Abstract
Objective
To examine the efficacy of an 8-week regimen combining repetitive task-specific practice with a myoelectric brace (RTP+Myomo) on paretic upper extremity (UE use in valued activities, perceived recovery, and reaching kinematics).
Subjects
Twelve subjects (4 males; mean age 53.5 years; mean time post stroke 61.7 months).
Interventions
Seven subjects were administered RTP+Myomo therapy, and 5 were administered RTP only. Both groups participated in individualized, 45-minute therapy sessions occurring 3 days/week over an 8-week period.
Main Outcome Measures
The arm, hand ability, activities of daily living, and perceptions of recovery subscales of the Stroke impact Scale (SIS), as well as UE reaching kinematics, assessed before and after the intervention.
Results
Subjects in the RTP+Myomo group showed greater improvements on all SIS subscales, with the recovery scale reaching statistical significance (p=0.03). Subjects in the RTP-only group showed a greater increase in hand velocity in the reach up task (p=0.02), but no changes were observed in the range of shoulder flexion or elbow extension during reaching. None of the changes in kinematic outcome measures significantly correlated with any of the changes in SIS subscales.
Conclusions
RTP integrating myoelectric bracing may be more beneficial than RTP only in improving self-reported function and perceptions of overall recovery. We observed no changes in the range of elbow extension, and no relationship between self-reported improvements and changes in reaching kinematics.
Keywords: Neuro-Rehabilitation, Stroke, Hemiplegia, Kinematics
Introduction
Stroke frequently causes debilitating upper extremity (UE) motor impairments that are retained well beyond rehabilitation discharge.1,2 In response, several UE motor rehabilitative approaches have been developed,3,4,5,6 with most adhering to the P.R.A.C.T.I.C.E. principles.7 Yet, many promising UE rehabilitative strategies3–6 are only efficacious in individuals already exhibiting high levels of active, paretic UE movement; only a small segment of the growing stroke survivor population.
Survivors with moderate to severe UE impairment are thought to constitute a larger proportion of the stroke population,8 and frequently exhibit limited active movement in their paretic elbow, and little to no active movement in their paretic wrists and fingers. Active elbow movement constitutes a critical component to carrying out valued UE activities (e.g., reaching for an item on a shelf located above one’s head; reaching for an item on a table surface in front of the individual to feed), and is often a target of UE rehabilitation in the growing, moderately impaired, stroke survivor population. Recently, reduced UE impairment and increased function were reported among survivors with moderate UE impairment participating in repetitive task-specific practice (RTP) that integrated a portable, electromyography (EMG) triggered, brace (“Myomo”).9,10,11 The use of an EMG triggered device in the absence of active elbow movement can be useful in enabling subjects to activate the Myomo and complete valued activities such as those mentioned above. This possibility was realized in the above preliminary studies, in which subjects exhibited new active elbow movement after completion of the Myomo intervention period, and new ability to carry out valued activities as a result of this participation. Such a regimen could address the unmet need for an efficacious, easily implemented UE therapy for stroke survivors with moderate UE impairment; hundreds of thousands of new patients annually.
As a next step, we wished to compare the efficacy of this regimen with the use of RTP only, which constitutes the standard of care in most outpatient environments.12,13 Concurrently, we also wished to characterize the motor behavior of stroke survivors exhibiting moderate UE impairment. Therefore, the purpose of this study was to compare the efficacy of an 8-week regimen combining RTP with Myomo use to the effect of RTP only on clients’ participation in common UE activities, perceptions of recovery, and UE kinematics. We also integrated UE kinematics as a secondary outcome measure, using a kinematic paradigm previously-validated by members of our team.14 To our knowledge, this was the first study examining the participatory or kinematic impact of portable myoelectrics. Despite its importance to carrying out functional activities, a focus on elbow extension was also felt to be unique.
Method
Subjects
Volunteers had been recruited using approved advertisements distributed to local stroke support groups and at outpatient rehabilitation clinics. They were screened using the following inclusion criteria:10 (a) UE Fugl-Meyer score ≥10-≤25 at time of screening; (b) volitionally activated paretic biceps brachii EMG amplitude ≥5ųV; (c) a single stroke, experienced >12 months ago; (d) a score ≥24 on the Folstein Mini Mental Status Examination; (e) age ≥35< 85; (f) discharged from physical rehabilitation. Exclusion criteria were: (a) ≥5 on a 10-point visual analog scale for pain in the paretic hand, arm or shoulder; (b) ≥2 on the Modified Ashworth Spasticity Scale in the paretic elbow; (c) participating in other experimental rehabilitation or drug studies; (d) ≤2.5 on the Alexander Apraxia scale; (e) history of neurological disorder other than stroke; (f) change in anti-spasticity medications in the last 6 months, and/or receipt of botulinum toxin in the paretic UE in the previous 4 months; (g) other conditions that may undermine safety or full participation of subjects.
