Abstract
Objective:
It is known that depression is common in obese individuals. Besides the effects of obesity, pathogenic effects of increase in visceral and abdominal fat mass on depression are also being investigated. Our study aimed to show the relationship between visceral fat percentage detected with practical methods and the presence and severity of depression.
Materials and Methods:
Our study included 104 obese patients and 50 healthy controls. In all individuals, the severity of depression was assessed using the Beck Depression Inventory (BDI). Anthropometric measurements, visceral fat percentage, and body fat percentage were measured using the bioelectric impedance method.
Results:
The mean age was 51.5±12.3 years, and 65 participants (62.5%) were women. BDI scores were statistically higher in the obese group than in the control group (23.1±10.9 and 12.1±9.4, p<0.001). In the obese group, 63.5% of patients were depressed, and in the control group, this was 24%. Women were more depressed in the obese group, but there was no significant difference between men and women in the control group. Body fat percentage was the highest correlating parameter with depression severity. Positive correlation was found between depression severity and body mass index, waist circumference, hip circumference, and visceral fat percentage. In the logistic regression analysis, obesity was found as an independent risk factor for depression (OR: 4.84, 2.1–10.7, p<0.001).
Conclusion:
According to the results of our study, obesity is a significant and independent risk factor for depression. Obesity type and body composition are important factors that determine the severity of depression.
Keywords: Obesity, depression, body composition, bioelectric impedance
Öz
Amaç:
Depresyonun obezlerde sık görüldüğü bilinmektedir. Obezite varlığının yanında, viseral ve abdominal yağ kitlesindeki artışın depresyon üzerindeki etkileri de araştırılmaktadır. Biz de çalışmamızda pratik yöntemlerle tespit edilen viseral yağ oranı ile depresyon varlığı ve şiddeti arasındaki ilişkiyi göstermeyi amaçladık.
Gereç ve Yöntem:
Çalışmamıza 104 obez hasta ve 54 sağlıklı kontrol alındı. Tüm bireylerde depresyon şiddeti Beck depresyon ölçeği ile değerlendirildi (BDI). Antropometrik ölçümler, viseral yağ oranı ve vücut yağ oranı biyoelektrik impedans yöntemi ile ölçüldü.
Bulgular:
Ortalama yaş 51,5±12,3 olarak bulundu ve vakaların 65 tanesi (62,5%) kadındı. BDI skorları obez grupta kontrol grubuna göre istatistiksel olarak anlamlı biçimde yüksekti (23,1±10,9 ve 12,1±9,4 p<0,001). Obez gruptaki hastaların % 63,5’i, kontrol grubundakilerin ise %24’ü depresifti. Obez gruptaki kadınlarda depresyon daha fazla idi, ancak kontrol grubunda kadınlar ve erkekler arasında anlamlı fark yoktu. Vücut yağ oranı, depresyon şiddeti ile en yüksek korelasyon gösteren parametreydi. Depresyon şiddeti ile vücut kitle indeksi, bel çevresi, kalça çevresi ve viseral yağ oranı arasında pozitif korelasyon vardı. Lojistik regresyon analizinde obezite, depresyon için bağımsız bir risk faktörü olarak bulundu (OR: 4,84, 2,1–10,7, p<0,001).
Sonuç:
Çalışmamızın sonuçlarına göre, obezite depresyon için önemli ve bağımsız bir risk faktörüdür. Obezite tipi ve vücut kompozisyonu depresyonun şiddetini belirleyen önemli faktörlerdir.
Introduction
Obesity and depression are two major health problems with increasing incidence in developed countries. The relationship between these two diseases has been reviewed in many studies. Some studies have reported positive relationship, some no relationship, and some others a negative relationship (the “jolly fat” hypothesis) [1, 2]. Some studies have found a significant correlation only in women [3, 4]. This is attributed to methodological differences between studies and ethnic factors. Etiopathogenesis is not well understood, and different hypotheses have been proposed on this issue. Increased cortisol secretion secondary to the hypothalamic-pituitary-adrenal and hypothalamic-pituitary-gonadal axes, deficits in the serotoninergic system, effects of adipocytokines, and chronic inflammation are some of these hypotheses [5–9].
