Abstract
Introduction:
Coronary heart disease (CHD) is associated with significant morbidity and mortality, including mental health comorbidity, which is associated with poor outcomes. Self-management is key, but there is limited access to self-management support. Internet-delivered interventions may increase access.
Objective:
The aim of this study was to conduct a systematic review to (1) determine the effectiveness of Internet-delivered CHD self-management support for improving CHD, mood, and self-management related outcomes and (2) identify and describe essential components for effectiveness.
Method:
Randomized controlled trials that met prespecified eligibility criteria were identified using a systematic search of 3 healthcare databases (Medline, PsychINFO, and Embase).
Results:
Seven trials, which included 1321 CHD patients, were eligible for inclusion. There was considerable heterogeneity between studies in terms of the intervention content, outcomes measured, and study quality. All 7 of the studies reported significant positive between-group effects, in particular for lifestyle-related outcomes. Personalization of interventions and provision of support to promote engagement may be associated with improved outcomes, although more data are required to confirm this. The theoretical basis of interventions was poorly developed though evidence-based behavior change interventions were used.
Conclusion:
More well-designed randomized controlled trials are needed. These should also explore how interventions work and how to improve participant retention and satisfaction and examine the role of personalization and support within interventions.
KEY WORDS: coronary heart disease, ehealth, Internet delivered intervention, self-management support
Coronary heart disease (CHD) is associated with significant morbidity and mortality. Approximately 3.5% of the general practice registered United Kingdom population has been diagnosed with CHD.1 To maintain quality of life and prevent poor outcomes, in particular myocardial infarction, risk factors must be addressed through behavioral and lifestyle changes, including smoking cessation, physical activity, weight loss, and reduced high saturated fat and alcohol intake alongside medication.2,3 However, many patients are symptomatic despite receiving usual care.4 For some symptomatic individuals, no underlying pathology or cause can be detected and available treatments are not fully effective for symptom relief. These patients continue to seek treatment from emergency departments and general practice.5,6 Exacerbation of CHD symptoms can occur as a result of depression and anxiety, which are common in people with CHD and associated with poor outcome.7,8 Psychological interventions such as cognitive behavioral therapy (CBT) are effective in improving mood9 but are not routinely available to CHD patients.
Self-management is key10 and requires lifestyle changes, such as improved diet and increased physical activity, adherence to treatment regimens, and management of distress. Lifestyle modification self-management programs have been found to be more effective than routine clinical care in improving mortality and cardiac risk factor–related behaviors.11 There is some evidence that personalized intervention is cost-effective and may help reduce symptoms in CHD patients with current chest pain and depression.12 A combination of patient self-efficacy and support from healthcare professionals has been found to be necessary for optimal self-management.13 However, professional support for self-management is limited. For instance, in the United Kingdom, CHD patients may have only 1 scheduled appointment with their family physician or practice nurse each year.
Self-management support delivered via the Internet may be 1 solution. Internet-delivered interventions are convenient for the user as they can be accessed at any time, have the potential to reach patients who might not seek support otherwise, and are cost effective.14,15 Interest in Internet-delivered interventions for patients with long-term conditions, including CHD, is increasing; however, their effectiveness and the elements essential for effectiveness are unknown.16–18 Determining this is complicated by the fact that interventions may vary in terms of their content and their target; for instance, they may aim to improve 1 or more CHD-related symptoms, behaviors, or emotions. Given the well-known, negative impact of comorbid mental health problems associated with CHD,7,8 it would seem that online interventions could potentially address this, especially given their success on mood- and anxiety-related outcomes and improvements in quality of life and functioning.19,20 However, to date, this potential has not been fully realized for people with CHD.18 The current systematic review establishes the state of the art by identifying and detailing interventions for Internet-delivered self-management support for CHD, which also address wellbeing (eg, mood, quality of life, functional status) outcomes.
Methods
Eligibility Criteria
Studies published in English in any year that met the following criteria were included:
Parallel group randomized controlled trials (RCTs), randomized cross-over or sequential-controlled, or cluster randomized trials.
Participants were adults (≥18 years) with a diagnosis (clinician or self-reported) of CHD. Studies including CHD patients with comorbidities and those with other long-term conditions were included if outcomes for patients with a primary diagnosis of CHD were reported independently.
Tested the effectiveness of Internet-delivered self-management support for CHD and addressed well-being outcomes, such as mood, quality of life, or functional status. Interventions were considered to be Internet delivered if they were accessible via the Internet in any setting outside a clinic, hospital, or health center and on any device. Self-management support was defined as any support designed to help CHD patients with at least 1 of the following: making lifestyle changes, adhering to treatment regimens, managing physical symptoms, and managing psychological distress.
Used 1 or more of the following comparison groups: usual care, waiting list, attention, information, or online discussion group.
Included outcomes relating to CHD signs and symptoms (eg, blood pressure, cardiac events, mortality, self-reported symptoms of CHD such as chest pain), lifestyle changes targeting CHD risk factors (eg, reduction in smoking and alcohol use, improved diet or increased physical activity), subjective measures of health (eg, quality of life, functional status, well-being), improved mood (eg, improvement in levels of depression or anxiety), or improvement in self-management related-factors (eg, self-efficacy, treatment adherence). Follow-up could be for any time period.