Apparatus
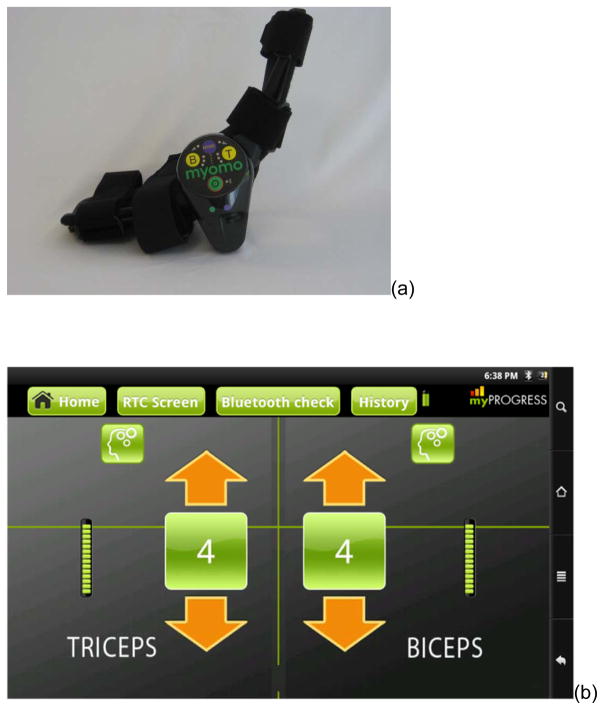
The Myomo e100 (Figure 1a) is a Food and Drug Administration–approved, lightweight (≈2lbs), myoelectric brace that uses surface EMG signals from the biceps and triceps brachii to assist the active muscle with movement of the paretic UE (see10 for more details). During active paretic UE movement attempts, the user’s intention to move is detected via his/her EMG. The treating therapist can then adjust the system parameters to alter the amount of mechanical assistance that the device provides on an as needed basis, using software on a tablet (Figure 1b).
Figure 1.
(a) Myoelectric brace used in the study and (b) screenshot of software that remotely controls the amount of support provided by the brace
Study Design and Assessments
Data reported here were collected as part of a larger randomized controlled trial determining the efficacy of Myomo use post-stroke. A subgroup of subjects from this larger study underwent a second randomization using a random numbers table. Those assigned to this subgroup were administered the SIS and UE kinematics above and beyond the behavioral and neuroimaging measures collected in the larger trial, with these data reported herein. All subjects had completed consent forms approved by the local ethics board.
Behavioral data
We administered the Stroke Impact Scale (SIS);15 a 64-item self-report measure assessing 8 domains (e.g., hand function, mobility, communication, memory). For this study, we focused on changes in the paretic UE (SIS arm and hand scales), ability to perform activities of daily living, and recovery scales.
Kinematic data
An 11-camera motion capture system (Motion Analysis Corporation Raptor-12 system, Santa Rosa, CA, USA) tracked 3D-motion of subjects’ paretic and less affected UEs during the experimental tasks. Twenty-six reflective markers were placed on the upper body (Figure 2), according to marker placements elucidated in our previous work with stroke survivors.13 Subjects were seated in a 45cm chair with no arm rests, and their hands flat (about shoulder width apart) on a 70cm table in front of them. Their chest was restrained by a Velcro strap to limit compensatory trunk movements,16,17 and their humerus was hanging down their body. Each subject performed 5 repetitions of two reaching tasks with the paretic and non-paretic UE. For the ‘reach-out’ task, a cylinder-shaped object (5cm diameter; 17cm height) was placed in front of the subject on the table, aligned with the subject’s sternum at 2/3 of paretic UE length (shoulder-to-elbow + elbow-to-wrist distances). For the ‘reach-up’ task, the same object was elevated by 24 cm. Subjects were instructed reach for the object as if they were reaching for a glass of water, without specific instructions on movement speed. If subjects were unable to grasp the object with their paretic UE, they were instructed to reach for the object and move it.
Figure 2.