Obesity type and body fat distribution have gained importance as other factors influencing the relationship between obesity and depression in recent studies [10, 11]. Accordingly, abdominal obesity, which is a criterion for metabolic syndrome and related to increased risk of coronary artery disease, is reported to be closely related to depression. It has been shown that depressive symptoms increase with increased waist circumference (WC), waist-to-hip ratio (WHR), visceral fat percentage, and adipocytokine levels [8, 9, 12]. Visceral fat is measured using several methods, such as abdominal computed tomography (CT), magnetic resonance imaging (MRI), bioelectric impedance, and dual-energy X-ray absorptiometry (DXA). The basis of the bioelectric impedance method is based on the difference in electrical conductivity of lean and fat tissues. Alternating current passing through the tissue shows a voltage drop depending on the tissue-specific resistance. Electric current has difficulty passing through high-resistance tissues such as bone and fat; conversely, electric current easily passes through low-resistance tissues such as skeletal muscle and visceral organs [13]. The bioelectric impedance method is widely used in research because it is practical and inexpensive, shows a high correlation with other methods, and has no side effects [14, 15]. There are no studies in the literature evaluating the relationship between depressive disorders and body fat percentage determined by bioelectric impedance. The aim of our study is to evaluate the relationship between increased body fat percentage determined using practical measures and the presence of depression and its severity.
Materials and Methods
Patient selection and study design
This cross-sectional study included patients who were admitted to our hospital’s internal medicine outpatient clinic, aged 18–80 years, and with body mass indexes (BMIs) of ≥30 kg/m2. Patients with a history of malignancy, thyroid disease, chronic renal failure, chronic liver disease, diabetes, hypertension, cardiac disease, known psychiatric disorders, or drug use were excluded. Cigarette and alcohol use, marital status, education level, and occupational status were questioned. The control group consisted of 50 healthy persons (30 women and 20 men) with BMIs 18.5–24.99 kg/m2. The study was conducted with the approval of the local ethics committee and in compliance with the World Medical Association’s Declaration of Helsinki and the Good Clinical and Laboratory Practices guidelines. The signatures of the participants were obtained in an informed consent form.
Anthropometric measurements
Height was measured using a stadiometer, and WC and hip circumference were measured in centimeters using a tape measure. In measurements of WC, hip circumference, and WHR, WHO’s recommendations were considered [16]. Weight, BMI, body fat percentage, visceral fat percentage, and muscle ratio measurements were performed using an Omron brand BF-510 body composition measuring device. Patients were told to drink seven to eight glasses of water and not to use tea, coffee, or cigarettes one day before. Measurements were performed in the morning, after at least 8 h of sleep, and with an empty stomach and bladder. Increased body fat percentage in the obese group was evaluated as ≥22% in men and ≥33.9% in women [17]. Abdominal obesity was described as WC of ≥94 cm or WHR of ≥0.90 in men and WC of ≥80 cm or WHR of ≥0.85 in women [16]. The cutoff level was considered 10% for visceral fat percentage [18].
Laboratory analysis
After a 12-h fasting, venous blood samples of patients were collected in anticoagulant or additive-free biochemistry tubes. Glucose, total cholesterol, triglyceride, Low-density lipoprotein (LDL) cholesterol and High-density lipo-protein (HDL) cholesterol levels were studied in an Architect 1600 auto-analyzer device using Abbott clinical chemistry kits.
Depression classification
A modified Beck Depression Inventory (BDI) test consisting of 21 questions was used in assessing depression severity. In a validation study performed in a Turkish population, the cutoff value for depression was determined to be 17 [19]. In our study, BDI scores of >17 were considered to indicate depression.
Statistical analysis
Statistical analysis were performed using the Statistical Package for Social Sciences version 21.0 (IBM Corp.; Armonk, NY, USA). Variables were investigated using visual (histograms and probability plots) and analytical methods (Kolmogorov-Smirnov and Shapiro-Wilk’s tests) to determine whether or not they are normally distributed.
