Abstract
Use of electronic cigarettes, devices that deliver a nicotine-containing vapor, has increased rapidly across the country and globally. Perceived and marketed as a “healthier alternative” to conventional cigarettes, few data exist regarding the safety of these devices and their efficacy in harm reduction and treatment of tobacco dependence; even less is known about their overall impact on population health. This review highlights the recent data regarding electronic cigarette toxicity, impact on lung function, and efficacy in smoking reduction and cessation. Studies show that the vapor generated from electronic cigarettes has variable amounts of nicotine and potential harmful toxins, albeit at levels lower than in conventional cigarettes. The long-term carcinogenic and lung function effects of electronic cigarettes are not known. Although some data demonstrate that electronic cigarettes may be effective in reducing conventional cigarette consumption, there are no data demonstrating the efficacy of electronic cigarettes as a tool to achieve cessation. Until robust longitudinal evaluations demonstrate the safety of electronic cigarettes and efficacy in treatment of tobacco dependence, their role as a harm reduction tool is unclear.
Keywords: e-cigarette, electronic tobacco products, smoking cessation, lung function
The 1964 landmark report by the Advisory Committee to the U.S. Surgeon General was one of the first to identify the adverse effects of cigarette smoking on health (1). Although advances have been made in diagnosis and treatment of smoking-related diseases, cigarette smoking continues to cause a massive burden of avoidable disease and premature mortality even into the 21st century (2). Although the tobacco epidemic is well entrenched in the United States and Europe, many countries are just starting to experience the toll from their own rocketing prevalence of tobacco use (3, 4). Smoking is a risk factor for six of the eight leading causes of death worldwide, including ischemic heart disease, cerebrovascular disease, lower respiratory infections, chronic obstructive pulmonary disease, tuberculosis, and lung cancer (5). There is continued evidence that successful treatment of nicotine addiction improves mortality, regardless of age at cessation (6). Data also suggest that in smokers unwilling or unable to quit, smoking reduction can improve some health outcomes and may ultimately lead to cessation (7–9). Over the last 50 years, comprehensive tobacco control programs and evidence-based treatment of tobacco dependence have demonstrated considerable, though insufficient, success at decreasing initiation of cigarette use in nonsmokers and in achieving cessation in others. Several nicotine replacement therapies with U.S. Food and Drug Administration (FDA) approval and regulation have been shown to enhance smoking reduction and cessation (10–13). These include nicotine-containing transdermal patches, nasal spray, gum, lozenges, and cigarette-shaped inhalers. Nonnicotine pharmacotherapies and psychosocial interventions are also available to improve reduction and cessation rates (4).
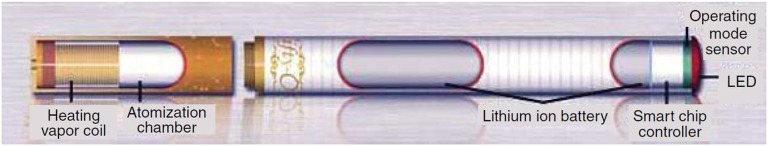
The electronic cigarette (e-cigarette) is a new class of electronic nicotine delivery system, introduced in 2004 (14–16). Distinctly different from FDA-approved nicotine inhalers, which deliver noncombusted aerosolized nicotine, absorbed in the oropharyngeal mucosa, the e-cigarette consists of a power source, electronic heating element, and liquid nicotine cartridge (Figure 1). The cartridge contains a stabilizing compound (e.g., propylene glycol or vegetable glycerin), varying amounts of nicotine, and flavoring additives. When activated by the user, the heating element atomizes the liquid, resulting in aerosolized nicotine vapor and a visible plume. This vapor is inhaled into the lungs, termed “vaping,” where nicotine is absorbed (17, 18).
Figure 1.
Schematic of an electronic cigarette. Reprinted by permission from Reference 61.
Use of e-cigarettes among U.S. middle and high school students more than doubled from 2011 to 2012 (19). Among high school students, ever use of e-cigarettes rose from 4.7 to 10.0%, with more than 1.78 million middle and high school students having tried e-cigarettes as of 2012. There is concern that electronic cigarettes may serve as a gateway to conventional cigarettes. In 2012, 20.3% of middle school, and 7.2% of high school, ever e-cigarette users reported never smoking conventional cigarettes; among current e-cigarette users, 61.1 and 80.5%, respectively, reported current conventional cigarette smoking. An estimated 160,000 students who reported ever using e-cigarettes had never smoked conventional cigarettes (20). The percentage of U.S. adult smokers trying e-cigarettes has increased similarly from 10% in 2010 to 21% in 2011 (21). International surveys show that one out of eight smokers has tried e-cigarettes, with highest use among younger, nonminority people (22). Surveys of e-cigarette users have found that they perceive e-cigarettes as a less harmful, less addictive, and healthier alternative to conventional cigarettes (22–26).