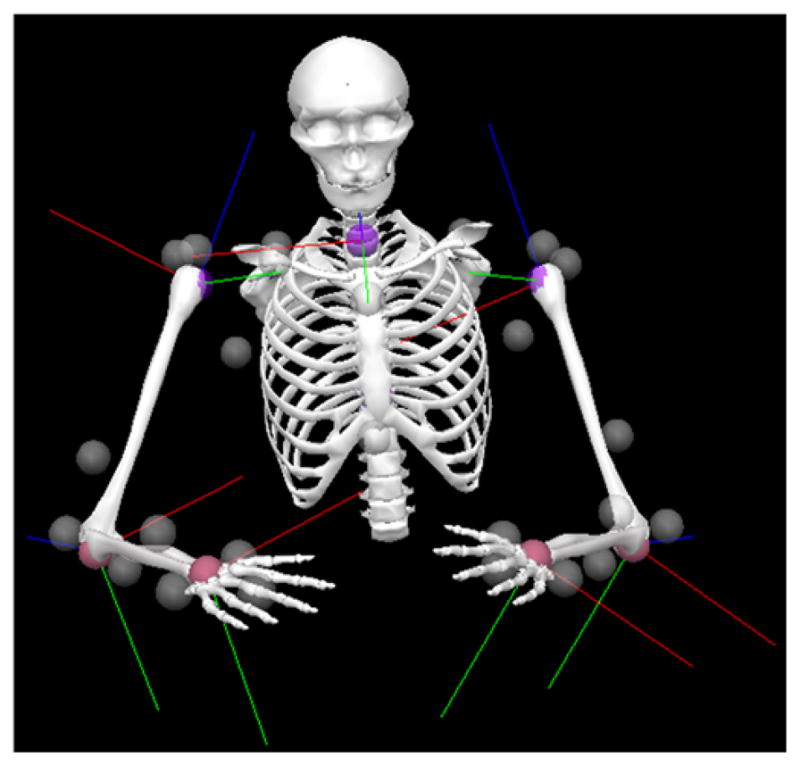
Kinematic Model of a Subject in the Starting Position
Intervention
Subjects were randomized into one of two treatment groups using a computer-generated random numbers table: (a) RTP; or (b) RTP+Myomo. Both groups participated in individualized, 45-minute therapy sessions occurring 3 days/week over an 8-week period. As described elsewhere,10 the intervention’s design and therapy session content involved subjects initially practicing 4–5 UE motor tasks, e.g. lifting a laundry basket, sit to stand transfers using the arms of a chair, and turning on-and-off a light switch located on a wall. As subjects’ movement in the paretic UE progressed, additional “whole-arm” tasks were added that emphasized gross movements and elbow use but also selectively involved the more distal regions (e.g., using a fishing rod; using a broom to sweep the floor). In all cases, the latter tasks were selected collaboratively with the patient, caregiver, and therapist. Using the recently-described P.R.A.C.T.I.C.E. principles as a guide to the nature and quality of practice,see 7 the common elements of the guided practice – with or without the Myomo - included repetition, choosing tasks that were functional/goal directed, integrating the paretic UE into whole-arm tasks that were salient to the subject, and use of part whole practice. Whereas many automated approaches18,19 and recent therapeutic approaches3–5 have primarily emphasized unilateral UE use, an inherent advantage of using a wearable, myoelectric brace was ability to easily integrate both UEs simultaneously so that practice conditions were more analogous to “real world” circumstances. Accordingly, therapy included both bilateral and unilateral UE tasks, and included components of muscle control, coordination, strength, endurance, and proprioception. All tasks could be graded and adapted according to the deficits exhibited by each subject (e.g., for speed, distance, space covered by the task, use of more distal and/or paretic UE regions), since challenge is a critical factor underlying learning, cortical plasticity, and subsequent UE functional change.e.g.20 Greater detail regarding grading of tasks involved in RTP programs is described elsewhere.e.g.10,21 In the RTP+Myomo group the lowest amount of assistance by the device to the paretic biceps and triceps (Figure 1b) was chosen.
Data Analyses
Based on our pilot experiences,14 and because the Myomo specifically assists elbow movement, the primary kinematic outcome of interest was the range of elbow extension in the paretic UE. In addition, we recorded shoulder (anterior) flexion and hand velocity data in both UE’s. As a rough measure of subject performance, we also counted the number of trials in which subjects were successful in moving the object.
Data collection and quality control was performed in Cortex (Motion Analysis Corporation, Santa Rosa, CA, USA). Data were then exported to Visual3D (C-Motion), and joint angles were calculated based on a standard upper extremity model and conventions for the shoulder joint.21 Kinematic time series were exported to Matlab 2013a for further analysis. Time series with artifacts due to marker drop-out were discarded from analyses (<5% of 1440 time series curves), and outcome measures were averaged over the remaining trials.
The range of shoulder flexion and elbow extension were quantified by the absolute difference between the maximum and minimum that occurred during the reaching task. To quantify the amount of change from pretest to posttest in the range of shoulder flexion, elbow extension and peak hand velocity in each patient, the pretest values were subtracted from the posttest values.
Given the small sample and unequal sizes of the two treatment conditions, a two-tailed Mann Whitney U test was used to compare all behavioral and kinematic changes between the two groups. Spearman’s correlation coefficients were calculated to explore any relationships between changes in self-reported and kinematic outcomes.
Results
Subject Demographics
From the overall pool of subjects enrolled in the larger trial (n = 34), 12 subjects were randomized and all agreed to participate in this additional testing (4 males; age=53.5±5.35 years; mean time post-stroke=61.7 months; 11 Caucasians, 1 African-American; 6 left-sided strokes; 10 ischemic strokes; 1 basal ganglia stroke; 3 strokes in the left-middle cerebral artery; 1 in the frontal lobe; 2 in the parietal lobe; 5 in unspecified locations): 7 subjects were administered RTP+Myomo, and 5 were administered RTP only.
