Key Points
Question
What is the status of kidney health care across the world?
Findings
In a survey of 125 (96%) of 130 International Society of Nephrology–affiliated countries (representing an estimated 93% of the world’s population) with a response rate of 85.8% (289 of 337 individuals surveyed), the findings identified major variation in reported service delivery, funding mechanisms for kidney replacement therapy, and available technologies, such as facilities for kidney disease detection and management (eg, serum creatinine and proteinuria assessments).
Meaning
These findings on the status of global kidney care may inform efforts by governmental and nongovernmental groups to improve the quality of kidney care worldwide.
Abstract
Importance
Kidney disease is a substantial worldwide clinical and public health problem, but information about available care is limited.
Objective
To collect information on the current state of readiness, capacity, and competence for the delivery of kidney care across countries and regions of the world.
Design, Setting, and Participants
Questionnaire survey administered from May to September 2016 by the International Society of Nephrology (ISN) to 130 ISN-affiliated countries with sampling of key stakeholders (national nephrology society leadership, policy makers, and patient organization representatives) identified by the country and regional nephrology leadership through the ISN.
Main Outcomes and Measures
Core areas of country capacity and response for kidney care.
Results
Responses were received from 125 of 130 countries (96%), including 289 of 337 individuals (85.8%, with a median of 2 respondents [interquartile range, 1-3]), representing an estimated 93% (6.8 billion) of the world’s population of 7.3 billion. There was wide variation in country readiness, capacity, and response in terms of service delivery, financing, workforce, information systems, and leadership and governance. Overall, 119 (95%), 95 (76%), and 94 (75%) countries had facilities for hemodialysis, peritoneal dialysis, and kidney transplantation, respectively. In contrast, 33 (94%), 16 (45%), and 12 (34%) countries in Africa had facilities for hemodialysis, peritoneal dialysis, and kidney transplantation, respectively. For chronic kidney disease (CKD) monitoring in primary care, serum creatinine with estimated glomerular filtration rate and proteinuria measurements were reported as always available in only 21 (18%) and 9 (8%) countries, respectively. Hemodialysis, peritoneal dialysis, and transplantation services were funded publicly and free at the point of care delivery in 50 (42%), 48 (51%), and 46 (49%) countries, respectively. The number of nephrologists was variable and was low (<10 per million population) in Africa, the Middle East, South Asia, and Oceania and South East Asia (OSEA) regions. Health information system (renal registry) availability was limited, particularly for acute kidney injury (8 countries [7%]) and nondialysis CKD (9 countries [8%]). International acute kidney injury and CKD guidelines were reportedly accessible in 52 (45%) and 62 (52%) countries, respectively. There was relatively low capacity for clinical studies in developing nations.
Conclusions and Relevance
This survey demonstrated significant interregional and intraregional variability in the current capacity for kidney care across the world, including important gaps in services and workforce. Assuming the responses accurately reflect the status of kidney care in the respondent countries, the findings may be useful to inform efforts to improve the quality of kidney care worldwide.
This study surveyed international nephrology society leaders, policy makers, and patient representatives to assess regional resources and ability to care for patients with kidney disease.
Introduction
Kidney disease is a substantial worldwide clinical and public health problem. Acute kidney injury (AKI) and chronic kidney disease (CKD) are linked to high health care costs, poor quality of life, and serious adverse health outcomes (including cardiovascular disease, kidney failure requiring kidney replacement therapy, infection, depression, and mortality). However, despite the burden and population health effect of kidney diseases, AKI and CKD are often not included in the major chronic disease control strategies. As an example, the World Health Organization’s (WHO’s) Global Status Report on Noncommunicable Diseases 2014 makes almost no mention of kidney disease. This presents an obstacle for engaging with various governments in addressing AKI and CKD.
The Closing the Gaps initiative is led by the International Society of Nephrology (ISN) and aims to define the current state of kidney care (for AKI and CKD) worldwide, including policy recommendations for improvement. As part of this initiative, a global survey, the Global Kidney Health Atlas (GKHA) Project, was conducted to collect information on the current state of readiness, capacity, and competence for the delivery of kidney health care in each country and region.
Methods
Design and Participants
The GKHA Project was a multinational survey conducted by the ISN to assess current capacity for kidney care across the world. The survey was administered electronically to individuals in 130 countries with ISN affiliate societies through the ISN’s 10 regional boards (Africa, Central and Eastern Europe, Latin America, Middle East, North America, North and East Asia, Oceania and South East Asia [OSEA], newly independent states and Russia, South Asia, and Western Europe). The project was approved by the University of Alberta Research Ethics Committee (protocol number PRO00063121). All individual participants provided written informed consent.
Purposive sampling was undertaken to include at least 3 key stakeholders per country (national nephrology society leadership, health policy makers, and patient organization/foundation/advocacy representatives), each of whom was identified as being knowledgeable about their country’s kidney care status and nominated by the country and regional nephrology leadership through the ISN. In some cases, country stakeholders had a dual role (eg, both nephrology leader and policy maker) or particular stakeholders (eg, consumer organization representative) were unable to be identified, such that some countries were represented by fewer than 3 key stakeholders. The key representatives were sent a letter of invitation to participate that included a link to the survey’s online portal (an electronic questionnaire via SurveyMonkey [https://www.surveymonkey.com/]). Respondents were asked specifically about important within-country heterogeneity on kidney care funding and delivery and to identify other potential key respondents, increasing the likelihood that relevant information would be widely captured. The survey was conducted from May to September 2016. During this period, follow-up was conducted by email and telephone to ISN regional leaders and country leadership to facilitate completion and timely responses. During the survey period, each survey respondent who had not yet returned their survey received a personalized email reminder every 2 to 3 weeks up to a maximum of 3 attempts.
