Abstract
Purpose
There is a need to better understand the epidemiological relationship between language development and psychiatric symptomatology. Language development can be particularly impacted by social factors, as seen in the developmental choices made for deaf children which can create language deprivation. A possible mental health syndrome may be present in deaf patients with severe language deprivation.
Methods
Electronic databases were searched to identify publications focusing on language development and mental health in the deaf population. Screening of relevant publications narrowed the search results to 35 publications.
Results
Although there is very limited empirical evidence, there appears to be suggestions of a mental health syndrome by clinicians working with deaf patients. Possible features include language dysfluency, fund of knowledge deficits, and disruptions in thinking, mood, and/or behavior.
Conclusion
The clinical specialty of deaf mental health appears to be struggling with a clinically observed phenomenon that has yet to be empirically investigated and defined within the DSM-5. Descriptions of patients within the clinical setting suggest a language deprivation syndrome. Language development experiences have an epidemiological relationship with psychiatric outcomes in deaf people. This requires more empirical attention and has implications for other populations with behavioral health disparities as well.
Keywords: behavioral health, language deprivation, sign language, hearing loss, social psychiatry
Psychiatric health is often epidemiologically affected by social factors such as poverty, social distress, and prejudice [1–5]. In this review, we argue that language development, or the disruption of language development, is another social factor that contributes to the epidemiology of mental illness – as observed in the deaf population.
In general, people experience hearing loss in different ways. The majority of hearing loss is age-related sensory impairment in people who have achieved language development milestones – namely, post-lingual hearing loss [6]. Those who lose their hearing at birth or during the critical period of language development, pre-lingual hearing loss, are the focus of this discussion. Approximately two to three out of 1,000 children experience pre-lingual hearing loss at birth [7]; in a sample of 37,828 deaf students with known hearing loss onset, at least 55.1% reported hearing problems before the age of two years[8], impacting first language development.
Language Deprivation
Language deprivation occurs due to a chronic lack of full access to a natural language during the critical period of language acquisition (when there is an elevated neurological sensitivity for language development), approximately the first five years of a child’s life [9,10]. Language deprivation during the critical period appears to have permanent consequences for long-term neurological development [11]. Neurological development can be altered to the extent that a deaf child “may be unable to develop language skills sufficient to support fluent communication or serve as a basis for further learning” [12].
Exposure to a fully accessible language has an independent influence on brain development separate from only the auditory experience of hearing loss. Indeed, recent neuroimaging studies indicate the presence of adult neurostructural differences in deaf people based on timing and quality of language access in early childhood [13–15].
Access to spoken language
Medical professionals are not able to assure that hearing aids and cochlear implants will result in positive language outcomes [16]. Many deaf children are significantly delayed in language skills despite their use of cochlear implants. Large-scale longitudinal studies indicate significant variability in cochlear implant-related outcomes when sign language is not used, and there is minimal predictive knowledge of who might and who might not succeed in developing a language foundation using just cochlear implants [17].
For example, a study of 27 French-speaking implanted children found that only half of these children displayed language skills comparable to their hearing peers at the word level and less than half at the sentence level [18]. Long-term language trajectories of 188 implanted children were described as “slower and more variable” than their 97 hearing peers and even those who were implanted earlier than 18 months of age continued to exhibit language delays of more than a year behind their peers [19]. Studies of long-term speech production and perception in 110 implanted children found extreme variability as some demonstrated zero ability to express or perceive spoken English clearly, while others performed nearly as high as 100% accuracy from elementary school to high school [20,21]. Finally, a meta-analysis of 12 studies focusing on spoken language vocabulary found that implanted children had significantly less expressive and receptive vocabulary knowledge than their hearing peers [22].
Access to visual language
In contrast to depending solely on spoken language, another communication option for deaf children is sign language – a fully accessible, visual language for deaf children. Contrary to popular – but uninformed – opinion, sign languages have their own grammars and linguistic rules equivalent to spoken languages [23]. Yet, less than eight percent of deaf children receive regular access to sign language in the home (i.e., fluent, bidirectional conversations) [8]. Although using sign language is encouraged for hearing babies to develop language skills before they can begin to speak, sign language is not routinely offered as a primary or complementary intervention for deaf children [24]. Rather, if offered at all, it is often proposed as a last-resort option to deaf children who have not developed speech abilities as expected [24].
This pattern occurs because many advocates, professionals, and educators believe that sign language acquisition will interfere with deaf children’s development of speech skills [25,26], despite research that has shown that signing implanted children actually demonstrate better speech development, language development, and intelligence scores than non-signing implanted children [20,27,28]. This resistance has been recently described as a prejudice against both sign languages and the state of being deaf [29]. As a result, delayed exposure to sign language is a “common educational occurrence arising from the priority frequently given to speech over sign by rehabilitation professionals and hearing parents” [9]. The end result is that most deaf children do not develop native fluency in sign language.
Based on the current literature, results suggest that technological interventions (e.g., hearing aids, cochlear implants) are insufficient as a stand-alone approach for language acquisition in deaf children. Paired with delayed or absent exposure to sign language during the critical period of language acquisition, a deaf child can be at risk for experiencing long-term language deprivation – which leads to a spectrum of neurological, educational, and developmental consequences across the lifepan. Therefore, many deaf children are likely experiencing some level of language deprivation that might contribute to greater health disparities relative to the general population, such as the increased prevalence of mental illness seen in the deaf population.
Behavioral Health
Deaf individuals experience a higher prevalence of behavioral health concerns than the general population. For example, a study conducted with a community sample of 236 deaf individuals found significantly poorer quality of life and higher levels of emotional distress compared to the general population [30]. Deaf female undergraduates are two times as likely to experience interpersonal trauma [31]. Additionally, a community sample of 308 deaf individuals found elevated reports of lifetime emotional abuse (27.5%), physical abuse (21.0%), and sexual violence (20.8%) [32]. Deaf adolescents can experience emotional and behavioral mental health problems associated with low self-esteem and peer rejection [33], and a range of developmental adversities unique to being deaf in a hearing world such as lack of accessible communication with parents and peers [34].
While overall increased rates of mental health problems and extreme barriers to behavioral health care are reported in the deaf population, early access to family and peer communication are protective factors against these disparities [35]. Indeed, some claim that the higher prevalence of trauma and psychiatric symptoms in the deaf population are partially caused by inappropriate and/or incomplete medical and educational language interventions early in life [36–39,24], which create risk for subsequent language deprivation and behavioral health problems. These associations warrant further research to guide interventions to target these mental health challenges in the deaf population.
The hypothetical existence of a unique mental health syndrome that has a relationship with language deprivation deserves investigation as language difficulties complicate diagnosis and treatment of many deaf patients [38,40–43]. There is a need to help clinicians to differentiate primary and secondary contributors to deaf patients’ mental health issues. The current structured literature review attempts to clarify potential psychiatric symptoms resulting from language deprivation and investigate whether such suggestions of a mental health syndrome exists.