Although there is increasing evidence of e-cigarette use among youth and adults, the population health impact of e-cigarettes is unknown. Of paramount concern is the risk that their use renormalizes and reglamorizes smoking, potentially reversing decades of efforts by the public health and medical communities. In addition to the possible role of e-cigarettes in establishing nicotine addiction and as a gateway to conventional cigarettes for youth, nicotine itself has a negative impact on adolescent brain development and on development of the fetal brain, with implications for use during pregnancy (27). Because e-cigarettes are not yet widely regulated, they may help perpetuate nicotine dependence in those who smoke conventional cigarettes and decrease incentives for cessation. Kralikova and colleagues found that 28.3% of people who use e-cigarettes regularly do so because e-cigarettes are allowed in places where smoking is banned (28). Any potential benefits related to cessation or reduction of conventional cigarette smoking due to e-cigarette use by individuals could be outweighed by an overall societal increase in nicotine dependence associated with e-cigarette initiation and with a renewed acceptance of smoking in general.
Under the Family Smoking Prevention and Tobacco Control Act, the FDA Center for Tobacco Products regulates cigarettes, cigarette tobacco, and smokeless tobacco, and the FDA Center for Drug Evaluation and Research regulates smoking-related products marketed for therapeutic benefit (Table 1). Under this act, a “tobacco product” is defined in part as any product “made or derived from tobacco” that is not a “drug,” “device,” or combination product under the Federal Food, Drug, and Cosmetic Act (29). Drugs and devices are defined as articles intended to diagnosis, cure, treat or prevent disease. The case of Sottera, Inc. v FDA (627 F.3d 891, D.C. Cir 2010) challenged the FDA determination of e-cigarettes as unapproved drug/device combinations. The court held that e-cigarettes can be regulated as tobacco products and are not considered drugs or devices unless marketed for therapeutic purposes. It is anticipated that the FDA will regulate e-cigarettes as tobacco products, not as a tool for the treatment of tobacco dependence (30, 31). This is in contrast to tightly controlled nicotine replacement therapies such as nicotine patches and inhalers, which are regulated as therapies to promote tobacco cessation.
Table 1.
Tobacco regulatory roles by the United States Food and Drug Administration
| Center for Tobacco Products:
Implementation of Family Smoking Prevention and Tobacco Control
Act |
| Require disclosure of tobacco products |
| Create standards for tobacco products |
| Review premarket applications for new or modified risk tobacco products |
| Establish and enforce tobacco sales and marketing restrictions |
| Require strong health warnings on tobacco packaging |
| Center for Drug Evaluation and Research: |
| Regulate smoking-related products marketed for therapeutic benefit |
| Ensure that health benefits of therapies outweigh known risks |
| Ensure truth in advertising |
| Oversee research, development, manufacture, and marketing of drugs |
In the current unregulated environment, most of the major U.S. and European tobacco companies have invested heavily in the e-cigarette market. Additionally, many companies have arisen that exclusively produce and sell e-cigarettes, some in China, where the device was first developed, and in other international sites. Major tobacco companies have bought some of these e-cigarette companies and are spending tremendous amounts of money advertising e-cigarettes as an alternative to conventional cigarettes; one product’s advertising funds increased from $992,000 to $12.4 million from 2011 to 2012 (32, 33). In this setting, e-cigarette sales have increased from $20 million in 2008 to $500 million in 2012 and are expected to reach nearly $2 billion by the end of 2013 (34). Beyond internet, print, and television marketing, tobacco companies have worked with organizations founded to promote e-cigarette use, such as the Electronic Cigarette Association, Consumer Advocates for Smoke-Free Alternatives Association, and Vapers International, Inc (16). These groups, along with other stakeholders, have worked to delay or eliminate legislation aimed at limiting e-cigarette sale and use.
This article summarizes the current knowledge of the potential adverse effects of e-cigarettes and reviews the studies examining their efficacy as a harm reduction tool in current smokers. Electronic databases (PubMed) and internet search engines were used to identify scholarly and media articles containing key words related to electronic cigarettes (e.g., electronic cigarettes, e-cigs, vaping). This review provides guidance for clinicians in counseling patients considering or already using e-cigarettes and offers insight for governing bodies tasked with regulating these products.
Constituents of e-Cigarette Vapor
It is essential to understand the components of inhaled vapor produced by the e-cigarette atomization process, including nicotine and potential toxicants. Commercially available e-cigarettes are marketed with different levels of nicotine, and the distribution of inhaled levels remains unclear. e-Cigarettes require higher levels of suction to smoke than conventional cigarettes, and the amount and density of aerosol produced by e-cigarettes diminish progressively as puffs are taken (35). Serum levels of nicotine detected are heterogeneous and depend on the user and the device (17, 18). A study of 16 different e-cigarettes demonstrated that the total level of nicotine in 15 puffs of vapor generated by an automatic smoking machine varied from 0.5 to 15.4 mg. The typical level from one smoked conventional cigarette ranges from 1.54 to 2.60 mg (36, 37). These studies highlight the nonuniformity of nicotine delivery from e-cigarettes and the subsequent challenges in considering them as an alternative to nicotine replacement therapy.
