Abstract
This study aimed to investigate whether atrial fibrillation (AF) predicts myocardial infarction (MI) or cardiovascular (CV) death. AF is a well-established risk factor for thrombotic stroke and all-cause mortality. PubMed, EmBase, and Cochrane Central were searched for articles comparing the incidence rates of MI, CV death, or CV events between AF and non-AF patients. Relative risk ratio (RR) was used as effect estimate. Crude and adjusted RRs were calculated. Data were pooled using a random-effects model. The meta-analysis included 27 studies. In the unadjusted analysis, AF patients had a nonsignificant trend toward a higher risk of MI compared with non-AF patients; however, a significant association was found. The crude data analysis showed that AF was associated with increased risk of CV death (P < 0.05) and CV events (P < 0.05). These associations remained significant after pooling data from adjusted models (CV death: RR = 1.95, 95% CI 1.51–2.51, P < 0.05; CV events: RR = 2.10, 95% CI 1.50–2.95, P < 0.05). These results showed that AF is an independent risk factor for MI, CV death, and CV events.
Introduction
Atrial fibrillation (AF) is the most commonly encountered clinically significant cardiac arrhythmia. It represents a major public health problem with increasing prevalence in elderly people and significant association with poor outcomes1, 2. Approximately 2.7–6.1 million patients suffer from AF in the United States, a number expected to double by 20503. AF is a well-established independent risk factor for stroke, and non-valvular AF increases the risk of stroke by fivefold1, 4. Antithrombotic medications, such as vitamin K antagonists (VKAs) and non-VKAs, are routinely recommended for AF patients to prevent stroke and systemic embolic events, while decreasing mortality5, 6.
Myocardial infarction (MI) has been recognized as a risk factor for new-onset AF since the Framingham Heart Study7, 8. Multiple studies demonstrated the unfavorable prognostic impact of AF in patients sustaining MI9, 10. The incidence of AF complicating acute MI is between 6% and 21%9. New-onset AF is associated with an increased risk of mortality even after adjusting for pivotal risk factors for AF11, 12. AF may lead to dismal prognosis in patients with MI through adverse hemodynamic effects, including loss of atrial contraction, high ventricular rates, loss of atrioventricular synchrony, and an irregular RR interval, leading to decreased cardiac output13.
Previous extensive studies have emphasized more on ischemic cerebrovascular rather than cardiovascular (CV) events, as the principal outcome in AF patients. A previous large cohort study suggested that AF is not strongly associated with ischemic heart disease14. Indeed, AF is associated with impaired coronary flow and diminished myocardial perfusion15. Numerous studies have illustrated the associations of AF with CV outcomes3, 16, 17. However, controversies exist because the annual rate of MI in AF patients is low, with drug intervention in biasing the size of effect estimate18, 19. For example,, warfarin, as a commonly prescribed drug for AF patients, may exert protective effects against MI20. Further, several studies suggested that the coexistence of atherosclerotic risk factors may contribute to increased risk of MI in AF21, 22. Also, concerns were raised regarding the increased risk of MI after use of non-VKAs, such as dabigatran23–25. Thus, a systematic review and meta-analysis was conducted to compare cardiovascular outcomes between AF and non-AF patients.
Methods
Data Sources, Search Strategy, and Selection Criteria
The present systematic review and meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines26. PubMed, EmBase, and Cochrane Central were searched from inception to June 2016. The following key words and medical terms were used in the literature search: “atrial fibrillation” AND (“acute coronary syndrome” OR “myocardial infarction” OR “coronary heart disease” OR “myocardial ischemia” OR “angina” OR “cardiac death” OR “cardiac event” OR “cardiac mortality” OR “cardiac events” OR cardiovascular) AND (random* OR trial OR cohort OR retrospective* OR database OR population-based OR “population based” OR prospective* OR follow-up OR follow up OR registry OR community-based). The search was limited to the English language. The references of included studies were manually screened for potentially eligible studies.
For inclusion in the meta-analysis, studies had to meet the following criteria: adult patient evaluation; availability of extractable data for MI, CV death, or CV events in individuals with AF. Both retrospective and prospective studies were selected. Studies that enrolled AF patients during the postoperative phase were excluded. The primary outcome of interest was MI, and secondary outcomes included CV death and CV events. The latest American College of Cardiology/American Heart Association guidelines suggested that CV death might be attributed to MI, sudden cardiac death (SCD), heart failure (HF), stroke, cardiovascular procedure, or vascular hemorrhage27. Among the included studies, the “cardiovascular” categories might vary widely. However, studies focusing only on the outcome of SCD, for which ventricular fibrillation was the predominant cause, were not considered. Studies including only AF patients after MI were excluded as well, considering that AF might be complicated by MI, leading to a bias in exploring their association.
Data extraction
Two researchers respectively screened the titles and abstracts, and excluded studies not meeting the inclusion criteria. Potentially eligible full-text articles were subsequently reviewed. In case of disagreement, consensus was achieved through consultation with the corresponding author. The following information was extracted: author, year, study design, region, number of patients, gender, population, AF diagnosis method, proportion of patients with prior MI, CHADS2 score, antithrombotic medications, cardiovascular outcomes, degree of adjustment, and follow-up. Crude and adjusted RRs were both directly extracted or indirectly calculated. The adjustment degree was categorized as “+” for age and/or sex only; “++” for those further adjusting for less than five standard vascular risk factors (i.e., blood pressure/hypertension, smoking, drinking, and body mass index); and “+++” for those further adjusting five or more risk factors, including unconventional or socioeconomic factors. The quality of the included studies was appraised by the Newcastle–Ottawa Scale (NOS)28. This scoring system mainly incorporated four aspects, including selection, comparability, exposure, and outcomes, with a total score ranging from 0 to 7 points: 0–2 points, low quality; 3–5 points, medium quality; more than 6 points, high quality.
Statistical analysis
Relative risk RATIO (RR) with associated 95% confidence interval (CI) was considered the effect estimate for binary outcomes. Hazard ratio was considered to be equivalent to RR in cohort studies. Given the low incidence of MI in AF patients, odds ratios (ORs) could be assumed to be accurate estimates of RRs. Crude and adjusted RRs were pooled separately. When adjusted RRs were presented by multiple multivariate models, the most adjusted one was selected. The meta-analysis was performed using a random-effects model29. Heterogeneity was assessed by the I 2 statistics30. Publication bias was assessed visually using funnel plots, and statistically by Begg’s and Egger’s tests31, 32. Also, sensitivity analysis was performed by excluding the included studies one by one. A stratified analysis was performed to assess the effects of publication year (2010 or after vs before 2010), study design (prospective cohort vs retrospective cohort), region (North America, Europe, or Asia), sample size (≥10000 vs <10000), mean age (60 years or older vs <60 years), female proportion (≥50% vs <50%), previous MI (≥20% vs <20%), adjustment degree (+,++, or+++), and follow-up duration (≥5 years vs <5 years). A meta-regression was conducted to investigate the impact of publication year, sample size, mean age, women proportion (%), previous MI (%) and follow-up duration on data heterogeneity. All analyses were conducted using the Stata software (version 12.0, Stata Corporation, TX, USA). All P values were two sided, with a significance level of 0.05.
Results
A total of 733 records from the initial search were identified, including 162 from PubMed, 392 from EmBase, and 179 from Cochrane Central. After discarding 122 duplicates and 505 irrelevant studies, 106 full-text articles were assessed. Further, studies that enrolled single-arm AF patients, included AF patients after ischemic coronary disease, explored the impact of risk factors, or focused on medications/surgeries were excluded. Thirty-two studies were included in a qualitative analysis. Then, two studies of duplicate cohorts and three articles assessing SCD were excluded. The study selection process is displayed in Fig. 1.
Figure 1.