Method
Search Strategy
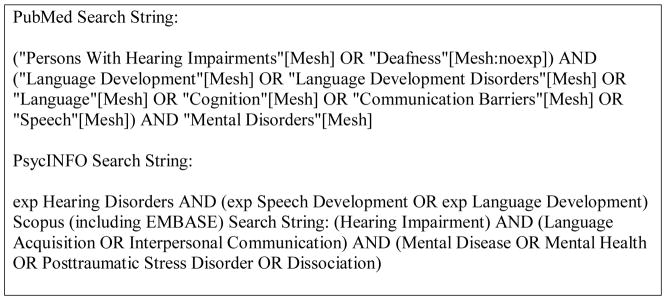
Five indexed databases were used for the literature search to identify articles that discuss the impact of language on mental health in the deaf population: MEDLINE (PubMed interface), PsycINFO (OVID interface), EMBASE (Scopus search engine), CINAHL, and ERIC (EBSCO interface). Searches were iteratively constructed to identify the most effective search terms and syntax. As a major goal was to document the literature over time, the authors looked back as far as possible within each database. No restrictions were placed on types of material to ensure that relevant literature would be included from English-only journals, books, and theses/dissertations. Figure 1 shows the search strategy applied to each database.
Figure 1.
Search strings by database.
Initial searches for the identification stage were conducted in January 2015. Results were imported into the RefWorks citation management database. Using RefWorks’ de-duplication feature, duplicate publications were eliminated. These publications were then exported into Excel.
Inclusion Criteria
Publications needed to meet the following criteria for inclusion in the structured literature review: (a) focus on the deaf population; (b) focus on at least one aspect of language development; and, (c) focus on behavioral health (i.e., mental health or substance use disorder). Due to the complex nature of language development and mental health outcomes, certain publications were accepted without meeting all the criteria if they provided important context.
Abstraction Form
An abstraction form is a standard method of systematically collecting data from literature reviews based on inclusion criteria. Our form elicited the following information about each included study: (1) description of the deaf individuals in the study sample; (2) type of language exposure; (3) type of intervention (where applicable; e.g., cochlear implant, social skills training, cognitive behavioral therapy), and (4) reported mental health/behavioral outcomes.
Search Results
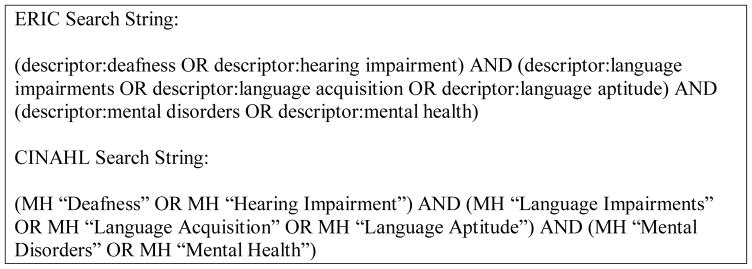
Figure 2 utilizes the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram [44], demonstrating the structured literature review steps up to the full-text review. During the identification stage, 1,505 publications were identified through database searching and 40 additional publications were found through other sources (e.g., Google Scholar, bibliography hand-searching). The screening process eliminated 1,372 publications, the remaining 173 were given full-text reviews. 14 non-English publications were immediately excluded. Upon full-text review, a further 49 publications were excluded. Abstraction forms were used for the remaining 110 full-text publications.
Figure 2.
PRISMA Flow Diagram
Seventy-five full-text publications were excluded during abstraction form review. The remaining 35 full-text publications were included in this paper, forming the basis of the structured literature review. Appendix A details the abstraction form results of the 35 structured literature review publications.
Results
Historical Attempts of Developing Diagnostic Concepts and Terms
Discussions of a potentially unique clinical disorder in the deaf mental health field appear to have begun in the 1960s [45–48]. Psychiatric diagnosis of deaf patients was described as extremely complex and time-consuming [49]. Unfortunately, there has been a general lack of awareness in the psychiatry field towards these unique deaf clinical presentations and features. This led one clinician to describe consistent misdiagnoses and clinical confusion associated with deaf patients as “catastrophic mistakes [leading to] unnecessary and prolonged hospitalizations, placing patients on [unnecessary] powerful psychotropic medications, and the failure to develop appropriate treatment programs or provide needed services” [38].
Various categorical terms were proposed including surdophrenia and primitive personality. The term surdophrenia stems from Basilier’s “Psychic Consequences of Congenital or Early Acquired Deafness” [46] and primitive personality was coined by Altshuler in several early 1960s publications [45] which compared some deaf patients to feral children abandoned in the wild (e.g., The Wild Boy of Aveyron [50]). The general theory behind these terms was that a unique cluster of mental health symptoms (e.g., behavioral issues, cognitive delays, lack of social skills) resulted from unavoidable communication difficulties of deafness (i.e., inadequate exposure to spoken or signed language).
Vernon and Raifman [51] explain their diagnosis of “primitive personality: surdophrenia” as applying to a subpopulation of approximately 5 – 15% of deaf individuals who have a linguistic disability that creates severe cognitive deprivation, as well as psychological naiveté and immaturity. Their suggested criteria include: (1) minimal or total absence of language knowledge (including sign language, English, or other language); (2) functional illiteracy as measured by a standardized educational achievement test; (3) a history of little or no formal education; (4) cognitive deprivation involving little or no knowledge of basics including paying taxes, or following recipes, etc.; and, (5) a performance IQ score of 70 or less.