Descriptive analyses were presented using tables of frequencies for the ordinal variables and using medians and interquartile range for the non-normally distributed variables. Descriptive analyses were presented using means and standard deviations for normally distributed variables. Ordinal and continuous variables that did not have normal distribution were compared using the Mann-Whitney U test. The student’s t-test was used to evaluate differences between the two study subgroups in normally distributed continuous variables. Correlations among the study variables were tested using the Pearson and Spearman correlation coefficient according to the suitability of data. For multivariate analysis, the possible factors identified with univariate analyses were further entered into a logistic regression analysis to determine independent predictors of depression. Hosmer-Lemeshow goodness of fit test was used to assess model fit. A 5% type I error level was considered to indicate statistical significance.
Results
The study involved 104 patients conforming to the definition of obesity. The control group was composed of 50 healthy volunteers. The mean age was 51.5±12.3, and 65 (62.5%) and 39 (37.5%) of the cases were women and men, respectively. There was no significant difference between the control and obese groups in terms of age, sex, or smoking and alcohol use. The unmarried rate was higher in the control group than in the obese group, but this difference was not significant (control: 38%, obese: 24%, p=0.73). In the obese group, the numbers of uneducated, educated for less than 6 years, and retired individuals were significantly higher than those in the control group (Table 1).
Table 1.
Demographic characteristics of study population
| Obese group (n=104) | Control group (n=50) | p | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean age (years) | 51.5±12.3 | 48.7±11.7 | >0.05 | |||
|
|
|
|||||
| n | % | n | % | |||
| Sex | Male | 39 | 37.5 | 20 | 40 | >0.05 |
| Female | 65 | 62.5 | 30 | 60 | ||
| Smoking | Present | 33 | 31.7 | 18 | 36 | >0.05 |
| Absent | 71 | 68.3 | 32 | 64 | ||
| Alcohol intake | Present | 11 | 10.6 | 5 | 10 | >0.05 |
| Absent | 93 | 89.4 | 45 | 90 | ||
| Exercise status | Present | 30 | 28.8 | 25 | 50 | <0.05 |
| Absent | 74 | 71.2 | 25 | 50 | ||
| Marital status | Single | 7 | 6.7 | 14 | 28 | |
| Married | 79 | 76 | 31 | 62 | ||
| Divorced | 6 | 5.8 | 1 | 2 | ||
| Widowed | 12 | 11.5 | 4 | 8 | ||
| Education level (years) | Uneducated | 9 | 8.7 | 2 | 4 | |
| <6 | 42 | 40.4 | 12 | 24 | ||
| 6–12 | 40 | 38.5 | 21 | 42 | ||
| >12 | 13 | 12.5 | 15 | 30 | ||
| Occupational status | Unemployed | 38 | 36.5 | 15 | 30 | |
| Employee | 31 | 29.8 | 27 | 54 | ||
| Employer | 14 | 13.5 | 5 | 10 | ||
| Retired | 21 | 20.2 | 3 | 6 | ||
Comparison of anthropometric measurements and laboratory data
Body fat percentage, visceral fat percentage, aspartate transaminase (AST), alanine transaminase (ALT), gamma-glutamyltransferase (GGT), Alkaline phosphatase (ALP), fasting plasma glucose, total cholesterol, LDL cholesterol, and triglyceride levels were significantly higher in the obese group than in the control group (Table 2).
Table 2.
