Abstract
Providing end-of-life care to patients suffering from chronic kidney disease (CKD) and/or end-stage renal disease often presents ethical challenges to families and health care providers. However, as the conditions these patients present with are multifaceted in nature, so should be the approach when determining prognosis and treatment strategies for this patient population. Having an interdisciplinary palliative team in place to address any concerns that may arise during conversations related to end-of-life care encourages effective communication between the patient, the family and the medical team. Through the use of a case study, the authors demonstrate how an interdisciplinary palliative team can be used to make decisions that satisfy the patient's and the medical team's desires for end-of-life care.
Keywords: palliative care, ESRD, ethics, interdisciplinary, quality of life
Introduction
Today's medical technology along with continuous advancement in medical interventions is allowing patients to live longer than 65 years of age. Over the next few decades, the number of people >65 years old is estimated to increase by a factor of three [1]. In addition, the prevalence of chronic kidney disease (CKD) reaching end-stage renal disease (ESRD) increases with age. Approximately 40% of patients >75 years of age are affected by CKD, and dialysis initiation is highest in patients ≥65 years of age [2]. Many patients who receive dialysis also suffer from multiple comorbidities [3–5], and 1-year mortality rates following initiation of dialysis is 41% in patients ≥75 years of age [6]. Dialysis patients often report feeling less independent, unable to participate in activities they enjoy and have an overall decline in functional status and quality of life [7].
Within this patient population, withdrawal from dialysis is associated with an increased mortality in ESRD patients [7]. No standardized criteria exist to guide how to approach patients with this option. Several patient factors are associated with the dialysis withdrawal decision, including advanced age, white race, low Karnofsky score, high comorbidity burden, female gender, higher physical discomfort index, educational level and late referral to a nephrologist [8–11].
The prognosis and outcome of this particular patient population is both heterogeneous and often difficult to predict. This unknown aspect of medicine can be emotionally taxing on the patient and his/her family and presents unique medical and ethical challenges as well to the treating physicians. End-of-life care is multifaceted and requires a biopsychosocial spiritual approach to patient health. In this review we will use a case example to demonstrate the role of an interdisciplinary palliative team and provide an ethical framework for decision making during end-of-life care.
This patient has been diagnosed with end-stage congestive heart failure(CHF) and dilated cardiomyopathy with an ejection fraction of 15% and no cardiac intervention on behalf of the cardiology team. In addition, she has end-stage renal disease (ESRD) and is undergoing hemodialysis (HD). There is no history of other comorbidities. However, due to reoccurring hemodynamic instability during HD, she has been hospitalized multiple times. There is evidence of a decline in performance status, she is alert, oriented, full code and there are no advanced directives. Mrs. M has been experiencing increased fatigue and shortness of breath for which she refuses medication. Moreover, she wishes to continue with HD as long as possible and declines home palliative medicine and/or hospice services. With respect to her family, she has an ex-husband and a son, with the ex-husband being more involved than the son with respect to Mrs. M's care, but not excessively active.
An interdisciplinary team meeting was planned with Mrs. M, her ex-husband and a cardiologist, nephrologist, palliative medicine specialist, bioethicist, case manager and nurse in order to come to an understanding with respect to her prognosis. It was explained to Mrs. M and her ex-husband about the continued difficulties with dialysis and decline of her heart function. Mrs. M was given the option of home hospice care and its goals were explained, but she is afraid of dying. Both Mrs. M and her ex-husband are determined to continue dialysis as long as possible. Based on her response to the information provided, the following disposition options were offered: transition to in-home or in-facility hospice care, transfer to a local skilled nursing facility and receive outpatient dialysis treatments or transfer to a long-term acute care (LTAC) facility and receive in-facility dialysis. The patient decided to look into transitioning to an LTAC facility. Following the family meeting, a social worker met with Mrs. M, who expressed her concerns with her heart, and Mr. M, who thought that if she went to an LTAC, dialysis could be performed there. Outside of the room, Mr. M expressed his concern with finances for the funeral, the strained relationship between Mrs. M and her son and the inability to care for her at home, as well as anxiety about the new facility. Mrs. M was accepted at the local LTAC facility and planned for discharge the next day.