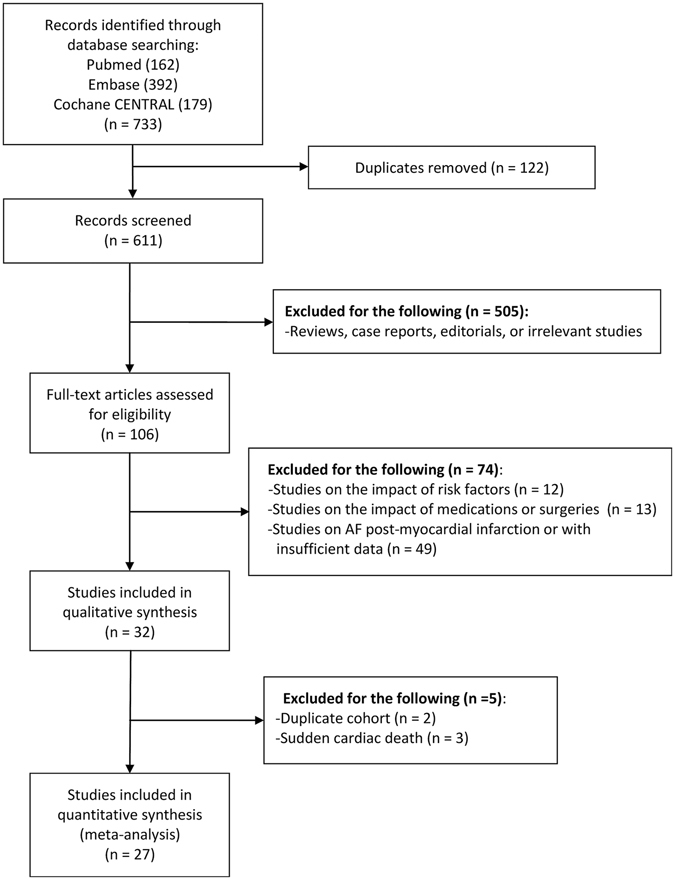
Flow diagram showing the study selection process.
Characteristics of the included studies
Overall, 27 studies fulfilled the inclusion criteria and were included in the final meta-analysis3, 8, 16, 33–56. Table 1 summarizes the baseline characteristics of these studies. They included 20 and 7 prospective and retrospective studies, respectively. The number of enrolled patients ranged from 590 to 704,225, with a total of 1,324,037 patients. Eleven studies were performed in North America, 5 in Asia, and 9 in Europe. Two were international multicenter studies. The median or mean follow-up duration ranged from 14 days to 44 years. In quality assessment using the NOS scale (Supplementary Table S1), 16 (59.3%) studies achieved high-quality scores of 6–7. The least satisfying items included the representativeness of patients (14/27), adequacy of follow-up (13/27), and control of confounding factors (18/27).
Table 1.
Characteristics of included studies.
| Author (year) | Study design | Region | Patients (n) | Population | AF diagnosis | Age (year) | Female (%) | Previous MI (%) | CHADS 2 scores | AT | Degree of adjustment | CV outcomes | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kannel (1982) | Prospective | USA | 590 | Framingham cohort | ECG | 48 | 55.2 | 6.9 | NA | NA | None | CV death | 22 years |
| Lake (1989) | Prospective | Australia | 1,770 | Community-based | Record | >60 | 48 | 11 | NA | NA | +++ | CV death | 17 years |
| Krahn (1995) | Prospective | Canada | 3,983 | Healthy pilots | ECG (85%) | 31 | 0 | 22.3 | NA | NA | +++ | CV death, MI | 44 years |
| Aronow (1995) | Prospective | USA | 1,359 | Heart disease | ECG | 81 | 70.2 | 47.1 | NA | NA | ++ | Coronary events | 42 months |
| Kaarisalo (1997) | Prospective | Finland | 6,912 | First ischemic stroke | ECG (>80%) | 64 | 44 | NA | NA | NA | None | CV death | 1 year |
| Benjamin (1998) | Prospective | USA | 1,863 | Framingham cohort | ECG | 75 | 52.3 | 13.6 | NA | NA | None | CV death | 40 years |
| Dries (1998) | Retrospective | USA | 6,517 | Heart failure | ECG | 60 | 14 | 74.5 | NA | 10.7 | None | MI | 33.4 months |
| Saxena (2001) | Prospective | International | 18,451 | Acute stroke | Record | 72 | 46.6 | NA | NA | NA | None | Coronary death | 14 days |
| Friberg (2004) | Prospective | Denmark | 29,310 | Community-based | ECG | 58 | 55.8 | 2.6 | NA | 4.4 | +++ | CV death | 4.7 years |
| Dhamoon (2007) | Prospective | USA | 655 | First ischemic stroke | Record | 70 | 55.4 | 16.2 | NA | NA | +++ | CV events | 4 years |
| Goto (2008) | Prospective | International | 63,589 | Atherothrombotic disease | Record | 68 | 36 | 31 | 0–6 | 86.3 | None | CV death, nonfatal MI | 1 year |
| Ruigómez (2009) | Retrospective | UK | 9,057 | Community-based | Record | 40–89 | 53.4 | NA | NA | NA | +++ | Coronary events | 6 years |
| Haywood (2009) | Prospective | USA | 39,056 | Hypertension | ECG (92.1%) | ≥55 | 45.9 | 25.7 | NA | 36.6 | None | Cardiac events | 4.9 years |
| Bouzas-Mosquera (2010) | Retrospective | Spain | 17,100 | Patients with known or suspected CAD | ECG | 64 | 41 | 17.3 | NA | NA | +++ | MI | 6.5 years |
| Winkel (2010) | Prospective | Europe | 3,655 | PAD | Record | 68 | 24.8 | 25.8 | NA | NA | +++ | CV events, CV death | 2 years |
| Conen (2011) | Prospective | USA | 34,722 | Community-based | Record | 53 | 100 | NA | 0–5 | NA | +++ | CV death | 15.4 years |
| Aguilar (2012) | Prospective | Spain | 3,848 | PAD, CAD, or CVD | Record | 58 | 25.8 | 37.3 | 0–6 | 7.6 | None | MI | 16 months |
| Chao (2014) | Retrospective | Taiwan | 24,228 | Healthy community-based | Record | 47 | 40.1 | NA | 0–1 | NA | +++ | AMI | 5.7 years |
| Martinez (2014) | Retrospective | Austrilia | 30,260 | Asymptomatic AF | Record | 71 | 38.4 | 4.7 | 1.1 | NA | None | MI | 3 years |
| Soliman (2014) | Prospective | USA | 23,928 | Community-based | ECG or record | 64 | 58.2 | 0 | 40.4 | NA | +++ | MI | 6.9 years |
| Albayrak (2015) | Prospective | Turkey | 2,230 | Community-based | ECG | 50 | 63.9 | NA | NA | NA | +++ | CV events | 3 years |
| Vermond (2015) | Prospective | Netherlands | 8,265 | Community-based | ECG | 49 | 50.2 | 3 | NA | NA | Adjusted | CV events, cardiac events | 9.7 years |
| Soliman (2015) | Prospective | USA | 14,462 | Community-based | ECG or record | 54 | 56 | 0 | 45.7 | NA | +++ | MI | 21.6 years |
| Li (2015) | Retrospective | Taiwan | 704,225 | Community-based | Record | >18 | 44.4 | NA | NA | NA | +++ | CV events | 4 years |
| Parisi (2015) | Prospective | UK | 256,710 | Psoriasis | Record | 48 | 56.3 | NA | NA | NA | +++ | CV events | 5.2 years |
| Shih (2016) | Retrospective | Taiwan | 12,988 | Hemodialysis | Record | 69 | 53.3 | 14 | 0–9 | 8.4% | +++ | CV death, MI | 3.2 years |
| O’Neal (2016) | Prospective | USA | 4304 | No CV disease | ECG or record | >65 | 61 | NA | NA | 1.4 | +++ | CHD, MI | 11 years |
AT, antithrombotic; ACM, all-cause mortality; CHD, coronary heart disease; CV, cardiovascular; CVD, cardiovascular disease; HF, heart failure; MI, myocardial infarction; NFMI, nonfatal MI; PAD, peripheral arterial disease.
