Abstract
INTRODUCTION:
The concept of sexual dysfunction is dysfunction in desire and emotional – social that it is Impact on the sexual response cycle and can cause stress and interpersonal difficulties. Quality of marital relationship is one of the important factors predicting sexual function disorders, which varies among different cancers. The purpose of this study is to determine the relationship between sexual dysfunction and quality of marital relationship in genital and breast cancers in women.
METHODS:
This correlational study was conducted on 150 breast and genital cancers in women referred to Sayedoshohada and Milad hospitals in Isfahan city through a two-stage sampling method. Participants completed questionnaires about demographic/disease and sexual function questionnaire (44 questions) and quality of marital relationship (11 questions). Collected data were analyzed using SPSS version 14 software, statistical test such as, Pearson correlation coefficient tests independent t- student, one way ANOVA.
RESULTS:
The results showed that 70.7% of women had breast cancer and 29.3% had gynaecological cancer. 60% of patient had good quality of marital relationship and 19.3% sexual dysfunction. There was a significant correlation between sexual function and quality of marital relationship (P = <0.001).
CONCLUSION:
There was a significant correlation between sexual function disorder and quality of marital relationship. The inclusion of patients educational programs and couple therapy in cancer disease rehabilitation program is important in order to improve the quality of marital relationship and subsequent sexual dysfunction in cancer patients.
Keywords: Cancer, marital, sexual function
Introduction
Sexual dysfunction in women creates considerable distresses for the person which generally are divided into four categories: (1) Desire disorder, (2) arousal disorder, (3) orgasmic disorder, and (4) pain disorder. Moreover, this disorder is divided into primary and secondary categories. Increasing evidence suggests that the desire is related to before the onset of sexual activity and during the sexual activity; however, probably both spouses appropriately achieve it and its existence is not necessary for pleasure and sexual satisfaction. In fact, the inability to begin sexual desire and arousal during sexual intercourse and initial lack of the desire are considered as the desire disorder. Therefore, the integration of sexual problems and the desire problems in the form of a disorder seems reasonable.[2] Approximately 13% of women in the world and 11% of women in the United States are suffering from various types of gynecologic cancers.[3] Meanwhile, the prevalence of sexual dysfunction in women with gynecologic cancer is up to 80%,[4] and the prevalence of sexual dysfunction is 31.15%.[5,6] Some factors affecting sexual response are age, type of treatment, and diseases, especially chronic diseases.[7,8,9] Because of some reasons, diseases are important factors in creating sexual problems.[10] Cancers, particularly women's cancers, are noted as the most influential diseases, and according to the organ involved, each of these diseases affects sexual cycle.[11] Diagnosis of cancer can have an adverse effect on sexual activity.[12] In this regard, a study in 2002 showed that symptoms of sexual dysfunction, especially reduced sexual satisfaction and dyspareunia are the first symptoms which lead to treatment stress for cervical cancer.[13] A prospective study on women with ovarian cancer showed that ovarian cancer can lead to reduced sexual desire, vaginal dryness, dyspareunia, and problems during orgasm. In this study, more than 60% of people had shown symptoms of sexual dysfunction. It also showed that low age of marriage, lack of receiving treatment, body image and good self-confidence, and long after the end of treatment are all influential on sexual activity.[14] Sexual problems in women with gynecological cancer and breast cancer are decreased sexual desire, dyspareunia, vaginal dryness related to the size, and type of treatment.[15] In this regard, Añelo and Bakool study showed the diagnosis and treatment of cancer have an enormous impact on psychological and sexual performance and sexual relations of the person.[16,17] It should be noted that sexual orientation is one of the most important aspects of life that is strongly related to biological, psychological, social, and cultural factors. It is also known as one of the factors affecting interpersonal communication, and if a couple does not show this behavior in life, that life is considered superficial and meaningless.[18] Meanwhile, cultural factors have a great impact on the quality and satisfaction of spousal relationship, and results of studies obtained from various countries have been different.[19] For example, a study conducted by Hinnen in the UK showed that women with breast cancer have low satisfaction from their married life.[20] Despite numerous studies, especially in developed countries, conducting sexual research in Iran has been difficult due to cultural, social, and family restrictions.[21] According to the Iranian family culture, marital relationship is a highly personal and private matter; therefore, treatment programs and medical and care follow-up of patients have not been discussed very often. Evaluating studies conducted in Iran shows that most of these studies have focused on the quality of life in cancer patients, and the less attention has been paid to the impact of the disease on close relationships of couples in various aspects, sexual excitement, love, devotion, commitment, and satisfaction.[22] Considering the high rate incidence of breast and gynecologic cancers among women, necessity of attention to the quality of relationships with their husbands is of utmost importance; moreover, the role of sexual aspect as one of the factors affecting the quality of the patients’ relationships with their husbands has always been considered significant. Therefore, the researcher of this study aimed to determine the relationship between sexual dysfunction and the quality of relationship with spouse in women with breast and genital cancers.