Conventional cigarette smoke contains more than 7,000 compounds with at least 70 recognized carcinogens (1, 38, 39), including carbonyl compounds such as formaldehyde, organic compounds such as benzene, tobacco-specific nitrosamines, free radicals, toxic gases, and heavy metals (40). In 2009, the FDA detected low levels of tobacco-specific nitrosamines and diethylene glycol in two brands of commercially available e-cigarettes (41), prompting an FDA warning that e-cigarettes may pose a health risk (42). More recent studies have examined 12 brands of e-cigarettes and one nicotine inhaler for the presence of 40 toxic compounds and carcinogens (40). Among 15 carbonyl compounds tested, four were detected in e-cigarettes. Trace amounts were also detected in the nicotine inhaler. Two of 11 volatile organic compounds were detected in e-cigarettes, and none were in the nicotine inhaler. Nearly all e-cigarettes contained tobacco-specific nitrosamines not found in the nicotine inhaler. The heavy metals cadmium, nickel, and lead were detected in the e-cigarettes, with trace levels also in the nicotine inhaler. Levels of measured toxins were compared with those described previously in conventional cigarettes (Table 2). The range of toxin levels was 9-fold to 450-fold higher in smoke from conventional cigarettes than vapor from e-cigarettes. Levels of carcinogens and toxins in e-cigarettes typically exceeded those measured in an FDA-approved nicotine inhaler, suggesting that FDA-approved devices may be a safer method of nicotine delivery.
Table 2.
Comparison of toxin levels in conventional and electronic cigarettes
| Toxin | Conventional cigarette (μg/cigarette in mainstream smoke) | Electronic cigarette (μg per 15 puffs) | Average ratio (conventional:electronic) |
|---|---|---|---|
| Carbonyl compounds | |||
| formaldehyde | 1.6–52 | 0.20–5.61 | 9 |
| acetaldehyde | 52–140 | 0.11–1.36 | 450 |
| acrolein | 2.4–62 | 0.07–4.19 | 15 |
| Toluene | 8.3–70 | 0.02–0.63 | 120 |
| Nitrosamines | |||
| N′-nitrosonornicotine | 0.005–0.19 | 0.00008–0.00043 | 380 |
| NNK | 0.012–0.11 | 0.00011–0.00283 | 40 |
Definition of abbreviation: NNK = 4-(methylnitrosoamino)-1-(3-pyridyl)-1-butanone.
Adapted by permission from Reference 40.
Czogala and colleagues measured the level of nicotine and other tobacco-related toxins from vapors exhaled by e-cigarette users in an environmental chamber (43). They found that exhaled vapors generated from two 5-minute ad libitum e-cigarette uses separated by 30 minutes had a measurable nicotine level. This level was higher than background exposure but nearly 10-fold lower than that measured after smoking two conventional cigarettes in the same pattern (3.22 vs. 31.60 μg/μl, respectively; P = 0.008). Similarly, the mean aerosol particle concentration was higher with exhaled e-cigarette vapor compared with background exposure, but fivefold lower than conventional cigarette use. There was no measurable difference between background and e-cigarette volatile organic compounds.
These data demonstrate that the vapor generated from e-cigarettes contains potentially harmful compounds, although in levels much lower than observed in smoke from conventional cigarettes. Moreover, use of e-cigarettes in indoor environments may expose nonusers to increased levels of nicotine and aerosol particles. Although these data suggest that e-cigarettes may be a safer alternative to conventional cigarettes, there are no data regarding the long-term cancer risk associated with low-level exposure to the detected carcinogens.
The Impact of e-Cigarettes on Lung Function
In addition to the potential carcinogenic risk associated with e-cigarette vapor, it is important to determine the effects of e-cigarette use on lung function. The additives in the liquid nicotine cartridge (glycol derivatives) are similar to theatrical smokes and fogs (44, 45). Acute exposure to propylene glycol for 1 minute in 27 healthy subjects without asthma resulted in a 2% reduction in FEV1/FVC (P = 0.049), with a 40-ml increase in FVC (P = 0.23) and 30-ml fall in FEV1 (P = 0.29) (45). In a longitudinal study of 101 employees working at sites using theatrical fog, individuals usually working 10 feet or less from fog-generating machines had 5% reductions in adjusted FEV1 and FVC compared with those working further away (44). Although these data cannot be directly extrapolated to e-cigarette use, they highlight the potential acute and long-term effects of vapors similar to those from e-cigarettes.
