Abstract
Colorectal cancer (CRC) is one of the most common cancers worldwide. Several policies of CRC screening are available in different countries. The idea of screening is to identify patients at risk by detection of precancerous and small cancers early enough before they become advanced. In Saudi Arabia (SA), there is no countrywide policy for CRC screening despite the increasing incidence of the disease. Screening for CRC is a multidisciplinary approach that requires education programs, substantial financial support, several logistic measures, and predetermined resources before implementing such a program. We performed a prospective and systematic analysis of the of the screening policy of CRC in SA in view of high demand, anticipated development, and implementation of such a policy in the near future. We also attempted to investigate the justification for developing such a policy, as well as the difficulties, barriers, and opportunities that may be faced in its implementation. Further, we highlighted the current view of similar international screening policies. In this analysis, we adopted the framework for health policy analysis that examines four areas which may affect policy development, namely; content, context, process and actors.
Keywords: Colonoscopy, colorectal cancer, policy analysis, screening, Saudi Arabia
INTRODUCTION
Colorectal cancer (CRC) is a malignant tumor of the colon and rectum (large intestine). It is the third most common cancer worldwide and the second cause of cancer-related deaths in the United States and most of the western countries.[1,2] Internationally, CRC incidence has a wide geographical distribution being higher in North America, Australia, Northern and Western Europe. Developing countries claim to have lower rates, especially Africa and Asia.[3] It is rare before the age of 40, with higher incidence between the ages of 40 and 50 years; the age-specific incidence rates increase with each following decade.[4] Worldwide, CRC represents 9.4% of all incidental cancers in men and 10.1% in women.[5] Data concerning CRC from the Middle-eastern region are infrequent. At present, there are several policies of screening of population at risk of CRC in USA, Canada, most of the European Union countries, Japan, as well as other countries in the world. The concept of screening is to identify patients at risk by detection of precancerous and small cancers early enough before they become advanced and are not suitable for treatment. In Saudi Arabia (SA), recently, clinical practice guidelines for CRC has been published,[6] which is undoubtedly an excellent step in controlling CRC. However, there is no national policy for CRC screening despite increasing disease incidence. It is important to clarify that guidelines purely function as a guide or optional suggestions for the best clinical practice. Guidelines are meant to be followed by the medical professional, however, it cannot be considered a violation if they are not. Although guidelines are not mandatory, they are a very important part of the entire process. On the other hand, policies are high-level strict statements produced by senior management and supported by a higher degree of consensus than guidelines. Policies are compulsory compared to guidelines, and hence, any failure to adhere is considered a violation. We report herein a health policy analysis of screening for CRC in SA in view of the high demand, anticipated development, and implementation of such a policy in the near future. The policy has to be administered, endorsed, and monitored by the Ministry of Health.
THE GLOBAL IMPORTANCE OF THIS PUBLIC HEALTH ISSUE
According to the American Cancer Society, CRC is one of the leading causes of cancer-related deaths in the United States. However, early diagnosis often leads to a complete cure. The American Cancer Society's estimates for the number of CRC cases in the United States for 2016 were 95270 new cases of colon cancer and 39220 new cases of rectal cancer.[7]
In Canada, CRC in males is the second most common cancer accounting for approximately 14% of all new male cancer cases. In females, colorectal cancer is the third most common cancer representing approximately 12% of all new female cases. In 2015, the total new CRC cases were 25100 (14000 males and 11100 females).[8]
In Europe, for men, the highest incidence of CRC incidence is found in Ireland, Austria and Denmark, with 58–61 cases per 100,000 and the lowest in Greece with 25 cases per 100,000. For women, the highest incidence is found in Denmark, the Netherlands and Ireland, with 40–43 cases per 100,000 and the lowest in Greece with 19 cases per 100,000.[9]
In SA, as per the report from the Saudi National Cancer Registry in 2004, CRC was the first and third most common cancer among Saudi male and female populations, respectively, accounting for 9.3% of all newly diagnosed cases with overall, female, and male, age-standardized rate (ASR) of 7.3, 6.3, and 8.3 per 100,000 population, respectively.[10] However, in the latest report from SA, CRC has continued at the same rank in males and females, as previously reported, but with an increased incidence. In 2010, there were 1033 cases of CRC accounting for 10.4% of all newly diagnosed cases with a male-to-female ratio of 110:100. The overall ASR increased to 9.6/100,000 (ASR was 9.9/100,000 for males and 9.2/100,000 for females).[11]