Methods
This cross-sectional study was conducted on 150 patients with breast and genital cancers who referred to Milad and Seyed-Al-Shohada hospitals in Isfahan in 2011–2013. In the present study, considering that in articles, relative frequency or prevalence of sexual dysfunction in people with genital and breast cancers has not been determined, the sample size is calculated as P = 0.5, and samples were obtained from the following formula: (Z confidence coefficient is 95%, i.e., 1.96, P = 0.5, D or the accuracy is 0.08). 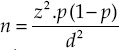 Based on this formula, the sample size is at least 150. Convenience sampling was carried out to select the patients from two Cancer Hospital in Isfahan. Researchers got a letter-of-introduction from the nursing and midwifery faculty, which was addressed to these two hospitals. After presenting the letter of introduction and explanation about research purposes, researchers asked the eligible patients, selected based on inclusion and exclusion criteria, to complete questionnaires. Inclusion criteria included married women, genital and breast cancers, passing of at least 1 year after treatment, being under coverage of Milad Hospital and Seyed-Al-Shohada, lack of sexual dysfunction before cancer diagnosis, avoiding the use of drugs that interfere with sexual function (such as antihypertensive drugs, antipsychotics, etc.), lack of diseases that interfere with sexual function, (including multiple sclerosis and Alzheimer's disease). Lack of any central nervous system disorders, severe depression, mental retardation, vasculitis, hypothyroidism and hyperthyroidism, genital trauma, tumors and masses, and dissatisfaction in completing the questionnaire were the exclusion criteria.
Based on this formula, the sample size is at least 150. Convenience sampling was carried out to select the patients from two Cancer Hospital in Isfahan. Researchers got a letter-of-introduction from the nursing and midwifery faculty, which was addressed to these two hospitals. After presenting the letter of introduction and explanation about research purposes, researchers asked the eligible patients, selected based on inclusion and exclusion criteria, to complete questionnaires. Inclusion criteria included married women, genital and breast cancers, passing of at least 1 year after treatment, being under coverage of Milad Hospital and Seyed-Al-Shohada, lack of sexual dysfunction before cancer diagnosis, avoiding the use of drugs that interfere with sexual function (such as antihypertensive drugs, antipsychotics, etc.), lack of diseases that interfere with sexual function, (including multiple sclerosis and Alzheimer's disease). Lack of any central nervous system disorders, severe depression, mental retardation, vasculitis, hypothyroidism and hyperthyroidism, genital trauma, tumors and masses, and dissatisfaction in completing the questionnaire were the exclusion criteria.
The data collection tools in this research were personal/disease demographic questionnaire, sexual dysfunction disorder questionnaire (in the form of four subsets of pain disorder, orgasmic disorder, arousal disorder, and sexual aversion), and the questionnaire of quality of relationships with partner, this questionnaire measures sexual dysfunction related to two stages of life (early marriage, recent infection). In this study, two standard questionnaires of female sexual function index (FSFI) (19 questions) and Sexual Function-Vaginal Changes Questionnaire (SVQ) (26 questions) were used to determine the sexual dysfunction. The validity of FSFI questionnaire was approved by content validity in the studies, including Beigi et al. and its reliability was confirmed using Cronbach's alpha coefficient (α = 0.875).[23] Questionnaire SVQ was used by jensen (2004) for the first time in cancer patients,[24] and the content validity and reliability of the Persian version were approved by Mohamadirizi et al. in cancer patients.[25]
The questionnaire of quality of relationships with partner is a researcher-made questionnaire that for the first time was developed by Beigi et al. in Iran. This questionnaire includes 11 questions based on Likert scale ranging from not at all to very much and its content validity and reliability have been confirmed in this study (Cronbach's alpha 0.925).[23] Finally, the information on 150 eligible women with breast and genital cancers were analyzed. Data were analyzed by Student's t-test, Mann–Whitney, ANOVA, Chi-square, and Pearson correlation coefficient using SPSS software version 11.5 [SPSS Inc., Chicago, IL, USA].