In a recent study of the effects of e-cigarette vapor on lung function, in 30 healthy smokers, use of e-cigarettes for 5 minutes resulted in increased total respiratory impedance, respiratory flow resistance, and overall peripheral airway resistance (46). In addition, e-cigarette use was associated with increasing oxidative stress as measured by lower levels of the fraction of exhaled nitric oxide. Flouris and colleagues examined the acute impact of active and passive e-cigarette vapor exposure on lung function in 15 smokers and 15 never-smokers (47). They included spirometry measurements before, immediately after, and 1 hour after three exposures: room air, conventional cigarette smoke (smoking two cigarettes for smokers or exposure for 1 h in a smoke chamber for nonsmokers), and e-cigarette vapor (30 min of e-cigarette use for smokers or 1 h in vapor chamber for nonsmokers). A 7-day washout period occurred between visits. No change was detected in FEV1 or FEV1/FVC with active or passive e-cigarette exposure. Active conventional cigarette smoke exposure was associated with an acute 7.2% reduction in FEV1/FVC (P < 0.001). These two studies represent the peer-reviewed data evaluating lung function in the setting of e-cigarette use. Although limited by small sample sizes, they suggest that e-cigarettes generate smaller acute effects on lung function than conventional cigarettes. Similar to cancer risk, there are no published data describing the long-term lung function or cardiovascular effects of e-cigarettes; ongoing surveillance, especially once e-cigarettes are regulated and standardized, will be necessary.
e-Cigarettes for Smoking Cessation
Several recent studies addressed the efficacy of e-cigarettes as a nicotine replacement in reducing cigarette consumption and promoting cessation. One of the first studied 40 people who were smoking 15 or more conventional cigarettes per day and not interested in quitting, in a 6-month observational trial (48). Participants were given e-cigarettes and supplies and seen at four follow-up visits over 6 months. They were told that e-cigarettes are a healthier alternative to conventional cigarettes and could be used freely as a substitute. The primary efficacy measure was sustained 50% reduction in the number of conventional cigarettes per day at week 24 from baseline. Of the 40 participants enrolled, 27 (68%) completed the 6-month follow-up. At least 50% reduction in daily conventional cigarette use was reported in 13 of 40 (33%) of participants, with 9 of the 13 achieving abstinence, confirmed by exhaled carbon monoxide, from conventional cigarettes. Six of the sustained quitters continued to use e-cigarettes. For the entire cohort, the median number of conventional cigarettes smoked per day decreased from 25 to 5 (P < 0.001). After completion of this intervention phase, the participants were followed for up to 2 years, without being provided additional e-cigarette supplies, to determine durable smoking reduction and biochemically confirmed cessation (49). Of the 40 participants initially enrolled, 23 (58%) completed 2-year follow-up, for whom median daily cigarette use was 4 cigarettes/d, compared with 24 cigarettes/d at baseline (P = 0.003). Eleven (28%) reported greater than 50% reduction in the number of cigarettes smoked per day, and smoking abstinence was reported in 5 of 40 (13%). Although this study suggests that e-cigarette use may lead to decreased daily conventional cigarette use, it was limited by small sample size, lack of a control group, and greater than 40% loss to follow-up.
A third report from the same authors investigated the efficacy of e-cigarettes in smoking reduction and cessation in smokers not motivated to quit (50). This study randomized 300 active smokers to one of three interventions: e-cigarette with 7.2 mg nicotine cartridge for 12 weeks, e-cigarette with 7.2 mg nicotine cartridge for 6 weeks followed by reduction to 5.4 mg cartridge for 6 more weeks, or e-cigarette with cartridge containing no nicotine for 12 weeks. After completion of the 12-week intervention phase, individuals were followed for an additional 40 weeks. During the observation phase, e-cigarettes were not provided, but participants were free to purchase them on their own. Similar to prior studies, participants were informed that e-cigarettes are a healthier alternative to conventional cigarettes and could be used as a substitute. The median number of conventional cigarettes smoked daily at 52 weeks was 7 to 10 lower than baseline in all three study groups. Interestingly, the reduction in daily cigarettes smoked did not significantly differ between the nicotine-containing cartridges and placebo cartridge at weeks 12 or 52 of follow-up. Exhaled carbon monoxide–confirmed quit rates at 52 weeks were 13% for the high nicotine group, 9% for the low nicotine group, and 4% for the placebo nicotine group. Together these data suggest that e-cigarettes can result in favorable modifications in smoking habits and trends in improved cessation rates among smokers not motivated to quit. An electronic cigarette company provided the e-cigarette supplies but did not have input in study design, data analysis, or presentation. However, caution must be taken in interpreting these data because the inclusion of a message that e-cigarettes represent a healthier alternative likely biased the smokers’ use. The lack of equipoise in these studies regarding the harms and benefits of e-cigarettes is a major limitation to inferring efficacy of e-cigarettes as a harm reduction tool.