Reports from USA have shown that the rate of CRC has declined, and it has been suggested that this is possibly due to disease prevention through screening procedures and removal of precancerous polyps, indicating the significant impact of screening on early detection of CRC.[12,13,14,15] This impact has been clarified further in more recent studies. Systematic reviews and meta-analyses of randomized controlled trials and observational studies have shown reliable evidence that screening sigmoidoscopy and colonoscopy prevent the majority of deaths from distal CRC. Furthermore, it has been reported that mortality from cancer of the proximal colon has decreased in populations who underwent CRC screening with colonoscopy compared with flexible sigmoidoscopy.[16] A more recent study advocates that more than 50% of the decrease in CRC mortality in US population could be attributed to the increase in CRC screening.[17]
Several regional studies have confirmed that Saudi patients present with CRC at a more advanced stage of the disease and at younger ages (less than 50 years) compared to Western populations. Mansoor et al.[18] reported that 39% of their patients were below 50 years of age. Aljebreen et al.[19] found that 37% of the patients were 50 years of age or younger. Al-Ahwal et al. reported that 29.7% of CRC patients were below the age of 40 years.[20] The national survival data from the Saudi Cancer Registry (SCR) between 1994 and 2004 showed that the five-year overall survival (OS) was 44.6%. Further, the five-year OS based on CRC stage was lower than the internationally reported survival rates.[21]
The knowledge and awareness of CRC screening among Saudi population have been studied in different regions. Khayyat et al.[22] found a deficiency of knowledge of CRC screening that was influenced by an individual's level of education and not by age or gender. Individuals who were aware of CRC screening have mainly chosen the endoscopic modality as a screening tool. In a public survey by Almadi et al.,[23] approximately 70.7% were willing to undergo a screening test for CRC, which increased to 83% in individuals who had a family history of CRC. Colonoscopy was accepted as a screening test in 69%. However, only 6.7% of those between 50 and 55 years of age had undergone CRC screening, which was far below the rate of screened individuals worldwide. In a third study by Zubaidi et al.,[24] 43% of the surveyed individuals agreed that colon cancer screening should start at the beginning of symptoms. Polyps as a risk factor for CRC was known to less than 20% of all respondents. Family history of CRC as a potential risk for CRC was known only to 34.8% of the surveyed individuals. Above mentioned recent studies indicate that the public awareness and understanding of the concept of screening for CRC is below the internationally reported figures. This highlights the need for a national education campaign along with a screening program.
Another equally important issue was the knowledge and awareness of family physicians regarding CRC screening. Demyati et al.[25] surveyed 130 family physicians and found that 56.2% of them were not practicing CRC screening despite their positive attitude; moreover, 94.6% of them considered CRC screening as effective. Elsamany et al.,[26] in a study of the clinicopathological patterns of CRC, found that advanced stage and a high incidence of adverse prognostic factors were more common presentations in young CRC patients. Young CRC patients seem to have worse survival compared to older Saudi patients. Similar results were reported by Sibiani et al.[27] and Amin et al.[28] In the study by Amin et al., out of 142 cases with CRC, 15.5% and 33.1% were found to be affected before 40 and 50 years of age, respectively. Lesions were detected in 16.9% in the right colon and 62.7% in the left colon. Intestinal obstruction was a common clinical presentation (41.5%), and 26.1% presented with symptoms indicating distant metastatic lesions. Adenocarcinoma was the major pathological finding (86.6%); metastatic CRC was diagnosed in 62.7%.[28] In a retrospective study by Almadi et al.[29] to identify the baseline polyp and adenoma (the precursors of adenocarcinoma) prevalence, a previous history of polyps that were removed was found in 4.8% of patients who had undergone screening. The detection rate of polyps and adenoma in those who underwent screening colonoscopy was 22.9% and 8.8%, respectively. The prevalence of polyps and adenoma in this study was 20.8% and 8.1%, respectively, which was less than that reported in the Western populations.
In a retrospective analysis of all cases of CRC from the SCR between January 2001 and December 2006, the incidence of CRC in SA was found to be on a constant rise, and the age at the time of diagnosis was lower when compared with results from developed countries.[30] All of the above data supports the need for a general population-based screening program in SA for a common yet preventable cancer. A screening program for CRC should preferably target individuals aged 40 years and above.
We propose that the development and implementation of a policy for screening of CRC in SA would be a very cost-effective project that will eventually decrease the burden on government expenditure and improve the populations' health status. Implementation of such a policy will result in the following: early detection of small tumors and commencing early treatment, preventing progression of CRC and saving the patient's life, saving money on very costly major surgeries, cutting the budget on buying very expensive chemotherapy and finally by increasing available beds in hospitals and better utilization of these beds for more important needs.