Search Strategy
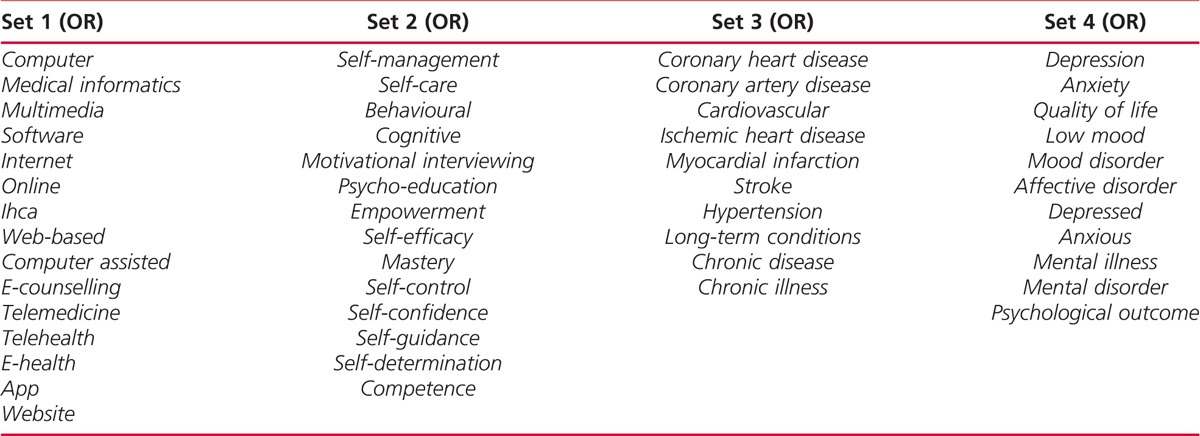
A systematic search of 3 electronic databases (Medline, PsychINFO, and Embase) was conducted in October 2016 by J.P. The search combined terms relating to online, Internet, self-management, and CHD with the Boolean operator AND. The reference lists of included studies were also searched. Details of the full search strategy are included in the Appendix.
Study Selection
A 2-stage screening process was conducted. Search results were uploaded to reference management software: Endnote21 and duplicates removed. The titles and abstracts were then screened independently by J.P. and D.R. The full text of potentially relevant studies was then retrieved. Studies meeting the inclusion criteria were selected independently by J.P. and G.A.L., disagreements were resolved through discussion with E.A.B. The complete process is summarized in a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram (Figure).
FIGURE.
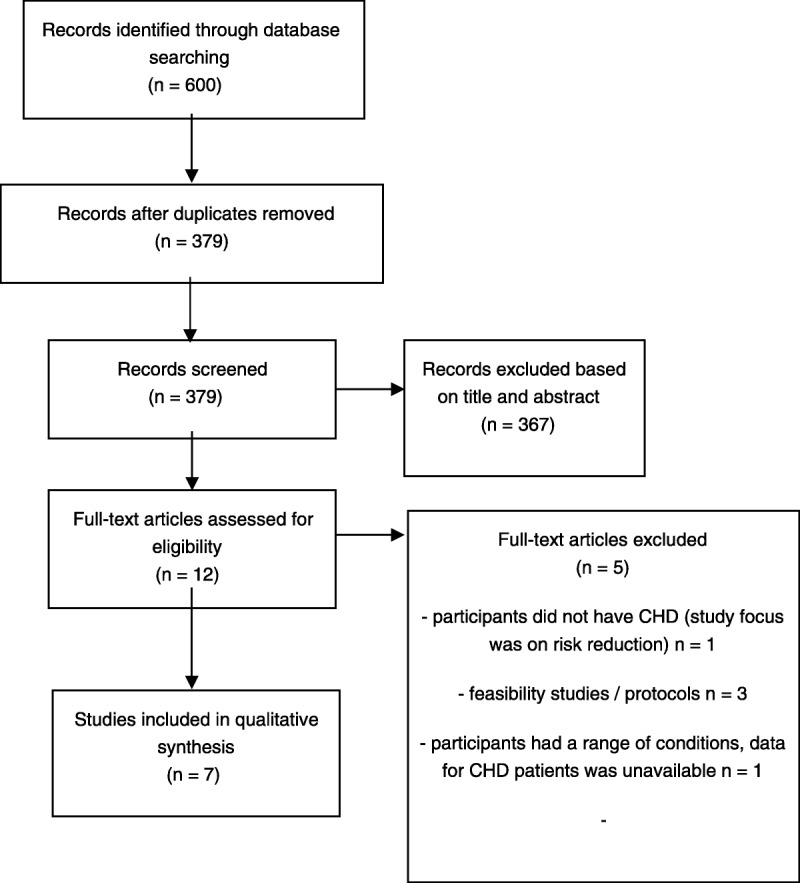
PRISMA diagram of literature search.
Data Extraction
The study designs, types of participants, intervention components, comparators, and outcome measures were extracted by J.P. and reviewed and checked by G.A.L. and M.D.
Assessment of Risk of Bias of Included Studies
The methodological quality of the included studies was assessed independently by M.D. and J.P. using the Cochrane Collaboration’s Tool for Assessing Risk of Bias22 to assess domains random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, completeness of outcome data, and selective reporting. Disagreements were resolved by E.A.B.
Data Synthesis
There was considerable heterogeneity between the included studies in terms of the content and aims of the interventions and the reported outcomes, so meta-analysis was not possible. A narrative synthesis was therefore conducted. Findings for outcomes relating to (1) CHD status, (2) lifestyle changes, (3) subjective health, (4) mood, and (5) self-management indicators are reported.
Results
Included Studies
The results of the literature search and reasons for study exclusion are detailed in the Figure. In summary, of 12 full-text articles assessed, 7 studies were eligible for inclusion. Studies were conducted in the United Kingdom (n = 1), Norway (n = 1), Australia (n = 2), New Zealand (n = 1), Canada (n = 1), and the United States (n = 1) (see Table 1).
TABLE 1.