The largest study investigating whether e-cigarettes are more effective than nicotine patches in achieving smoking cessation was recently published (51). This study randomized 657 smokers wanting to quit to one of three interventions: 16 mg nicotine e-cigarette, placebo e-cigarette, or 21 mg nicotine patch. Participants also received telephone-based behavioral support. The primary outcome was 6-month biologically confirmed, self-reported smoking abstinence. Loss to follow-up was 22%. There was no significant difference in 6-month verified abstinence, with all interventions equally ineffective at promoting cessation: 7.3% with nicotine e-cigarettes, 4.1% with placebo e-cigarettes, and 5.8% with nicotine patches. One-month and 3-month cessation rates also did not differ. e-Cigarettes with or without nicotine were as effective as nicotine patches in achieving 6-month smoking cessation. Notably, cessation rates were quite low in the study, reinforcing the challenges of achieving durable cessation in people with tobacco dependence. As seen previously, placebo e-cigarettes and nicotine-containing e-cigarettes resulted in similar cessation rates, suggesting that the mimicry of conventional smoking behaviors with e-cigarettes may be leading to the modest cessation effect. In this study, nicotine patches were administered at a fixed 21-mg dose, regardless of the number of cigarettes smoked per day, and without tapering; it is unclear if adjunct nicotine gum or lozenges were offered. Previous studies have demonstrated higher cessation rates with nicotine patches and that multimodal approaches can be more effective than patches alone (10). With the findings from this study and lack of additional studies comparing e-cigarettes to other forms of nicotine replacement therapy, there are no data supporting e-cigarettes as a more effective tool than available FDA-approved nicotine replacement therapies for smoking cessation.
The Future Directions for e-Cigarettes
As this review highlights, there are many unanswered questions surrounding the potential harms and benefits of e-cigarettes. Although levels of harmful toxins appear to be lower in e-cigarettes compared with conventional cigarettes, there are no long-term data demonstrating that e-cigarettes are a “healthier alternative.” A few studies suggest that e-cigarettes may represent an effective harm reduction tool in individuals not interested in tobacco cessation, but they do not appear to be more effective than available nicotine replacement therapies. Although many research participants decreased their consumption of conventional cigarettes, they continued to smoke daily, thereby maintaining the cardiovascular risks of tobacco use. The health impacts of dual use of electronic cigarettes and conventional cigarettes have not been explored. The perception of e-cigarettes as a harm reduction tool in the absence of clear evidence is associated with risk (52–55), as exemplified by the historical promotion from tobacco companies of “light” and/or filtered cigarettes, which were later proven no safer than other cigarettes. Moreover, the identification of e-cigarettes as potentially acceptable or beneficial could promote social normalization of smoking behaviors and paradoxically increase conventional cigarette use. There are no data on the potential dangers of using e-cigarettes during pregnancy, and there is a growing literature on the detrimental effects of nicotine on the fetal brain.
Standardization and regulation of e-cigarette products is needed to permit robust longitudinal evaluations of safety and efficacy. A number of professional societies have produced guidelines and policy recommendations aimed at minimizing harms related to hasty electronic cigarette adoption (56–58) (Table 3). The British Medical Association applauded the 2012 regulation of e-cigarettes by the Medicines and Healthcare Products Regulatory Agency (responsible for regulating all medicines and medical devices in the UK), with strong recommendations for research evaluating the efficacy and health implications of e-cigarettes to determine if they reduce or reinforce smoking behaviors (59). In October 2013, the legislative body of the European Union rejected a proposal to regulate e-cigarettes as medicinal devices. It endorsed establishment of a minimum purchase age of 18 years as well as advertising and sponsorship restrictions consistent with conventional cigarettes. In the United States, an increasing number of local and state governments, as well as commercial enterprises, have passed laws related to e-cigarettes. The FDA has announced plans to issue a proposed rule on the regulation of electronic cigarettes in the near future. Until electronic cigarette safety and efficacy data are available, the promotion of e-cigarettes as a harm reduction and cessation tool in smokers is premature, although it could possibly occur if a modified risk tobacco product claim is submitted and approved. Such a claim would require evidence that e-cigarettes significantly reduce the “harm and risk of tobacco-related disease” and “will benefit the health of the population as a whole” (60). Importantly, with known limitations of the machine measurements of the toxicants, and multiple unanswered questions regarding safety and population impact, care must be taken to avoid misleading the public yet again with this new product by the tobacco industry.
Table 3.
Professional society electronic cigarette regulatory policies
| Electronic cigarettes
should be regulated as tobacco products |
| Electronic cigarettes should not be used in smoke-free areas |
| Electronic cigarettes should be taxed at rates equivalent with conventional cigarettes and other tobacco products |
| Candy and menthol flavors should be banned |
| Sales to minors and internet sales should be regulated |
| The FDA should have regulatory authority over electronic cigarettes including |
| Warning labels |
| Advertising |
| Health claims |
| Manufacturing processes |
| Liquid cartridge chemical composition and nicotine content |
Definition of abbreviation: FDA = U.S. Food and Drug Administration.
Acknowledgments
Acknowledgment
The authors thank Drs. Ivor Douglas, Jonathan Samet, Smita Pakhale, and Kai-Hakon Carlsen for their input with this review.