The following day Mrs. M underwent dialysis in the morning for 4 h, but was unable to complete it due to hemodynamic compromise. The nephrologist overseeing Mrs. M's care determined that she will be unable to receive dialysis at the local outpatient clinic because the risks outweigh the benefits. Both the cardiologist and the nephrologist, after discussing with Mrs. M and her ex-husband, agreed that HD put her at unnecessary risk and will no longer be offered. After this decision, it is agreed that Mrs. M will go to inpatient hospice. The next morning, Mrs. M died due to hemodynamic perturbation.
Case presentation: Mrs. M (female; 70 years old; African American)
We propose an approach to advance care planning in ESRD in older adults that involves an interdisciplinary team and asking important questions during the disease process, starting with CKD (Figure 1). Psychosocial, religious and spiritual issues and beliefs drive patient preferences, competency and understanding with respect to expectations regarding quantity and quality of life. In addition, comprehension of the goal of care by the staff, patient and family is imperative to provide the best possible patient care. When faced with requests to provide intervention(s) that cannot accomplish the intended physiological goals, clinicians should seek to understand the reasons underlying such requests. Although it is generally accepted that palliative care is pertinent for geriatric patients with nonmalignant life-threatening illnesses, current evidence suggests that symptom control, psychosocial and family support, informed and open communication and the opportunity to voice a choice at end-of-life is not satisfied [12]. In these circumstances the patients feel a loss of security and/or control of their identity to their illness [13].
Figure 1:
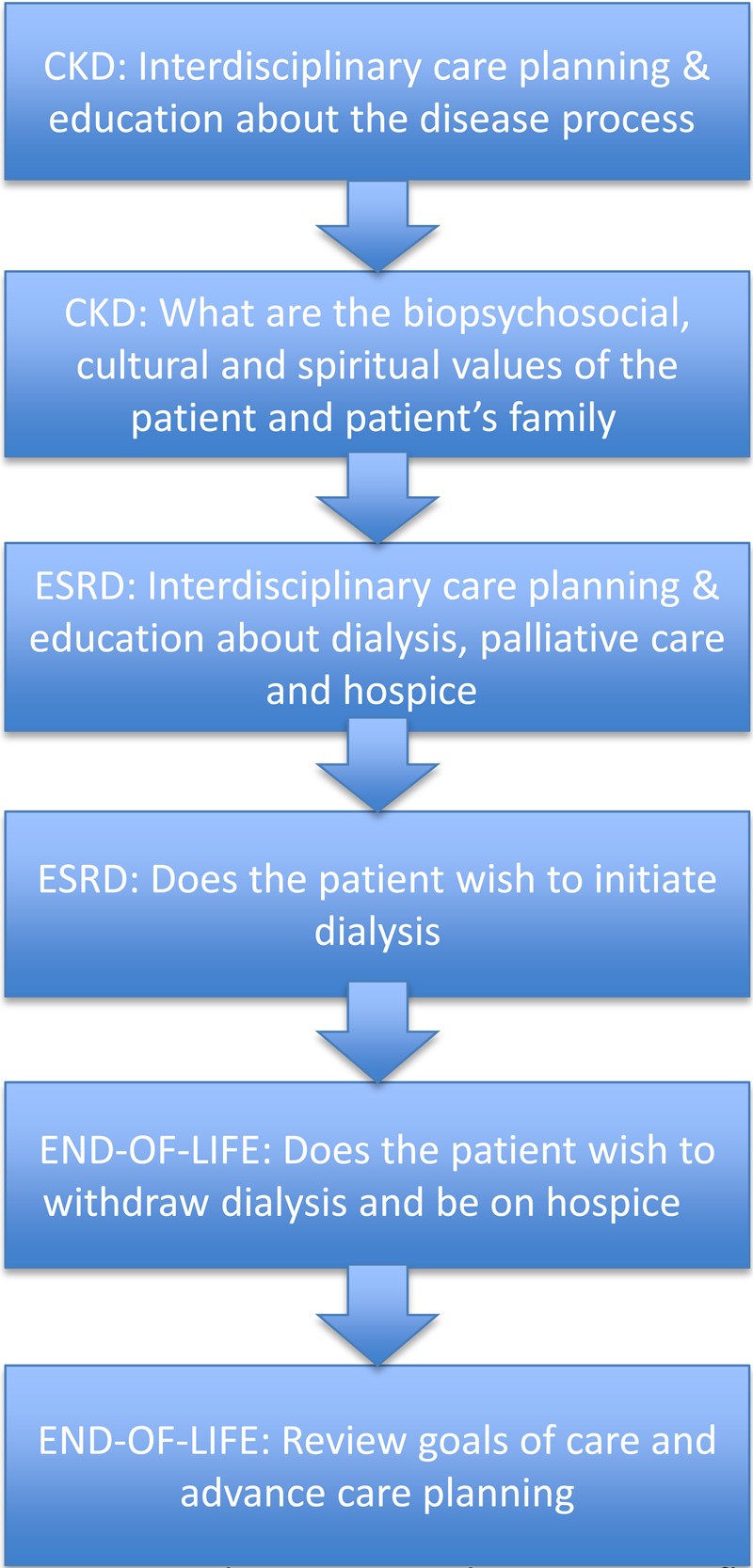
Proposed question and intervention flow chart for approaching palliative care and hospice in CKD and ESRD through the end of life.
Increased attention and study has been devoted to understanding culture as it relates to death and dying [14–16] and in exploring the relationship of culture and its influence on the end-of-life [17–20]. Effective end-of-life communication is one that is ‘culturally sensitive’ to the patient's individual ethnic, cultural and religious values. It may involve including