Anthropometric measurements and laboratory results
| Obese group (n=104) | Control group (n=50) | p | |
|---|---|---|---|
| BMI (kg/m2) | 34.6 (32.2–38.7) | 22.5 (21–23.3) | <0.001 |
| Waist circumference (cm) | 108 (92–119.7) | 73 (66.7–81) | <0.001 |
| Hip circumference (cm) | 117.1±10.2 | 93.2±6.1 | <0.001 |
| Body fat percentage (%) | 45 (33–51.4) | 24.1 (15.6–31.8) | <0.001 |
| Visceral fat percentage (%) | 14 (11–17) | 5 (3.7–6) | <0.001 |
| Muscle ratio (%) | 24.3 (21.5–29.9) | 34.1 (28.1–39.1) | <0.001 |
| AST (U/dL) | 19.5 (15.2–23) | 15.5 (13–20.5) | <0.05 |
| ALT (U/mL) | 21 (16–29.7) | 13.5 (11–18) | <0.001 |
| ALP (U/mL) | 72 (60–90) | 63.5 (50–76) | <0.05 |
| GGT (U/dL) | 28 (20.2–40.7) | 16.5 (12.7–27.2) | <0.001 |
| Fasting glucose (mg/dL) | 99.5 (91–119.7) | 84 (76.7–93.2) | <0.001 |
| Total cholesterol (mg/dL) | 216.1±45.7 | 180.9±44.5 | <0.001 |
| LDL (mg/dL) | 137 (110–171.5) | 112.5 (95–132.5) | <0.001 |
| HDL (mg/dL) | 43 (36–51) | 47 (38.7–61.2) | >0.05 |
| Triglyceride (mg/dL) | 146 (95.2–213.5) | 74.5 (53–116.5) | <0.001 |
BMI: Body Mass Index; AST: aspartate aminotransferase; ALT: alanine aminotransferase; ALP: alkaline phosphatase; GGT: gamma-glutamyltransferase
Values are presented using mean±standard deviations for normally distributed and medians and first and third quartiles in the brackets for the non-normally distributed variables.
Demographic findings and depression relations
Beck Depression Inventory scores of the unemployed in the obese group were significantly higher than those of the employed (22.8±11.2 and 16.3±11.2, respectively, p<0.001). There was no difference in depression scores in the control group according to occupational status. Depression scores were similar in both the obese and control groups in terms of educational level, marital status, smoking and alcohol use, and exercise level.
Obesity, body composition, and depression relations
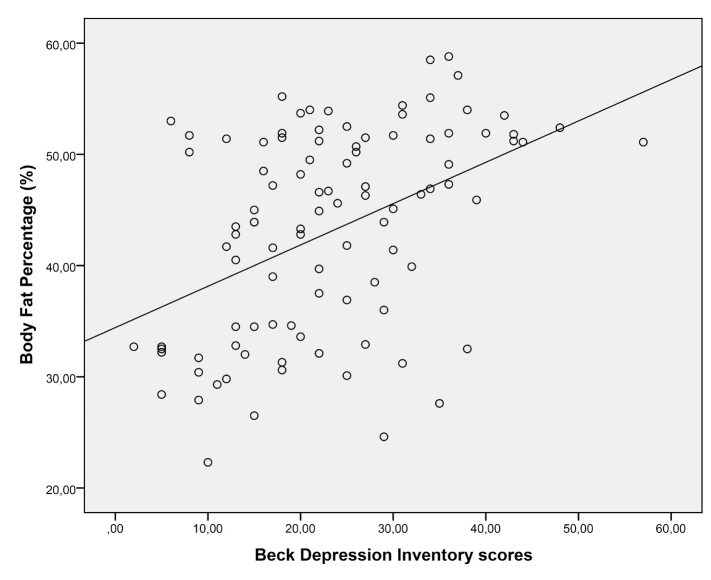
Beck Depression Inventory scores in the obese group were significantly higher than those in the control group (23.1±10.9 and 12.1±9.4, p<0.001). In the obese group, 63.5% of patients were depressed, while 24% of patients were depressed in the control group. In the obese group, women were significantly more depressed, but there was no significant difference between sexes in the control group. There was a positive and significant correlation between depression severity and BMI, WC, hip circumference, WHR, body fat percentage, and visceral fat percentage. In these parameters, the highest correlation with depression severity was with body fat percentage (r: 0.53, p<0.001) (Figure 1). In laboratory evaluations, this correlation was found only with fasting plasma glucose (Table 3). In patients with depression according to BDI scores in the obese group, WC, hip circumference, body fat percentage, and visceral fat percentage were significantly higher than in those without depression (Table 4). In logistic regression analysis, the risk of depression in the obese group was found to be significantly higher, independent of age, sex, occupational status, and educational level (OR: 4.84, 2.1–10.7, p<0.001).