Footnotes
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Terry L.Smoking and health: report of the Advisory Committee to the Surgeon General of the United States. In: U-23 Department of Health, Education and Welfare. Washington DC: Public Health Service Publication No. 1103; 1964[accessed 2013 Oct 15]. Available from: http://profiles.nlm.nih.gov/ps/retrieve/ResourceMetadata/NNBBMQ
- 2.Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, Hartge P, Gapstur SM. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368:351–364. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. World Health Organization Report on the global tobacco epidemic, 2011. warning about the dangers of tobacco [accessed 2013 Oct 15]. Available from: http://www.who.int/tobacco/global_report/2011/en/
- 4.Rigotti N. Smoking cessation in patients with respiratory disease: existing treatments and future directions. Lancet Respiratory Medicine. 2013;1:241–250. doi: 10.1016/S2213-2600(13)70063-8. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. World Health Organization Fact Sheet 2009- Tobacco. 2009[accessed 2013 Dec 17]. Available from: http://www.who.int/nmh/publications/fact_sheet_tobacco_en.pdf
- 6.Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, McAfee T, Peto R. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368:341–350. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- 7.Godtfredsen NS, Prescott E, Osler M. Effect of smoking reduction on lung cancer risk. JAMA. 2005;294:1505–1510. doi: 10.1001/jama.294.12.1505. [DOI] [PubMed] [Google Scholar]
- 8.Bolliger CT, Zellweger JP, Danielsson T, van Biljon X, Robidou A, Westin A, Perruchoud AP, Säwe U. Influence of long-term smoking reduction on health risk markers and quality of life. Nicotine Tob Res. 2002;4:433–439. doi: 10.1080/1462220021000018380. [DOI] [PubMed] [Google Scholar]
- 9.Wennike P, Danielsson T, Landfeldt B, Westin A, Tønnesen P. Smoking reduction promotes smoking cessation: results from a double blind, randomized, placebo-controlled trial of nicotine gum with 2-year follow-up. Addiction. 2003;98:1395–1402. doi: 10.1046/j.1360-0443.2003.00489.x. [DOI] [PubMed] [Google Scholar]
- 10.Stead LF, Perera R, Bullen C, Mant D, Hartmann-Boyce J, Cahill K, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2012;11:CD000146. doi: 10.1002/14651858.CD000146.pub4. [DOI] [PubMed] [Google Scholar]
- 11.Bolliger CT, Zellweger JP, Danielsson T, van Biljon X, Robidou A, Westin A, Perruchoud AP, Säwe U. Smoking reduction with oral nicotine inhalers: double blind, randomised clinical trial of efficacy and safety. BMJ. 2000;321:329–333. doi: 10.1136/bmj.321.7257.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rennard SI, Glover ED, Leischow S, Daughton DM, Glover PN, Muramoto M, Franzon M, Danielsson T, Landfeldt B, Westin A. Efficacy of the nicotine inhaler in smoking reduction: a double-blind, randomized trial. Nicotine Tob Res. 2006;8:555–564. doi: 10.1080/14622200600789916. [DOI] [PubMed] [Google Scholar]
- 13.Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev. 2013;5:CD009329. doi: 10.1002/14651858.CD009329.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yamin CK, Bitton A, Bates DW. E-cigarettes: a rapidly growing Internet phenomenon. Ann Intern Med. 2010;153:607–609. doi: 10.7326/0003-4819-153-9-201011020-00011. [DOI] [PubMed] [Google Scholar]
- 15.Caponnetto P, Campagna D, Papale G, Russo C, Polosa R. The emerging phenomenon of electronic cigarettes. Expert Rev Respir Med. 2012;6:63–74. doi: 10.1586/ers.11.92. [DOI] [PubMed] [Google Scholar]
- 16.Noel JK, Rees VW, Connolly GN. Electronic cigarettes: a new ‘tobacco’ industry? Tob Control. 2011;20:81. doi: 10.1136/tc.2010.038562. [DOI] [PubMed] [Google Scholar]
- 17.Vansickel AR, Eissenberg T. Electronic cigarettes: effective nicotine delivery after acute administration. Nicotine Tob Res. 2013;15:267–270. doi: 10.1093/ntr/ntr316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vansickel AR, Cobb CO, Weaver MF, Eissenberg TE. A clinical laboratory model for evaluating the acute effects of electronic “cigarettes”: nicotine delivery profile and cardiovascular and subjective effects. Cancer Epidemiol Biomarkers Prev. 2010;19:1945–1953. doi: 10.1158/1055-9965.EPI-10-0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention, US Department of Health and Human ServicesNational Youth Tobacco Survey. Atlanta; 2013[accessed 2013 Oct 15]. Available from: http://www.cdc.gov/tobacco/data_statistics/surveys/nyts