WHY NO POLICY EXISTS SO FAR IN SAUDI ARABIA AND HOW TO DEVELOP SUCH A POLICY
The health system in SA has been concentrating for a long time on the treatment aspects more than on the prevention of diseases. Furthermore, even when prevention policies were considered, they were directed towards communicable diseases and their prevention. This may be due to the prioritization policy in the health care system development in SA. Although there is a cancer registry that was established several years ago, cancer prevention and early detection was not a primary goal in the health plan or health care policies. This has led to a substantial delay in developing such a policy. Another important reason was the lack, in previous literature, of data on adenoma prevalence in Saudi population and whether this rate merited a nationwide screening program. However, recently, this issue has been clarified, with support for the need of such a program. Earlier diagnosis reduces the subsequent risk and cost. The chance of cure of all kinds of cancer is directly related to its stage at the time of diagnosis. However, cancer is generally diagnosed at a relatively advanced stage. World Health Organization (WHO) has stated that 40% of cancers could be avoided by prevention and 40% could be cured if detected early, and the rest should be managed with palliation.[31]
Development of a national colorectal cancer control policy
In May 2005, the World Health Assembly resolved that all countries should develop and implement national cancer control programs.[32] The policy is required to be made in writing, such that it can be reviewed and contributions can be sought by all stakeholders. It is normally essential for the document to be endorsed and supported by the Ministry of Health so that the necessary political commitment with respect to resource allocation required for it is implementation, chose either or at least for the implementation of high priority actions, is assured. Health authorities should apply careful strategies to face the expected increase in the incidence of CRC that will be anticipated by early detection. They should recruit highly trained health care professionals, especially primary care and family practitioners, gastroenterologists endoscopy nurses, and technicians, as well as build up more endoscopy units. The stakeholders in this plan will include patients and their families, primary care and family physicians, gastroenterologists (who perform colonoscopy), oncologists, colorectal surgeons, Saudi gastroenterology association, Saudi society of colon and rectal surgery, Saudi oncology society, hospital managers, district and regional health managers, the Ministry of health officials and the Ministry of finance. As expected, they are different in terms of general influence on policy-making as well as on its implementation.
There are powerful partners such as the Minister of Health, the health district managers, and Ministry of Finance. The intermediate power will include the gastroenterologists, colorectal surgeons, hospital managers, scientific associations and finally, weak stakeholders such as the primary care and family physicians, patients and their families. It is expected that the Ministry of Finance will oppose the plan for policy as it implicates further expenditure. Physicians and surgeons dealing with such a medical problem, the patients and their families will certainly support the plan for such a policy.
Patient advocate groups and scientific organization will certainly support the plan for policy, but unfortunately, their political influence is not considerable. We should look/search for those who are interested in pursuing this policy, and then we should involve them ahead of time. We can also seek to convince them by lobbying for change. Using a systems approach will help to identify other factors, in health services and in the global environment, that may affect the policy of screening for CRC in SA.
Principles of policy development
WHO has recommended the following principles as a guide for effective programs that provides practical advice for program managers and policy-makers on how to advocate, plan, and implement effective cancer control programs:[33]
Leadership to create clarity and unity of purpose, and to encourage team building, broad participation, ownership of the process, continuous learning, and mutual recognition of efforts made
Involvement of stakeholders of all related sectors, and at all levels of the decision-making process, to enable active participation and commitment of key players for the benefit of the program
Creation of partnerships to enhance effectiveness through mutually beneficial relationships, and build upon trust and complementary capacities of partners from different disciplines and sectors
Responding to the needs of people at risk of developing cancer or already presenting with the disease to meet their physical, psychosocial, and spiritual needs across the full continuum of care
Decision-making based on evidence, social values, and efficient and cost-effective use of resources that benefit the target population in a sustainable and equitable manner
Application of a systemic approach by implementing a comprehensive program with interrelated key components sharing the same goals and integrated with other related programs and to the health system
Seeking continuous improvement, innovation, and creativity to maximize performance and to address social and cultural diversity, as well as the needs and challenges presented by a changing environment
Adoption of a stepwise approach to planning and implementing interventions, based on local considerations and needs.
ANALYSIS OF THE POLICY
Although the policy does not exist currently, there is enough information and indications that can allow for anticipation of the effect of its development and subsequent implementation in the near future. To have a complete idea on the decision to develop policy interventions, we will apply the model introduced by Walt et al.[34] for health policy analysis that examines four areas which may affect policy development.
Content
The policy is about the screening of patients at risk for development of CRC in SA. It is a health care issue that will detect CRC at a very early stage when treatment is very simple and aiming for cure.
Context
This policy shall be made at a national (country-wide) level. It should be applicable all over SA. The current situation in the country is an ideal environment to develop this policy, as appears by stability in politics, availability of budgets, and the fact that SA is looking at further development in the health field and improvement of health services.