Results
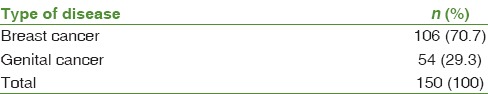
The mean (± standard deviation) regarding some of the demographic characteristics is given in Table 1. 54 patients (36%) had university studies, and 94 patients (62.7%) were housewives. Table 2 shows the distribution of cancer types.
Table 1.
Statistical indicators related to demographic variables in women with genital and breast cancers
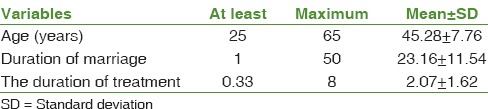
Table 2.
Frequency distribution of participants according to type of cancer
47.3% were under treatment of radiotherapy and chemotherapy, and 31.7% were under treatment of radiotherapy, chemotherapy, and surgery. Moreover, McNemar's test showed that the frequency of recent sexual disorders in all areas has been significantly higher than the primary disorder [Table 3].
Table 3.
Frequency distribution of sexual dysfunction in women with genital and breast cancers by type of disorders
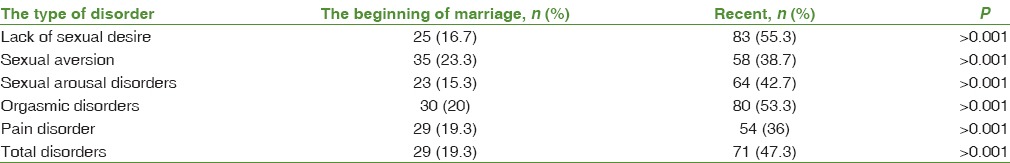
Figure 1 shows that the majority of participants have reported good quality of relationship with their spouses.
Figure 1.
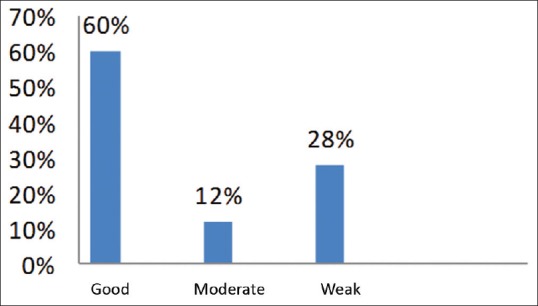
Frequency distribution of participants based on the quality of relationship with their spouses
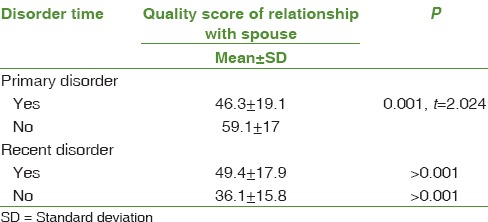
Independent t-tests showed that in women with primary sexual dysfunction mean score of quality of relationship with spouse has been less than women without sexual dysfunction [Table 4]. Furthermore, in women with recent sexual dysfunction, the score of quality of relationship with spouse has been significantly less than those who did not have disorders.
Table 4.
Mean score of quality of relationship with spouse according to lack or presence of primary and recent disorders
Discussion
Results of the present study showed that a there was a significant relationship between sexual dysfunction and quality of relationships with spouse. In this regard, the study by Speer et al. revealed that women with cancer, who had more intimacy and as a result had a better sex life with their husbands, reported less sexual dysfunction.[26] In addition, in another study, the results showed that women with breast cancers who had better physical and sexual relationship with their husbands reported less sexual problems, including sexual arousal and disgust.[27] In addition, regarding the chronicity of cancer, the results of Lemack and Zimmern's study also showed that women with vaginal cancers demonstrated a significant reduction in sexual activity following surgery.[28] Considering the impact of the disease and its complications in the course of treatment, patients usually face with depression, anxiety, and unhealthy feelings and due to failure to comply with major life issues, their sexual desire, and resultantly, the sexual satisfaction of their husbands reduce.[29] However, the results of some studies, including Mehrabi et al.'s study has shown that in marital relations, there was not a significant difference in terms of sexual activity between patients with myocardial infarction and healthy people.[30]
Counclusion
Finally, regarding the high rate of sexual dysfunction in genital and breast cancers in the present study, and it is relation to the quality of spousal relationships in these patients, it is necessary to pay more attention to performing reviews, preventing, and treating these disorders by caregivers and healthcare staff. Moreover, it is vital to provide consulting services to solve these problems.