- 20.Corey C, Wang B, Johnson S, Apelberg B, Husten C Centers for Disease Control and Prevention (CDC) Notes from the field: electronic cigarette use among middle and high school students - United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 2013;62:729–730. [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention, US Department of Health and Human ServicesPress release: About one in five U.S. adult cigarette smokers have tried electronic cigarette. Atlanta; 2013[accessed 2013 Nov 10] Available from: http://www.cdc.gov/media/releases/2013/p0228_electronic_cigarettes.html
- 22.Adkison SE, O’Connor RJ, Bansal-Travers M, Hyland A, Borland R, Yong HH, Cummings KM, McNeill A, Thrasher JF, Hammond D, et al. Electronic nicotine delivery systems: international tobacco control four-country survey. Am J Prev Med. 2013;44:207–215. doi: 10.1016/j.amepre.2012.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goniewicz ML, Lingas EO, Hajek P. Patterns of electronic cigarette use and user beliefs about their safety and benefits: an internet survey. Drug Alcohol Rev. 2013;32:133–140. doi: 10.1111/j.1465-3362.2012.00512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pearson JL, Richardson A, Niaura RS, Vallone DM, Abrams DB. e-Cigarette awareness, use, and harm perceptions in US adults. Am J Public Health. 2012;102:1758–1766. doi: 10.2105/AJPH.2011.300526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Etter JF, Bullen C. Electronic cigarette: users profile, utilization, satisfaction and perceived efficacy. Addiction. 2011;106:2017–2028. doi: 10.1111/j.1360-0443.2011.03505.x. [DOI] [PubMed] [Google Scholar]
- 26.Dawkins L, Turner J, Roberts A, Soar K. ‘Vaping’ profiles and preferences: an online survey of electronic cigarette users. Addiction. 2013;108:1115–1125. doi: 10.1111/add.12150. [DOI] [PubMed] [Google Scholar]
- 27.Dwyer JB, McQuown SC, Leslie FM. The dynamic effects of nicotine on the developing brain. Pharmacol Ther. 2009;122:125–139. doi: 10.1016/j.pharmthera.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kralikova E, Novak J, West O, Kmetova A, Hajek P. Do e-cigarettes have the potential to compete with conventional cigarettes?: a survey of conventional cigarette smokers’ experiences with e-cigarettes. Chest. 2013;144:1609–1614. doi: 10.1378/chest.12-2842. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Food and Drug AdministrationRegulation of e-cigarettes and other tobacco products. 2011[accessed 2013 Dec 6]. Available from: http://www.fda.gov/newsevents/publichealthfocus/ucm252360.htm
- 30.Benowitz NL, Goniewicz ML. The regulatory challenge of electronic cigarettes. JAMA. 2013;310:685–686. doi: 10.1001/jama.2013.109501. [DOI] [PubMed] [Google Scholar]
- 31.Cobb NK, Cobb CO. Regulatory challenges for refined nicotine products. Lancet Respiratory Medicine. 2013;1:431–432. doi: 10.1016/S2213-2600(13)70160-7. [DOI] [PubMed] [Google Scholar]
- 32.Elliott S.E-cigarette makers’ ads echo tobacco's heyday. New York Times August 30, 2013[accessed 2013 Oct 15]. Available from: http://www.nytimes.com/2013/08/30/business/media/e-cigarette-makers-ads-echotobaccos-heyday.html
- 33.Rodu B.The e-cigarette revolution. Rstreet.org December 12, 2012[accessed 2013 Nov 11]. Available at http://www.rstreet.org/op-ed/the-e-cigarette-revolution/
- 34.Robehmed N.E-cigarette sales surpass $1 billion as big tobacco moves in. Forbes Magazine Online September 17, 2013[accessed 2013 Oct 15]. Available from: http://www.forbes.com/sites/natalierobehmed/2013/09/17/e-cigarette-sales-surpass-1-billion-as-big-tobacco-moves-in/
- 35.Trtchounian A, Williams M, Talbot P. Conventional and electronic cigarettes (e-cigarettes) have different smoking characteristics. Nicotine Tob Res. 2010;12:905–912. doi: 10.1093/ntr/ntq114. [DOI] [PubMed] [Google Scholar]
- 36.Goniewicz ML, Kuma T, Gawron M, Knysak J, Kosmider L. Nicotine levels in electronic cigarettes. Nicotine Tob Res. 2013;15:158–166. doi: 10.1093/ntr/nts103. [DOI] [PubMed] [Google Scholar]
- 37.Djordjevic MV, Stellman SD, Zang E. Doses of nicotine and lung carcinogens delivered to cigarette smokers. J Natl Cancer Inst. 2000;92:106–111. doi: 10.1093/jnci/92.2.106. [DOI] [PubMed] [Google Scholar]
- 38.Counts ME, Morton MJ, Laffoon SW, Cox RH, Lipowicz PJ. Smoke composition and predicting relationships for international commercial cigarettes smoked with three machine-smoking conditions. Regul Toxicol Pharmacol. 2005;41:185–227. doi: 10.1016/j.yrtph.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 39.U.S. Department of Health and Human Services. How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health2010 [PubMed] [Google Scholar]
- 40.Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, Prokopowicz A, Jablonska-Czapla M, Rosik-Dulewska C, Havel C, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. doi: 10.1136/tobaccocontrol-2012-050859. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Westenberger BJ.Evaluation of e-cigarettes. US Food and Drug Administration Release. Silver Spring, MD [accessed 2013 Oct 15]. Available from: http://www.fda.gov/downloads/drugs/scienceresearch/ucm173250.pdf