Characteristics of the Included Studies
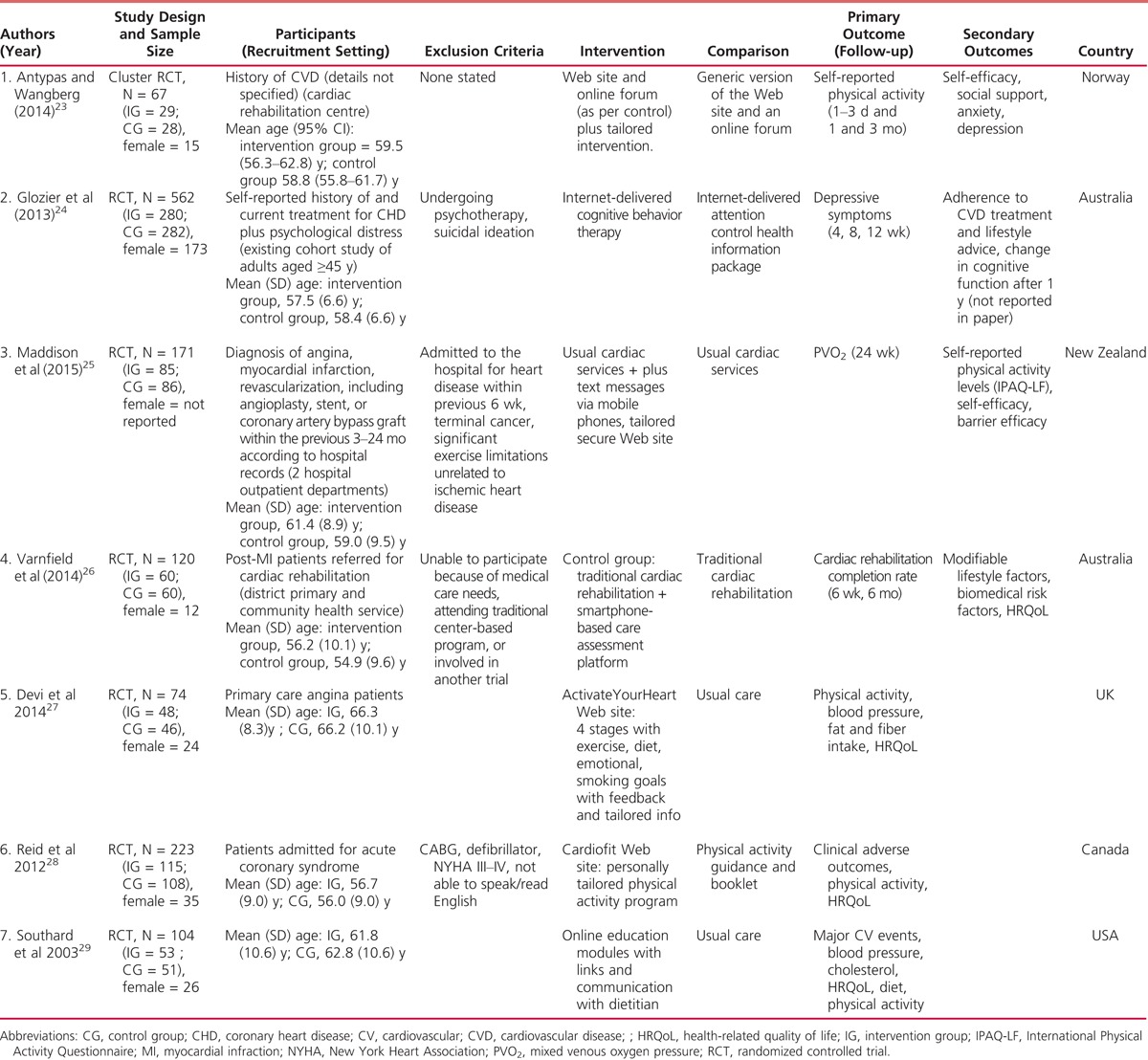
Characteristics of Included Studies
The studies included a total of 1321 participants, of which 670 (50.7%) participated in the interventions. Sample sizes varied from 67 participants23 to 562 participants.26 A minority of participants (285/1321) were female (although 1 study25 did not report this). All participants had CHD; in 1 study,26 some participants also had chronic back pain (n = 357/571). In another study,24 patients receiving treatment for CHD were recruited only if they also reported psychological distress for at least 6 months duration (n = 562).
All 7 studies were RCTs, including 1 cluster RCT.23 A wide range of Internet interventions designed to improve CHD self-management were tested; each is described below. Comparisons were with usual care or no Internet delivered intervention25–29 or with a more generic (eg, information only) version of the Internet intervention.23,24 Study characteristics are summarized in Table 1.
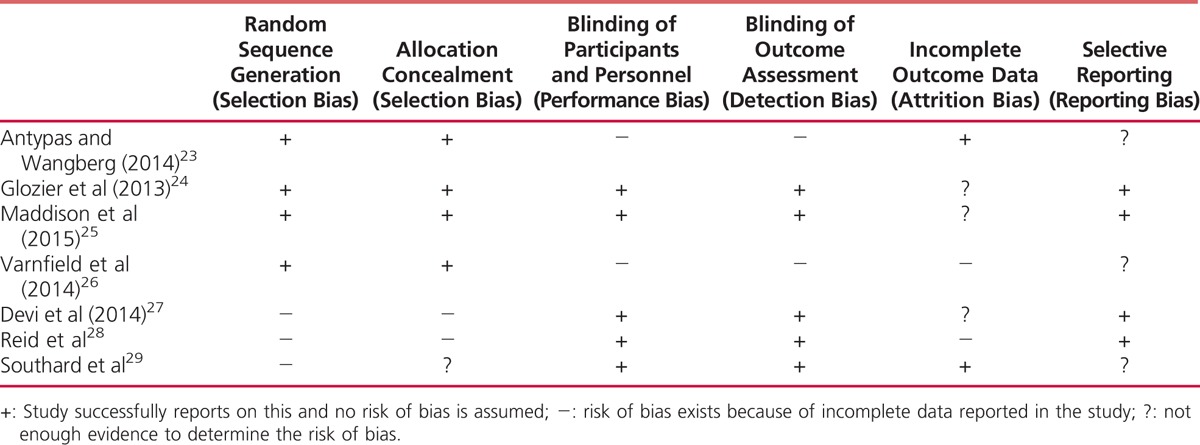
Assessment of Risk of Bias of Included Studies
Overall, the included studies were assessed as having a low risk of selection bias (Table 2) using the Cochrane Tool for Assessment of Risk of Bias.22 In 2 studies,23,26 there was risk of performance bias due to knowledge of the allocated interventions by participants and or personnel during the study. The same 2 studies had a high risk of detection bias as participants were not blinded and made their own subjective assessment of self-reported outcomes. Attrition was high in 2 of the studies (ie, more than 10%): Varnfield et al (2014)26 had end-point data on 26 of 41 control group participants and 46 of 53 intervention group participants. Reid et al (2012)28 assessed 223 at baseline and 153 (69%) at 12-month follow-up. Three trials24,25,27 did not provide enough evidence to judge whether there was selective outcome reporting.
