance with data collection and the subjects for their participation.
The results of the present study do not constitute endorsement by ACSM, and are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
Footnotes
Conflict of Interest: None
References
- 1.Ainsworth BEHW. Compendium of Physical Activites: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 2.Bassett DR, John D. Detection of lying down, sitting, standing, and stepping using two activPAL monitors. Med Sci Sports Exerc. 2014;46:2025–9. doi: 10.1249/MSS.0000000000000326. [DOI] [PubMed] [Google Scholar]
- 3.Bassett DR, Rowlands A, Trost SG. Calibration and validation of wearable monitors. Med Sci Sports Exerc. 2012;44:S32–8. doi: 10.1249/MSS.0b013e3182399cf7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bonomi AG, Goris AH, Yin B, Westerterp KR. Detection of type, duration, and intensity of physical activity using an accelerometer. Med Sci Sports Exerc. 2009;41:1770–7. doi: 10.1249/MSS.0b013e3181a24536. [DOI] [PubMed] [Google Scholar]
- 5.Chastin SF, Baker K, Jones D, Burn D, Granat MH, Rochester L. The pattern of habitual sedentary behavior is different in advanced Parkinson’s disease. Mov Disord. 2010;25:2114–20. doi: 10.1002/mds.23146. [DOI] [PubMed] [Google Scholar]
- 6.Chastin SF, Granat MH. Methods for objective measure, quantification and analysis of sedentary behaviour and inactivity. Gait Posture. 2010;31:82–6. doi: 10.1016/j.gaitpost.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Chastin SF, Mandrichenko O, Helbostadt JL, Skelton DA. Associations between objectively-measured sedentary behaviour and physical activity with bone mineral density in adults and older adults, the NHANES study. Bone. 2014;64:254–62. doi: 10.1016/j.bone.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 8.Chomistek AK, Manson JE, Stefanick ML, et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: results from the Women’s Health Initiative. J Am Coll Cardiol. 2013;61:2346–54. doi: 10.1016/j.jacc.2013.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clarke CL, Holdsworth RJ, Ryan CG, Granat MH. Free-living physical activity as a novel outcome measure in patients with intermittent claudication. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg. 2013;45(2):162–7. doi: 10.1016/j.ejvs.2012.11.027. [DOI] [PubMed] [Google Scholar]
- 10.Crouter SE, Churilla JR, Bassett DR. Estimating energy expenditure using accelerometers. Eur J Appl Physiol. 2006;98:601–12. doi: 10.1007/s00421-006-0307-5. [DOI] [PubMed] [Google Scholar]
- 11.Crouter SE, Clowers KG, Bassett DR. A novel method for using accelerometer data to predict energy expenditure. J Appl Physiol. 2006;100:1324–31. doi: 10.1152/japplphysiol.00818.2005. [DOI] [PubMed] [Google Scholar]
- 12.Dall PM, McCrorie PRW, Granat MH, Stansfield BW. Step accumulation per minute epoch is not the same as cadence for free-living adults. Med Sci Sports Exerc. 2013;45(10):1995–2001. doi: 10.1249/MSS.0b013e3182955780. [DOI] [PubMed] [Google Scholar]
- 13.Dowd K, Harrington D, Donnelly A. Criterion and Concurrent Validity of the activPAL™ Professional Physical Activity Monitor in Adolescent Females. PLoS One. 2012;7:10. doi: 10.1371/journal.pone.0047633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freedson P. Assessment of physical activity using wearable monitors: recommendations for monitor calibration and use in the field. Med Sci Sports Exerc. 2012;44:S1–4. doi: 10.1249/MSS.0b013e3182399b7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gennuso KP, Gangnon RE, Matthews CE, Thraen-Borowski KM, Colbert LH. Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc. 45:1493–500. doi: 10.1249/MSS.0b013e318288a1e5. 20130717 DCOM- 20140320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Godfrey A, Culhane KM, Lyons GM. Comparison of the performance of the activPAL Professional physical activity logger to a discrete accelerometer-based activity monitor. Med Eng Phys. 2007;29:930–4. doi: 10.1016/j.medengphy.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Granat M, Clarke C, Holdsworth R, Stansfield B, Dall P. Quantifying the cadence of free-living walking using event-based analysis. Gait Posture. 2015;42(1):85–90. doi: 10.1016/j.gaitpost.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 18.Grant PM, Dall PM, Mitchell SL, Granat MH. Activity-monitor accuracy in measuring step number and cadence in community-dwelling older adults. J Aging Phys Act. 2008;16:201–14. doi: 10.1123/japa.16.2.201. [DOI] [PubMed] [Google Scholar]
- 19.Gyllensten IC, Bonomi AG. Identifying types of physical activity with a single accelerometer: evaluating laboratory-trained algorithms in daily life. IEEE Trans Biomed Eng. 2011;58(9):2656–63. doi: 10.1109/TBME.2011.2160723. [DOI] [PubMed] [Google Scholar]