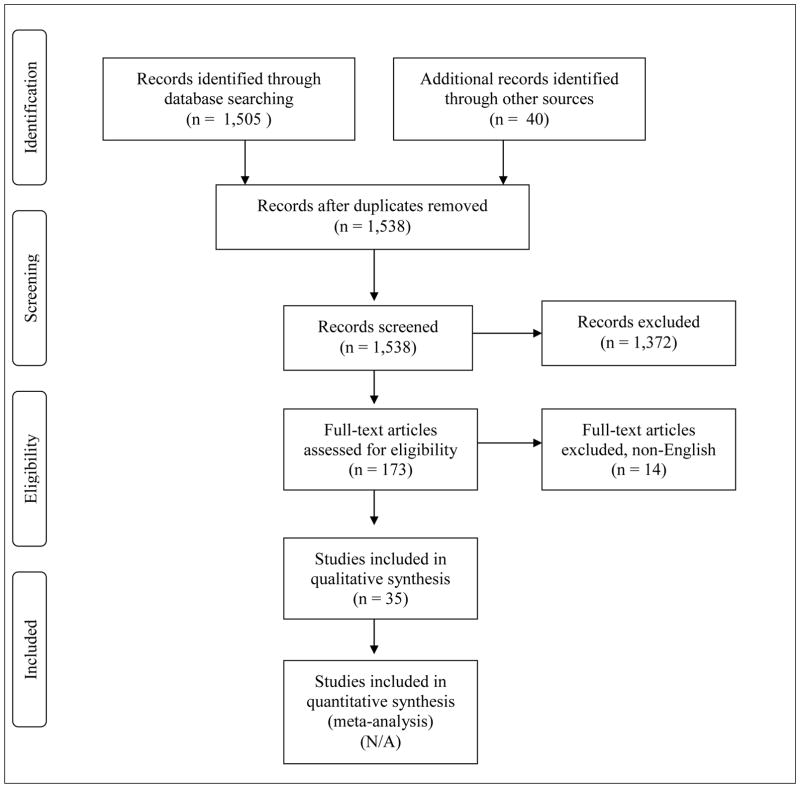
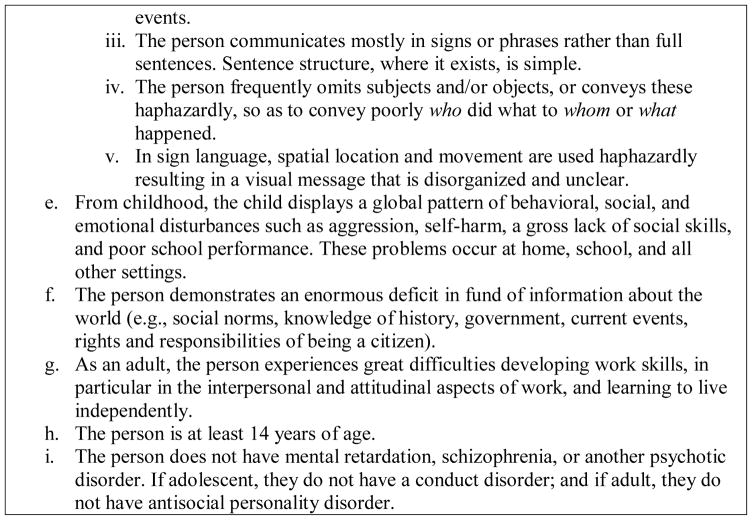
Clinical descriptions of patients often referred to “problem behaviors of deafness,” invariably including some reference to immaturity, impulsiveness, explosiveness, and general lack of skills (e.g., “soft skills”) that promote success in society [49,52]. Since that time, criticism of this sentiment in the literature – in which there appeared to be an underlying belief that these behaviors were actually characteristic of deaf people themselves – has redirected these “problem behaviors of deafness” as a consequence of language deprivation or other adverse developmental experiences [37]. Glickman [41] attempted to address the weaknesses and bias of previous diagnostic attempts by developing his own label and criteria (Figure 3), with the goal of further solidifying a potential diagnostic concept.
Figure 3.
Glickman’s proposed criteria of “language deprivation with deficiencies in behavioral, emotional, and social adjustment.”
Language Dysfluency
Language dysfluency occurs when a person’s best language is considered not fluent [38]. Ironically, although language dysfluency may be more common in deaf people, literature discussing language dysfluency in deaf individuals is extremely limited. Dysfluency may be caused by either language deprivation and/or neurological deficits unrelated to language deprivation, including life events (such as traumatic brain injuries and prenatal illness) and mental illness [53]. It can be more difficult to assess a deaf individual’s psychiatric symptoms due to extremely wide variability in developmental language experiences that lead to variable degrees of language dysfluency in many deaf patients [54]. An inpatient unit serving deaf patients documented a high prevalence of language dysfluency using subjective communication assessments [38,55]. Approximately 75% of patients were found to be language dysfluent, yet only 28% to have a psychotic disorder (compared to 88.9% of hearing inpatients) [55], but the generalizability of these findings is unknown. As a result, many deaf patients appear to be hospitalized not for mental illness, but for the various sequelae related to language deprivation – including language dysfluency – that social and medical systems failed to adequately address. Languages in either modality (auditory or visual) have rules and structures that make them languages; some suggest that language dysfluency may cause disruption in these rules and structures. Descriptions of psychosis-related sign language dysfluency suggest that it follows “classic” symptoms seen in hearing patients including neologisms, clang associations, and content poverty, among others [54,56]. One clinician’s case study of a deaf inpatient with suggested non-psychotic language dysfluency highlights limited vocabulary, lack of time referents, disturbed spatial organization, and lack of syntax as possible key features of language deprivation-related dysfluency in sign language [for a review, see 38]. A language dysfluent patient’s vocabulary may be limited to “concrete objects, actions, and descriptions [a person] has experienced directly...” [38]. While telling a narrative, typical time markers (i.e., day, week, month, year) may be missing. Temporal organization may be extremely disturbed to the point where patients may struggle with general awareness of time. As a three-dimensional visual language, ASL relies heavily on spatial organization and locations (the three-dimensional space in front of a person) as part of its grammar structure to hold and communicate information. However, the language-dysfluent patient established a town in one spatial location then did not refer to it again and subsequently reused that same spatial location for a different town in the same conversation (a violation of ASL grammar), causing confusion to the conversational partner. Overall, language dysfluency is described as resembling a “series of pictures in the present tense, organized loosely as a kind of collage… almost a stream of consciousness” with an emphasis that these features are not a part of psychosis phenomena [38]. While limited to one case study, disturbance of these features likely would make a language dysfluent person struggle with understanding other people and the world around them as well as to be understood.
Fund of Knowledge Deficits
Fund of knowledge deficits (also known as fund of information deficits) are best described as gaps in knowledge due to an “accumulated lack of [environmental] information” [57]. Normal acquisition of passive information is made through media such as radio, newspapers, television, and word of mouth – avenues not always accessible to deaf individuals. Deaf people’s increased risk of deficits in accumulative general knowledge has been noted in the literature for some time [36,49,54,57–61]. For example, a 1970s deaf inpatient unit described their patients as poorly educated “with limited general knowledge” [49]. As such, primary treatment for these patients often consists of “the social skill education that they should have received at home and in school” [38].
Deaf epistemology notes a dinner table syndrome in which deaf children and adults are frequently left out of conversations with hearing family members and friends in many everyday settings, including at home and in school [61]. This consistent lack of exposure to everyday opportunities likely results in an overall loss of understanding of how many aspects of society function, such as school interactions, government functions, healthy personal behaviors, and many others. The dinner table syndrome phenomenon, coupled with the chronic effects of language deprivation and dysfluency, is likely to also exert a significant lifelong impact on deaf individual’s physical, mental, and social health – partially mediated through a chronic lack of health literacy and knowledge [62,63].
Disruptions in Thinking, Mood, and/or Behavior
Deaf patients have been described in the historical psychiatric literature as having more negative personality traits than the general population, such as denial, lack of insight, immaturity, impulsivity, lack of insight, as well as increased rage and aggression [37,48,52,64]. This is echoed by Cooper [59], who proposed that the most common disorders in the deaf psychiatric literature at the time were “problems of behavior and maladjustment apparently related to deafness.” The view of deafness has historically been heavily negative, seemingly attributing various psychiatric symptoms to the experience of being deaf itself. Instead, it is possible that these various observed symptoms are more accurately attributed to language delays. The case study of a patient with language dysfluency [38] specifically mentioned the “inference” of unstructured language implying unstructured thinking, suggesting that gaps in language access create similar gaps in thinking processes. Deaf individuals do generally appear to be at heightened risk for various psychiatric issues compared to the general population [35]. This risk is likely partially magnified due to language deprivation, which is a rarity in the hearing population.