- 42.US Food and Drug AdministrationFDA warns of health risks posed by e-cigarettes: consumer update, 2009[accessed 2013 Oct 15]. Available from: http://www.fda.gov/forconsumers/consumerupdates/ucm173401.htm
- 43.Czogala J, Goniewicz ML, Fidelus B, Zielinska-Danch W, Travers MJ, Sobczak A. Secondhand exposure to vapors from electronic cigarettes. Nicotine Tob Res. doi: 10.1093/ntr/ntt203. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Varughese S, Teschke K, Brauer M, Chow Y, van Netten C, Kennedy SM. Effects of theatrical smokes and fogs on respiratory health in the entertainment industry. Am J Ind Med. 2005;47:411–418. doi: 10.1002/ajim.20151. [DOI] [PubMed] [Google Scholar]
- 45.Wieslander G, Norbäck D, Lindgren T. Experimental exposure to propylene glycol mist in aviation emergency training: acute ocular and respiratory effects. Occup Environ Med. 2001;58:649–655. doi: 10.1136/oem.58.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vardavas CI, Anagnostopoulos N, Kougias M, Evangelopoulou V, Connolly GN, Behrakis PK. Short-term pulmonary effects of using an electronic cigarette: impact on respiratory flow resistance, impedance, and exhaled nitric oxide. Chest. 2012;141:1400–1406. doi: 10.1378/chest.11-2443. [DOI] [PubMed] [Google Scholar]
- 47.Flouris AD, Chorti MS, Poulianiti KP, Jamurtas AZ, Kostikas K, Tzatzarakis MN, Wallace Hayes A, Tsatsakis AM, Koutedakis Y. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhal Toxicol. 2013;25:91–101. doi: 10.3109/08958378.2012.758197. [DOI] [PubMed] [Google Scholar]
- 48.Polosa R, Caponnetto P, Morjaria JB, Papale G, Campagna D, Russo C. Effect of an electronic nicotine delivery device (e-Cigarette) on smoking reduction and cessation: a prospective 6-month pilot study. BMC Public Health. 2011;11:786. doi: 10.1186/1471-2458-11-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Polosa R, Morjaria JB, Caponnetto P, Campagna D, Russo C, Alamo A, Amaradio M, Fisichella A. Effectiveness and tolerability of electronic cigarette in real-life: a 24-month prospective observational study. Intern Emerg Med. doi: 10.1007/s11739-013-0977-z. (In press) [DOI] [PubMed] [Google Scholar]
- 50.Caponnetto P, Campagna D, Cibella F, Morjaria JB, Caruso M, Russo C, Polosa R. EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS ONE. 2013;8:e66317. doi: 10.1371/journal.pone.0066317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bullen C, Howe C, Laugesen M, McRobbie H, Parag V, Williman J, Walker N. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382:1629–1637. doi: 10.1016/S0140-6736(13)61842-5. [DOI] [PubMed] [Google Scholar]
- 52.Cahn Z, Siegel M. Electronic cigarettes as a harm reduction strategy for tobacco control: a step forward or a repeat of past mistakes? J Public Health Policy. 2011;32:16–31. doi: 10.1057/jphp.2010.41. [DOI] [PubMed] [Google Scholar]
- 53.Hastings G, de Andrade M, Moodie C. Tobacco harm reduction: the devil is in the deployment. BMJ. 2012;345:e8412. doi: 10.1136/bmj.e8412. [DOI] [PubMed] [Google Scholar]
- 54.Britton J, McNeill A. Nicotine regulation and tobacco harm reduction in the UK. Lancet. 2013;381:1879–1880. doi: 10.1016/S0140-6736(13)61122-8. [DOI] [PubMed] [Google Scholar]
- 55.Zeller M, Hatsukami D Strategic Dialogue on Tobacco Harm Reduction Group. The Strategic Dialogue on Tobacco Harm Reduction: a vision and blueprint for action in the US. Tob Control. 2009;18:324–332. doi: 10.1136/tc.2008.027318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.American Thoracic SocietyATS policy position: e-cigarettes. 2013[accessed 2013 Nov 11]. Available from: http://www.thoracic.org/advocacy/press-releases/ATS_Policy_Position_eCigarettes.pdf
- 57.American College of PhysiciansTobacco Control and Prevention: Policy Monograph. Philadelphia: American College of Physicians; 2010 [Google Scholar]
- 58.World Health OrganizationQuestions and answers on electronic cigarettes or electronic nicotine delivery systems (ENDS). July 9, 2013[accessed 2013 Nov 11]. Available from: http://www.who.int/tobacco/communications/statements/eletronic_cigarettes/en/
- 59.British Medical AssociationBMA response to MHRA’s announcement on e-cigarettes. Press Release June 12, 2013[accessed 2013 Nov 9]. Available from: http://web2.bma.org.uk/pressrel.nsf/wall/1F182180B5D17A6B80257B8800472B4D
- 60.US Food and Drug AdministrationModified risk tobacco products. 2012[accessed 2013 Dec 6]. Available from: http://www.fda.gov/tobaccoproducts/labeling/tobaccoproductreviewevaluation/ucm304465.html
- 61.Wollscheid KA, Kremzner ME. Electronic cigarettes: safety concerns and regulatory issues. Am J Health Syst Pharm. 2009;66:1740–1742. doi: 10.2146/ajhp090127. [DOI] [PubMed] [Google Scholar]