Figure 1.
Correlation graphic between body fat percentage and beck depression scores.
Table 3.
Correlation analysis between BDI score and obesity-related measurements
| r | p | ||
|---|---|---|---|
| BDI score | BMI | 0.50 | <0.001 |
| Body fat percentage | 0.53 | <0.001 | |
| Visceral fat percentage | 0.35 | <0.001 | |
| Muscle ratio | −0.43 | <0.001 | |
| Waist circumference | 0.42 | <0.001 | |
| Hip circumference | 0.52 | <0.001 | |
| WHR | 0.15 | 0.62 | |
| Fasting glucose | 0.40 | <0.001 |
BDI: Beck Depression Inventory; BMI: Body Mass Index; WHR: waist-to-hip ratio
Table 4.
Comparison of body compositions between depressed and non-depressed patients in the obese group
| Depression present | Depression absent | p | |
|---|---|---|---|
| Waist circumference | 112 (106–120.2) | 109 (99.7–114.7) | 0.01 |
| Hip circumference | 118±9.9 | 114.1±10.2 | 0.02 |
| Waist-to-hip ratio | 0.96 (0.9–1) | 0.97 (0.8–1) | 0.84 |
| Body fat percentage | 48.6 (38.2–51.9) | 39.7 (32.1–45.4) | <0.001 |
| Visceral fat percentage | 14 (12–18) | 12 (10–17) | 0.02 |
Values are presented using means±standard deviations for normally distributed and medians and first and third quartiles in the brackets for the non-normally distributed variables.
Discussion
Although there are many studies on the relationship between depression and obesity, the relationship and pathogenesis are still controversial [1, 2, 4]. In this study, obese and healthy subjects were compared for the presence and severity of depression. Furthermore, obese individuals with and without abdominal obesity were evaluated for depression characteristics. Our study indicated that depression is more frequent and severe in the obese and that abdominal obesity and increased body fat percentage also contributes to this. In the literature, some similar studies evaluated body fat percentage and visceral fat percentage with MRI, CT, and DXA, but these methods cannot be easily applied in clinical practice [20, 21]. In our study, when investigating the relationship between depression and body fat percentage and visceral fat percentage, the bioelectric impedance method was used to measure fat ratios, which is a more practical method. In Crisp and McGuiness’s study in 1976, in middle-aged men and women living outside the city, obesity was found to be associated with lower anxiety. Furthermore, in same study, obesity was found to be associated with lower levels of depression in men [1]. Although this study raised the “jolly fat” hypothesis, studies in later years obtained different results. Some studies have reported that obese people have an increased risk of depression, and in some other studies, middle-aged, overweight people were less depressed [2, 22–25]. A few studies have indicated that obesity does not affect depression risk [26–28]. In our study, the severity of depression in obese individuals was found to be significantly higher than that in normal individuals. These different results in the literature may be related to differences in study populations or definitions of obesity and depression.
The images shown by the media and the dominant impression of underweight people in the general population affect an individual’s perception of weight. In addition, negative criticism made to overweight individuals contributes to this [26]. It has been shown that medium and high-grade psychological distress is more frequent in normal BMI patients with overweight perception than obese individuals [29]. Gavin et al. [30] found in their study, which included 4523 women, that body image dissatisfaction mediates the obesity-depression association. In parallel with this study, the opinion that the relationship between obesity and depression may vary depending on sex has been suggested. Likewise, a large study indicated that the prevalence of depression is higher in obese women than in obese men [31]. A study performed by Carpenter et al. [4] indicated that the presence of depression was associated with high BMIs in women and low BMIs in men. Our study similarly supported the results in the literature, indicating that depression scores were significantly higher in obese women than in obese men.