The underlying implication is that deafness – in and of itself – does not create psychiatric symptoms; rather, the influence of language (or lack thereof) on cognition results in such symptoms. This aligns with research suggesting a relationship between psychiatric disorders and speech/language issues in hearing children [65], including a study of adolescent hearing inpatients where most had some type of language impairment [66]. Additionally, a study of deaf individuals with schizophrenia found better linguistic ability (via earlier ages of sign language exposure) to be associated with greater functional outcomes [67]. While there appears to be general agreement on a higher prevalence of psychopathology in deaf patients, this has commonly focused only upon behavior and adjustment issues [36]. Several literature reviews highlight a strong link between language and behavior issues, especially among deaf children [68,69]. A study of 120 oral (speech-only) deaf children suggested that those children with the least developed language abilities had significantly more behavior problems than their hearing peers [68]. Elevated rates of emotional problems and disorders [33] and interpersonal trauma exposure [31,32,34,57] are present, and may have a relationship with language ability [70]. A relationship between language and behavioral health psychopathology appears evident in the deaf population. For a small subset of the population, this psychopathology may be serious enough to require long-lasting care in both outpatient and inpatient settings.
Discussion
The etiology of this possible language deprivation syndrome appears to have sociocultural origins. The language deprivation that deaf people frequently experience is a social occurrence centered around the developmental choices made for them as children [24,36,38,40,71,72]. These developmental choices drastically increase the risk of a “snowball” effect of cognitive and social skills consequences that, in turn, increase the likelihood of mental illness.
Policy Implications
Language deprivation occurs in the deaf population primarily as a function of medical and education policies. These policies are generally created without the inclusion of deaf people and are ones in which sign language has been – and is – excluded as a primary and/or complementary language intervention option for deaf children [12,24,39,47,52,58,72–76]. In sum, “a change in [medical and] education policy provides the most powerful opportunity in preventive psychiatry for deaf people” [37]. Early assessment of language access is crucial; this would increase the likelihood of deaf children reaching appropriate language milestones to maintain a healthy developmental path. Subsequently, immersing deaf children in a rich signing environment would likely reduce the risk of harm associated with language deprivation [24]. Current early childhood education should shift to prioritizing language and cognitive development, not solely speech or spoken language outcomes, especially at the expense of general education and development [74].
Diagnostic Implications
In theory, the arrays of symptoms caused by language deprivation are not unique to only the deaf population. A hearing person who experiences similar deprivation in their early childhood (such as the famous case of “Genie” [77]) may present with similar symptoms. In contrast to the everyday occurrence for deaf children, for hearing children to experience similar consequences of language deprivation requires extreme situations of neglect and/or abuse. In essence, “there is no such thing as a typical deaf personality” [36]; rather, there is likely a typical presentation of extreme language deprivation in a subset of the deaf population that requires extensive psychiatric care. The clinical specialty of deaf mental health is struggling with the inadequacy of existing Diagnostic and Statistical Manual of Mental Disorders 5 diagnoses (DSM-5) to capture an observed clinical phenomenon, and to not only define it but also obtain legitimate psychiatric recognition. The DSM-5 group of neurodevelopmental disorders [78] contains diagnoses that may describe specific observed symptoms (e.g., intellectual disability, language disorder, social communication disorder, specific learning disorder), but using multiple diagnoses to explain one condition is both inefficient and inappropriate.
Proposed diagnostic concept
Although an agreed-upon diagnostic label continues to escape the field, deaf people and professionals frequently encounter the consequences associated with developmental experiences of language deprivation [40]. Glickman [79] describes the most commonly-used term as “low functioning deaf.” The vocational rehabilitation field offers its own description – a “traditionally underserved person who is deaf,” a subset of deaf people who exhibit limited communication abilities, difficulty maintaining employment without assistance or support, poor social/emotional skills including problem-solving, impulsivity, low frustration tolerance, inappropriately aggressive, and inability to live independently [60]. We recommend the term “language deprivation syndrome” [40,42,43] to highlight the possible cluster of symptoms that result from language deprivation. There is not enough empirical evidence to currently formulate formal diagnostic criteria, but there appears to be a need to begin empirically developing these criteria. Potential diagnostic concept areas needing empirical attention include language dysfluency, fund of knowledge deficits, and disruptions in thinking, mood, and behavior. Empirically-supported recognition would also help deaf individuals interacting with mental health and legal systems, and identify areas to intervene for systematic prevention (e.g., medical and education systems) [38]. Research focused on the deaf population is severely lacking and needs to be prioritized, especially on the topic of language deprivation and its associated mental health issues. Future research directions should especially consider how to measure sign language dysfluency, the role of behavioral problems in diagnosis, and the potential existence of other clinical comorbidities (e.g., conduct disorder, antisocial personality disorder).
Limitations
Although the results of our review suggest a possible language deprivation syndrome, there are some limitations to our findings. The reviewed literature included only those articles that were written or translated into English, due to the authors’ lack of fluency in other languages. This means potentially relevant publications in other languages are not captured here. Additionally, the literature is lacking empirical evidence – this is likely due to the clinical priorities of many of the authors, and the lack of existing deaf research methodology to quantify their observations (a problem that still exists today), among other possible reasons. Finally, there is a historically prevalent negative, biased view of deafness that may have influenced psychiatric descriptions of character traits attributed to deaf people.
Conclusion
Results from the current structured literature review suggest that there is critical need for further empirical and clinical attention on a possible language deprivation syndrome. This attention may eventually lead to formal diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders. What appears to be a recognized everyday occurrence in the deaf mental health field and the Deaf community (i.e., “low functioning deaf” [79]) has not garnered significant attention in the general community. Language exposure has an inextricable impact on one’s development across the lifespan. Early suggestions of a language deprivation syndrome indicate that it may be a natural consequence of chronic lack of full access to language. This has implications for language development as a social factor influencing the epidemiology of mental health. Although this phenomenon is most obvious in the deaf population, understanding the linkage between language exposure and mental health outcomes also contributes to our broader understanding of behavioral health epidemiology. As such, experiences of language exposure and mental health outcomes in other populations should be given more empirical attention (e.g., low socioeconomic status and immigrants moving to different countries). The socioemotional development of deaf children has been historically described as “delayed” or “developmental retardation” [58,59,80]. These negative descriptions might more accurately describe the development of the language-deprived child, rather than a deaf child. This descriptive shift is powerful in allowing for a change in the general philosophical approach to deaf child development. Language deprivation in deaf children is preventable. Proactive prevention of language deprivation appears to be a much-needed approach, rather than continued attempts to avoid “auditory deprivation” and the subsequent need to provide long-term behavioral health treatment for the most extreme consequences of chronic language deprivation.
Acknowledgments
This work was supported in part by Department of Psychiatry, University of Massachusetts Medical School and grant no. K12 GM106997 from the National Institute of General Medical Sciences of the National Institutes of Health. The authors thank Jacqueline Pransky and Peter Hauser, PhD for insights and feedback during the writing process. The authors specially thank Douglas Ziedonis, MD, MPH for conceptualization assistance and initial sponsorship.