Financial support and sponsorship
This study was supported by Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This article was derived from a master thesis with project number 289237 Isfahan University of Medical Sciences, Isfahan, Iran.
References
- 1.Laurent SM, Simons AD. Sexual dysfunction in depression and anxiety: Conceptualizing sexual dysfunction as part of an internalizing dimension. Clin Psychol Rev. 2009;29:573–85. doi: 10.1016/j.cpr.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Berek JS. Common psychiatric problems. Berek & Novak's Gynecology. 14th ed. USA: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 3.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 4.Matulonis UA, Kornblith A, Lee H, Bryan J, Gibson C, Wells C, et al. Long-term adjustment of early-stage ovarian cancer survivors. Int J Gynecol Cancer. 2008;18:1183–93. doi: 10.1111/j.1525-1438.2007.01167.x. [DOI] [PubMed] [Google Scholar]
- 5.Hopkinson JB, Fenlon DR, Okamoto I, Wright DN, Scott I, Addington-Hall JM, et al. The deliverability, acceptability, and perceived effect of the Macmillan approach to weight loss and eating difficulties: A phase II, cluster-randomized, exploratory trial of a psychosocial intervention for weight- and eating-related distress in people with advanced cancer. J Pain Symptom Manage. 2010;40:684–95. doi: 10.1016/j.jpainsymman.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Ismail KM. Psychological challenges in obstetrics and gynecology. Obstet Gynaecol. 2008;10:206. [Google Scholar]
- 7.Anderson JL. Acknowledging female sexual dysfunction in women with cancer. Clin J Oncol Nurs. 2013;17:233–5. doi: 10.1188/13.CJON.233-235. [DOI] [PubMed] [Google Scholar]
- 8.Rodin G, Olmsted MP, Rydall AC, Maharaj SI, Colton PA, Jones JM, et al. Eating disorders in young women with type 1 diabetes mellitus. J Psychosom Res. 2002;53:943–9. doi: 10.1016/s0022-3999(02)00305-7. [DOI] [PubMed] [Google Scholar]
- 9.Pinto AC. Sexuality and breast cancer: Prime time for young patients. J Thorac Dis. 2013;5(Suppl 1):S81–6. doi: 10.3978/j.issn.2072-1439.2013.05.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodin G, Olmsted MP, Rydall AC, Maharaj SI, Colton PA, Jones JM, et al. Eating disorders in young women with type 1 diabetes mellitus. J Psychosom Res. 2002;53:943–9. doi: 10.1016/s0022-3999(02)00305-7. [DOI] [PubMed] [Google Scholar]
- 11.Carter J, Huang H, Chase DM, Walker JL, Cella D, Wenzel L. Sexual function of patients with endometrial cancer enrolled in the Gynecologic Oncology Group LAP2 Study. Int J Gynecol Cancer. 2012;22:1624–33. doi: 10.1097/IGC.0b013e31827277fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brotto LA, Heiman JR, Goff B, Lentz GM, Swisher E. “A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer”. Archives of Sexual Behavior. 2008;37(2):317–29. doi: 10.1007/s10508-007-9196-x. [DOI] [PubMed] [Google Scholar]
- 13.Bergmark K, Avall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Patient-rating of distressful symptoms after treatment for early cervical cancer. Acta Obstet Gynecol Scand. 2002;81:443–50. doi: 10.1034/j.1600-0412.2002.810512.x. [DOI] [PubMed] [Google Scholar]
- 14.Gershenson DM, Miller AM, Champion VL, Monahan PO, Zhao Q, Cella D, et al. Reproductive and sexual function after platinum-based chemotherapy in long-term ovarian germ cell tumor survivors: A Gynecologic Oncology Group Study. J Clin Oncol. 2007;25:2792–7. doi: 10.1200/JCO.2006.08.4590. [DOI] [PubMed] [Google Scholar]