Behavioral Outcomes
All of the subjects completed the protocol with no compliance issues noted (i.e. attendance at all therapy sessions occurred as prescribed). The duration of therapy per session (45 minutes/therapy session) was also consistent from subject to subject, and was documented in treatment notes. No adverse events or protocol deviations were noted.
Table 1 shows individual and group scores on the arm, hand, ADL and recovery SIS subscales. Subjects administered RTP+Myomo tended to exhibit larger improvements on all scales than subjects administered RTP only. This difference between groups reached significance for SIS recovery (U=4, p=0.032, point probability=0.015), and came close to statistical significance for SIS ADL (U=6, p=0.061, point probability=0.001).
Table 1.
Scores on the hand, arm, ADL, and overall recovery subscales of the Stroke Impact Scale (SIS) before (‘PRE’) and after (‘POST’) the intervention.
| ID | Intervention | PRE Arm | POST Arm | PRE Hand | POST Hand | PRE ADL | POST ADL | PRE Recovr | POST Recovr |
|---|---|---|---|---|---|---|---|---|---|
| 13 | RTP + Myomo | 80 | 97.5 | 25 | 30 | 56.25 | 65.625 | 50 | 60 |
| 14 | 82.5 | 95 | 0 | 30 | 40.625 | 50 | 75 | 80 | |
| 19 | 82.5 | 77.5 | 0 | 25 | 46.875 | 56.25 | 75 | 85 | |
| 21 | 67.5 | 80 | 5 | 30 | 53.125 | 65.625 | 40 | 70 | |
| 23 | 75 | 75 | 0 | 0 | 90.625 | 90.625 | 70 | 70 | |
| 25 | 90 | 95 | 0 | 30 | 87.5 | 87.5 | 60 | 70 | |
| 31 | 65 | 60 | 0 | 25 | 37.5 | 100 | 50 | 65 | |
| Group mean (SD) | 77.5 (8.90) | 82.9 (13.7) | 4.29 (9.32) | 24.3 (11.0) | 58.9 (21.6) | 73.7 (19.0) | 60.0 (13.8) | 71.4 (8.52) | |
| Group change (SD) | 5.6 (9.1) | 20.0 (12.2) | 14.7 (21.6) | 11.4 (9.4) | |||||
| 17 | RTP only | 75 | 65 | 30 | 0 | 59.375 | 84.375 | 40 | 45 |
| 18 | 95 | 77.5 | 30 | 10 | 68.75 | 46.875 | 40 | 40 | |
| 24 | 40 | 42.5 | 0 | 25 | 56.25 | 53.125 | 30 | 30 | |
| 27 | 75 | 87.5 | 0 | 10 | 81.25 | 56.25 | 55 | 50 | |
| 29 | 72.5 | 75 | 10 | 45 | 59.375 | 31.25 | 50 | 55 | |
| Group mean (SD) | 71.5 (19.8) | 69.5 (17.1) | 14.0 (15.2) | 18.0 (17.5) | 65.0 (10.2) | 54.4 (19.3) | 43.0 (9.75) | 44.0 (9.62) | |
| Group change (SD) | −2.0 (11.8) | 4.0 (28.2) | −10.6 (22.2) | 1.0 (4.2) | |||||
Kinematic Outcomes
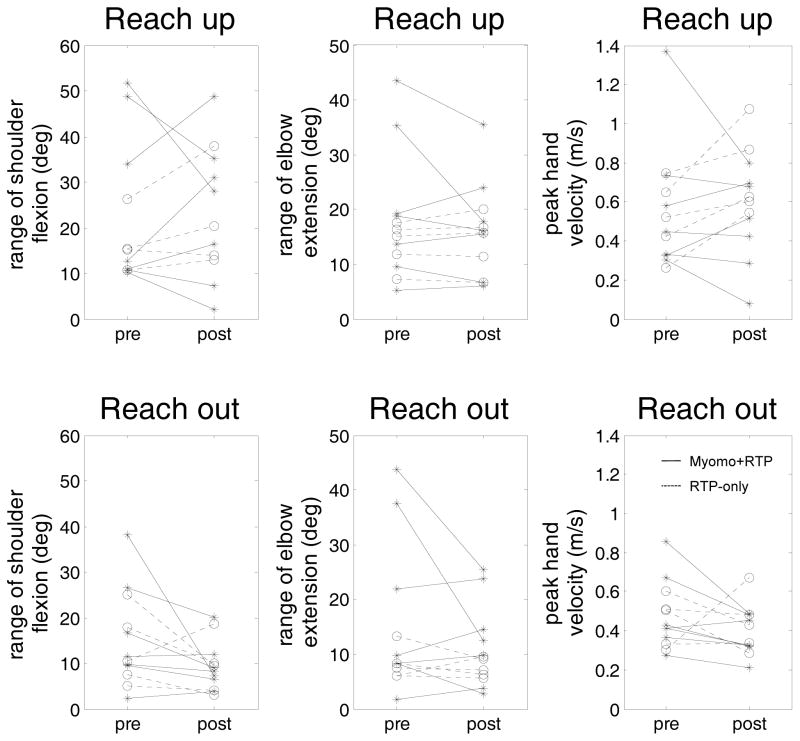
None of the subjects was able to actually grasp and lift the object with their paretic limb. Therefore, kinematic analyses focused only on the reaching part of the movement, which ended when the hand touched the object. When subjects were unable to touch the object, we analyzed the full attempt. Most patients demonstrated improved capability to move the object after completing the intervention (Table 2). Figure 3 and Table 3 show the individual changes in kinematic measures from pretest to posttest in the paretic limb. The change in hand velocity from pretest to posttest in the ‘reach-up’ task was significantly larger in the RTP only group compared to the Myomo+RTP group (U=3, p=0.018, point probability=0.04). None of the other changes in kinematic variables from pretest to posttest were significantly different between groups (all p>0.53).