The studies investigating the cause of the relationship between obesity and depression focus on “impairment in the hypothalamic-pituitary-adrenal axis” [5]. Cortisol secretion is regulated by this axis, and in depressive disorders, defects are formed in cortisol secretion. Cortisol causes central adiposity, and also many studies have found a relationship between central adiposity and depression [32, 33]. In our study, we found a significant correlation between depression severity and WC, supporting previous results. In the study performed by Weber-Hamann et al. [5], visceral fat percentage was measured by CT, and hypercortisolemic depressed patients showed greater visceral fat deposits than normocortisolemic patients. Although we performed a different method, visceral fat percentage is correlated with the severity of depression in our study, like in the study by Weber-Hamann et al. [5].
In study by Johnston et al. [34] of 2431 individuals with BMIs of ≥18.5 kg/m2, a lack of education was shown to be an independent risk factor for the presence of depression. Also, the Alameda study obtained similar results [35]. In accordance with these results, in our study, individuals with higher education levels were found to have lower depression severity.
A limitation of our study was the use of BDI as a screening test. We evaluated patients who had not been diagnosed with any psychiatric disease before. Our aim was to determine the severity of depression between two groups. It could be better to compose a depressed group from patients with a diagnosis of depression before.
According to the results of our study, depression is common and more severe in obese than in normal-weight individuals. However, besides the presence of obesity, the type of obesity seems to be important. Among depressed and obese individuals, those who have high visceral and body fat percentages and abdominal obesity have to be treated firstly for depression, and after this, it may be appropriate to treat obesity. However, because depressed individuals have increased visceral and body fat percentages, these individuals could be recommended to take precautions regarding cardiovascular risks.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the medical ethics committee of Bakırköy Dr. Sadi Konuk Training and Research Hospital (17.05.2010/19).
Informed Consent: Written informed consent was obtained from patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - U.I.K., A.R.K., E.B.O.; Design - U.I.K., O.H.K.; Supervision - U.I.K., Z.E., A.R.K., E.B.O., O.H.K.; Resource - U.I.K., E.B.O.; Materials - U.I.K., E.B.O.; Data Collection and/or Processing - A.R.K., Z.E.; Analysis and /or Interpretation - U.I.K., A.R.K.; Literature Search - U.I.K.; Writing - U.I.K.; Critical Reviews - A.R.K., O.H.K.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Crisp AH, McGuiness B. Jolly fat: relation between obesity and psychoneurosis in general population. Br Med J. 1976;1:7–9. doi: 10.1136/bmj.1.6000.7. https://doi.org/10.1136/bmj.1.6000.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palinkas LA, Wingard DL, Barrett-Connor E. Depressive symptoms in overweight and obese older adults: a test of the “jolly fat” hypothesis. J Psychosom Res. 1996;40:59–66. doi: 10.1016/0022-3999(95)00542-0. https://doi.org/10.1016/0022-3999(95)00542-0. [DOI] [PubMed] [Google Scholar]
- 3.Istvan J, Zavela K, Weidner G. Body weight and psychological distress in NHANES I. Int J Obes Relat Metab Disord. 1992;16:999–1003. [PubMed] [Google Scholar]
- 4.Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90:251–7. doi: 10.2105/ajph.90.2.251. https://doi.org/10.2105/AJPH.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weber-Hamann B, Hentschel F, Kniest A, et al. Hypercortisolemic depression is associated with increased intra-abdominal fat. Psychosom Med. 2002;64:274–7. doi: 10.1097/00006842-200203000-00010. https://doi.org/10.1097/00006842-200203000-00010. [DOI] [PubMed] [Google Scholar]