Myocardial infarction
Crude unadjusted data relating to MI were presented in 11 studies3, 16, 35, 38, 42, 46, 48–51, 56. Two studies investigated the same cohort (REACH registry)42, 46, and the one with the largest sample size was selected42. Thus, 10 studies were included in the current meta-analysis. Dries et al. showed two sub-cohorts that were aggregated using fixed- and random-effects models38. Compared with non-AF patients, AF patients had an insignificant trend toward a higher risk of MI (RR = 1.22, 95% CI 0.96–1.55, P = 0.11), with high heterogeneity (I 2 = 92.2%, P < 0.05) (Fig. 2). Sensitivity analysis by excluding the included studies one by one showed no substantial alteration.
Figure 2.
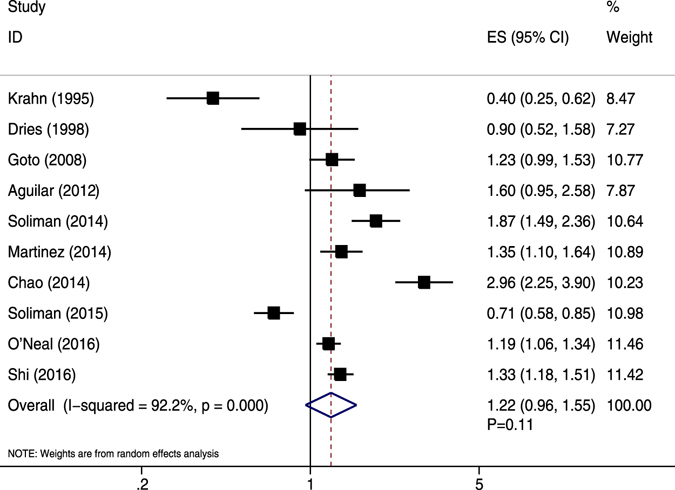
Forest plot showing the comparison between AF and non-AF patients in the pooled analysis of crude relative risk for myocardial infarction.
The meta-regression showed a significant impact of follow-up duration on the overall effect for unadjusted MI (P = 0.010). However, publication year, sample size, mean age, female proportion, and previous MI were not significant contributors of the association between AF and unadjusted MI (Table 2). The findings of subgroup analyses are presented in Table 3. Interestingly, AF was significantly correlated with increased risk of unadjusted MI in studies published after 2010; conducted in Asia; with retrospective design, sample size ≥ 10000, mean age ≥60.0 years, and follow-up duration <5.0 years. No other significant associations of AF with unadjusted MI were detected (Table 3).
Table 2.
Meta-regression findings.
| Outcomes | Publication year | Sample size | Age | Female (%) | Previous MI (%) | Follow-up duration |
|---|---|---|---|---|---|---|
| Unadjusted MI | 0.058 | 0.419 | 0.243 | 0.188 | 0.774 | 0.010 |
| Adjusted MI | 0.910 | 0.378 | 0.693 | 0.595 | 0.020 | 0.667 |
| Unadjusted CV death | 0.473 | 0.507 | 0.561 | 0.418 | 0.535 | 0.655 |
| Adjusted CV death | 0.719 | 0.040 | 0.640 | 0.206 | 0.067 | 0.350 |
| Unadjusted CV events | 0.546 | 0.009 | 0.233 | 0.326 | 0.243 | 0.299 |
| Adjusted CV events | 0.913 | 0.082 | 0.390 | 0.748 | 0.581 | 0.728 |
Table 3.
Subgroup analyses of crude relative risk for myocardial infarction and adjusted relative risk for myocardial infarction.
| Outcomes | Group | RR and 95%CI | P value | Heterogeneity (%) | P value for heterogeneity | P value between subgroups |
|---|---|---|---|---|---|---|
| Crude relative risk for myocardial infarction | Publication year | |||||
| 2010 or after | 1.43 (1.09–1.87) | 0.011 | 93.1 | <0.001 | 0.006 | |
| Before 2010 | 0.77 (0.37–1.60) | 0.482 | 90.3 | <0.001 | ||
| Study design | ||||||
| Prospective | 1.05 (0.75–1.47) | 0.789 | 92.5 | <0.001 | <0.001 | |
| Retrospective | 1.53 (1.05–2.23) | 0.027 | 90.3 | <0.001 | ||
| Region | ||||||
| North America | 0.92 (0.60–1.39) | 0.68 | 93.7 | <0.001 | <0.001 | |
| Europe | 1.60 (0.97–2.64) | 0.065 | — | — | ||
| Asia | 1.72 (1.13–2.61) | 0.011 | 92.9 | <0.001 | ||
| International | 1.23 (0.99–1.53) | 0.061 | — | — | ||
| Sample size | ||||||
| 10000 or greater | 1.42 (1.02–1.97) | 0.036 | 94 | <0.001 | 0.016 | |
| <10000 | 0.91 (0.53–1.57) | 0.743 | 87.9 | <0.001 | ||
| Mean age | ||||||
| 60 or older | 1.33 (1.16–1.51) | <0.001 | 63.9 | 0.017 | 0.005 | |
| <60 | 1.07 (0.45–2.59) | 0.872 | 96.8 | <0.001 | ||
| Women proportion | ||||||
| ≥50% | 1.20 (0.88–1.63) | 0.246 | 93.6 | <0.001 | 0.051 | |
| <50% | 1.21 (0.77–1.91) | 0.41 | 92.2 | <0.001 | ||
| Previous myocardial infarction | ||||||
| ≥20% | 0.92 (0.52–1.63) | 0.774 | 87.4 | <0.001 | 0.025 | |
| <20% | 1.24 (0.86–1.77) | 0.248 | 93.7 | <0.001 | ||
| Adjustment degree | ||||||
| +++ | 1.19 (0.83–1.70) | 0.347 | 95.5 | <0.001 | 0.631 | |
| None | 1.28 (1.12–1.47) | <0.001 | 0 | 0.455 | ||
| Follow-up duration | ||||||
| ≥5 years | 1.15 (0.70–1.90) | 0.586 | 96.4 | <0.001 | 0.148 | |
| <5 years | 1.31 (1.19–1.43) | <0.001 | 0 | 0.599 | ||
| Adjusted relative risk for myocardial infarction | Publication year | |||||
| 2010 or after | 1.45 (1.07–1.99) | 0.018 | 91.3 | <0.001 | 0.241 | |
| Before 2010 | 1.02 (0.66–1.58) | 0.93 | — | — | ||
| Study design | ||||||
| Prospective | 1.48 (1.25–1.74) | <0.001 | 35.4 | 0.2 | 0.013 | |
| Retrospective | 1.34 (0.66–2.72) | 0.414 | 95.9 | <0.001 | ||
| Region | ||||||
| North America | 1.48 (1.25–1.74) | <0.001 | 35.4 | 0.2 | 0.002 | |
| Europe | 0.77 (0.53–1.11) | 0.166 | — | — | ||
| Asia | 1.75 (0.65–4.73) | 0.272 | 97.6 | <0.001 | ||
| Sample size | ||||||
| 10000 or greater | 1.42 (0.84–2.41) | 0.188 | 94.3 | <0.001 | 0.106 | |
| <10000 | 1.41 (1.15–1.73) | 0.001 | 46.6 | 0.154 | ||
| Mean age | ||||||
| 60 or older | 1.20 (0.92–1.56) | 0.187 | 81.5 | 0.001 | <0.001 | |
| <60 | 1.73 (1.02–2.93) | 0.04 | 89.3 | <0.001 | ||
| Women proportion | ||||||
| ≥50% | 1.40 (1.10–1.78) | 0.007 | 83 | 0.001 | 0.036 | |
| <50% | 1.33 (0.55–3.24) | 0.528 | 94.6 | <0.001 | ||
| Previous myocardial infarction | ||||||
| ≥20% | 1.02 (0.66–1.58) | 0.93 | — | — | <0.001 | |
| <20% | 1.24 (0.91–1.70) | 0.18 | 86.6 | <0.001 | ||
| Adjustment degree | ||||||
| +++ | 1.39 (1.05–1.85) | 0.022 | 89.8 | <0.001 | — | |
| ++ | — | — | — | — | ||
| Follow-up duration | ||||||
| ≥5 years | 1.47 (1.07–2.02) | 0.018 | 87.1 | <0.001 | <0.001 | |
| <5 years | 1.06 (0.93–1.20) | 0.366 | — | — | ||
Adjusted data regarding MI were described in seven studies3, 16, 35, 45, 49, 51, 56. All studies had a sufficient degree of adjustment (+++). AF was significantly associated with a reduction in the risk of MI (RR = 1.39, 95% CI 1.05–1.85, P < 0.05) (Fig. 3). A high level of heterogeneity was present (I 2 = 89.8%, P < 0.05). No substantial change in the overall effect was shown after exclusion of any individual study.