Table 2.
Patients’ Ability to Touch the Object in the ‘Reach Out’ and ‘Reach Up’ Tasks, Before and After the Intervention.
| Subject | Intervention | # Trials with object contact | ||
|---|---|---|---|---|
| Reach out (pre → post) | Reach up (pre → post) | Overall improvement (summed over tasks) | ||
| 13 | Myomo + RTP | 5 → 5 | 5 → 5 | = |
| 14 | 5 → 5 | 5 → 5 | = | |
| 19 | 0 → 3 | 0 → 0 | +3 | |
| 21 | 5 → 4 | 0 → 5 | +4 | |
| 23 | 0 → 1 | 0 → 0 | +1 | |
| 25 | 3 → 5 | 0 → 0 | +2 | |
| 31 | 2 → 5 | 5 → 4 | +2 | |
| 17 | RTP only | 1 → 5 | 4 → 5 | +5 |
| 18 | 5 → 5 | 5 → 5 | = | |
| 24 | 0 → 4 | 0 → 0 | +4 | |
| 27 | 0 → 5 | 0 → 0 | +5 | |
| 29 | 0 → 2 | 0 → 0 | +2 | |
Figure 3.
Individual Changes in Paretic Limb Kinematics from Pretest to Posttest for the Reach Up (upper panel) and Reach Out Tasks (lower panel).
Table 3.
Individual and Group Changes in Reaching Kinematics Following the Intervention (Pretest Values Subtracted from Posttest Values)
| ID | Group | Reach out | Reach up | ||||
|---|---|---|---|---|---|---|---|
| Range shoulder flexion change | Range elbow extension change | Peak hand velocity change | Range shoulder flexion change | Range elbow extension change | Peak hand velocity change | ||
| 13 | RTP+Myomo | −6.5 | −25.0 | −0.19 | 14.8 | −17.4 | −0.06 |
| 14 | RTP+Myomo | −31.0 | −18.4 | 0.04 | −23.8 | −8.2 | 0.12 |
| 19 | RTP+Myomo | −1.6 | 1.7 | −0.09 | 5.3 | −2.6 | −0.02 |
| 21 | RTP+Myomo | 0.5 | 4.8 | −0.11 | 18.0 | 2.0 | 0.19 |
| 23 | RTP+Myomo | 1.5 | 2.0 | −0.06 | −8.2 | 0.7 | −0.22 |
| 25 | RTP+Myomo | −3.1 | −5.6 | −0.04 | −3.5 | −2.9 | −0.05 |
| 31 | RTP+Myomo | −7.7 | 1.4 | −0.37 | −13.7 | 4.7 | −0.57 |
| RTP+Myomo group mean change (SD) | −6.8 (11.2) | −5.6 (11.6) | −0.12 (0.13) | −1.6 (15.2) | −3.4 (7.4) | −0.09 (0.25) | |
| 17 | RTP-only | −4.2 | −2.1 | 0.00 | 5.0 | −0.5 | 0.43 |
| 18 | RTP-only | 8.0 | 3.5 | −0.03 | 11.6 | 0.7 | 0.08 |
| 24 | RTP-only | −1.2 | −0.5 | 0.37 | 2.3 | 0.6 | 0.28 |
| 27 | RTP-only | −7.9 | −0.4 | −0.22 | −1.2 | −0.3 | 0.20 |
| 29 | RTP-only | −15.4 | −4.2 | −0.17 | No data | 2.4 | 0.12 |
| RTP only group mean change (SD) | −4.1 (8.6) | −0.7 (2.8) | −0.01 (0.23) | 4.4 (5.4) | 0.6 (1.2) | 0.22 (0.14) | |
A trend towards a significant correlation was observed between the change in the SIS arm subscale and the change in range of elbow extension during the reach up task. However, Spearman’s correlation coefficient was negative (rho=−0.57, p=0.054), which indicates that subjects with larger elbow range of motion while reaching up, tended to report lower arm function SIS scores. None of the changes in other kinematic variables significantly correlated with any of the changes in SIS subscales (all p≥0.12).