Appendix A STRUCTURED SUMMARIES AND COMMENTARIES
| First author | Type of publication | Deaf individuals | Language exposure | Intervention (if applicable) | Mental health/behavioral outcomes |
|---|---|---|---|---|---|
| Altshuler 1971 USA | Clinical observations (16 years total) | 1,000 New York State inpatients and outpatients | General lack of language exposure during early development | Schizophrenia prevalence comparable to general population, impulsive/aggressive behaviors, less depressive symptoms | |
| Altshuler 1986 USA | Literature review | Literature review | General lack of language exposure during early development | Schizophrenic presentation different in deaf individuals, impulsive/aggressive behaviors common | |
| Anderson 2011 USA | Quantitative study of trauma prevalence | 100 deaf female college students | 75 ASL, 21 English, 4 other | Deaf females approximately two times as likely to experience interpersonal victimization and trauma as hearing females | |
| Anderson 2016 USA | Qualitative study of deaf-unique trauma experiences | 17 deaf trauma survivors | ASL | Some trauma experiences overlap with general population, others are unique to deaf people (i.e., lack of communication with family) | |
| Barker 2009 USA | Analysis of language and behavior problems | 188 families with implanted, deaf children compared to 97 families with hearing children | Spoken English | Cochlear implant | Implanted children evidenced more behavior problems, oral language deficits, and parent-child communication than hearing children |
| Barnett 2011 USA | Literature review and commentary | Literature review and commentary | Limited access to environmental information | Low health literacy and health disparities exist in Deaf sign language populations | |
| Basilier 1964 Norway | Theoretical review | Theoretical review | General lack of language exposure during early development | Associates general experience of deafness with a “deaf personality structure” and stresses a need for specialized psychiatric services | |
| Black 2006 USA | Archival analysis of clinical records | 64 discharged deaf inpatients | 75% of deaf inpatients classified as “language deprived” or “dysfluent due to language deprivation” | Deaf inpatients more likely to present associated behavior issues with language deprivation than a psychotic disorder diagnosis | |
| Cooper 1976 England | Literature review | Literature review | Differences in psychiatric presentation depending on hearing loss onset and severity | Highlights “problems of behavior and maladjustment related to deafness” as most common disorders in psychiatric literature as well as general knowledge deficits especially with early onset | |
| Denmark 1971 England | Literature review | Literature review | Highlights relationship between deafness and psychiatry relating to impoverished language exposure | Personality development of deaf child described as “developmental retardation,” risk of general knowledge deficits | |
| Denmark 1972 England | Describes process and barriers in establishing psychiatric unit for deaf people | 109 deaf inpatients at time of publication | Inpatients generally had poor language exposure, and “educational retardation” | Staff communication in sign language beneficial for treatment, hired teacher for social skills training | Highlights psychiatric diagnosis as complex and time-consuming, describes patients as impulsive and lacking skills |
| Fellinger 2012 Austria | Literature review | Literature review | Connects poor language abilities with behavioral and psychosocial problems | Generally suggests prevalence of mental and behavioral health issues in deaf people to be elevated compared to general population, highlights lack of access to treatment | |
| Gaines 2009 USA | Analysis of language and learning challenges in hearing adolescent inpatients | 34 adolescent hearing inpatients | Generally had native language exposure but poor language skills | Concrete skills development, rather than traditional talk therapies | Poor language skills associated with psychiatric disorders and inpatient hospitalization in hearing adolescents |
| Giddan 1996 USA | Study of speech and language deficits prevalence in preadolescent hearing inpatients | 55 preadolescent hearing inpatients | Native language exposure but clear speech and language deficits | 60% of admitted inpatients had speech and language deficits, most prevalent in those with anxiety and aggressive conduct disorder | |
| Glickman 2007 USA | Case study of deaf inpatient with language dysfluency | Deaf inpatient (“Juanita”) | Little to no education or sign language exposure | In-depth description of language dysfluency features connected to language deprivation | |
| Glickman 2009a USA | Literature review and commentary | Literature review and commentary | Offers diagnostic criteria for “language deprivation with deficiencies in behavioral, emotional, and social adjustment” | Highlights social causes of language deprivation, potential co-morbidity of language deprivation with various behavioral diagnoses | |
| Hauser 2010 USA | Literature review and commentary | Literature review and commentary | Highlights dinner table syndrome and general worldly knowledge deficits | Deaf individuals at risk for physical and mental health issues, less health literacy and knowledge | |
| Horton 2010 USA | Study of sign language ability, cognition and functional status in deaf outpatients with schizophrenia | 34 deaf outpatients with schizophrenia | Earlier sign language exposure associated with greater functional outcomes | Better language ability appears to improve functional outcomes of deaf individuals with schizophrenia | |
| Huber 2011 USA | Quantitative study of mental health status | 32 deaf adolescents with cochlear implant, 212 hearing adolescents | Spoken language | Cochlear implant | Implanted children more likely to experience peer problems, signing ability may have a relationship with emotional problems |
| Kitson 1990 England | Literature review and commentary | Literature review and commentary | General lack of language exposure during early development | Suggests that increased prevalence of mental health issues in deaf people is related to spoken-language policy in their education | |
| Lane 1976 USA | Literature review and commentary | A hearing feral child, the Wild Boy of Aveyron | Raised by animals, delayed exposure to language | Described as “feral” and not being able to behave appropriately according to social norms | |
| Long 1993 USA | Literature review and commentary | Literature review and commentary | Delayed language exposure creates “traditionally underserved” deaf individuals | Limited communication skills, difficulty maintaining employment without support, poor socio-emotional skills, inability to live independently | |
| McKee 2015 USA | Quantitative study of health literacy assessment | 166 deaf individuals and 239 hearing individuals | Health literacy was correlated with reading literacy | 48% of deaf participants had inadequate health literacy, 6.9 times more likely than hearing individuals | |
| Pollard 2014 USA | Quantitative study of intimate partner violence | 308 deaf individuals from Rochester, 162 deaf individuals from national sample, 1,906 hearing individuals from Monroe County, NY | Ranging language experiences | Deaf individuals more likely to experience emotional abuse and forced sex from their partner than hearing individuals | |
| Pollard 1998 USA | Literature review and commentary | Literature review and commentary | Generally highlights delayed language exposure in deaf mental health population | Describes language dysfluency as separate from psychotic symptoms | |
| Rainer 1966 USA | Report of comprehensive mental health services for the deaf in New York State | Literature review and commentary | Generally highlights delayed language exposure in deaf mental health population | Highlights deaf patients not fitting existing diagnostic criteria, discusses “Primitive Personality Disorder” existing in the deaf mental health population | |
| Schenkel 2014 USA | Study of maltreatment and trauma prevalence | 147 deaf college students, 317 hearing college students | Ranging language experiences | Deaf participants more at risk for maltreatment and trauma experiences, general knowledge deficits as well | |
| Sinkkonen 1994 Finland | Dissertation study | 379 deaf students, 234 hearing students | Early exposure for deaf children with signing hearing parents | Found no difference in mental health prevalence between signing deaf and hearing children | |
| Stevenson 2010 USA | Quantitative study of language development and behavior problems | 120 children with hearing loss, 63 hearing children | Spoken English (signing children excluded from analyses) | Cochlear implant in some participants | Children with hearing loss had higher behavior problems, level of problems were highest among those children with least developed language |
| Thacker 1994 England | Quantitative study of sign language use in schizophrenic patients | 30 schizophrenic and 7 maniac deaf adults | British Sign Language as primary means of communication | Formal communication disorder can occur in sign language | |
| van Gent 2011 USA | Quantitative study of psychosocial risk factors | 68 deaf adolescents | Spoken Dutch | Deaf adolescents at risk for self-esteem issues, emotional problems, and hearing peer rejection | |
| Vernon 1969 USA | Book chapter focusing on hearing loss sociological and psychological factors | Literature review and commentary | Discusses delayed language exposure in deaf population | Generally suggests intelligence of deaf people to be comparable to hearing people, highlights social causes of deaf people’s lagging achievement in multiple developmental and educational areas from delayed language exposure | |
| Vernon 1997 USA | Literature review and commentary | Literature review and commentary | Severely delayed language exposure | Suggests “Primitive Personality: Surdophrenia” and potential diagnostic criteria for especially deaf individuals with language deprivation who are placed in the legal system | |
| Vernon 1968 USA | Literature review and commentary | Literature review and commentary | Discusses the deaf population as generally language-delayed | Delayed language exposure leads to defensive mechanisms, lack of insight, psychological immaturity, impulsiveness, higher incidence of certain psychiatric disorders | |
| Weiler 2013 USA | Case study | Deaf inpatient (“D.S.”) | Complex history with incomplete language records and potential brain-based issues from pre-natal rubella | Risperidone, divalproex sodium | Physical aggression, paranoia, thought disorganization, learning difficulties, minimal language skills |
Footnotes
Conflict of interest statement: On behalf of all the authors, the corresponding author states there is no conflict of interest.
