Abstract
Background
A 57-year-old male diagnosed with Plasmodium vivax malaria presented with a subacute onset of hand tremor, slowness, and gait difficulty.
Phenomenology
A bilateral upper extremity kinetic tremor was seen, as well as a right upper extremity rigidity and body bradykinesia.
Educational Value
Parkinsonism and tremor are neurological manifestations that may occur in malaria as a result of globus pallidi and dentate nuclei involvement.
Keywords: Parkinsonism, tremor, malaria, cerebral, Plasmodium vivax
A 57-year-old male presented with hand tremor, bradykinesia, and gait difficulty. The patient visited an emergency room with initial symptoms of persistent fevers and myalgia. Temperature was 39.1°C, blood pressure 85/54, heart rate 129 bpm, respiratory rate 18 and 99% SpO2. Laboratory results were notable for a mild anemia (hemoglobin of 11.7 g/dL; reference values 13–17 g/dL), thrombocytopenia (platelet count of 35,000; reference values 150–400 × 103/µL), and elevated transaminase (aspartate aminotransferase 42; reference values <40, alanine aminotransferase 59; reference values <41). As he lived in an endemic area for malaria (Kyong-gi province) and engaged in gardening, serological testing for malaria antibodies (Abs) and antigens (Ags) (i.e., Plasmodium falciparum, Plasmodium vivax) was performed, which was positive for P. vivax Ag and Ab. Microscopy of a peripheral blood smear confirmed the presence of P. vivax. He was diagnosed with malaria and completed a 2-week course of chloroquine 2,000 mg and primaquine 26.3 mg every day.
The patient presented to our institution approximately 4 weeks following treatment of malaria with symptoms of hand tremor, slowness, and gait difficulty (Figure 1). He stated that these symptoms had developed during the course of treatment for malaria. On neurological examination, hypomimia and hypophonia were noted. Tone was increased in the right upper extremity, and a bilateral upper extremity kinetic tremor was seen. Mild limb bradykinesia was noted on finger tapping in the right upper extremity and on opening and closing of both hands. Decreased right arm swing and en-bloc turning was noted on gait and postural instability. The Unified Parkinson Disease Rating Scale part III was 11 (Video 1).
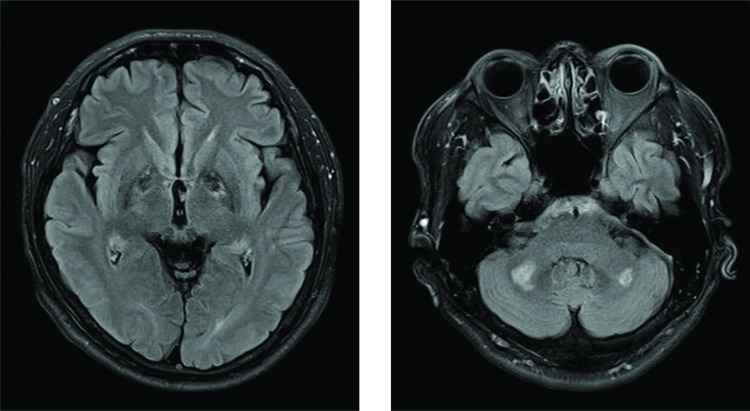
Figure 1. Magnetic Resonance Imaging of the Brain: Fluid-attenuated Inversion Recovery Sequence. Hyperintensities are seen in bilateral globus pallidi (left). Hyperintense lesions are noted in bilateral dentate nuclei (right).
Video 1. Patient on Initial Visit to our Institution. Hypomimia and hypophonia are noted, as well as a kinetic tremor of both upper extremities. Body bradykinesia and en-bloc turning is seen on casual gait. Postural instability is noted on the pull test.
Brain magnetic resonance imaging revealed hyperintensities of bilateral globus pallidi on fluid-attenuated inversion recovery (FLAIR). Hyperintensities in the bilateral dentate nuclei of the cerebellum were also seen on T2 and FLAIR sequences. The patient was started on carbidopa–levodopa 25–100 mg three times a day, and experienced mild improvement of body bradykinesia.
Discussion
We report a case of Parkinsonism and tremor in a patient diagnosed with malaria. P. vivax is the main etiology for malaria in South Korea, mostly present along the demilitarized zone.1 Our patient’s initial presentation of fevers and myalgia is consistent with the clinical picture of malaria.2 The hand tremor, slowness and gait difficulty however, is an unusual presentation. Cerebral malaria is a rare complication (2.4% incidence in P. vivax infection),1,3 which can result in cerebral edema and increased mortality,3 but Parkinsonism has not been previously reported. Cerebral malaria has been reported to result in diffuse edema and less commonly, bithalamic and cerebellar lesions in P. falciparum malaria.3 In our patient, globus pallidi and cerebellar involvement may have occurred as a result of hypoxic–ischemic injury. We presume that the globus pallidi lesions resulted in the Parkinsonian features including bradykinesia, rigidity and postural instability. The hand tremor, however, is likely secondary to dentate nuclei involvement, as this was seen as a largely symmetric kinetic tremor, not consistent with the resting tremor seen in Parkinsonism.
Footnotes
Funding: None.
Financial Disclosures: Dr. Park has received research grants from the Dystonia Medical Research Foundation, SK chemicals, and the National Research Foundation of Korea.
Conflicts of Interest: The author reports no conflict of interest.
Ethics Statement: All patients that appear on video have provided written informed consent; authorization for the videotaping and for publication of the videotape was provided.
References
- 1.Im JH, Kwon HY, Baek J, et al. Severe Plasmodium vivax infection in Korea. Malar J. 2017;16:51. doi: 10.1186/s12936-017-1684-4. doi: 10.1186/s12936-017-1684-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Svenson JE, MacLean JD, Gyorkos TW, Keystone J. Imported malaria. Clinical presentation and examination of symptomatic travelers. Arch Intern Med. 1995;155:861–868. doi: 10.1001/archinte.155.8.861. doi: 10.1001/archinte.1995.00430080109013. [DOI] [PubMed] [Google Scholar]
- 3.Patankar TF, Karnad DR, Shetty PG, Desai AP, Prasad SR. Adult cerebral malaria: prognostic importance of imaging findings and correlation with postmortem findings. Radiology. 2002;224:811–816. doi: 10.1148/radiol.2243010588. doi: 10.1148/radiol.2243010588. [DOI] [PubMed] [Google Scholar]