- 6.de Kloet ER. Hormones, brain and stress. Endocr Regul. 2003;37:51–68. [PubMed] [Google Scholar]
- 7.Wurtman JJ. Depression and weight gain: the serotonin connection. J Affect Disord. 1993;29:183–92. doi: 10.1016/0165-0327(93)90032-f. https://doi.org/10.1016/0165-0327(93)90032-F. [DOI] [PubMed] [Google Scholar]
- 8.Soczynska JK, Kennedy SH, Woldeyohannes HO, et al. Mood disorders and obesity: understanding inflammation as a pathophysiological nexus. Neuromolecular Med. 2011;13:93–116. doi: 10.1007/s12017-010-8140-8. https://doi.org/10.1007/s12017-010-8140-8. [DOI] [PubMed] [Google Scholar]
- 9.Morris AA, Ahmed Y, Stoyanova N, et al. The association between depression and leptin is mediated by adiposity. Psychosom Med. 2012;74:483–8. doi: 10.1097/PSY.0b013e31824f5de0. https://doi.org/10.1097/PSY.0b013e31824f5de0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vogelzangs N, Kritchevsky SB, Beekman AT, et al. Depressive symptoms and change in abdominal obesity in older persons. Arch Gen Psychiatry. 2008;65:1386–93. doi: 10.1001/archpsyc.65.12.1386. https://doi.org/10.1001/archpsyc.65.12.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Everson-Rose SA, Lewis TT, Karavolos K, Dugan SA, Wesley D, Powell LH. Depressive symptoms and increased visceral fat in middle-aged women. Psychosom Med. 2009;71:410–6. doi: 10.1097/PSY.0b013e3181a20c9c. https://doi.org/10.1097/PSY.0b013e3181a20c9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao G, Ford ES, Li C, Tsai J, Dhingra S, Balluz LS. Waist circumference, abdominal obesity, and depression among overweight and obese U.S. adults: National Health and Nutrition Examination Survey 2005–2006. BMC Psychiatry. 2011;11:130. doi: 10.1186/1471-244X-11-130. https://doi.org/10.1186/1471-244X-11-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baumgartner RN, Chumlea WC, Roche AF. Bioelectric impedance for body composition. Exerc Sport Sci Rev. 1990;18:193–224. https://doi.org/10.1249/00003677-199001000-00009. [PubMed] [Google Scholar]
- 14.Houtkooper LB, Going SB, Lohman TG, Roche AF, Van Loan M. Bioelectrical impedance estimation of fat-free body mass in children and youth: a cross-validation study. J Appl Physiol. 1992;72:366–73. doi: 10.1152/jappl.1992.72.1.366. [DOI] [PubMed] [Google Scholar]
- 15.Shanholtzer BA, Patterson SM. Use of bioelectrical impedance in hydration status assessment: reliability of a new tool in psychophysiology research. Int J Psychophysiol. 2003;49:217–26. doi: 10.1016/s0167-8760(03)00143-0. https://doi.org/10.1016/S0167-8760(03)00143-0. [DOI] [PubMed] [Google Scholar]
- 16.Nishida C, Ko GT, Kumanyika S. Body fat distribution and noncommunicable diseases in populations: overview of the 2008 WHO Expert Consultation on Waist Circumference and Waist-Hip Ratio. Eur J Clin Nutr. 2010;64:2–5. doi: 10.1038/ejcn.2009.139. https://doi.org/10.1038/ejcn.2009.139. [DOI] [PubMed] [Google Scholar]
- 17.Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72:694–701. doi: 10.1093/ajcn/72.3.694. [DOI] [PubMed] [Google Scholar]
- 18.Eren İ, Erdi Ö. Obez hastalarda psikiyatrik bozuklukların sıklığı. Klin Psikiyatri. 2003;6:152–7. [PubMed] [Google Scholar]
- 19.Hisli N. Beck Depresyon Envanteri’nin geçerliliği üzerine bir çalışma. Turk Psikol Derg. 1988;6:118–26. [Google Scholar]
- 20.Jebb SA, Goldberg GR, Jennings G, Elia M. Dual-energy X-ray absorptiometry measurements of body composition: effects of depth and tissue thickness, including comparisons with direct analysis. Clin Sci (Lond) 1995;88:319–24. doi: 10.1042/cs0880319. https://doi.org/10.1042/cs0880319. [DOI] [PubMed] [Google Scholar]