References
- 1.Draine J, Salzer MS, Culhane DP, Hadley TR. Role of social disadvantage in crime, joblessness, and homelessness among persons with serious mental illness. Psychiatric Services. 2002;53(5):565–573. doi: 10.1176/appi.ps.53.5.565. [DOI] [PubMed] [Google Scholar]
- 2.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. The Medical Journal of Australia. 2007;187(7 Suppl):S26–30. doi: 10.5694/j.1326-5377.2007.tb01332.x. [DOI] [PubMed] [Google Scholar]
- 4.Mazza JR, Boivin M, Tremblay RE, Michel G, Salla J, Lambert J, Zunzunegui MV, Cote SM. Poverty and behavior problems trajectories from 1.5 to 8 years of age: Is the gap widening between poor and non-poor children? Soc Psychiatry Psychiatr Epidemiol. 2016 doi: 10.1007/s00127-016-1252-1. [DOI] [PubMed] [Google Scholar]
- 5.Mensah FK, Kiernan KE. Parents' mental health and children's cognitive and social development: families in England in the Millennium Cohort Study. Soc Psychiatry Psychiatr Epidemiol. 2010;45(11):1023–1035. doi: 10.1007/s00127-009-0137-y. [DOI] [PubMed] [Google Scholar]
- 6.Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National health interview survey, 2012. Vital and Health Statistics. 2012;10(260):1–163. [PubMed] [Google Scholar]
- 7.Mitchell RE, Karchmer MA. Parental hearing status and signing among deaf and hard of hearing students. Sign Language Studies. 2005;5(2):231–244. [Google Scholar]
- 8.Institute GR. Regional and national summary report of data from the 2009–10 annual survey of deaf and hard of hearing children and youth. 2011:1–12. [Google Scholar]
- 9.Mayberry RI, Lock E. Age constraints on first versus second language acquisition: Evidence for linguistic plasticity and epigenesis. Brain and Language. 2003;87(3):369–384. doi: 10.1016/s0093-934x(03)00137-8. [DOI] [PubMed] [Google Scholar]
- 10.Newport EL. Maturational constraints on language learning. Cognitive Science. 1990;(14):11–28. [Google Scholar]
- 11.Leybaert J, D'Hondt M. Neurolinguistic development in deaf children: The effect of early language experience. International Journal of Audiology. 2003;42(Suppl 1):S34–40. doi: 10.3109/14992020309074622. [DOI] [PubMed] [Google Scholar]
- 12.Lederberg AR, Schick B, Spencer PE. Language and literacy development of deaf and hard-of-hearing children: Successes and challenges. Developmental Psychology. 2013;49(1):15–30. doi: 10.1037/a0029558. [DOI] [PubMed] [Google Scholar]
- 13.Mayberry RI, Chen JK, Witcher P, Klein D. Age of acquisition effects on the functional organization of language in the adult brain. Brain and Language. 2011;119(1):16–29. doi: 10.1016/j.bandl.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 14.Penicaud S, Klein D, Zatorre RJ, Chen JK, Witcher P, Hyde K, Mayberry RI. Structural brain changes linked to delayed first language acquisition in congenitally deaf individuals. Neuroimage. 2013;66:42–49. doi: 10.1016/j.neuroimage.2012.09.076. [DOI] [PubMed] [Google Scholar]
- 15.Skotara N, Salden U, Kugow M, Hanel-Faulhaber B, Roder B. The influence of language deprivation in early childhood on L2 processing: An ERP comparison of deaf native signers and deaf signers with a delayed language acquisition. BMC Neuroscience. 2012;13:44. doi: 10.1186/1471-2202-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hyde M, Punch R, Komesaroff L. Coming to a decision about cochlear implantation: Parents making choices for their deaf children. Journal of Deaf Studies and Deaf Education. 2010;15(2):162–178. doi: 10.1093/deafed/enq004. [DOI] [PubMed] [Google Scholar]
- 17.Kral A, Kronenberger WG, Pisoni DB, O'Donoghue GM. Neurocognitive factors in sensory restoration of early deafness: a connectome model. Lancet Neurology. 2016 doi: 10.1016/S1474-4422(16)00034-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duchesne L, Sutton A, Bergeron F. Language achievement in children who received cochlear implants between 1 and 2 years of age: Group trends and individual patterns. Journal of Deaf Studies and Deaf Education. 2009;14(4):465–485. doi: 10.1093/deafed/enp010. [DOI] [PubMed] [Google Scholar]
- 19.Niparko JK, Tobey EA, Thal DJ, Eisenberg LS, Wang NY, Quittner AL, Fink NE, Team CDI. Spoken language development in children following cochlear implantation. JAMA. 2010;303(15):1498–1506. doi: 10.1001/jama.2010.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davidson LS, Geers AE, Blamey PJ, Tobey EA, Brenner CA. Factors contributing to speech perception scores in long-term pediatric cochlear implant users. Ear Hear. 2011;32(1 Suppl):19S–26S. doi: 10.1097/AUD.0b013e3181ffdb8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tobey EA, Geers AE, Sundarrajan M, Shin S. Factors influencing speech production in elementary and high school-aged cochlear implant users. Ear Hear. 2011;32(1 Suppl):27S–38S. doi: 10.1097/AUD.0b013e3181fa41bb. [DOI] [PubMed] [Google Scholar]
- 22.Lund E. Vocabulary Knowledge of Children With Cochlear Implants: A Meta-Analysis. Journal of Deaf Studies and Deaf Education. 2015 doi: 10.1093/deafed/env060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liddell SK. Grammar, gesture, and meaning in American Sign Language. Cambridge University Press; New York, NY: 2003. [Google Scholar]
- 24.Humphries T, Kushalnagar P, Mathur G, Napoli DJ, Padden C, Rathmann C, Smith SR. Language acquisition for deaf children: Reducing the harms of zero tolerance to the use of alternative approaches. Harm Reduction Journal. 2012b;9:16. doi: 10.1186/1477-7517-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lyness C, Woll B, Campbell R, Cardin V. How does visual language affect crossmodal plasticity and cochlear implant success? Neuroscience and Biobehavioral Reviews. 2013;37:2621–2630. doi: 10.1016/j.neubiorev.2013.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sugar M. Dispelling myths about deafness. 2016 http://www.agbell.org/in-the-news/response-nyle-dimarco/