Figure 3.
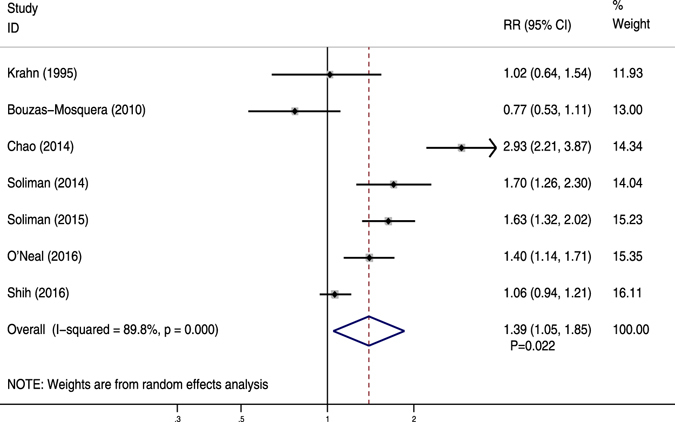
Forest plot showing the comparison between AF and non-AF patients in the pooled analysis of adjusted relative risk for myocardial infarction.
The meta-regression showed previous MI contributed to the association of AF with adjusted MI (P = 0.020). Publication year, sample size, mean age, female proportion, and follow-up duration did not appear to affect meta-regression data (Table 2). The results of stratified analyses showed that the association remained significant for studies published after 2010; conducted in North America; with prospective design, sample size <10000, mean age <60.0 years, female proportion≥50%, and follow-up duration≥5.0 years (Table 3).
CV death
Ten studies displayed crude data8, 33, 35–37, 39, 40, 42, 47, 56. Except for one retrospective study56, most studies were prospectively designed. Compared with non-AF patients, AF patients had significantly increased risk of CV death (RR = 2.25, 95% CI 1.70–3.00, P < 0.05) (Fig. 4). High heterogeneity was revealed (I 2 = 96.2%, P < 0.05). Sensitivity analysis by excluding any single study did not alter the overall effect. Meta-regression suggested that publication year, sample size, mean age, female proportion, previous MI, and follow-up duration did not account for data heterogeneity (Table 2). In subgroup analysis (Supplementary Table S2), the results turned to be insignificant for two Asian studies (P = 0.612) and two European trials (P = 0.224).
Figure 4.
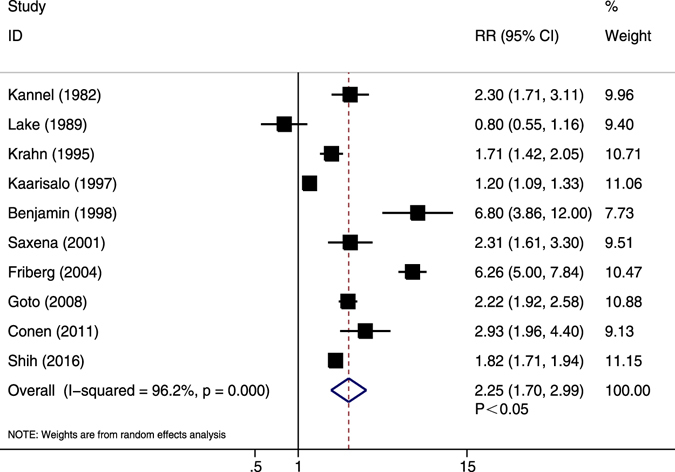
Forest plot showing the comparison between AF and non-AF patients in the pooled analysis of crude relative risk for cardiovascular mortality.
Adjusted data were available from five studies33, 35, 40, 47, 56. The pooled data revealed that AF patients were at a higher risk of CV death compared with non-AF patients (RR = 1.95, 95% CI 1.51–2.51, P < 0.05; I 2 = 82.3%, P < 0.05) (Fig. 5). After excluding the only retrospective study56, the significant trend was not markedly changed (RR = 2.08, P < 0.05). The meta-regression showed sample size contributed to the association of AF with adjusted MI (P = 0.040). Publication year, mean age, female proportion, previous MI and follow-up duration did not appear to affect meta-regression data (Table 2). These findings in stratified analyses were consistent with overall analysis for adjusted CV death (Supplementary Table S2).
Figure 5.
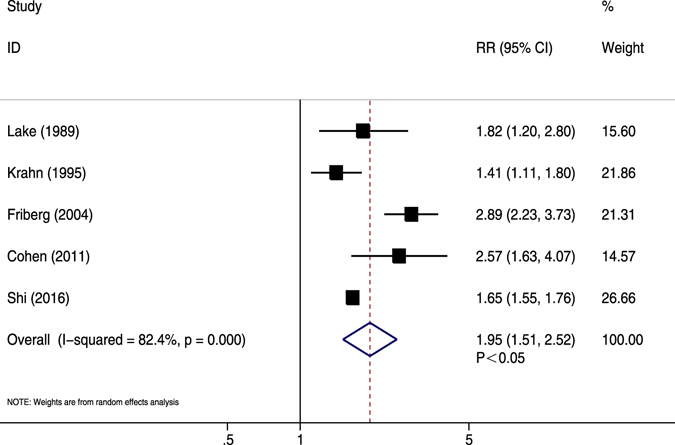
Forest plot showing the comparison between AF and non-AF patients in the pooled analysis of adjusted relative risk for cardiovascular mortality.
CV events
Crude data were shown in eight studies16, 34, 41, 43, 44, 46, 53, 55. AF patients had substantially higher risk of CV events compared with non-AF patients (RR = 2.03, 95% CI 1.40–2.93, P < 0.05). A high heterogeneity was demonstrated (I 2 = 98.3%, P < 0.05) (Fig. 6). After sequential exclusion of each study from pooled analyses, the conclusion was not affected. The finding of meta-regression showed sample size contributed to the association of AF and unadjusted CV events (P = 0.009) (Table 2). Subgroup analyses showed AF was not associated with the risk of unadjusted CV events with mean age <60 years (Supplementary Table S3).
Figure 6.