- 21.Seidell JC, Bakker CJ, van der Kooy K. Imaging techniques for measuring adipose-tissue distribution--a comparison between computed tomography and 1.5-T magnetic resonance. Am J Clin Nutr. 1990;51:953–7. doi: 10.1093/ajcn/51.6.953. [DOI] [PubMed] [Google Scholar]
- 22.Ross CE. Overweight and depression. J Health Soc Behav. 1994;35:63–79. https://doi.org/10.2307/2137335. [PubMed] [Google Scholar]
- 23.Roberts RE, Kaplan GA, Shema SJ, Strawbridge WJ. Are the obese at greater risk for depression? Am J Epidemiol. 2000;152:163–70. doi: 10.1093/aje/152.2.163. https://doi.org/10.1093/aje/152.2.163. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan PW, Ghushchyan V, Wyatt HR, Wu EQ, Hill JO. Impact of cardiometabolic risk factor clusters on health-related quality of life in the U.S. Obesity (Silver Spring) 2007;15:511–21. doi: 10.1038/oby.2007.580. https://doi.org/10.1038/oby.2007.580. [DOI] [PubMed] [Google Scholar]
- 25.Stewart AW, Jackson RT, Ford MA, Beaglehole R. Underestimation of relative weight by use of self-reported height and weight. Am J Epidemiol. 1987;125:122–6. doi: 10.1093/oxfordjournals.aje.a114494. https://doi.org/10.1093/oxfordjournals.aje.a114494. [DOI] [PubMed] [Google Scholar]
- 26.Friedman N, Fanning EL. Overweight and obesity: an overview of prevalence, clinical impact, and economic impact. Dis Manag. 2004;7(Suppl 1):S1–6. doi: 10.1089/1093507042317152. https://doi.org/10.1089/dis.2004.7.S-1. [DOI] [PubMed] [Google Scholar]
- 27.Faubel M. Body image and depression in women with early and late onset obesity. J Psychol. 1989;123:385–95. doi: 10.1080/00223980.1989.10542993. https://doi.org/10.1080/00223980.1989.10542993. [DOI] [PubMed] [Google Scholar]
- 28.Hällström T, Noppa H. Obesity in women in relation to mental illness, social factors and personality traits. J Psychosom Res. 1981;25:75–82. doi: 10.1016/0022-3999(81)90093-3. https://doi.org/10.1016/0022-3999(81)90093-3. [DOI] [PubMed] [Google Scholar]
- 29.Faith MS, Matz PE, Jorge MA. Obesity-depression associations in the population. J Psychosom Res. 2002;53:935–42. doi: 10.1016/s0022-3999(02)00308-2. https://doi.org/10.1016/S0022-3999(02)00308-2. [DOI] [PubMed] [Google Scholar]
- 30.Gavin AR, Simon GE, Ludman EJ. The association between obesity, depression, and educational attainment in women: the mediating role of body image dissatisfaction. J Psychosom Res. 2010;69:573–81. doi: 10.1016/j.jpsychores.2010.05.001. https://doi.org/10.1016/j.jpsychores.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beydoun MA, Wang Y. Pathways linking socioeconomic status to obesity through depression and lifestyle factors among young US adults. J Affect Disord. 2010;123:52–63. doi: 10.1016/j.jad.2009.09.021. https://doi.org/10.1016/j.jad.2009.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosmond R, Björntorp P. Quality of life, overweight, and body fat distribution in middle-aged men. Behav Med. 2000;26:90–4. doi: 10.1080/08964280009595757. https://doi.org/10.1080/08964280009595757. [DOI] [PubMed] [Google Scholar]
- 33.Larsson B, Seidell J, Svärdsudd K, et al. Obesity, adipose tissue distribution and health in men--the study of men born in 1913. Appetite. 1989;13:37–44. doi: 10.1016/0195-6663(89)90025-1. https://doi.org/10.1016/0195-6663(89)90025-1. [DOI] [PubMed] [Google Scholar]
- 34.Johnston E, Johnson S, McLeod P, Johnston M. The relation of body mass index to depressive symptoms. Can J Public Health. 2004;95:179–83. doi: 10.1007/BF03403643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roberts RE, Deleger S, Strawbridge WJ, Kaplan GA. Prospective association between obesity and depression: evidence from the Alameda County Study. Int J Obes Relat Metab Disord. 2003;27:514–21. doi: 10.1038/sj.ijo.0802204. https://doi.org/10.1038/sj.ijo.0802204. [DOI] [PubMed] [Google Scholar]