the patient's clergy or a professional chaplain or simply asking the patient what cultural or religious values are important to them regarding their end-of-life care. Such communication, which takes into consideration a patient's culture and religious values, is pivotal to ensure the patient's understanding of their medical condition and what care and treatment options are available to them [21]. This approach encourages patient participation in decision making, while demonstrating ‘cultural sensitivity’ by health care professionals, which is an important factor determining the level of patient satisfaction and those overseeing their end-of-life care [22]. In addition, the patient's family also plays an important role in this process. There are generally two types of families that have been observed in these end-of-life circumstances. The first is a family that appears to function well together, providing appropriate support and able to achieve conflict resolution. This type of family, with high levels of encouragement and unity, tends to present with decreased levels of psychosocial morbidity [13]. The second type of family tends to be more hostile and ill-tempered. Those families in between both extreme family types are commonly associated with increasing distress levels and poor social adjustment [13]. A lack of support on behalf of the family may strongly influence the well-being of the patient and be a powerful morbidity risk factor. Involvement of consultants or ancillary services, such as palliative care or ethics consultants or hospital chaplains, may be helpful during these discussions.
When there is no consensus
If this approach does not lead to a consensus or if there is any uncertainty on futility as expressed by any member of the interdisciplinary treatment team, clinicians should seek a second opinion from a qualified and independent provider. In the case of Mrs. M, the risk of HD treatment outweighed the benefits. Whether treatment is considered medically futile is difficult because whoever defines the situational futility often skews it to meet their point of view [23]. Deciding to continue or cease dialysis in patients that are deteriorating clinically is particularly challenging for nephrologists when the patient no longer possesses the capacity to make decisions [7]. The lack of advance care is all too common.