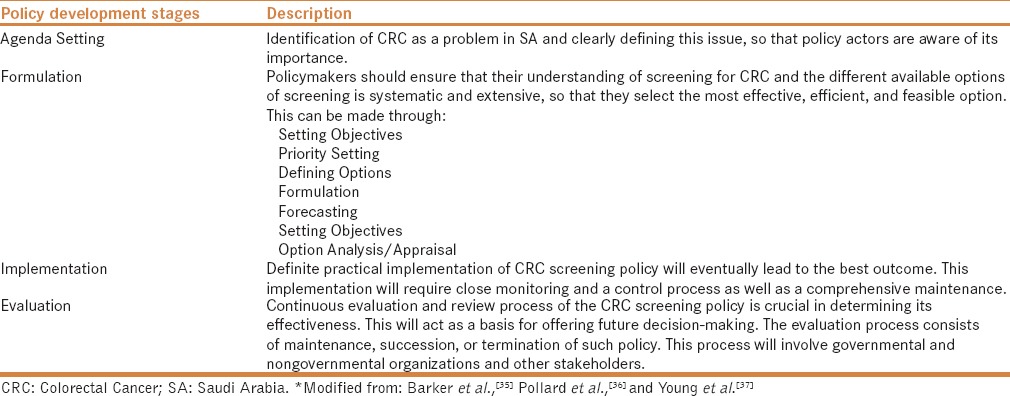
Process
The different stages of policy development of CRC in SA will be made according to previous reports,[35,36,37] as summarized in Table 1.
Table 1.
The policy of development process for CRC screening in SA*
Actors
Individuals and groups involved in developing the policy. Actors may influence the policy process at the local, regional, national, or international level. Actors who make policy may include
Individual with influence: Districts and regional governors, politicians, religious leaders, and media
Local scientific associations: Saudi Gastroenterology Association, Saudi Oncology Society, Saudi Society of Colon and Rectal Surgery
International organizations: WHO, American Gastroenterology Association, the American Cancer Society, the European Society for Medical Oncology, the Association of European Cancer Leagues, the United European Gastroenterology
State or government institutions: Regional Health Directory, The Saudi Commission for Health Specialties (SCHS) is a scientific body founded by virtue of the Royal Decree in 1992 that provides licensing and privilege for all health care providers
Non-state actors: Civil society organizations and charities, Saudi Cancer Society.
There should be solid, continuous and dynamic cooperation among these four main aspects. The relationship between these four areas was structured according to Walt et al.[34]
JUSTIFICATION OF DEVELOPING SUCH POLICY, DIFFICULTIES, AND PITFALLS THAT MAY FACE THIS POLICY IMPLEMENTATION
The current international status
In Canada, the Ontario Expert Panel on Colorectal Cancer recommends a multiphase screening program, beginning with fecal occult blood testing (FOBT), for people at normal risk between the ages of 50 and 75 years.[38] A recent recommendation by the Canadian Association of Gastroenterology has suggested that Colon cancer screening in Canada should be delivered through a regional or provincial program with high-sensitivity guaiac-based FOBT (g-FOBT) or fecal immunochemical testing (FIT) be used in colon cancer screening programs along with flexible sigmoidoscopy.[39] In 2016, the Canadian Task Force on Preventive Health Care recently have recommended that adults aged 50 to 59 years with a strong recommendation for individuals aged 60 to 74 years to be screened for CRC with g-FOBT or FIT every 2 years or flexible sigmoidoscopy every 10 years.[40]
In USA, reports from the Centers for Disease Control and Prevention (CDC) on the results from the Behavioral Risk Factor Surveillance System (BRFSS) in 1999 indicated that only 44% of Americans who were entitled for CRC screening have undergone screening with either FOBT within the year preceding the survey or sigmoidoscopy within the preceding 5 years.[41] In 2001, 53.1% of the population underwent screening with either FOBT in the past 1 year or a sigmoidoscopy or colonoscopy in the last 10 years.[42] In 2010, the rate of screening increased to 64.5% of the individuals having had one of the following colorectal screening tests, FOBT within 1 year, sigmoidoscopy within 5 years with FOBT within 3 years, or colonoscopy within 10 years preceding the survey.[43] Numerous reasons have been proposed for this low rate of test acceptance, including patients' resistance of endoscopic tests and noncompliance with physicians' recommendations. However, it is possible that failure of physicians to implement screening guidelines may be an important factor. Zack et al. in a charts review study found that only 16% of all eligible patients had undergone endoscopic CRC screening or FOBT compared with 66% of eligible female patients who had undertaken mammography screening.[44] The American Cancer Society, the U.S. Multi-Society Task Force on CRC, and the American College of Radiology jointly recommended screening for CRC beginning at 50 years of age by high-sensitivity FOBT or fecal immunochemical testing yearly, flexible sigmoidoscopy every 5 years, double-contrast barium enema every 5 years, CT colonography (CTC) every 5 years, colonoscopy every 10 years, or fecal DNA at an unspecified interval. The report indicated that endoscopic method was the best option.[45] The American College of Physicians recommended that screening for CRC in average-risk adults aged 50 to 75 years should be by 1 of 4 strategies: (1) annual high-sensitivity g-FOBT or FIT, (2) flexible sigmoidoscopy every 5 years, (3) high-sensitivity g-FOBT or FIT every 3 years plus flexible sigmoidoscopy every 5 years, or (4) colonoscopy every 10 years.[46] In 2008, the U.S. Preventive Services Task Force (USPSTF) recommended screening with colonoscopy every 10 years, annual FIT, annual high-sensitivity FOBT, or flexible sigmoidoscopy every 5 years combined with high-sensitivity FOBT every 3 years. However, more recently, they recommended not to emphasize specific screening methods, but to highlight that there is convincing evidence that colorectal cancer screening substantially reduces deaths from the disease among adults aged 50 to 75 years. USPSTF concludes that additional research is still needed before approving recommendation of colonoscopy, flexible sigmoidoscopy, CTC, and stool tests in CRC screening.[47,48]