- 15.Hawkins Y, Ussher J, Gilbert E, Perz J, Sandoval M, Sundquist K. Changes in sexuality and intimacy after the diagnosis and treatment of cancer: The experience of partners in a sexual relationship with a person with cancer. Cancer Nurs. 2009;32:271–80. doi: 10.1097/NCC.0b013e31819b5a93. [DOI] [PubMed] [Google Scholar]
- 16.Anllo LM. Sexual life after breast cancer. J Sex Marital Ther. 2000;26:241–8. doi: 10.1080/00926230050084632. [DOI] [PubMed] [Google Scholar]
- 17.Bakewell RT, Volker DL. Sexual dysfunction related to the treatment of young women with breast cancer. Clin J Oncol Nurs. 2005;9:697–702. doi: 10.1188/05.CJON.697-702. [DOI] [PubMed] [Google Scholar]
- 18.Meradith D, Noonan AC, Sharby N, Ventura SH. Psychosocial Aspects of Heath Care. 2nd ed. Ventura: Pearson Prentice; 2007. [Google Scholar]
- 19.Tuinman MA, Fleer J, Sleijfer DT, Hoekstra HJ, Hoekstra-Weebers JE. Marital and sexual satisfaction in testicular cancer survivors and their spouses. Support Care Cancer. 2005;13:540–8. doi: 10.1007/s00520-004-0758-3. [DOI] [PubMed] [Google Scholar]
- 20.Hinnen C, Hagedoorn M, Ranchor AV, Sanderman R. Relationship satisfaction in women: A longitudinal case-control study about the role of breast cancer, personal assertiveness, and partners’ relationship-focused coping. Br J Health Psychol. 2008;13(Pt 4):737–54. doi: 10.1348/135910707X252431. [DOI] [PubMed] [Google Scholar]
- 21.Mazinani R, Akbari Mehr M, Kaskian A, Kashanian M. Evaluation of prevalence of sexual dysfunctions and its related factors in women. Razi J Med Sci. 2013;19:59–66. [Google Scholar]
- 22.Sarhadi M, Navidian A, Fasihi Harandy T, Ansari Moghadam AR. Comparing quality of marital relationship of spouses of patients with and without a history of myocardial infarction. J Health Promot Manage. 2012;2:39–48. [Google Scholar]
- 23.Beigi M, Fahami F, Hassanzahraei R, Arman S. Associative factors to sexual dysfunction in menopause women. Iran J Nurs Midwifery Res. 2007;13:32–5. [Google Scholar]
- 24.Jensen PT, Klee MC, Thranov I, Groenvold M. Validation of a questionnaire for self-assessment of sexual function and vaginal changes after gynaecological cancer. Psychooncology. 2004;13:577–92. doi: 10.1002/pon.757. [DOI] [PubMed] [Google Scholar]
- 25.Mohamadirizi S, Fahami F, Savabi M, Shirani N. Relationship between sexual dysfunction and treatment modality in patients With Gynecologic And Breast Cancers. Iranian Journal of Obstetrics, Gyneocology and Infertility. 2014;17:15–22. [Google Scholar]
- 26.Speer JJ, Hillenberg B, Sugrue DP, Blacker C, Kresge CL, Decker VB, et al. Study of sexual functioning determinants in breast cancer survivors. Breast J. 2005;11:440–7. doi: 10.1111/j.1075-122X.2005.00131.x. [DOI] [PubMed] [Google Scholar]
- 27.Alder J, Zanetti R, Wight E, Urech C, Fink N, Bitzer J. Sexual dysfunction after premenopausal stage I and II breast cancer: Do androgens play a role? J Sex Med. 2008;5:1898–906. doi: 10.1111/j.1743-6109.2008.00893.x. [DOI] [PubMed] [Google Scholar]
- 28.Lemack GE, Zimmern PE. Sexual function after vaginal surgery for stress incontinence: Results of a mailed questionnaire. Urology. 2000;56:223–7. doi: 10.1016/s0090-4295(00)00626-9. [DOI] [PubMed] [Google Scholar]
- 29.Sarhadi M, Navidian A, Fasihi Harandy T, Ansari Moghadam AR. Comparing quality of marital relationship of spouses of patients with and without a history of myocardial infarction. J Health Promot Manage. 2013;2:40–9. [Google Scholar]
- 30.Mehrabi T, Moeini M, Bakhtiyari S, Qaleriz P. Marital satisfaction in patients with and without myocardial infarction. Iran J Nurs Midwifery Res. 2008;1:6–9. [Google Scholar]