TABLE 2.
Summary of Risk of Bias in Included Studies
Description of Internet-delivered Interventions
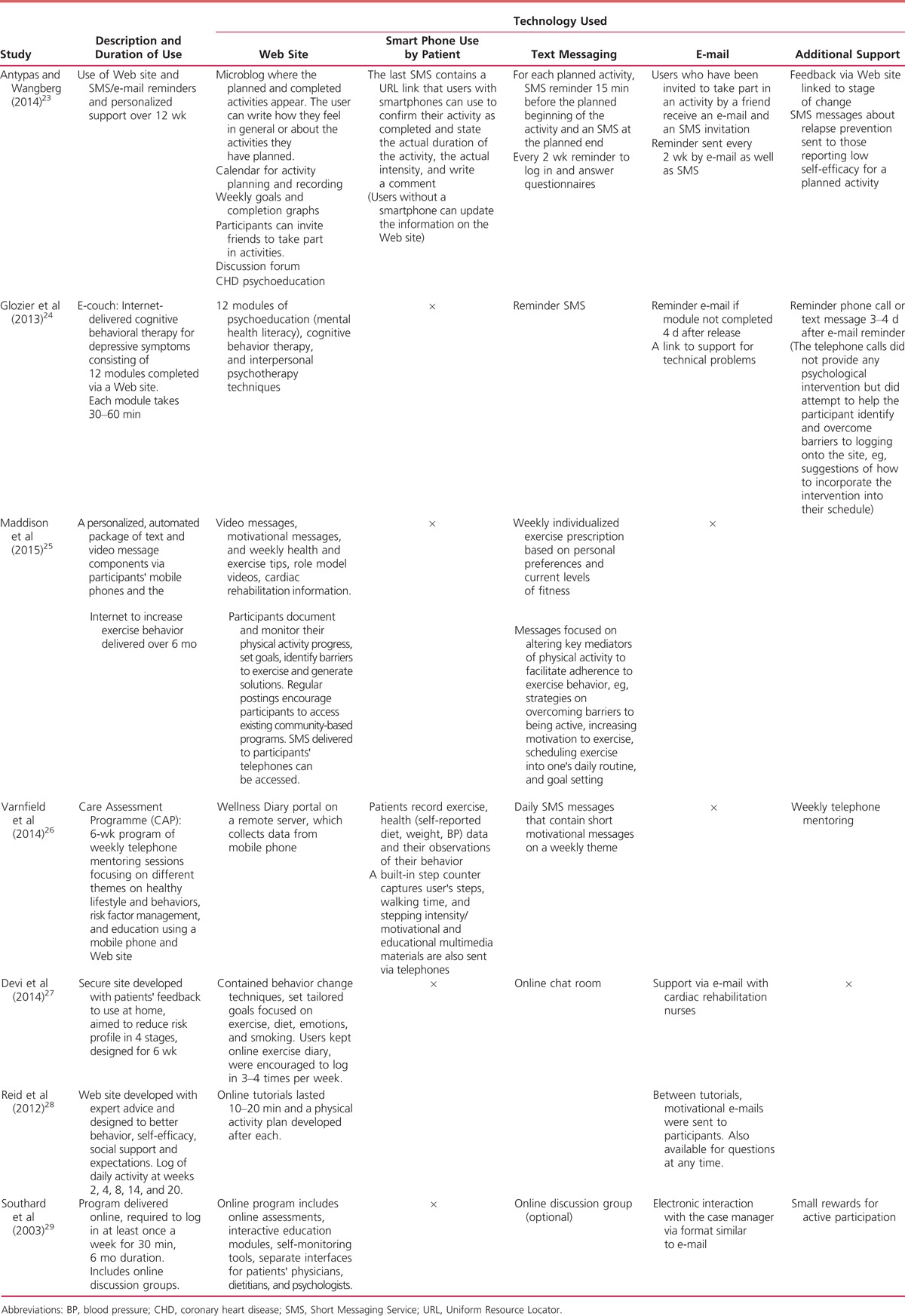
The interventions are described in Table 3, specific components were identified for comparison.
TABLE 3.