In Europe, although it varies from one country to the other, the recommendations state that screening with FIT for hemoglobin and g-FOBT should be seriously considered as a preventive measure. If screening programs are applied, they should utilize the FOBT test and sigmoidoscopy. In some countries, colonoscopy is used for the follow-up of cases with positive tests. Screening should be performed for males and females aged 50 to 74 years. The screening intervals should be 1–2 years.[9,49,50] The European Union's Advisory Committee on Cancer Prevention advocate that average-risk individuals be screened only with FOBT every 1–2 years, along with performing endoscopic screening for only those who had positive FOBT results.[51]
In Asia, The Asia Pacific Working group on Colorectal Cancer consensus recommendations for CRC screening state that screening for CRC should be commenced at the age of 50 years. FOBT, guaiac-based, immunochemical testing, sigmoidoscopy and colonoscopy have been advocated for CRC screening. Double-contrast barium enema and CT colonography were not desirable choices. FOBT was the suggested preference for CRC screening in resource-limited countries. In a recent update of the Asia Pacific consensus recommendations, the age range for CRC screening was outlined as 50–75 years. Quantitative FIT, and not g-FOBT, is preferred in average-risk individuals. A risk-stratified scoring system was advocated to select high-risk patients for early colonoscopy.[52,53]
IDENTIFYING BARRIERS AND OPPORTUNITIES
For each policy, there will be supporters and opponents. It is important to know ahead of time the possible barriers as well as the opportunities that will facilitate the development and implementation of such a policy.
Expected barriers
Lack of political interest and leadership for developing the policy. The strong supporters have weak political power
Excessive reliance on treatment approaches, disregarding prevention and early detection
Inequity, inequalities, and the competing health problems in SA
Limited understanding about advocacy, need for advocacy, and lack of advocacy skills between supporters.
Expected opportunities
The recent commitments by WHO member states to develop an Action Plan for the Global Strategy for the Prevention and Control of Non-communicable Diseases and to promote and reinforce the comprehensive approach for cancer control (World Health Assembly resolution)[32,54]
The existence of clinical practice guidelines for CRC.
The availability of countries that have developed cancer control programs
The high willingness of international and national leaders and organizations in advocating comprehensive policies
The availability of a conceptual framework and guidelines for developing a comprehensive cancer control policy from governmental and nongovernmental perspectives[55,56,57]
The easy access to cancer control research and guidelines, which provides a good basis for advocacy.
Question and critique related to this policy
The biggest challenges for the future are: Would this policy be properly implemented, monitored and maintained in all SA health districts? Another important issue is how to evaluate these tests to determine the most efficacious, practical, and cost-effective method for population-based CRC screening.
CONCLUSION
CRC screening reduces morbidity and mortality from evolution and advancement of cancer. It is obvious that screening for CRC is not only life saving but decreases morbidity along with being a cost-effective measure. It is significantly cost-effective to perform colonoscopy and remove a precancerous lesion during screening than to attempt treating advanced CRC with major surgery and expensive chemotherapy. This review has clearly shown that there is an increasing demand for developing and implementing a screening policy for CRC in SA to face the increasing rate of this fatal disease, especially in a young age group. Screening program for CRC is a multidisciplinary approach that requires an education program, substantial financial support, and several logistic sharing in a time of predetermined resources; consequently, before implementing such a program, all issues connected with its success should be adjusted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
There is no financial or funding support from any source for this manuscript.