Discussion
This study evaluated self-reported function and reaching kinematics following an 8-week myoelectric brace intervention in patients >1 year post-stroke. Subjects in the RTP+Myomo group demonstrated better improvements in self-reported function, specifically in perceived overall recovery. Subjects in the RTP-only group showed a larger increase in peak hand velocity during the ‘reach up’ task, but no intervention effects were observed in shoulder flexion or elbow extension. Most subjects exhibited increased ability to reach the object, but none of the changes in reaching kinematics correlated to changes in self-reported function.
While kinematics are useful for focusing on range of motion changes in a single joint (e.g., the paretic elbow in the current study), the UE moves as part of a larger kinematic chain involving joints in the paretic UE, the less affected UE, the upper torso and, for some activities, the lower torso and/or the head (for a review see ref22). These relationships – and the fact that elbow kinematics alone do not speak to changes in paretic limb strength, or changes in function, the ability to perform activities, self-efficacy, or spontaneous UE use – likely explain our findings. These interrelationships also underscore the importance of future researchers administering UE kinematic paradigms in concert with other measures of function, participation, and recovery, as was the case in this study.
Anecdotally, subjects reported new ability to perform valued activities involving the paretic elbow and hand, including turning off and on a light switch, getting in and out of their cars, and pushing a grocery cart while ambulating. Interestingly, subjects in the RTP+Myomo group also reported new grasp and release abilities in the paretic UE, enabling them to further participate in valued activities. Together, these changes compare favorably with pilot Myomo work in people with moderate UE impairment,9.10 which similarly suggested reduced paretic UE impairment and increased UE function following Myomo use. Such trends suggest that a therapeutic approach integrating myoelectric brace use may yield functional effects that are comparable and, in some domains, superior, to those derived from RTP only in the large and growing population of stroke survivors with moderate UE impairments.
Aside from new findings about the utility of myoelectric bracing in moderately impaired stroke, this study adds to a limited body of literature characterizing reaching kinematics in stroke survivors.e.g.23–26 Given that individuals with moderate UE impairment comprise a large portion of the stroke survivor population, and our sample size was relatively small (n = 12), it would be beneficial for future authors to repeat our kinematic methods in a larger sample–especially in parallel to behavioral measures. The relatively dense impairment levels exhibited by our subjects caused some heterogeneity in task execution, and varied necessity for chest restraint during kinematic testing (although it was used with all subjects). Future studies could explore whether other UE motor tasks or kinematic variables may be more sensitive in detecting changes in perceived recovery following rehabilitation interventions. Objective and reliable measures of UE function will help to optimize training programs and recovery in chronic stroke patients. In parallel, we also believe that some focus on duration and frequency of this intervention would be beneficial at this time in this line of research. Indeed, while this study adds to a growing body of literature supporting the use of myoelectrics in increasing UE function and participation, it is plausible that an intervention administered over a longer period and/or with greater session duration may confer greater functional benefits, and possibly render kinematic benefits. Moreover, the optimal duration of this intervention – or any intervention in the moderately impaired stroke survivor population – has heretofore not been investigated in depth. Likewise, the stability of treatment effect was also not investigated in this study and deserves consideration.
Conclusion
RTP integrating myoelectric bracing might be more beneficial than RTP only in improving subjects’ perceptions of their overall recovery. However, this approach does not convey superior benefits to RTP only in terms of UE kinematics, and no significant correlations were observed between changes in self-reported outcomes and reaching kinematics. When taken in combination with results of other studies, our findings suggest that clinicians may be able to reduce the debilitating impact of moderate UE impairment using RTP+Myomo, but future studies with larger samples are needed to support these preliminary findings.
Clinical Messages.
Repetitive task specific practice (RTP) using a myoelectric brace increases perceptions of overall recovery and ability to perform valued activities using the paretic hand significantly more than RTP only. Moreover, people using RTP + myoelectrics display increased paretic hand and arm recovery. These findings corroborates findings of previous studies suggesting that such an integrated regimen increases post stroke recovery in people with moderate upper extremity impairments.
People participating in myoelectric-assisted RTP also exhibit new ability to perform valued activities involving the paretic elbow and hand, despite being years post stroke.
Despite these behavioral changes, all subjects – regardless of grouping – displayed changes in ability to reach out for an object using kinematics, and no difference between the groups were seen on other kinematic variables that examined velocity or range of motion changes at the different arm joints. We suspect that this is because the UE moves as part of a larger kinematic chain involving joints in the paretic UE, the less affected UE, and the upper torso, such that analyses of isolated joints may not entirely reflect or coincide with functional changes as were detected herein.