There is widespread agreement that clinicians are not obligated to provide futile treatments. When examining physiologic futility, the efficacy of the treatment and/or technology is assessed for its ability to fulfill its intended purpose in a given patient [23]. With respect to HD, it must be determined whether it is adequately replacing the patient's renal function. This presents an interesting dynamic between the opportunity to extend life and the obligation to extend life. Providing futile therapy goes against the ethical obligation of physicians to act to benefit their patients and to refrain from harming them [24]. For most dialysis patients, the quality of their lives determines their acceptance or rejection of medical interventions to prolong life. Because the quality of their lives changes, their goals for care and treatment change [25].
Discussion
CKD and ESRD patients wish to be aware of all treatment choices (i.e. symptom management and option to withdrawal), but often information regarding these choices is not always accessible [2, 26]. According to Davison et al. [2], 61% of the patients evaluated felt that their decision to begin dialysis treatment was determined based on their physician or family's preference, and they later regretted this choice [2]. This speaks to the importance of providing care that focuses on ‘individual preferences and values’, which may or may not be in line with the person's ethnic or religious culture or with the patient's family values. It should be remembered that even medicine is a ‘cultural system’ with its own language, values and practices. As health care providers it is important that we do our own ‘cultural assessment’ to better understand how our cultural world view affects our relationship with patients and our ability to deliver unbiased culturally sensitive care. In a qualitative study with ‘semi structured interviews’, Tonkin-Crine et al. [27] addressed the issue of dialysis versus conservative management in older patients with chronic kidney failure in the UK. The mean age of these patients was 82 years, with an overall range of 74–92 years [27]. There were four themes that emerged from the interviews (i) patients' understanding of the management of CKD, (ii) patients, perceptions of their own CKD, (iii) patients, experiences of making a management decision about their CKD and (iv) patients' experiences revising management decisions [27]. Results showed that a distinct difference emerged among dialysis patients and conservative management patients in expectations of living longer and experiencing a better or worse quality of life [27]. In addition, the staff treating these patients had a strong influence on the views of the patients with respect to their treatment and treatment options. It appeared that a small number of patients who chose conservative management had been informed about expected disease or progression [27]. Patients that initially chose conservative management often were not adequately informed on how their disease would progress. In turn, when these patients began to experience negative effects from their illness, they opted for alternative treatment [27]. This study was unique because it provided insight into how influential those caring for ESRD and CKD patients are. Furthermore, when inadequate information was provided to these patients, an informed decision that put the patients comfort and desires at the forefront of the care plan could not be made [27].
It has been observed that despite an annual mortality rate of >20%, dialysis patients are half as likely to receive hospice services compared with other hospice diagnoses [28]. In light of the previously mentioned study, inadequate and delayed education of CKD and ESRD patients on their disease progression clearly is a factor in causing underutilization of hospice services and has been attributed to deficiencies in training nephrologists and other members of the interdisciplinary team in advance care planning and end-of-life counseling [29]. These training deficiencies suggest a greater need for interdisciplinary training and the need for earlier and more frequent discussions of advance care planning and end-of-life counseling with CKD and ESRD patients (Table 1).
Table 1.
Ways to improve advance care planning for patients with CKD and ESRD
| Disease stage | Ways to improve advance care planning |
|---|---|
| CKD |
|
| ESRD |
|
| End of life |
|
Many comorbidities and complexities are present when caring for geriatric patients, including visual impairment, hearing loss, social issues, financial problems, malnutrition, isolation, altered cognitive function, etc. [1]. However, these comorbidities and complexities need to be taken into consideration when constructing a palliative care plan for ESRD and CKD patients that require end-of-life care. Advanced care planning is necessary in these patients, because much like the progression of ESRD, it is patient-specific and is susceptible to change based on patient outcome [25]. Currently, health care in the USA is not formatted in a way that patients receiving end-of-life care are efficiently managed [23]. Although the benefit of continuing treatment can be approached in an economic manner, it should not be the primary determining factor when deciding whether or not care is futile [23]. When attempting to determine treatment goals and prognosis for ESRD patients, factors such as age, frailty and comorbidity may be more predictive [6]. Even though the goal is to provide a more patient-centered care plan, it is necessary to educate nephrologists and other medical staff on how to effectively communicate and address all concerns with these patients and their families [6].