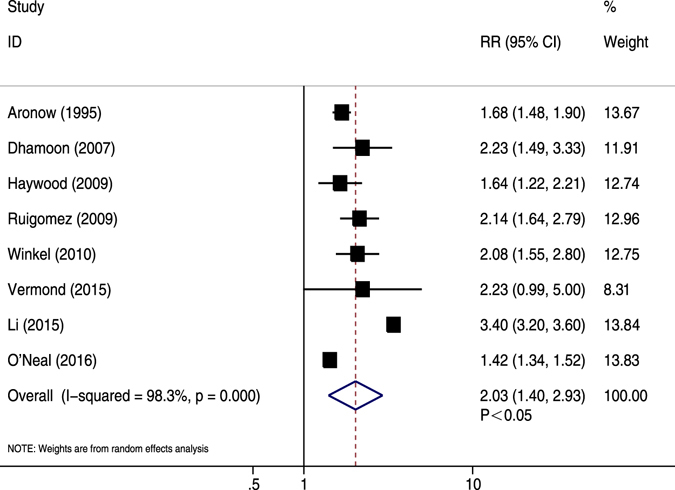
Forest plot showing the comparison between AF and non-AF patients in the pooled analysis of crude relative risk for cardiovascular events.
Nine studies showed adjusted data16, 34, 41, 44, 46, 53–55. Except for one study with an adjustment degree of “++”34, most studies showed a sufficient degree of adjustment (+++). The pooled results demonstrated that AF patients had significantly higher risk of CV events compared with those without AF (RR = 2.10, 95% CI 1.50–2.95, P < 0.05; I 2 = 96.4%, P < 0.05) (Fig. 7). Sensitivity analysis did not suggest a substantial effect for any single study. Publication year, sample size, mean age, female proportion, previous MI and follow-up duration did not appear to affect the association of AF with adjusted CV events (Table 2). The significant trend was changed with female proportion <50% (Supplementary Table S3).
Figure 7.
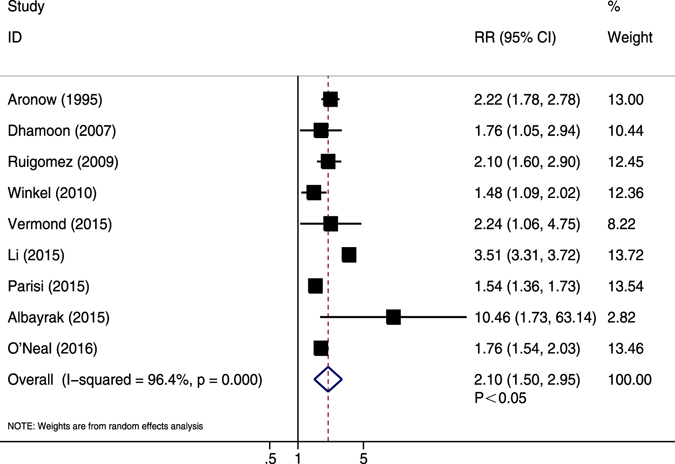
Forest plot showing the comparison between AF and non-AF patients in the pooled analysis of adjusted relative risk for cardiovascular events.
Publication bias
For studies assessing MI outcomes, no publication bias was revealed in Begg’s test (P = 0.86) or Egger’s test (P = 0.40). The funnel plot appeared to be symmetrical (Fig. 8). For studies of the CV death outcome, the P value was 0.37 in Begg’s test and 0.07 in Egger’s test. The funnel plot was also symmetrical (Fig. 9).
Figure 8.
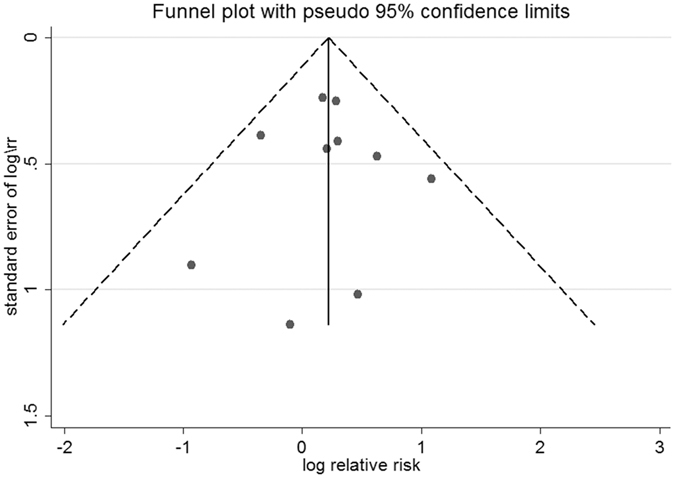
Funnel plot of studies assessing the myocardial infarction outcome.
Figure 9.
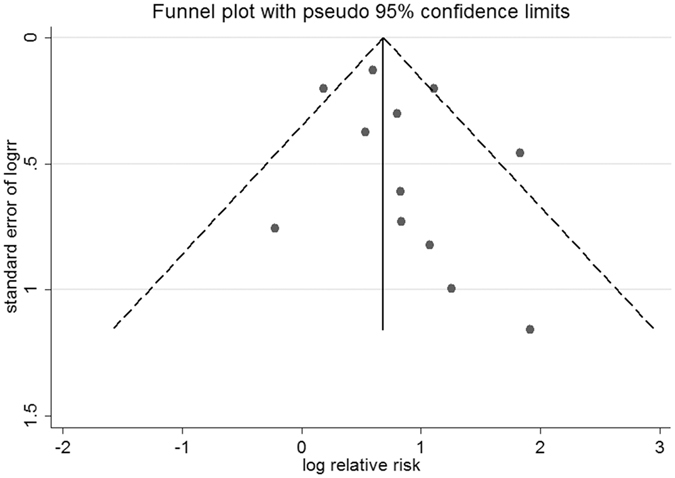
Funnel plot of studies assessing the CV death outcome.
Discussion
The association of AF with the risk of thromboembolic stroke has been confirmed in previous studies; however, evidence regarding the association of AF with cardiac outcomes is lacking. A previous study suggested that a vast majority of deaths are related to cardiac causes (37.4%) rather than stroke (9.8%) in the contemporary anticoagulated AF population57. Although studies illustrated the association of AF with increased risk of SCD58, 59, it remains unclear whether AF is a predictor for SCD caused by coronary events. Besides, the meta-analysis revealed that AF is an independent predictor of mortality for patients with MI11, 60. However, the relation between AF and the development of MI remains poorly understood. Therefore, MI outcomes were studied, and the composite outcomes of CV death or events were selected as the main elements. This study was meaningful in summarizing and evaluating the current evidence of ischemic coronary outcomes in AF patients.
Pooled data from adjusted models showed a significant increase by 39% in the risk of MI for AF patients compared with non-AF individuals. This trend was insignificant when pooling crude RRs. It was inferred that potential confounding risk factors for MI might weaken the association of AF with MI. AF patients were associated with markedly increased likelihood of CV death or CV events. The risk of CV death or CV events in patients was approximately twice that in patients without AF (adjusted RR = 2.25 and crude RR = 1.95 for CV death; adjusted RR = 2.03 and crude RR = 2010 for CV events). A large long-term cohort showed no significant change in the trend of mortality among AF patients without a preexisting CV disease61, which supported the finding that AF is an independent predictor for CV death.
A previous study suggested an association of AF with increased risk of mortality in MI patients. New AF with no history of AF before MI remained associated with increased risk of mortality even after adjustment for several important risk factors for AF62. However, participants with other characteristics were not illustrated. Further, Emidin et al. conducted a meta-analysis of cohort studies to evaluate gender-related differences in the associations of AF with CV outcomes, indicating that AF is a stronger risk factor for cardiovascular disease and death in women compared with men, but the impact of confounders was not determined63. Important strengths of this meta-analysis include a comprehensive inclusion of relevant studies with a large sample size. Most cohorts were prospectively designed and population based. Long follow-up was found in most studies with a satisfying response rate. AF occurrence rates were reliably recorded following the International Classification of Diseases code or by direct evidence from electrocardiography (ECG) reports. Further, broad baseline characteristics that ensured the applicability of summary results to worldwide populations were included, representing global data of different regions or races. Both the adjusted and crude data were analyzed, which ensured completeness of the analysis, and demonstrated the potential impact of confounding factors. Overall, adjusted data were consistent in demonstrating the significant association of AF with studied outcomes. Crude data analysis failed to show significance only for MI. Also, data heterogeneity was assessed in multiple ways. No publication bias was found in the present study.