- 27.Hassanzadeh S. Outcomes of cochlear implantation in deaf children of deaf parents: comparative study. The Journal of Laryngology & Otology. 2012;126(10):989–994. doi: 10.1017/S0022215112001909. [DOI] [PubMed] [Google Scholar]
- 28.Ajallouiyan M, Amirsalari S, Amraei K. Comparison of intelligence quotients of first- and second-generation deaf children with cochlear implants. International Journal of Pediatric Otorhinolaryngology. 2016 doi: 10.1016/j.ijporl.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Humphries T, Kushalnagar P, Mathur G, Napoli DJ, Padden C, Rathmann C, Smith SR. Discourses of prejudice in the professions: The case of sign languages. 2016 doi: 10.1136/medethics-2015-103242. Unpublished manuscript. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fellinger J, Holzinger D, Dobner U, Gerich J, Lehner R, Lenz G, Goldberg D. Mental distress and quality of life in a deaf population. Social Psychiatry and Psychiatric Epidemiology. 2005;40(9):737–742. doi: 10.1007/s00127-005-0936-8. [DOI] [PubMed] [Google Scholar]
- 31.Anderson ML, Leigh IW. Intimate partner violence against deaf female college students. Violence Against Women. 2011;17(7):822–834. doi: 10.1177/1077801211412544. [DOI] [PubMed] [Google Scholar]
- 32.Pollard RQ, Jr, Sutter E, Cerulli C. Intimate partner violence reported by two samples of deaf adults via a computerized American Sign Language survey. Journal of Interpersonal Violence. 2014;29(5):948–965. doi: 10.1177/0886260513505703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Gent T, Goehart AW, Treffers PDA. Self-concept and psychopathology in deaf adolescents: Preliminary support for moderating effects of deafness-related characterisitics and peer problems. Journal of Child Psychology and Psychiatry. 2011;52(6):720–728. doi: 10.1111/j.1469-7610.2011.02392.x. [DOI] [PubMed] [Google Scholar]
- 34.Anderson ML, Wolf Craig KS, Hall WC, Ziedonis DM. A pilot study of deaf trauma survivors' experiences: Early traumas unique to being deaf in a hearing world. Journal of Child & Adolescent Trauma. 2016 doi: 10.1007/s40653-016-0111-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fellinger J, Holzinger D, Pollard R. Mental health of deaf people. The Lancet. 2012;379(9820):1037–1044. doi: 10.1016/S0140-6736(11)61143-4. [DOI] [PubMed] [Google Scholar]
- 36.Sinkkonen J. Hearing impairment, communication and personality development. University of Helsinki; Helsinki, Finland: 1994. [Google Scholar]
- 37.Kitson N, Fry R. Prelingual deafness and psychiatry. British Journal of Hospital Medicine. 1990;44(5):353–356. [PubMed] [Google Scholar]
- 38.Glickman NS. Do you hear voices? Problems in assessment of mental status in deaf persons with severe language deprivation. Journal of Deaf Studies and Deaf Education. 2007;12(2):127–147. doi: 10.1093/deafed/enm001. [DOI] [PubMed] [Google Scholar]
- 39.Humphries T, Kushalnagar P, Mathur G, Napoli DJ, Padden C, Pollard R, Smith SR. What medical education can do to ensure robust language development in deaf children. Medical Science Educator. 2014a;24(4):409–419. [Google Scholar]
- 40.Gulati S. Psychiatric care of culturally deaf people. In: Glickman NS, Gulati S, editors. Mental Health Care of Deaf People: A Culturally Affirmative Approach. Lawrence Erlbaum Associates; Mahwah, NJ: 2003. pp. 33–107. [Google Scholar]
- 41.Glickman NS. Summary and conclusions. In: Glickman NS, editor. Cognitive-behavioral therapy for deaf and hearing persons with language and learning challenges. Routledge; New York, NY: 2009a. [Google Scholar]
- 42.Gulati S. ASL Lecture Series. Brown University; 2014. Language deprivation syndrome. https://www.youtube.com/watch?v=8yy_K6VtHJw. [Google Scholar]
- 43.Humphries T, Kushalnagar P, Mathur G, Napoli DJ, Padden C, Rathmann C, Smith SR. Avoiding linguistic neglect of deaf children. Social Service Review. 2016;90(4):589–619. doi: 10.1086/689543. [DOI] [Google Scholar]
- 44.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rainer JD, Altshuler KZ. Comprehensive mental health services for the deaf. Columbia University; New York, NY: 1966. [Google Scholar]
- 46.Basilier T. Surdophrenia. The Psychic Consequences of Congenital or Early Acquired Deafness. Some Theoretical and Clinical Considerations. Acta Psychiatrica Scandinavica. 1964;40(SUPPL 180):363. doi: 10.1111/j.1600-0447.1964.tb04948.x. [DOI] [PubMed] [Google Scholar]
- 47.Vernon M. Sociological and psychological factors associated with hearing loss. Journal of Speech and Hearing Research. 1969;12(3):541–563. doi: 10.1044/jshr.1203.541. [DOI] [PubMed] [Google Scholar]
- 48.Vernon M, Rothstein DA. Prelingual deafness: An experiment of nature. Archives of General Psychiatry. 1968;19(3):361–369. doi: 10.1001/archpsyc.1968.01740090105011. [DOI] [PubMed] [Google Scholar]
- 49.Denmark JC, Warren F. A psychiatric unit for the deaf. British Journal of Psychiatry. 1972;120(557):423–428. doi: 10.1192/bjp.120.557.423. [DOI] [PubMed] [Google Scholar]
- 50.Lane H. The wild boy of Aveyron. Harvard University Press; Cambridge, MA: 1976. [Google Scholar]
- 51.Vernon M, Raifman LJ. Recognizing and handling problems of incompetent deaf defendants charged with serious offenses. International Journal of Law and Psychiatry. 1997;20(3):373–387. doi: 10.1016/s0160-2527(97)00010-1. [DOI] [PubMed] [Google Scholar]
- 52.Altshuler KZ. Perceptual handicap and mental illness, with special reference to early profound deafness. The American Journal of Social Psychiatry. 1986;6(2):125–128. [Google Scholar]
- 53.Weiler C, Landsberger SA, Diaz DR. Differential diagnosis of psychosis in a deaf inpatient with language dysfluency: A case study. Clinical Schizophrenia and Related Psychoses. 2013;7(1):42–45. doi: 10.3371/CSRP.WELA.032513. [DOI] [PubMed] [Google Scholar]
- 54.Pollard RQ. Psychopathology. In: Marschark M, Clark MD, editors. Psychological perspectives on deafness. Vol. 2. Lawrence Erlbaum, Inc; Mahwah, NJ: 1998. pp. 171–197. [Google Scholar]