REFERENCES
- 1.Howe HL, Wu X, Ries LA, Cokkinides V, Ahmed F, Jemal A, et al. Annual report to the nation on the status of cancer, 1975-2003, featuring cancer among U.S. Hispanic/Latino populations. Cancer. 2006;107:1711–42. doi: 10.1002/cncr.22193. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006;56:106–30. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 3.Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin. 1999;49:33–64. doi: 10.3322/canjclin.49.1.33. [DOI] [PubMed] [Google Scholar]
- 4.Eddy DM. Screening for colorectal cancer. Ann Intern Med. 1990;113:373–84. doi: 10.7326/0003-4819-113-5-373. [DOI] [PubMed] [Google Scholar]
- 5.Boyle P, Langman JS. ABC of colorectal cancer: Epidemiology. BMJ. 2000;321:805–8. doi: 10.1136/bmj.321.7264.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alsanea N, Almadi MA, Abduljabbar AS, Alhomoud S, Alshaban TA, Alsuhaibani A, et al. National Guidelines for Colorectal Cancer Screening in Saudi Arabia with strength of recommendations and quality of evidence. Ann Saudi Med. 2015;35:189–95. doi: 10.5144/0256-4947.2015.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Key statistics for colorectal cancer. American Cancer Society Web site. [Last accessed on 2016 Jul 08]. Available from: http://www.cancer.org/cancer/colonandrectumcancer/detailedguide/colorectal-cancer-key-statistics .
- 8.Canadian Cancer Society's Advisory Committee on Cancer Statistics. Canadian Cancer Statistics 2015. Toronto, ON: Canadian Cancer Society 2015; [Last accessed on 2016 Jul 25]. Available from: https://www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%20101/Canadian%20cancer%20statistics/Canadian-Cancer-Statistics-2015-EN.pdf . [Google Scholar]
- 9.Recommendations on cancer screening in the European Union. Advisory Committee on Cancer Prevention. Eur J Cancer. 2000;36:1473–8. doi: 10.1016/s0959-8049(00)00122-2. [DOI] [PubMed] [Google Scholar]
- 10.National Cancer Registry. Cancer Incidence Report, Saudi Arabia. Ministry of Health: Riyadh, 2004; 38-39. [Last accessed on 2016 May 12]. Available from: http://www.chs.gov.sa/Ar/HealthRecords/CancerRegistry/CancerRegistryReports/Incidence%20Report%202004.pdf .
- 11.National Cancer Registry. Cancer Incidence Report, Saudi Arabia 2010. Ministry of Health: Riyadh, 2014; 38-39. [Last accessed on 2016 Jul 05]. Available from: http://www.chs.gov.sa/Ar/mediacenter/NewsLetter/2010%20Report%20(1).pdf .
- 12.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: Results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–40. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 13.Robertson RH, Burkhardt JH, Powell MP, Eloubeidi MA, Pisu M, Weissman NW. Trends in colon cancer screening procedures in the US Medicare and Tricare populations: 1999-2001. Prev Med. 2006;42:460–2. doi: 10.1016/j.ypmed.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 14.Vogelaar I, van Ballegooijen M, Schrag D, Boer R, Winawer SJ, Habbema JD, et al. How much can current interventions reduce colorectal cancer mortality in the US. Mortality projections for scenarios of risk-factor modification, screening, and treatment? Cancer. 2006;107:1624–33. doi: 10.1002/cncr.22115. [DOI] [PubMed] [Google Scholar]
- 15.Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood: Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328:1365–71. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- 16.Brenner H, Stock C, Hoffmeister M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: Systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ. 2014;348:g2467. doi: 10.1136/bmj.g2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zauber AG. The impact of screening on colorectal cancer mortality and incidence: Has it really made a difference? Dig Dis Sci. 2015;60:681–91. doi: 10.1007/s10620-015-3600-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mansoor I, Zahrani IH, Abdul Aziz S. Colorectal cancers in Saudi Arabia. Saudi Med J. 2002;23:322–7. [PubMed] [Google Scholar]
- 19.Aljebreen AM. Clinico-pathological patterns of colorectal cancer in Saudi Arabia: Younger with an advanced stage presentation. Saudi J Gastroenterol. 2007;13:84–7. doi: 10.4103/1319-3767.32183. [DOI] [PubMed] [Google Scholar]
- 20.Al-Ahwal MS, Al-Ghamdi AA. Pattern of colorectal cancer at two hospitals in the western region of Saudi Arabia. Saudi J Gastroenterol. 2005;11:164–9. doi: 10.4103/1319-3767.33320. [DOI] [PubMed] [Google Scholar]