Several lines of mechanisms may explain the increased ischemic coronary burden for AF patients. AF could facilitate the induction of ventricular tachyarrhythmia, which is the predominant cause of SCD. This risk was especially high in patients with structural heart disease64, 65. In a porcine model, a rapid atrial pacing could induce ventricular ischemia and endothelial dysfunction in the microvasculature, and increased oxidative stress despite normal coronary vessels showing no atherosclerosis66. In AF patients, myocardial perfusion is impaired, with increased coronary vascular resistance. Notably, these changes are reversible to some extent after cardioversion of sinus rhythm67.
The impact of various AF patterns on different types of MI remains uncertain. Persistent AF results in worse patient survival compared with paroxysmal AF68. However, Senoo et al. suggested that the risk of cardiovascular death is higher in anticoagulated patients with permanent AF than in those with nonpermanent AF69. A large population-based study revealed that paroxysmal AF does not differ from other types of AFs in risk of overall mortality. In the adjustment model including concurrent MI, stroke, and HF, the risk of CV death is also independent of AF patterns47. Ruigómez et al. revealed that both chronic and paroxysmal AF cases are markedly associated with increased risk of coronary events, without a significant difference between the two subtypes44. A recent large cohort study revealed that AF is significantly associated with increased risk of non–ST-segment-elevation MI (NSTEMI) but not ST-segment-elevation MI (STEMI)3. It was inferred that partial occlusion of coronary arteries or increased oxygen demand, rather than coronary thrombo-embolization, is more likely to explain the observed association of AF with MI3.
Although adjusted data analysis showed significant results, various clinical or social factors might independently contribute to the development of ischemic coronary disease in AF patients, which deserves in-depth exploration70–72. The present findings may be confounded by differences in these measured or unmeasured baseline characteristics, including age, sex, race, hypertension, HF, smoking, and education. It has been demonstrated that black female AF patients, with warfarin prescription, and high CHADS2 score, are associated with higher risk of MI compared with their counterparts51. Of note, the roles of some relevant covariates remain controversial. The risk of acute myocardial infarction was shown to be higher in men with AF than in female counterparts49. However, the meta-analysis proved that AF was a stronger risk factor for CV events and death in women than in men63. With respect to antithrombotic therapy, different anticoagulation combinations, drug types, and treatment compliance are all possible confounding variables for CV outcomes. Some authors recommended adding antiplatelet drugs to vitamin K antagonist (VKA) when AF is complicated with coronary diseases. However, a national cohort revealed that addition of antiplatelet drugs to VKA therapy is not associated with decreased risk of coronary events in AF patients with coexisting coronary heart disease, HF, or vascular disease73, 74. The percentage of patients on antithrombotic therapy was low or unknown in the included cohorts. It is possible that many patients did not undergo standard anticoagulation following the guidelines52. Good anticoagulation was shown to be associated with a significant reduction in major cardiovascular events among AF patients75. Interestingly, a national cohort study suggested that future events tend to mirror the recent disease status in AF patients. For example, patients with previous MI have a higher risk of MI76. However, comorbid conditions were often not coded uniformly or described sufficiently among most cohorts.
Several limitations of this meta-analysis should be mentioned. Some studies identified AF patients by medical records rather than via ECG, and might have underestimated the number of undetected patients with asymptomatic AF at baseline42. Indeed, as an elusive arrhythmia, AF is difficult to ascertain in population-based cohorts. Data assessing the use of antithrombotic agents, AF type (paroxysmal, persistent, or chronic), and CHADS2 score were not collected in several large population-based cohorts8, 33–36. Meanwhile, inherent recall bias and selection bias were associated with retrospective cohorts38, 45, 49. Most studies did not collect information on continuous ECG recordings49. The information on percentage or indication for antithrombotic therapy could not be obtained in most cohorts. The majority of cohorts enrolled AF patients from individuals with heart disease or stroke34, 36, 38, 39, rather than healthy community-based enrollment, which might have limited the generalization of the current association with all AF populations. For CV death or events, categories may be heterogeneous among studies. Some studies may include stroke in these compound outcomes, which may exaggerate the association of AF with ischemic cardiac outcomes. Besides, the ascertainment of the cause of death may be liable to bias and misclassification77.
Conclusions
In summary, AF was associated with MI, CV mortality, and CV events. The present study strongly supports the routine surveillance of ischemic heart disease, especially MI, among patients with AF. Future studies are warranted to clarify the interaction among confounding risk factors, and investigate effective preventive measures against adverse outcomes.
Electronic supplementary material
Acknowledgements
This work was supported by Henan Province scientific and technological projects: Feasibility and Safety Study of Prehospital Thrombolysis in Acute Myocardial Infarction (Project No. 122102310156).
Author Contributions
Wenqi He and Yingjie Chu conceived and coordinated the study, carried out data collection and analysis; and wrote the manuscript. All authors reviewed the results and approved the final version of the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-03653-5
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.January CT, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:e199–267. doi: 10.1161/CIR.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110:1042–1046. doi: 10.1161/01.CIR.0000140263.20897.42. [DOI] [PubMed] [Google Scholar]
- 3.Soliman EZ, et al. Atrial Fibrillation and Risk of ST-Segment-Elevation Versus Non-ST-Segment-Elevation Myocardial Infarction: The Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2015;131:1843–1850. doi: 10.1161/CIRCULATIONAHA.114.014145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–988. doi: 10.1161/01.STR.22.8.983. [DOI] [PubMed] [Google Scholar]
- 5.Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–867. doi: 10.7326/0003-4819-146-12-200706190-00007. [DOI] [PubMed] [Google Scholar]
- 6.You JJ, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e531S–575S. doi: 10.1378/chest.11-2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benjamin EJ, et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840–844. doi: 10.1001/jama.1994.03510350050036. [DOI] [PubMed] [Google Scholar]
- 8.Kannel WB, Abbott RD, Savage DD, McNamara PM. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N Engl J Med. 1982;306:1018–1022. doi: 10.1056/NEJM198204293061703. [DOI] [PubMed] [Google Scholar]
- 9.Schmitt J, Duray G, Gersh BJ, Hohnloser SH. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J. 2009;30:1038–1045. doi: 10.1093/eurheartj/ehn579. [DOI] [PubMed] [Google Scholar]
- 10.Batra G, et al. All types of atrial fibrillation in the setting of myocardial infarction are associated with impaired outcome. Heart. 2016;102:926–933. doi: 10.1136/heartjnl-2015-308678. [DOI] [PubMed] [Google Scholar]