Characteristics of Included Internet Interventions to Support Coronary Heart Disease
Theoretical Basis
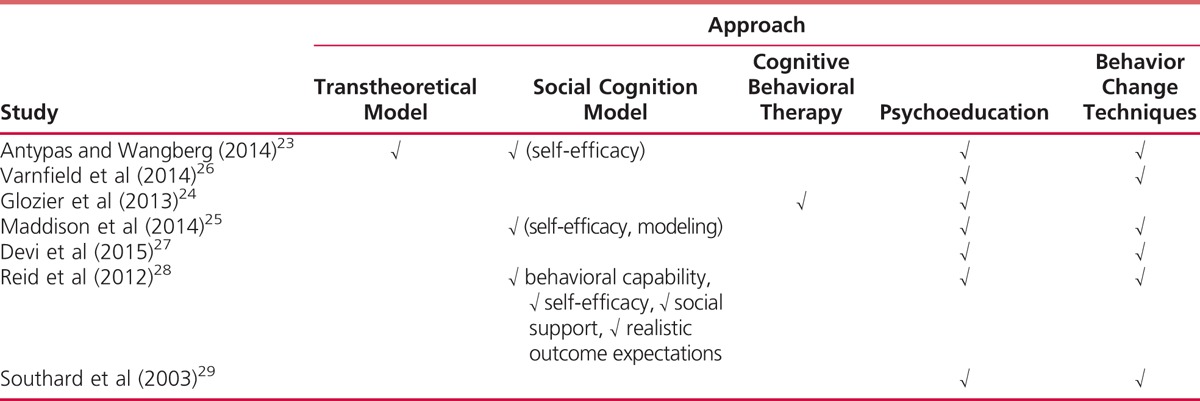
All the interventions included some form of psychoeducation (see Table 4). Six studies23,24,26–29 used evidence-based behavior change techniques such as goal setting, activity planning, and biofeedback. The intervention reported by Maddison et al (2015)25 also uses role model videos. The intervention by Glozier et al (2013)24 is CBT for depression and has no CHD-specific content (although the control group received heart disease-related psychoeducation). The intervention by Glozier et al (2013)24 also used techniques from interpersonal therapy.
TABLE 4.
Approach to Self-management Employed by Internet Interventions
Use of Personalization
Six of the interventions were personalized; that is, feedback was provided according to the individual participant’s responses and progress through the intervention. Modifications were made in response to clinical status22,24–27 or the participant’s rating of their stage of change or self-efficacy for an activity.23 In 5 studies, feedback was provided electronically,23,25,27–29 and in a sixth study,26 feedback was provided by trained “mentors” through weekly telephone consultations. Calls lasted approximately 15 minutes and were audio or video recorded according to participant preference. Mentors accessed the patients’ data on a Web portal before the consultation to facilitate and personalize feedback and goal setting.
Use of Support to Promote Engagement
Training to use the interventions was provided in 4 studies.23,26–28 In 4 studies,23–26,28 e-mail reminders and/or motivational SMS were sent. In 1 study,29 participants were given small rewards such as “key chains, athletic socks, book markers, and refrigerator magnets each month for active participation,” for instance, for completing modules and entering data.
Intervention Effectiveness
Study findings are summarized below, and main outcomes for each category are reported in Tables 5–8 although not all studies reported data in the same way. Each study reported different outcomes, so we were unable to synthesize results.
TABLE 5.
Intervention Effectiveness: Coronary Heart Disease Status and Lifestyle Changes
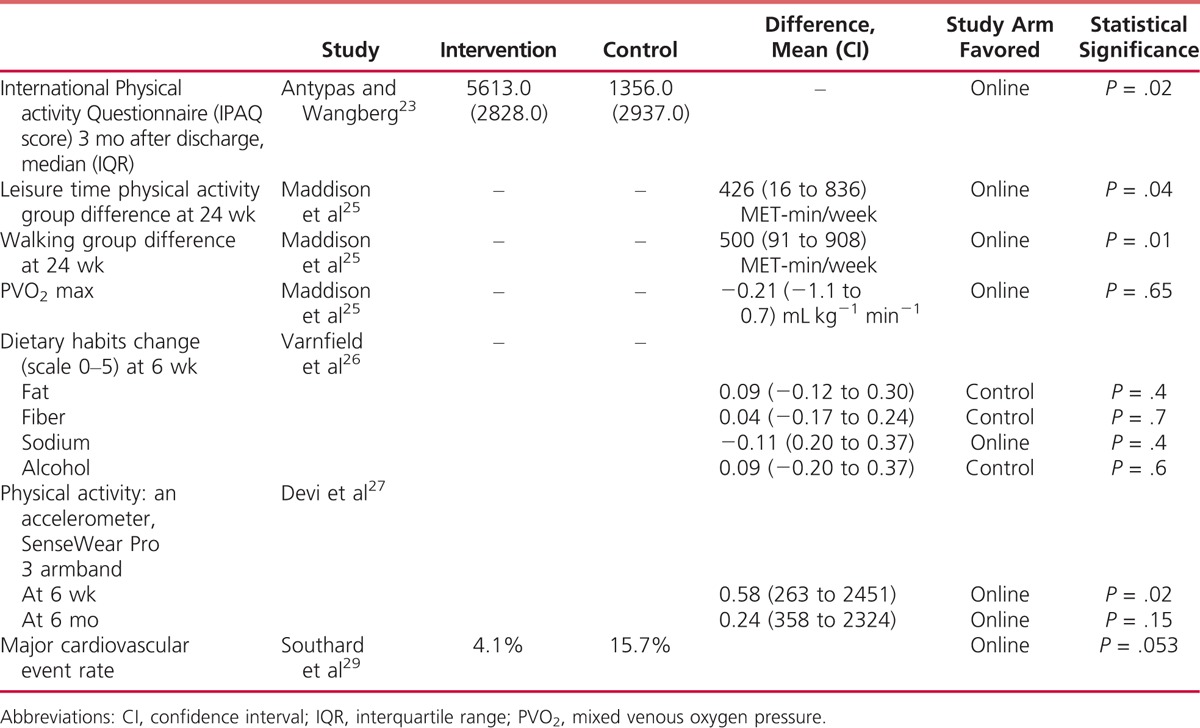
TABLE 8.