To emphasize advance care planning and prognosis sharing with CKD/ESRD patients and their families, the Renal Physicians Association developed guidelines in 2010 [30]. The key recommendations, which help in shared decision making, include (i) build a good rapport between the doctor and patient; (ii) thorough education of patients regarding their diagnosis, prognosis and available treatment options; (iii) share the prognosis estimate with the patient pertinent to their overall condition; (iv) initiate advance care planning—interdisciplinary team discussion with the patient and family in order to get written advance directives and to encourage patients with decision-making capacity to designate their legal agent; (v) do not initiate dialysis in patients with very poor prognostic conditions like advanced dementia, severe hypotension, age >75 years or CKD stage 5 with high comorbidity score/significantly impaired functional status/severe chronic malnutrition; (vi) provide a time-bound trial of dialysis for patients who require it or with uncertain prognosis or in a situation where consensus cannot be reached about dialysis—discussion should be held between the nephrologist, patient, designated legal agent and the patient's family; (vii) resolve conflicts with regards to dialysis—use a methodical approach to resolve conflicts arising within the health care provider team or between the renal care team and the patient/designated legal agent; (viii) provide palliative care services and interventions to patients experiencing disease complications—a multidisciplinary team should be involved to address physical, psychosocial and spiritual aspects, including end-of-life care for patients who opt out/refuse/discontinue dialysis; (ix) use a methodical multidisciplinary empathetic approach to share the diagnosis, prognosis, treatment options and goals of care with patients, designated legal agents and their families [30].
In a study on advance care planning involving patients and family/friends from dialysis units, it is found that poor communication with the nephrologists/dialysis team and diminished trust may adversely affect advance care planning discussions [31]. A study by Amro et al. [32] revealed that advance care planning in high-risk HD subjects was associated with a better understanding of end-of-life management options. In this study, selected high-risk HD patients were educated on advance care planning by nephrologists, resulting in remarkable changes in documented end-of-life care preferences. Eneanya et al. [33] designed a multicenter prospective cohort compared with a retrospective cohort to test the impact of the ‘Shared Decision-Making Renal Supportive Care’ (SDM-RSC) communication intervention on end-of-life care in ESRD patients who are on HD and at increased risk of death. This study involves interdisciplinary approach comprised of trained nephrologists and social workers sharing prognosis and advance care planning in one-on-one meetings with ESRD patients and their families. Regular monthly meetings with a social worker follow thereafter for a period of 18 months regarding additional support, patient education and hospice care. We await the results of this study to see whether SDM-RSC communication intervention improves end-of-life care outcomes in ESRD patients.
Honoring cultural diversity at the end of life can also be a balancing act between cultural sensitivity and ethical practice. Supporting patients' cultural values and beliefs is an important part of ‘starting with the client.’ On the other hand, there may be times when health care professionals have to use their ethical decision-making skills as they balance respect and acceptance of cultural practices while upholding established federal regulations about informed consent, such as the Patient Self-Determination Act. Genuine and respectful conversations with patients and families about these dilemmas are essential to exchanging information about cultural differences and creating collaborative partnerships. Demonstrating sincere cultural curiosity is of tremendous value in furthering our understanding of the patients' cultural values and beliefs regarding end-of-life care [34].