- 11.Jabre P, et al. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta-analysis. Circulation. 2011;123:1587–1593. doi: 10.1161/CIRCULATIONAHA.110.986661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Behar S, Zahavi Z, Goldbourt U, Reicher-Reiss H. Long-term prognosis of patients with paroxysmal atrial fibrillation complicating acute myocardial infarction. SPRINT Study Group. Eur Heart J. 1992;13:45–50. doi: 10.1093/oxfordjournals.eurheartj.a060046. [DOI] [PubMed] [Google Scholar]
- 13.Clark DM, Plumb VJ, Epstein AE, Kay GN. Hemodynamic effects of an irregular sequence of ventricular cycle lengths during atrial fibrillation. J Am Coll Cardiol. 1997;30:1039–1045. doi: 10.1016/S0735-1097(97)00254-4. [DOI] [PubMed] [Google Scholar]
- 14.Onundarson PT, Thorgeirsson G, Jonmundsson E, Sigfusson N, Hardarson T. Chronic atrial fibrillation–epidemiologic features and 14 year follow-up: a case control study. Eur Heart J. 1987;8:521–527. doi: 10.1093/oxfordjournals.eurheartj.a062312. [DOI] [PubMed] [Google Scholar]
- 15.Luo C, et al. Predictive value of coronary blood flow for future cardiovascular events in patients with atrial fibrillation. Int J Cardiol. 2014;177:545–547. doi: 10.1016/j.ijcard.2014.08.102. [DOI] [PubMed] [Google Scholar]
- 16.O’Neal, W. T., Salahuddin, T., Broughton, S. T. & Soliman, E. Z. Atrial Fibrillation and Cardiovascular Outcomes in the Elderly. Pacing Clin Electrophysiol (2016). [DOI] [PubMed]
- 17.Rahman F, et al. Atrial flutter: Clinical risk factors and adverse outcomes in the Framingham Heart Study. Heart Rhythm. 2016;13:233–240. doi: 10.1016/j.hrthm.2015.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Polimeni L, Perri L, Saliola M, Basili S, Violi F. The risk of myocardial infarction in patients with atrial fibrillation: an unresolved issue. Intern Emerg Med. 2010;5:91–94. doi: 10.1007/s11739-010-0352-2. [DOI] [PubMed] [Google Scholar]
- 19.Violi, F., Soliman, E. Z., Pignatelli, P. & Pastori, D. Atrial Fibrillation and Myocardial Infarction: A Systematic Review and Appraisal of Pathophysiologic Mechanisms. J Am Heart Assoc5 (2016). [DOI] [PMC free article] [PubMed]
- 20.Lip GY, Lane DA. Does warfarin for stroke thromboprophylaxis protect against MI in atrial fibrillation patients? Am J Med. 2010;123:785–789. doi: 10.1016/j.amjmed.2010.01.031. [DOI] [PubMed] [Google Scholar]
- 21.Pastori D, et al. Incidence of myocardial infarction and vascular death in elderly patients with atrial fibrillation taking anticoagulants: relation to atherosclerotic risk factors. Chest. 2015;147:1644–1650. doi: 10.1378/chest.14-2414. [DOI] [PubMed] [Google Scholar]
- 22.Blackshear JL, et al. Aortic plaque in atrial fibrillation: prevalence, predictors, and thromboembolic implications. Stroke. 1999;30:834–840. doi: 10.1161/01.STR.30.4.834. [DOI] [PubMed] [Google Scholar]
- 23.Douxfils J, et al. Dabigatran etexilate and risk of myocardial infarction, other cardiovascular events, major bleeding, and all-cause mortality: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3:e000515. doi: 10.1161/JAHA.113.000515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tornyos A, Kehl D, D’Ascenzo F, Komocsi A. Risk of Myocardial Infarction in Patients with Long-Term Non-Vitamin K Antagonist Oral Anticoagulant Treatment. Prog Cardiovasc Dis. 2016;58:483–494. doi: 10.1016/j.pcad.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Hohnloser SH, et al. Myocardial ischemic events in patients with atrial fibrillation treated with dabigatran or warfarin in the RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) trial. Circulation. 2012;125:669–676. doi: 10.1161/CIRCULATIONAHA.111.055970. [DOI] [PubMed] [Google Scholar]
- 26.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hicks KA, et al. 2014 ACC/AHA Key Data Elements and Definitions for Cardiovascular Endpoint Events in Clinical Trials: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards) Circulation. 2015;132:302–361. doi: 10.1161/CIR.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 28.Wells GA, et al. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis. Applied Engineering in Agriculture. 2000;18:727–734. [Google Scholar]
- 29.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 30.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 33.Lake FR, Cullen KJ, de Klerk NH, McCall MG, Rosman DL. Atrial fibrillation and mortality in an elderly population. Aust N Z J Med. 1989;19:321–326. doi: 10.1111/j.1445-5994.1989.tb00271.x. [DOI] [PubMed] [Google Scholar]
- 34.Aronow WS, Ahn C, Mercando AD, Epstein S. Correlation of atrial fibrillation, paroxysmal supraventricular tachycardia, and sinus rhythm with incidences of new coronary events in 1,359 patients, mean age 81 years, with heart disease. Am J Cardiol. 1995;75:182–184. doi: 10.1016/S0002-9149(00)80074-0. [DOI] [PubMed] [Google Scholar]
- 35.Krahn AD, Manfreda J, Tate RB, Mathewson FA, Cuddy TE. The natural history of atrial fibrillation: incidence, risk factors, and prognosis in the Manitoba Follow-Up Study. Am J Med. 1995;98:476–484. doi: 10.1016/S0002-9343(99)80348-9. [DOI] [PubMed] [Google Scholar]
- 36.Kaarisalo MM, et al. Atrial fibrillation and stroke. Mortality and causes of death after the first acute ischemic stroke. Stroke. 1997;28:311–315. doi: 10.1161/01.STR.28.2.311. [DOI] [PubMed] [Google Scholar]
- 37.Benjamin EJ, et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98:946–952. doi: 10.1161/01.CIR.98.10.946. [DOI] [PubMed] [Google Scholar]
- 38.Dries DL, et al. Atrial fibrillation is associated with an increased risk for mortality and heart failure progression in patients with asymptomatic and symptomatic left ventricular systolic dysfunction: a retrospective analysis of the SOLVD trials. Studies of Left Ventricular Dysfunction. J Am Coll Cardiol. 1998;32:695–703. doi: 10.1016/S0735-1097(98)00297-6. [DOI] [PubMed] [Google Scholar]
- 39.Saxena R, Lewis S, Berge E, Sandercock PA, Koudstaal PJ. Risk of early death and recurrent stroke and effect of heparin in 3169 patients with acute ischemic stroke and atrial fibrillation in the International Stroke Trial. Stroke. 2001;32:2333–2337. doi: 10.1161/hs1001.097093. [DOI] [PubMed] [Google Scholar]
- 40.Friberg J, et al. Comparison of the impact of atrial fibrillation on the risk of stroke and cardiovascular death in women versus men (The Copenhagen City Heart Study) Am J Cardiol. 2004;94:889–894. doi: 10.1016/j.amjcard.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 41.Dhamoon MS, et al. Risk of myocardial infarction or vascular death after first ischemic stroke: the Northern Manhattan Study. Stroke. 2007;38:1752–1758. doi: 10.1161/STROKEAHA.106.480988. [DOI] [PubMed] [Google Scholar]
- 42.Goto, S. et al. Prevalence, clinical profile, and cardiovascular outcomes of atrial fibrillation patients with atherothrombosis. Am Heart J156, 855–863, 863 e852 (2008). [DOI] [PubMed]
- 43.Haywood LJ, et al. Atrial fibrillation at baseline and during follow-up in ALLHAT (Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial) J Am Coll Cardiol. 2009;54:2023–2031. doi: 10.1016/j.jacc.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 44.Ruigomez A, Johansson S, Wallander MA, Edvardsson N, Garcia Rodriguez LA. Risk of cardiovascular and cerebrovascular events after atrial fibrillation diagnosis. Int J Cardiol. 2009;136:186–192. doi: 10.1016/j.ijcard.2008.04.050. [DOI] [PubMed] [Google Scholar]
- 45.Bouzas-Mosquera A, et al. Effect of atrial fibrillation on outcome in patients with known or suspected coronary artery disease referred for exercise stress testing. Am J Cardiol. 2010;105:1207–1211. doi: 10.1016/j.amjcard.2009.12.037. [DOI] [PubMed] [Google Scholar]