- 21.Al-Ahwal MS, Shafik YH, Al-Ahwal HM. First national survival data for colorectal cancer among Saudis between 1994 and 2004: What's next? BMC Public Health. 2013;13:73. doi: 10.1186/1471-2458-13-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khayyat YM, Ibrahim EM. Public awareness of colon cancer screening among the general population: A study from the Western Region of Saudi Arabia. Qatar Med J. 2014;16:17–24. doi: 10.5339/qmj.2014.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Almadi MA, Mosli MH, Bohlega MS, Al Essa MA, AlDohan MS, Alabdallatif TA, et al. Effect of public knowledge, attitudes, and behavior on willingness to undergo colorectal cancer screening using the health belief model. Saudi J Gastroenterol. 2015;21:71–7. doi: 10.4103/1319-3767.153814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zubaidi AM, AlSubaie NM, AlHumaid AA, Shaik SA, AlKhayal KA, AlObeed OA. Public awareness of colorectal cancer in Saudi Arabia: A survey of 1070 participants in Riyadh. Saudi J Gastroenterol. 2015;21:78–83. doi: 10.4103/1319-3767.153819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Demyati E. Knowledge, Attitude, Practice, and Perceived Barriers of Colorectal Cancer Screening among Family Physicians in National Guard Health Affairs, Riyadh. Int J Family Med 2014. 2014:457354. doi: 10.1155/2014/457354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elsamany SA, Alzahrani AS, Mohamed MM, Elmorsy SA, Zekri JE, Al-Shehri AS, et al. Clinico-pathological patterns and survival outcome of colorectal cancer in young patients: Western Saudi Arabia experience. Asian Pac J Cancer Prev. 2014;15:5239–43. doi: 10.7314/apjcp.2014.15.13.5239. [DOI] [PubMed] [Google Scholar]
- 27.Sibiani A, Shaheen M, Fallatah H, Akbar H, Qari Y, Bazaraa S, et al. Colorectal Cancer in Saudi Arabia King Abdul Aziz University Hospital: A Five Year Experience. J Med Med Sci. 2011;2:1126–30. [Google Scholar]
- 28.Amin TT, Suleman W, Al Taissan AA, Al Joher AL, Al Mulhim O, Al Yousef AH. Patients' profile, clinical presentations and histopathological features of colo-rectal cancer in Al Hassa region, Saudi Arabia. Asian Pac J Cancer Prev. 2012;13:211–6. doi: 10.7314/apjcp.2012.13.1.211. [DOI] [PubMed] [Google Scholar]
- 29.Almadi MA, Alharbi O, Azzam N, Wadera J, Sadaf N, Aljebreen AM. Prevalence and characteristics of colonic polyps and adenomas in 2654 colonoscopies in Saudi Arabia. Saudi J Gastroenterol. 2014;20:154–61. doi: 10.4103/1319-3767.132986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mosli MH, Al-Ahwal MS. Colorectal cancer in the Kingdom of Saudi Arabia: Need for screening. Asian Pac J Cancer Prev. 2012;13:3809–13. doi: 10.7314/apjcp.2012.13.8.3809. [DOI] [PubMed] [Google Scholar]
- 31.Towards a strategy for cancer control in the Eastern Mediterranean Region/World Health Organization. Regional Office for the Eastern Mediterranean, 2009. [Last accessed on 2016 Apr 02]. Available from: http://applications.emro.who.int/dsaf/dsa1002.pdf .
- 32.World Health Assembly. WHA 58.22 cancer prevention and control. [Last accessed on 2016 May 01]. Available from: http://apps.who.int/gb/ebwha/pdf_files/WHA58-REC1/english/A58_2005_REC1-en.pdf .
- 33.Policy and Advocacy. Cancer control: Knowledge into action: WHO guide for effective programmes; module 6. [Last accessed on 2016 Apr 05]. Available from: http://www.who.int/cancer/FINAL.Advocacy-Module%206.pdf .
- 34.Walt G, Gilson L. Reforming the health sector in developing countries: The central role of policy analysis. Health Policy Plan. 1994;9:353–70. doi: 10.1093/heapol/9.4.353. [DOI] [PubMed] [Google Scholar]
- 35.Barker C. The health care policy process. London: SAGE Publications Ltd; 1996. [Last accessed on 2015 Dec 09]. Available from: http://dx.doi.org/10.4135/9781446250471 . [Google Scholar]
- 36.Pollard A, Court J. 'How Civil Society Organisations Use Evidence to Influence Policy Processes: A literature review', ODI Working Paper 249, London: ODI. Overseas Development Institute 2005. ISBN 0850037611 [Google Scholar]
- 37.Young E, Quinn L. Writing Effective Public Policy Papers: A Guide to Policy Advisers in Central and Eastern Europe, 2002. Local Government and Public Reform Initiative; Budapest, Hungary. [Last accessed on 2015 Apr 07]. Available from: http://www.icpolicyadvocacy.org/sites/icpa/files/downloads/writing_effective_public_policy_papers_young_quinn.pdf .
- 38.Cancer Care Ontario, Expert Panel. Colorectal Cancer Screening: Final Report of the Ontario Expert Panel. 1999. Apr, [Last accessed on 2016 Jun 03]. Available from: https://www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=13608 .