Acknowledgments
This work was supported by a grant from the National Institutes of Health (1 R03 HD062545-02).
Abbreviations
- RTP
repetitive task-specific practice
- UE
upper extremity
- EMG
electromyography
- SIS
stroke impact scale
- ADL
activities of daily living
Contributor Information
N.W. Willigenburg, The Ohio State University, OSU Sports Medicine, Sports Health and Performance Institute, Columbus (OH), USA
Michael P McNally, The Ohio State University, Department of Orthopaedics, OSU Sports Medicine, Sports Health and Performance Institute, Columbus (OH), USA.
Timothy E Hewett, The Ohio State University, Departments of Physiology & Cell Biology, Family Medicine, Biomedical Engineering, and Orthopaedics, OSU Sports Medicine, Sports Health and Performance Institute, Columbus (OH), USA.
Stephen J. Page, B.R.A.I.N. (Better Rehabilitation and Assessment for Improved Neurorecovery) Laboratory, Division of Occupational Therapy, School of Health and Rehabilitation Sciences, The Ohio State University Medical Center, Columbus, OH, USA.
References
- 1.Gresham G, Fitzpatrick T, Wolf P, McNamara P, Kannel W, Dawber T. Residual disability in survivors of stroke--the Framingham study. N Engl J Med. 1975;293:954–956. doi: 10.1056/NEJM197511062931903. [DOI] [PubMed] [Google Scholar]
- 2.Kelly-Hayes M, Beiser A, Kase CS, Scaramucci A, D’Agostino RB, Wolf PA. The influence of gender and age on disability following ischemic stroke: The Framingham study. J Stroke Cerebrovasc Dis. 2003;12:119–126. doi: 10.1016/S1052-3057(03)00042-9. [DOI] [PubMed] [Google Scholar]
- 3.Wolf SL, Winstein CJ, Miller JP, Taub E, Uswatte G, Morris D, Giuliani C, Light KE, Nichols-Larsen D EXCITE Investigators. Effect of constraint-induced movement therapy on upper extremity function 3 to 9 months after stroke: the EXCITE randomized clinical trial. JAMA. 2006 Nov 1;296(17):2095–104. doi: 10.1001/jama.296.17.2095. [DOI] [PubMed] [Google Scholar]
- 4.Page SJ, Levine P, Leonard A. Mental practice in chronic stroke: Results of a randomized, placebo controlled trial. Stroke. 2007 Apr;38(4):1293–7. doi: 10.1161/01.STR.0000260205.67348.2b. [DOI] [PubMed] [Google Scholar]
- 5.Page SJ, Levine P, Leonard AC, Szaflarski J, Kissela B. Modified constraint-induced therapy in stroke: Results of a single blinded, randomized controlled trial. Phys Ther. 2008;88(3):333–40. doi: 10.2522/ptj.20060029. [DOI] [PubMed] [Google Scholar]
- 6.Kimberley TJ, Lewis SM, Auerbach EJ, Dorsey LL, Lojovich JM, Carey JR. Electrical stimulation driving functional improvements and cortical changes in subjects with stroke. Exp Brain Res. 2004 Feb;154(4):450–60. doi: 10.1007/s00221-003-1695-y. [DOI] [PubMed] [Google Scholar]
- 7.Page SJ, Peters H. Mental Practice: Applying Motor PRACTICE and Neuroplasticity Principles to Increase Upper Extremity Function. Stroke. doi: 10.1161/STROKEAHA.114.004313. in press. [DOI] [PubMed] [Google Scholar]
- 8.Heller A, Wade DT, Wood VA, Sunderland A, Hewer RL, Ward E. Arm function after stroke: measurement and recovery over the first three months. J Neurol Neurosurg Psychiatry. 1987;50:714–719. doi: 10.1136/jnnp.50.6.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stein J, Narendran K, McBean J, Krebs K, Hughes R. Electromyography controlled exoskeletal upper-limb–powered orthosis for exercise training after stroke. Am J Phys Med Rehabil. 2007;86:255–261. doi: 10.1097/PHM.0b013e3180383cc5. [DOI] [PubMed] [Google Scholar]
- 10.Page SJ, Hermann VH, Levine PG, Lewis E, Stein J, DePeel J. Portable neurorobotics for the severely affected arm in chronic stroke: a case study. J Neurol Phys Ther. 2011 Mar;35(1):41–6. doi: 10.1097/NPT.0b013e31820c4b00. [DOI] [PubMed] [Google Scholar]
- 11.Page SJ, Hill V, White S. Portable upper extremity robotics is as efficacious as upper extremity rehabilitative therapy: a randomized controlled pilot trial. Clin Rehabil. 2013 Jun;27(6):494–503. doi: 10.1177/0269215512464795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jette DU, Latham NK, Smout RJ, Gassaway J, Slavin MD, Horn SD. Physical therapy interventions for patients with stroke in inpatient rehabilitation facilities. Phys Ther. 2005 Mar;85(3):238–48. [PubMed] [Google Scholar]