- 20.Harrington DM, Welk GJ, Donnelly AE. Validation of MET estimates and step measurement using the ActivPAL physical activity logger. J Sports Sci. 2011;29:627–33. doi: 10.1080/02640414.2010.549499. [DOI] [PubMed] [Google Scholar]
- 21.Healy GN, Dunstan DW, Salmon J, Shaw JE, Zimmet PZ, Owen N. Television time and continuous metabolic risk in physically active adults. Med Sci Sports Exerc. 2008;40:639–45. doi: 10.1249/MSS.0b013e3181607421. [DOI] [PubMed] [Google Scholar]
- 22.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32:590–7. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31:369–71. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 24.Intille SS, Lester J, Sallis JF, Duncan G. New horizons in sensor development. Med Sci Sports Exerc. 2012;44:S24–31. doi: 10.1249/MSS.0b013e3182399c7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Janssen X, Cliff D, Reilly J, et al. Predictive Validity and Classification Accuracy of ActiGraph Energy Expenditure Equations and Cut-Points in Young Children. J Sci Med Sport. 2013;8(11):e79124. doi: 10.1371/journal.pone.0079124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly P, Fitzsimons C, Baker G. Should we reframe how we think about physical activity and sedentary behaviour measurement? Validity and reliability reconsidered. Int J Behav Nutr Phys Act. 2016;13(32) doi: 10.1186/s12966-016-0351-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc. 2011;43:1561–7. doi: 10.1249/MSS.0b013e31820ce174. [DOI] [PubMed] [Google Scholar]
- 28.Lyden K, Keadle SK, Staudenmayer J, Freedson PS. A method to estimate free-living active and sedentary behavior from an accelerometer. Med Sci Sports Exerc. 2014;46:386–97. doi: 10.1249/MSS.0b013e3182a42a2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lyden K, Keadle SL, Staudenmeyer JW, Freedson PS. A comprehensive evaluation of commonly used accelerometer energy expenditure and MET prediction equations. Eur J Appl Physiol. 2011;111:187–201. doi: 10.1007/s00421-010-1639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lyden K, Kozey Keadle SL, Staudenmayer JW, Freedson PS. Validity of two wearable monitors to estimate breaks from sedentary time. Med Sci Sports Exerc. 2012;44:2243–52. doi: 10.1249/MSS.0b013e318260c477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lyden K, Petruski N, Staudenmayer J, Freedson P. Direct observation is a valid criterion for estimating physical activity and sedentary behavior. J Phys Act Health. 2014;11:860–3. doi: 10.1123/jpah.2012-0290. [DOI] [PubMed] [Google Scholar]
- 32.Lyden K, Staudenmayer J. Process activPAL Events Files. 2016. [Google Scholar]
- 33.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–13. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paltechnologies. Activpal Operating Guide [Internet] 2010 Available from: http://www.paltechnologies.com/
- 35.Plasqui G, Bonomi AG, Westerterp KR. Daily physical activity assessment with accelerometers: new insights and validation studies. Obes Rev. 2013;14:451–62. doi: 10.1111/obr.12021. [DOI] [PubMed] [Google Scholar]
- 36.Ryan CG, Grant PM, Tigbe WW, Granat MH. The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med. 2006;40:779–84. doi: 10.1136/bjsm.2006.027276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Staudenmayer J, Pober D, Crouter S, Bassett D, Freedson P. An artificial neural network to estimate physical activity energy expenditure and identify physical activity type from an accelerometer. J Appl Physiol. 2009;107:1300–7. doi: 10.1152/japplphysiol.00465.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Team RDC. R: A language and environment for statistical computing. 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1: R Source (example R script)
Supplemental Digital Content 10: Bland-Altman Figure – Minutes of Sedentary Bouts >30 Minutes
Supplemental Digital Content 11: Bland-Altman Figure – Number of Sedentary Bouts >60 Minutes
Supplemental Digital Content 2: Appendix I – Step-by-step instructions on use of R package.
Supplemental Digital Content 3: Bland-Altman Figure – Sedentary Minutes
Supplemental Digital Content 4: Bland-Altman Figure – Light Minutes
Supplemental Digital Content 5: Bland-Altman Figure – MVPA Minutes
Supplemental Digital Content 6: Bland-Altman Figure – Guideline Minutes
Supplemental Digital Content 7: Bland-Altman Figure – Guideline Bouts
Supplemental Digital Content 8: Bland-Altman Figure – Number of Sedentary Bouts >30 Minutes
Supplemental Digital Content 9: Bland-Altman Figure – Number of Sedentary Bouts >60 Minutes