- 39.Leddin DJ, Enns R, Hilsden R, Plourde V, Rabeneck L, Sadowski DC, et al. Canadian Association of Gastroenterology position statement on screening individuals at average risk for developing colorectal cancer: 2010. Can J Gastroenterol. 2010;24:705–14. doi: 10.1155/2010/683171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Canadian Task Force on Preventive Health Care. Recommendations on screening for colorectal cancer in primary care. CMAJ. 2016;188:340–8. doi: 10.1503/cmaj.151125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Trends in screening for colorectal cancer. United States, 1997 and 1999. MMWR Morb Mortal Wkly Rep. 2001;50:162–6. [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Colorectal cancer test use among persons aged 50 years—United States, 2001. MMWR Morb Mortal Wkly Rep. 2003;52:193–6. [PubMed] [Google Scholar]
- 43.Joseph DA, King JB, Miller JW, Richardson LC Centers for Disease Control and Prevention (CDC) Prevalence of colorectal cancer screening among adults-Behavioral Risk Factor Surveillance System, United States, 2010. MMWR Suppl. 2012;61:51–6. [PubMed] [Google Scholar]
- 44.Zack DL, DiBaise JK, Quigley EM, Roy HK. Colorectal cancer screening compliance by medicine residents: Perceived and actual. Am J Gastroenterol. 2001;96:3002–8. doi: 10.1111/j.1572-0241.2001.04678.x. [DOI] [PubMed] [Google Scholar]
- 45.Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: A joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–95. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 46.Wilt TJ, Harris RP, Qaseem A High Value Care Task Force of the American College of Physicians. Screening for cancer: Advice for high-value care from the American College of Physicians. Ann Intern Med. 2015;162:718–25. doi: 10.7326/M14-2326. [DOI] [PubMed] [Google Scholar]
- 47.US Preventive Services Task Force. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315:2564–75. doi: 10.1001/jama.2016.5989. [DOI] [PubMed] [Google Scholar]
- 48.Lin JS, Piper MA, Perdue LA, Rutter CM, Webber EM, O'Connor E, et al. Screening for Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016;315:2576–94. doi: 10.1001/jama.2016.3332. [DOI] [PubMed] [Google Scholar]
- 49.Zavoral M, Suchanek S, Zavada F, Dusek L, Muzik J, Seifert B, et al. Colorectal cancer screening in Europe. World J Gastroenterol. 2009;15:5907–15. doi: 10.3748/wjg.15.5907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.von Karsa L, Patnick J, Segnan N, Atkin W, Halloran S, Lansdorp-Vogelaar I, Malila N, Minozzi S, et al. European Colorectal Cancer Screening Guidelines Working Group. European guidelines for quality assurance in colorectal cancer screening and diagnosis: Overview and introduction to the full supplement publication. Endoscopy. 2013;45:51–9. doi: 10.1055/s-0032-1325997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Recommendations on cancer screening in the European Union. Advisory Committee on Cancer Prevention. Eur J Cancer. 2000;36:1473–8. doi: 10.1016/s0959-8049(00)00122-2. [DOI] [PubMed] [Google Scholar]
- 52.Sung JJ, Lau JY, Young GP, Sano Y, Chiu HM, Byeon JS, et al. Asia Pacific Working Group on Colorectal Cancer. Asia Pacific consensus recommendations for colorectal cancer screening. Gut. 2008;57:1166–76. doi: 10.1136/gut.2007.146316. [DOI] [PubMed] [Google Scholar]
- 53.Sung JJ, Ng SC, Chan FK, Chiu HM, Kim HS, Matsuda T, et al. Asia Pacific Working Group. An updated Asia Pacific Consensus Recommendations on colorectal cancer screening. Gut. 2015;64:121–32. doi: 10.1136/gutjnl-2013-306503. [DOI] [PubMed] [Google Scholar]
- 54.Sixty-first world health assembly. Geneva, May 2008. Resolutions and decisions annexes. [Last accessed on 2015 Apr 06]. Available at: http://apps.who.int/gb/ebwha/pdf_files/WHA61.REC1/A61_REC1.en.pdf .
- 55.National cancer control programmes: Policies and managerial guidelines. WHO. 2002. [Last accessed on 2015 Apr 04]. Available at: http://whqlibdoc.who.int/hq/2002/9241545577.pdf?ua=1 .
- 56.Abed J, Reilley B, Butler MO, Kean T, Wong F, Hohman K. Developing a framework for comprehensive cancer prevention and control in the United States: An initiative of the Centers for Disease Control and Prevention. J Public Health Manag Pract. 2000;6:67–78. doi: 10.1097/00124784-200006020-00011. [DOI] [PubMed] [Google Scholar]
- 57.Bridging the gap. UICC Annual Report 2006. International Union against Cancer. [Last accessed on 2015 Apr 08]. Available at: http://www.uicc.org/sites/main/files/private/Annual%20report%202006%20.pdf .