- 13.Latham NK, Jette DU, Coster W, Richards L, Smout RJ, James RA, Gassaway J, Horn SD. Occupational therapy activities and intervention techniques for clients with stroke in six rehabilitation hospitals. Am J Occup Ther. 2006 Jul-Aug;60(4):369–78. doi: 10.5014/ajot.60.4.369. [DOI] [PubMed] [Google Scholar]
- 14.Hewett TE, Ford KR, Levine P, Page SJ. Reaching kinematics to measure motor changes after mental practice in stroke. Top Stroke Rehabil. 2007 Jul-Aug;14(4):23–9. doi: 10.1310/tsr1404-23. [DOI] [PubMed] [Google Scholar]
- 15.Duncan PW, Wallace D, Lai SM, Johnson D, Embretson S, Laster LJ. The stroke impact scale version 2.0. Evaluation of reliability, validity, and sensitivity to change. Stroke. 1999;30(10):2131–40. doi: 10.1161/01.str.30.10.2131. [DOI] [PubMed] [Google Scholar]
- 16.Subramanian SK, Yamanaka J, Chilingaryan G, Levin MF. Validity of Movement Pattern Kinematics as Measures of Arm Motor Impairment Poststroke. Stroke. 2010;41:2303–2308. doi: 10.1161/STROKEAHA.110.593368. [DOI] [PubMed] [Google Scholar]
- 17.Massie CL, Malcolm MP, Greene DP, Browning RC. Kinematic Motion Analysis and Muscle Activation Patterns of Continuous Reaching in Survivors of Stroke. J Motor Behav. 2012;44(3):213–222. doi: 10.1080/00222895.2012.681321. [DOI] [PubMed] [Google Scholar]
- 18.Volpe BT, Lynch D, Rykman-Berland A, Ferraro M, Galgano M, Hogan N, Krebs HI. Intensive sensorimotor arm training mediated by therapist or robot improves hemiparesis in patients with chronic stroke. Neurorehabil Neural Repair. 2008 May-Jun;22(3):305–10. doi: 10.1177/1545968307311102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lo A, Guarino PD, Richards LG, Haselkorn JK, Witterberg GI, Federman DG, Ringer RJ, Wagner TH, Krebs HJ, Volpe BT, Bever CT, Bravata DM, Duncan PW, Corn BH, Maffucci AD, Nadeau SE, Conroy SS, Powell JM, Huang GD. Robot-assisted therapy for long term upper limb impairment after stroke. N Eng Med J. 2010;362:1777–1783. doi: 10.1056/NEJMoa0911341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nudo RJ. Plasticity. NeuroRx. 2006 Oct;3(4):420–7. doi: 10.1016/j.nurx.2006.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Page SJ, Boe S, Levine P. What are the “ingredients” of modified constraint-induced therapy? An evidence-based review, recipe, and recommendations. Restor Neurol Neurosci. 2013;31(3):299–309. doi: 10.3233/RNN-120264. [DOI] [PubMed] [Google Scholar]
- 22.Kitago T, Liang J, Huang VS, Hayes S, Simon P, Tenteromano L, Lazar RM, Marshall RS, Mazzoni P, Lennihan L, Krakauer JW. Improvement after constraint-induced movement therapy: Recovery of normal motor control or task-specific compensation? Neurorehabil Neural Repair. 2013;27(2):99–109. doi: 10.1177/1545968312452631. [DOI] [PubMed] [Google Scholar]
- 23.Lum PS, Mulroy S, Amdur RL, Requejo P, Prilutsky BI, Dromerick AW. Gains in upper extremity function after stroke via recovery or compensation: Potential differential effects on amount of real-world limb use. Top Stroke Rehabil. 2009;16(4):237–253. doi: 10.1310/tsr1604-237. [DOI] [PubMed] [Google Scholar]
- 24.Merians AS, Poizner H, Boian R, Burdea G, Adamovich S. Sensorimotor training in a virtual reality environment: Does it improve functional recovery poststroke? Neurorehabil Neural Repair. 2006;20:252–267. doi: 10.1177/1545968306286914. [DOI] [PubMed] [Google Scholar]
- 25.van Kordelaar J, van Wegen EEH, Nijland RHM, Daffersthofer A, Kwakkel G. Understanding adaptive motor control of the paretic upper limb early poststroke: The EXPLICIT-stroke program. Neurorehabil Neural Repair. 2013;27(9):854–863. doi: 10.1177/1545968313496327. [DOI] [PubMed] [Google Scholar]
- 26.van Vliet P, Pelton TA, Hollands KL, Carey L, Wing AM. Neuroscience findings on coordination of reaching to grasp an object: Implications for research. Neurorehabil Neural Repair. 2013;27(7):622–635. doi: 10.1177/1545968313483578. [DOI] [PubMed] [Google Scholar]