Conclusion
Since there are many factors that determine an ESRD patient's decision to withdrawal from dialysis, it is the goal of the palliative care team to address these issues. By establishing a common goal to meet the biopsychosocial, cultural and spiritual values of the patient, the patient's family and his/her care team will be able to make decisions that benefit the patient. Therefore, utilizing an interdisciplinary team (nephrologist, palliative medicine specialist, social worker, nurses, case management, etc.) will help address any previously unmet concerns held by the patient and/or the patient's family. Resolution of ethical issues at the end of life in patients with ESRD involves interdisciplinary care and multiple discussions about the disease process that ideally should begin before dialysis is needed. This case illustrates the complex issues involved in reaching a consensus between the ESRD patient with multiple comorbidities and the health care team. No matter how diverse the community or how advanced the health care setting, the needs, preferences and values of the patient and family (cultural sensitivity), blended with today's knowledge of medical science and technology, will continue to be at the core of ethical decision making at the end of life.
Conflict of interests statement
None declared.
References
- 1. Fassett RG. Current and emerging treatment options for the elderly patient with chronic kidney disease. Clin Interv Aging 2014; 9: 191–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Davison CM, Kahwa E, Atkinson U et al. . Ethical challenges and opportunities for nurses in HIV and AIDS community-based participatory research in Jamaica. J Empir Res Hum Res Ethics 2013; 8: 55–67 [DOI] [PubMed] [Google Scholar]
- 3. O'Connor NR, Dougherty M, Harris PS et al. . Survival after dialysis discontinuation and hospice enrollment for ESRD. Clin J Am Soc Nephrol 2013; 8: 2117–2122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lin YT, Wu PH, Kuo MC et al. . High cost and low survival rate in high comorbidity incident elderly hemodialysis patients. PLoS One 2013; 8: e75318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ng Y-Y, Hung YN, Wu SC et al. . Progression in comorbidity before hemodialysis initiation is a valuable predictor of survival in incident patients. Nephrol Dial Transplant 2013; 28: 1005–1012 [DOI] [PubMed] [Google Scholar]
- 6. Vandecasteele SJ, Kurella M. Tamura, A patient-centered vision of care for ESRD: dialysis as a bridging treatment or as a final destination? J Am Soc Nephrol 2014; 25: 1647–1651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schmidt RJ, Moss AH. Dying on dialysis: the case for a dignified withdrawal. Clin J Am Soc Nephrol 2014; 9: 174–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Moss AH. Dialysis decisions and the elderly. Clin Geriatr Med 1994; 10: 463–473 [PubMed] [Google Scholar]
- 9. Bajwa K, Szabo E, Kjellstrand CM. A prospective study of risk factors and decision making in discontinuation of dialysis. Arch Intern Med 1996; 156: 2571–2577 [PubMed] [Google Scholar]
- 10. Murtagh F, Cohen LM, Germain MJ. Dialysis discontinuation: quo vadis? Adv Chronic Kidney Dis 2007; 14: 379–401 [DOI] [PubMed] [Google Scholar]
- 11. Chan HW, Clayton PA, McDonald SP et al. . Risk factors for dialysis withdrawal: an analysis of the Australia and New Zealand Dialysis and Transplant (ANZDATA) Registry, 1999–2008. Clin J Am Soc Nephrol 2012; 7: 775–781 [DOI] [PubMed] [Google Scholar]
- 12. Coventry PA, Grande GE, Richards DA et al. . Prediction of appropriate timing of palliative care for older adults with non-malignant life-threatening disease: a systematic review. Age Ageing 2005; 34: 218–227 [DOI] [PubMed] [Google Scholar]
- 13. Milberg A, Wahlberg R, Krevers B. Patients’ sense of support within the family in the palliative care context: what are the influencing factors? Psychooncology 2014; 23: 1340–1349 [DOI] [PubMed] [Google Scholar]