- 55.Black PA, Glickman NS. Demographics, psychiatric diagnoses, and other characteristics of North American Deaf and hard-of-hearing inpatients. Journal of Deaf Studies and Deaf Education. 2006;11(3):303–321. doi: 10.1093/deafed/enj042. [DOI] [PubMed] [Google Scholar]
- 56.Thacker AJ. Formal communication disorder. Sign language in deaf people with schizophrenia. British Journal of Psychiatry. 1994;165(6):818–823. doi: 10.1192/bjp.165.6.818. [DOI] [PubMed] [Google Scholar]
- 57.Schenkel LS, Rothman-Marshall G, Schlehofer DA, Towne TL, Burnash DL, Priddy BM. Child maltreatment and trauma exposure among deaf and hard of hearing young adults. Child Abuse Neglect. 2014;38(10):1581–1589. doi: 10.1016/j.chiabu.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 58.Denmark JC. Psychiatry and the deaf. Current Psychiatric Therapies. 1971;11:68–72. [PubMed] [Google Scholar]
- 59.Cooper AF. Deafness and psychiatric illness. British Journal of Psychiatry. 1976;129:216–226. doi: 10.1192/bjp.129.3.216. [DOI] [PubMed] [Google Scholar]
- 60.Long G, Long N, Ouellette SE. Service provision issues with traditionally underserved persons who are deaf. Research and Practice in Deafness: Issues and Questions in Education, Psychology, and Vocational Service Provision. 1993:107–126. [Google Scholar]
- 61.Hauser PC, O'Hearn A, McKee M, Steider A, Thew D. Deaf epistemology: Deafhood and deafness. American Annals of the Deaf. 2010;154(5):486–492. doi: 10.1353/aad.0.0120. [DOI] [PubMed] [Google Scholar]
- 62.Barnett S, McKee M, Smith SR, Pearson TA. Deaf sign language users, health inequities, and public health: Opportunity for social justice. Preventing Chronic Disease. 2011;8(2):A45. [PMC free article] [PubMed] [Google Scholar]
- 63.McKee MM, Paasche-Orlow MK, Winters PC, Fiscella K, Zazove P, Sen A, Pearson T. Assessing Health Literacy in Deaf American Sign Language Users. Journal of Health Communication. 2015;20(Suppl 2):92–100. doi: 10.1080/10810730.2015.1066468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Altshuler KZ. Studies of the deaf: Relevance to psychiatric theory. American Journal of Psychiatry. 1971;127(11):1521–1526. doi: 10.1176/ajp.127.11.1521. [DOI] [PubMed] [Google Scholar]
- 65.Giddan JJ, Milling L, Campbell NB. Unrecognized language and speech deficits in preadolescent psychiatric inpatients. American Journal of Orthopsychiatry. 1996;66(1):85–92. doi: 10.1037/h0080158. [DOI] [PubMed] [Google Scholar]
- 66.Gaines J, Meltzer B, Glickman NS. Language and learning challenges in adolescent hearing psychiatric inpatients. In: Glickman NS, editor. Cognitive-Behavioral Therapy for Deaf and Hearing Persons with Language and Learning Challenges. Routledge; New York, NY: 2009. pp. 79–102. [Google Scholar]
- 67.Horton HK. Linguistic ability and mental health outcomes among deaf people with schizophrenia. The Journal of Nervous and Mental Disease. 2010;198(9):634–642. doi: 10.1097/NMD.0b013e3181e9dd23. [DOI] [PubMed] [Google Scholar]
- 68.Stevenson J, McCann D, Watkin P, Worsfold S, Kennedy C Hearing Outcomes Study T. The relationship between language development and behaviour problems in children with hearing loss. Journal of Child Psychology and Psychiatry. 2010;51(1):77–83. doi: 10.1111/j.1469-7610.2009.02124.x. [DOI] [PubMed] [Google Scholar]
- 69.Barker DH, Quittner AL, Fink NE, Eisenberg LS, Tobey EA, Niparko JK, Team CDI. Predicting behavior problems in deaf and hearing children: the influences of language, attention, and parent-child communication. Development and Psychopathology. 2009;21(2):373–392. doi: 10.1017/S0954579409000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Huber M, Kipman U. The mental health of deaf adolescents with cochlear implants compared to their hearing peers. International Journal of Audiology. 2011;50(3):146–154. doi: 10.3109/14992027.2010.533704. [DOI] [PubMed] [Google Scholar]
- 71.Williams CE. Some psychiatric observations on a group of maladjusted deaf children. Journal of Child Psychology and Psychiatry. 1970;11(1):1–18. doi: 10.1111/j.1469-7610.1970.tb01008.x. [DOI] [PubMed] [Google Scholar]
- 72.Mayberry RI. Cognitive development in deaf children. In: Segalowitz SJ, Rapin I, editors. Handbook of Neuropsychology. Vol. 8. Elsevier Health Sciences; New York, NY: 2002. pp. 71–107. [Google Scholar]
- 73.Bonvillian JD, Charrow VR, Nelson KE. Psycholinguistic and educational implications of deafness. Human Development. 1973;16(5):321–345. doi: 10.1159/000271286. [DOI] [PubMed] [Google Scholar]
- 74.Bailes C, Erting C, Erting L, Thumann-Prezioso C. Language and literacy acquisition through parental mediation in American Sign Language. Sign Language Studies. 2009;9(4):417–456. [Google Scholar]
- 75.Stewart DA. The use of sign by deaf children: The opinions of a deaf community. The American Annals of the Deaf. 1983;128(7):878–883. doi: 10.1353/aad.2012.0868. [DOI] [PubMed] [Google Scholar]
- 76.Goldberg B, Lobb H, Kroll H. Psychiatric problems of the deaf child. Canadian Psychiatric Association Journal. 1975;20(1):75–83. doi: 10.1177/070674377502000113. [DOI] [PubMed] [Google Scholar]
- 77.Fromkin V, Krashen S, Curtiss S, Rigler D, Rigler M. The development of language in Genie: A case of language acquisition beyond the “Critical Period”. Brain and Language. 1974;1:81–107. [Google Scholar]
- 78.Association AP. Diagnostic and statistical manual of mental disorders. 5. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- 79.Glickman NS. Adapting best practices in CBT for deaf and hearing persons with language and learning challenges. Journal of Psychotherapy Integration. 2009b;19(4):354–384. [Google Scholar]
- 80.Cantwell DP, Baker L. Psychiatric disorder in children with speech and language retardation. A critical review. Archives of General Psychiatry. 1977;34(5):583–591. doi: 10.1001/archpsyc.1977.01770170093009. [DOI] [PubMed] [Google Scholar]