Intervention Effectiveness. Self-management Indicators
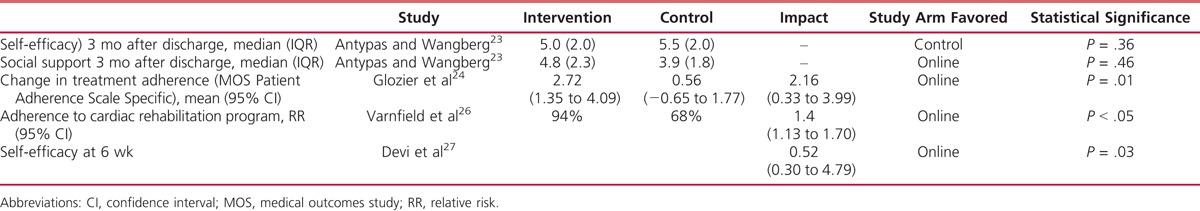
TABLE 6.
Intervention Effectiveness: Well-being and Functioning

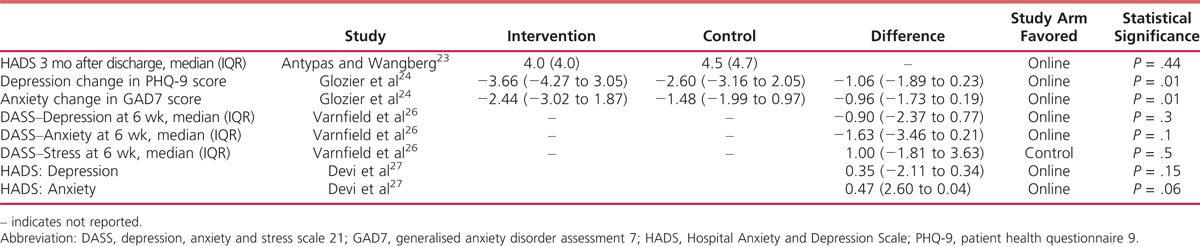
TABLE 7.
Intervention Effectiveness: Mood
CHD status: Maddison et al (2014)25 measured peak oxygen uptake as their primary outcome measure but found no statistically significant difference between groups. Varnfield et al (2014)26 recorded blood pressure, resting heart rate and lipid profile though no between-group statistically significant differences were found apart from triglycerides (P = .04). Devi et al (2014)27 found significant improvement in favor of the intervention at 6 weeks in weight loss (−0.56 kg; 95% confidence interval [CI], −1.78 to −0.15; P = .02) and angina frequency (95% CI, 8.57–35.05; P = .002); improvements in angina frequency were also found at 6 months follow-up (95% CI, 1.89–29.41; P = .02). At 6-month follow-up, Southard et al29 also found greater weight loss in the intervention group (−3.68 vs +0.47 lb; P = .003); there were no other significant between-group differences for any other measured CHD outcome, although the number of cardiovascular events was lower in the intervention group compared with the control group (P = .053).
Lifestyle changes: Six studies measured outcomes related to lifestyle changes, including physical activity and eating behavior. Five studies found significant improvement in favor of the intervention, with improvements in dietary outcomes26 and increased physical activity23,25,27,28 reported.
Subjective health: Four studies25–28 measured quality of life. Two studies26,27 found a clinically relevant overall increase at 6 weeks in the intervention compared with the control group. In 1 study, this was also found at 6 months follow-up.27 In a third study,28 improvements in emotional and physical domains of quality of life were found only over the 12-month study period.
Mood: Four studies23,24,26,27 measured mood-related outcomes. Only the study that tested the depression-specific intervention24 found a significant difference, with depression and anxiety scores at 6 weeks decreasing more in the intervention group. The patient health questionnaire 9 was reduced in the intervention group from 12 (±3.4) at baseline to 8.4 (±5.1) post intervention while the generalised anxiety disorder assessment 7 anxiety scores were reduced from 8.9 (±4.2) to 6.5 (±4.6).
Self-management indicators: Two studies23,27 tested self-efficacy as an outcome; no significant differences were found at 3 months in 1 study.23 In another study,27 improvement was found at 6 weeks (95% CI, 0.30–4.79; P = .03), but not at 6 months. Maddison et al (2015)25 tested and reported that changes in self-efficacy have a mediating effect of 13% on physical activity (P = .021). Antypas and Wangberg (2014)23 reported an increase in social support in the personalized group, and a decrease in support in the control group. The difference between the groups, however, was not statistically significant (P = .46). Two studies24,26 found statistically significant differences in treatment adherence favoring the intervention group. The intervention test by Reid et al (2014)28 was “designed to foster behavioural capability, self-efficacy, social support, and realistic outcome expectations”, though these factors were not measured explicitly.
Effect of Specific Components
There was some indication that personalization may be important. Of the Internet-delivered intervention studies reporting significant positive between-group effects, 6 used personalization.23,25–29 More frequent access and usage of content may also lead to better outcomes, although there is a lack of data to test this and this may be difficult to compare across studies of interventions of differing intensity. There were insufficient data to determine the effectiveness of other components of the interventions.
Discussion
This systematic review identified 7 studies (1321 participants) that compared Internet-delivered CHD self-management support with usual care or an inactive control and considered both physical and well-being outcomes. The quality of these studies was reasonable, but there was heterogeneity between studies in terms of intervention content and the outcomes measured. This means that, although there was some supportive evidence, the overall effectiveness of such interventions could not be determined. Specific intervention components that varied between studies included the theoretical basis, the use of personalization (eg, feedback based on personal data), and the use of support (help to promote the use of the intervention). Data were insufficient to determine the effectiveness of these components, although there was some indication that increased engagement through personalization and support is important.
A surprising finding, given the size of the problem of CHD self-management24 and the well-recognized potential for Internet interventions,14,15 is the small number of relevant studies. However, we also identified 6 protocols for studies that would meet our inclusion criteria. More evidence should therefore be available soon. The current review nevertheless provides useful information to inform the design and appraisal of future studies and of interventions.