- 46.Winkel TA, et al. Prognosis of atrial fibrillation in patients with symptomatic peripheral arterial disease: data from the REduction of Atherothrombosis for Continued Health (REACH) Registry. Eur J Vasc Endovasc Surg. 2010;40:9–16. doi: 10.1016/j.ejvs.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 47.Conen D, et al. Risk of death and cardiovascular events in initially healthy women with new-onset atrial fibrillation. JAMA. 2011;305:2080–2087. doi: 10.1001/jama.2011.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aguilar E, et al. Clinical outcome of stable outpatients with coronary, cerebrovascular or peripheral artery disease, and atrial fibrillation. Thromb Res. 2012;130:390–395. doi: 10.1016/j.thromres.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 49.Chao TF, et al. Acute myocardial infarction in patients with atrial fibrillation with a CHA2DS2-VASc score of 0 or 1: a nationwide cohort study. Heart Rhythm. 2014;11:1941–1947. doi: 10.1016/j.hrthm.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 50.Martinez C, Katholing A, Freedman SB. Adverse prognosis of incidentally detected ambulatory atrial fibrillation. A cohort study. Thromb Haemost. 2014;112:276–286. doi: 10.1160/TH4-04-0383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Soliman EZ, et al. Atrial fibrillation and the risk of myocardial infarction. JAMA Intern Med. 2014;174:107–114. doi: 10.1001/jamainternmed.2013.11912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Albayrak S, et al. Predictors of major adverse cardiovascular events; results of population based MELEN study with prospective follow-up. Eur Rev Med Pharmacol Sci. 2015;19:1446–1451. [PubMed] [Google Scholar]
- 53.Li CY, et al. Newly diagnosed atrial fibrillation is an independent factor for future major adverse cardiovascular events. PLoS One. 2015;10:e0123211. doi: 10.1371/journal.pone.0123211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Parisi R, et al. Psoriasis and the Risk of Major Cardiovascular Events: Cohort Study Using the Clinical Practice Research Datalink. J Invest Dermatol. 2015;135:2189–2197. doi: 10.1038/jid.2015.87. [DOI] [PubMed] [Google Scholar]
- 55.Vermond RA, et al. Incidence of Atrial Fibrillation and Relationship With Cardiovascular Events, Heart Failure, and Mortality: A Community-Based Study From the Netherlands. J Am Coll Cardiol. 2015;66:1000–1007. doi: 10.1016/j.jacc.2015.06.1314. [DOI] [PubMed] [Google Scholar]
- 56.Shih CJ, et al. Risks of Death and Stroke in Patients Undergoing Hemodialysis With New-Onset Atrial Fibrillation: A Competing-Risk Analysis of a Nationwide Cohort. Circulation. 2016;133:265–272. doi: 10.1161/CIRCULATIONAHA.115.018294. [DOI] [PubMed] [Google Scholar]
- 57.Marijon E, et al. Causes of death and influencing factors in patients with atrial fibrillation: a competing-risk analysis from the randomized evaluation of long-term anticoagulant therapy study. Circulation. 2013;128:2192–2201. doi: 10.1161/CIRCULATIONAHA.112.000491. [DOI] [PubMed] [Google Scholar]
- 58.Chen LY, Benditt DG, Alonso A. Atrial fibrillation and its association with sudden cardiac death. Circ J. 2014;78:2588–2593. doi: 10.1253/circj.CJ-14-0814. [DOI] [PubMed] [Google Scholar]
- 59.Reinier K, et al. The association between atrial fibrillation and sudden cardiac death: the relevance of heart failure. JACC Heart Fail. 2014;2:221–227. doi: 10.1016/j.jchf.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 60.Angeli F, et al. Atrial fibrillation and mortality in patients with acute myocardial infarction: a systematic overview and meta-analysis. Curr Cardiol Rep. 2012;14:601–610. doi: 10.1007/s11886-012-0289-3. [DOI] [PubMed] [Google Scholar]
- 61.Miyasaka Y, et al. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. J Am Coll Cardiol. 2007;49:986–992. doi: 10.1016/j.jacc.2006.10.062. [DOI] [PubMed] [Google Scholar]
- 62.Jabre P, et al. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review andmeta-analysis. Circulation. 2011;123:1587–93. doi: 10.1161/CIRCULATIONAHA.110.986661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Emdin CA, et al. Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies. BMJ. 2016;532:h7013. doi: 10.1136/bmj.h7013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Deo R, et al. Risk factor and prediction modeling for sudden cardiac death in women with coronary artery disease. Arch Intern Med. 2011;171:1703–1709. doi: 10.1001/archinternmed.2011.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen LY, et al. Atrial fibrillation and the risk of sudden cardiac death: the atherosclerosis risk in communities study and cardiovascular health study. JAMA Intern Med. 2013;173:29–35. doi: 10.1001/2013.jamainternmed.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Goette A, et al. Acute atrial tachyarrhythmia induces angiotensin II type 1 receptor-mediated oxidative stress and microvascular flow abnormalities in the ventricles. Eur Heart J. 2009;30:1411–1420. doi: 10.1093/eurheartj/ehp046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Range FT, et al. Impaired myocardial perfusion and perfusion reserve associated with increased coronary resistance in persistent idiopathic atrial fibrillation. Eur Heart J. 2007;28:2223–2230. doi: 10.1093/eurheartj/ehm246. [DOI] [PubMed] [Google Scholar]
- 68.Steinberg BA, et al. Higher risk of death and stroke in patients with persistent vs. paroxysmal atrial fibrillation: results from the ROCKET-AF Trial. Eur Heart J. 2015;36:288–296. doi: 10.1093/eurheartj/ehu359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Senoo K, Lip GY, Lane DA, Buller HR, Kotecha D. Residual Risk of Stroke and Death in Anticoagulated Patients According to the Type of Atrial Fibrillation: AMADEUS Trial. Stroke. 2015;46:2523–2528. doi: 10.1161/STROKEAHA.115.009487. [DOI] [PubMed] [Google Scholar]
- 70.Miyasaka Y, et al. Coronary ischemic events after first atrial fibrillation: risk and survival. Am J Med. 2007;120:357–363. doi: 10.1016/j.amjmed.2006.06.042. [DOI] [PubMed] [Google Scholar]
- 71.Kwon Y, et al. Association of Smoking, Alcohol, and Obesity with Cardiovascular Death and Ischemic Stroke in Atrial Fibrillation: The Atherosclerosis Risk in Communities (ARIC) Study and Cardiovascular Health Study (CHS) PLoS One. 2016;11:e0147065. doi: 10.1371/journal.pone.0147065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin YS, et al. Peripheral arterial disease and atrial fibrillation and risk of stroke, heart failure hospitalization and cardiovascular death: A nationwide cohort study. Int J Cardiol. 2016;203:204–211. doi: 10.1016/j.ijcard.2015.10.091. [DOI] [PubMed] [Google Scholar]
- 73.Lamberts M, et al. Antiplatelet therapy for stable coronary artery disease in atrial fibrillation patients taking an oral anticoagulant: a nationwide cohort study. Circulation. 2014;129:1577–1585. doi: 10.1161/CIRCULATIONAHA.113.004834. [DOI] [PubMed] [Google Scholar]
- 74.Lamberts M, et al. Antithrombotic treatment in patients with heart failure and associated atrial fibrillation and vascular disease: a nationwide cohort study. J Am Coll Cardiol. 2014;63:2689–2698. doi: 10.1016/j.jacc.2014.03.039. [DOI] [PubMed] [Google Scholar]
- 75.Pastori D, et al. Inadequate anticoagulation by Vitamin K Antagonists is associated with Major Adverse Cardiovascular Events in patients with atrial fibrillation. Int J Cardiol. 2015;201:513–516. doi: 10.1016/j.ijcard.2015.08.054. [DOI] [PubMed] [Google Scholar]
- 76.Piccini JP, et al. Clinical course of atrial fibrillation in older adults: the importance of cardiovascular events beyond stroke. Eur Heart J. 2014;35:250–256. doi: 10.1093/eurheartj/eht483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lauer MS, Blackstone EH, Young JB, Topol EJ. Cause of death in clinical research: time for a reassessment? J Am Coll Cardiol. 1999;34:618–620. doi: 10.1016/S0735-1097(99)00250-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