- 14. Irish DP, Lundquist KF, Nelsen VJ. Ethnic Variations in Dying, Death and Grief: Diversity in Universality. New York: Routledge, 2014. [Google Scholar]
- 15. Parkes CM, Laungani P, Young W. Death and Bereavement Across Cultures. New York: Routledge, 2003. [Google Scholar]
- 16. Parry JK, Ryan AS. A Cross-Cultural Look at Death, Dying, and Religion. Chicago: Nelson-Hall, 1995. [Google Scholar]
- 17. Braun KL, Karel H, Zir A. Family response to end-of-life education: differences by ethnicity and stage of caregiving. Am J Hosp Palliat Med 2006; 23: 269–276 [DOI] [PubMed] [Google Scholar]
- 18. Braun KL, Pietsch JH, Blanchette PL. Cultural Issues in End-of-Life Decision Making. Thousand Oaks, CA: Sage, 1999. [Google Scholar]
- 19. Kemp C, Bhungalia S. Culture and the end of life: A review of major world religions. J Hosp Palliat Nurs 2002; 4: 235–242 [Google Scholar]
- 20. Lopez S, Katz R, Johnson T. The Influence of Culture and Ethnicity on End-of-Life Care. When Professionals Weep: Emotional and Counter-Transference Responses in end-of-Life Care. New York: Routledge, 2006, 91–102 [Google Scholar]
- 21. Grossman D, Rootenberg M, Perri GA et al. . Enhancing communication in end-of-life care: a clinical tool translating between the Clinical Frailty Scale and the Palliative Performance Scale. J Am Geriatr Soc 2014; 62: 1562–1567 [DOI] [PubMed] [Google Scholar]
- 22. Evans N, Costantini M, Pasman HR et al. . End-of-life communication: a retrospective survey of representative general practitioner networks in four countries. J Pain Symptom Manage 2014; 47: 604–619 e3 [DOI] [PubMed] [Google Scholar]
- 23. Swetz KM, Burkle CM, Berge KH et al. . Ten common questions (and their answers) on medical futility. Mayo Clin Proc 2014; 89: 943–959 [DOI] [PubMed] [Google Scholar]
- 24. Thorsteinsdottir B, Swetz KM, Tilburt JC. Dialysis in the frail elderly—a current ethical problem, an impending ethical crisis. J Gen Intern Med 2013; 28: 1511–1516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Holley JL. Advance care planning in CKD/ESRD: an evolving process. Clin J Am Soc Nephrol 2012; 7: 1033–1038 [DOI] [PubMed] [Google Scholar]
- 26. Koncicki HM, Swidler MA. Decision making in elderly patients with advanced kidney disease. Clin Geriatr Med 2013; 29: 641–655 [DOI] [PubMed] [Google Scholar]
- 27. Tonkin-Crine S, Okamoto I, Leydon GM et al. . Understanding by older patients of dialysis and conservative management for chronic kidney failure. Am J Kidney Dis 2015; 65: 443–450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Murray AM, Arko C, Chen SC et al. . Use of hospice in the United States dialysis population. Clin J Am Soc Nephrol 2006; 1: 1248–1255 [DOI] [PubMed] [Google Scholar]
- 29. Schell JO, Holley JL. Opportunities to improve end-of-life care in ESRD. Clin J Am Soc Nephrol 2013; 8: 2028–2030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Renal Physicians Association. Shared Decision-Making in the Appropriate Initiation of and Withdrawal From Dialysis. Clinical Practice Guideline, 2nd ed.Rockville, MD: Renal Physicians Association, 2010. [Google Scholar]
- 31. Goff SL, Eneanya ND, Feinberg R et al. . Advance care planning: a qualitative study of dialysis patients and families. Clin J Am Soc Nephrol 2015; 10: 390–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Amro OW, Ramasamy M, Strom JA et al. . Nephrologist-facilitated advance care planning for hemodialysis patients: a quality improvement project. Am J Kidney Dis 2016; 68: 103–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Eneanya ND, Goff SL, Martinez T et al. . Shared decision-making in end-stage renal disease: a protocol for a multi-center study of a communication intervention to improve end-of-life care for dialysis patients. BMC Palliat Care 2015; 14: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lopez SA. Honoring cultural diversity at the end of life. Social Work Today 2007; 7: 6. [Google Scholar]