Findings to Inform Study Design
The included studies made adequate use of randomization and allocation concealments. However, there was a lack of blinding and evidence of incomplete or selective reporting for some studies (Table 2). Future trials should ensure that they adhere to established standards.30 In addition, some trials had high rates of attrition. High dropout rates may indicate lack of acceptability of the intervention; future studies should investigate this. For instance, none of the included interventions involved users in their development (which may improve acceptability and satisfaction). Four of the interventions tested included components designed to support engagement such as text messaging or reminders.23,25,26,28 Future studies should be designed to test specifically the effectiveness of this.
Variation between studies in reported outcomes made comparison across studies difficult. The development of a standardized set of CHD and self-management–related outcome measures would solve this problem. In addition, only 4 studies25–27,29 reported on objective measures of CHD. That online interventions are commonly tested in “remote” populations (ie, participants sign up online and have no contact with clinicians) may account for this lack of objective data. Although this approach may be cost effective, pragmatic, and consistent with the topic, the disproportionate collection of subjective outcomes, which are more prone to bias,17 may be a flaw in trials of online interventions. In future, trial designers should consider creative ways to obtain objective data concerning CHD status; this should be possible using remote technology.31
Findings to Inform Intervention Design
Evidence for the effectiveness of online interventions for improving mood in CHD was very limited. Four studies23,24,26,27 examined this, but only 1 study24 found a statistically significant improvement in the intervention compared with the control group. This intervention used CBT, which is well known to be effective. Depression and anxiety have been found to be independent predictors of poor cardiac outcomes in CHD,4 so the development of Internet interventions for CHD that also target mood is a priority.
The interventions included in this review varied considerably in terms of their theoretical basis and content, and whether, or how much, they were personalized. All of the interventions included evidence-based behavior change techniques, including 1 or more of goal setting, action planning, biofeedback, and role modeling. This is encouraging; however, more data are required to determine the optimal intensity of their use and the best method of delivery. Only 3 of the included studies23,25,28 described some kind of theoretical basis for the intervention, although in a particular study,28 the authors state that “the content was designed to foster behavioral capability, self-efficacy, social support, and realistic outcome expectations,” which suggests that the intervention was informed by the social cognitive model. The impact of these factors was not tested however. Understanding of the mechanisms by which interventions may be expected to work helps to refine and improve them, hence, those designing interventions are encouraged to report this.32
A systematic review11 of more than 550 high-quality studies of a range of interventions to support self-management indicates that building self-efficacy is key to a range of improve outcomes. It is therefore surprising that only 3 trials23,25,27 specifically tested improvements in self-efficacy or its role in mediating other improvements. Future interventions should therefore include components to promote self-efficacy, and trials should aim to identify the most effective methods. The role of other mediating and moderating variables should also be investigated as this review has identified a lack of data concerning this.
There was some indication that the use of personalization and support to increase engagement may increase the effectiveness of interventions. Further research is needed to test this, but this is supported by previous meta-analytic research in depressed or anxious people without CHD.33 A trial of online CBT plus a trained supporter who provided personalized feedback and encouragement to engage found a 3-fold increase in engagement and a 3-fold decrease in dropout rates compared with unsupported online therapy interventions.34
Strengths and Limitations of the Review
We conducted a systematic and comprehensive literature search that identified published trials and protocols that test Internet-delivered CHD self-management support for physical and mental health. However, we did not search for unpublished trials, which may provide additional evidence. For some of the included trials, data were missing for some reported outcomes; we did not contact authors to try to obtain these data.
Conclusion
Internet-delivered CHD self-management support for improving CHD and self-management–related outcomes is potentially effective, but existing trial evidence is insufficient to draw definitive conclusions. More trials are currently underway. Future research should involve well-designed RCTs, which are adequately reported. In particular, more research is needed to test which intervention components are effective, the theoretical basis by which interventions may work, and the mediating and moderating factors. Effort should be made to determine the intervention’s effect on objectively measured physiological markers of CHD. Trials should test how best to increase patient self-efficacy and how to improve retention of participants and examine the role of personalization and support within interventions.
What’s New and Important
Internet-delivered self-management support for improving CHD, well-being and self-management–related outcomes is potentially effective, but existing trial evidence is insufficient to draw definitive conclusions.
There is a lack of evidence on the impact of such interventions on objectively measured outcomes.
Future well-designed trials should test how interventions work, how to improve retention of participants, and the impact of personalization and support.
APPENDIX.
Search Strategy
Footnotes
This work was funded by NHS England under their Small Business Research Initiative.
Conflicts of interest: G.L., A.C., I.J.N., D.R., and E.A.B. are involved in the development of an Internet-delivered intervention for people with cardiovascular disease and psychological distress (Space From Heart Disease). This review was conducted to inform that work.
REFERENCES
- 1.Townsend NWK, Bhatnagar P, Smolina K, et al. Coronary Heart Disease Statistics 2012 Edition. London, England: British Heart Foundation; 2012. [Google Scholar]
- 2.Frasure-Smith N, Lespérance F. Depression and cardiac risk: present status and future directions. Postgrad Med J. 2010;86(1014):193–196. [DOI] [PubMed] [Google Scholar]
- 3.Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058 doi:10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walters P, Barley EA, Mann A, Phillips R, Tylee A. Depression in primary care patients with coronary heart disease: Baseline findings from the UPBEAT UK study. PLoS One. 2014;9(6):e98342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee G, Dix S, Mitra B, Coleridge J, Cameron P. The efficacy and safety of a chest pain protocol for short stay unit patients: a one year follow-up. Eur J Cardiovasc Nurs. 2015;14(5):416–422. [DOI] [PubMed] [Google Scholar]
- 6.Marks EM, Chambers JB, Russell V, Bryan L, Hunter MS. The rapid access chest pain clinic: unmet distress and disability. QJM. 2014;107(6):429–434. [DOI] [PubMed] [Google Scholar]
- 7.Kroenke K. Patients presenting with somatic complaints: epidemiology, psychiatric comorbidity and management. Int J Methods Psychiatr Res. 2003;12(1):34–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davidson KW, Kupfer DJ, Bigger JT, et al. Assessment and treatment of depression in patients with cardiovascular disease: National Heart, Lung, and Blood Institute working group report. Ann Behav Med. 2006;32(2):121–126. [DOI] [PubMed] [Google Scholar]
- 9.Rutledge T, Redwine LS, Linke SE, Mills PJ. A meta-analysis of mental health treatments and cardiac rehabilitation for improving clinical outcomes and depression among patients with coronary heart disease. Psychosom Med. 2013;75(4):335–349. [DOI] [PubMed] [Google Scholar]
- 10.Department of Health. Cardiovascular Disease Outcomes Strategy. Improving Outcomes for People With or at Risk of Cardiovascular Disease. London: Department of Health; 2013. [Google Scholar]
- 11.Janssen V, De Gucht V, Dusseldorp E, Maes S. Lifestyle modification programmes for patients with coronary heart disease: a systematic review and meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2013;20(4):620–640. [DOI] [PubMed] [Google Scholar]
- 12.Barley EA, Walters P, Haddad M, et al. The UPBEAT nurse-delivered personalized care intervention for people with coronary heart disease who report current chest pain and depression: a randomised controlled pilot study. PLoS One. 2014;9(6):e98704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Silva D. Evidence: Helping People Help Themselves. London, United Kingdom: The Health Foundation; 2011. [Google Scholar]
- 14.Laplante C, Peng W. A systematic review of e-health interventions for physical activity: an analysis of study design, intervention characteristics, and outcomes. Telemed J E Health. 2011;17(7):509–523. [DOI] [PubMed] [Google Scholar]
- 15.Fanning J, Mullen SP, McAuley E. Increasing physical activity with mobile devices: a meta-analysis. J Med Internet Res. 2012;14(6):e161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lustria ML, Noar SM, Cortese J, Van Stee SK, Glueckauf RL, Lee J. A meta-analysis of Web-delivered tailored health behavior change interventions. J Health Commun. 2013;18(9):1039–1069. [DOI] [PubMed] [Google Scholar]
- 17.Samoocha D, Bruinvels DJ, Elbers NA, Anema JR, van der Beek AJ. Effectiveness of Web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res. 2010;12(2):e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Devi R, Singh SJ, Powell J, Fulton EA, Igbinedion E, Rees K. Internet-based interventions for the secondary prevention of coronary heart disease. Cochrane Database Syst Rev. 2015;12:CD009386 doi:10.1002/14651858.CD009386.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richards D, Richardson T. Computer-based psychological treatments for depression: A systematic review and meta-analysis. Clin Psychol Rev. 2012;32(4):329–342. doi:10.1016/j.cpr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Cuijpers P, Marks IM, van Straten A, Cavanagh K, Gega L, Andersson G. Computer-aided psychotherapy for anxiety disorders: a meta-analytic review. Cogn Behav Ther. 2009;38(2):66–82. [DOI] [PubMed] [Google Scholar]
- 21. Thomson Reuters. Endnote. Clarivate Analytics; 2014. http://endnote.com/product-details.
- 22.Higgins JPT, Green S. eds. Cochrane Handbook for Systematic Reviews of Interventions. Sussex, England: John Wiley & Sons Ltd.; 2009. [Google Scholar]
- 23.Antypas K, Wangberg SC. An Internet- and mobile-based tailored intervention to enhance maintenance of physical activity after cardiac rehabilitation: short-term results of a randomized controlled trial. J Med Internet Res. 2014;16(3):e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glozier N, Christensen H, Naismith S, et al. Internet-delivered cognitive behavioural therapy for adults with mild to moderate depression and high cardiovascular disease risks: a randomised attention-controlled trial. PLoS One. 2013;8(3):e59139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maddison R, Pfaeffli L, Whittaker R, et al. A mobile phone intervention increases physical activity in people with cardiovascular disease: Results from the HEART randomized controlled trial. Eur J Prev Cardiol. 2015;22(6):701–709. [DOI] [PubMed] [Google Scholar]
- 26.Varnfield M, Karunanithi M, Lee CK, et al. Smartphone-based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: results from a randomised controlled trial. Heart. 2014;100(22):1770–1779. [DOI] [PubMed] [Google Scholar]
- 27.Devi R, Powell J, Singh S. A Web-based program improves physical activity outcomes in a primary care angina population: randomized controlled trial. J Med Internet Res. 2014;16(9):e186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reid RD, Morrin LI, Beaton LJ, et al. Randomized trial of an Internet-based computer-tailored expert system for physical activity in patients with heart disease. Eur J Prev Cardiol. 2012;19(6):1357–1364. [DOI] [PubMed] [Google Scholar]
- 29.Southard BH, Southard DR, Nuckolls J. Clinical trial of an Internet-based case management system for secondary prevention of heart disease. J Cardiopulm Rehabil. 2003;23(5):341–348. [DOI] [PubMed] [Google Scholar]
- 30.Schulz KF, Altman DG, Moher D; for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Ann Int Med. 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barley E. Care at the click of a button. Nurs Stand. 2014;28(43):64–65. [DOI] [PubMed] [Google Scholar]
- 32.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: Template for Intervention Description and Replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
- 33.Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One. 2010;5(10):e13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doherty G, Sharry J. Engagement with online health interventions: An explanatory study of a treatment for depression. Human Factors in Computing Systems Conference Proceedings; 2012; Austin, Texas.