Development and Validation of Survey Instrument
The design of the GKHA questionnaire was meant to collect information about nations’ capacities and responses about noncommunicable disease prevention and control. The survey development process considered a number of documents, including WHO’s Universal Health Coverage: Supporting Country Needs, the ISN’s AKI “0 by 25” project, WHO Noncommunicable Disease Surveys (2000, 2005, 2010, and 2013), the World Heart Federation’s “25 by 25” goal, the International Diabetes Federation’s Global Diabetes Atlas, and WHO’s Global Atlas on Cardiovascular Disease Prevention and Control, as well as multiple United Nations policy documents on strategies, and policies for noncommunicable diseases. The initial survey questions were further developed through a series of reviews with relevant experts, the ISN Executive Committee, and regional leaderships.
The questionnaire was reviewed by the GKHA steering committee (scientific experts) and ISN regional leaders for content validity and comprehensiveness. The questionnaire was piloted across the 10 ISN regional board memberships to identify any logistical and feasibility issues (eg, need for translation). The format and content of the questionnaire (eAppendix 1 in the Supplement) were finalized based on feedback and identified issues, including translating the original English-language survey instrument into French and Spanish by certified translators. The French and Spanish surveys were checked by relevant regional boards and were back-translated into English.
The questionnaire was designed in 2 sections that addressed the core areas of country and regional capacity for kidney care delivery. The first section comprised 6 modules assessing country and regional profile for readiness, capacity, and response to CKD and AKI premised on the 6 health system building blocks (access to essential medicines and technologies, health systems financing, health service delivery, health workforce, health information systems, and leadership and governance). The second section contained questions that assessed response of the nephrology community (including care guidelines, position papers, service frameworks, and advocacy initiatives) and capacity for research and development.
Data Handling, Analysis, and Reporting
To facilitate data collation, responses to the French and Spanish surveys were first converted to English by certified translators. Data from all individual questionnaires were subsequently automatically extracted and checked for inconsistencies, missing data, duplications, and formatting errors. The data were then merged into a single file to create the global database. This was housed in a secured centralized computer system with automated backups.
Liaison with ISN regional leaders was undertaken to ensure that collated data were consistent with their understanding and were of high quality. Each of 10 regional boards reviewed their output to clarify any ambiguity or inconsistencies. Any major inconsistencies that remained following the reviews were systematically addressed by follow-up of individuals who responded to the survey. Further validation was carried out at country and regional levels by triangulation of the findings with published literature and other sources of information (government reports and other sources provided by the survey respondents). For example, among the responses for New Zealand, 2 indicated that there was an official registry for dialysis and transplantation, whereas 1 indicated that there was not an official registry. The existence of a New Zealand dialysis registry was subsequently confirmed by cross-checking with the OSEA Regional Board and the Australian and New Zealand Dialysis and Transplant Registry (http://www.anzdata.org.au/). Similarly, 2 Kenyan respondents indicated that there was a nephrology training program in Kenya, whereas 1 respondent said there was not a nephrology training program but also indicated only moderate certainty of the answer. Telephone discussion with the African Regional Board confirmed that a nephrology training program did exist in Kenya.
The framework developed by WHO (Assessing National Capacity for the Prevention and Control of Noncommunicable Diseases) was leveraged in the approach to the statistical analysis of the collated data. The analysis was conducted using Stata version 13 software (Stata Corp). The unit of analysis was responding country, and results were stratified by ISN region (n = 10) and World Bank country classification (n = 4) as low-, lower middle–, upper middle–, and high-income nations. Responses were summarized based on the key questionnaire domains using a descriptive statistical approach and reported as counts and percentages or medians and interquartile ranges, as appropriate. Nonquantitative data (text response items of the questionnaire) were thematically analyzed using a standard approach. The results were examined with an emphasis on identification of key gaps and challenges across the various domains based on the preexisting protocol and reported according to the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) statement.
Results
Response Rate
Responses were received from 125 (96%) of 130 countries, including 289 (85.8%) of 337 individuals (median of 2 respondents per country [interquartile range, 1-3]) representing an estimated 93% (6.8 billion) of the world’s population of 7.3 billion (Table 1). Responses were received from 100% (18/18), 97% (34/35), 91% (32/35), and 98% (40/41) of low-income, lower middle–income, upper middle–income, and high-income countries, respectively (Table 1). The respondent countries were representative of the countries in each region by population size (Table 1). The survey respondents consisted of nephrologists (247 [85%]), other physicians (10 [3%]), administrators/policy makers (16 [6%]), and others (16 [6%]) affiliated with kidney disease patient advocacy (Table 2).
Table 1. Countries and Populations.
| Total No. of Countries Recognized by UN | Total Population in All UN-Recognized Countries, in Millions | Total No. of Countries Receiving Survey | Total Population in Countries Receiving Survey, in Millions | No. (%) of Countries Completing Surveya | Total Population in Countries Completing Survey, in Millions | % of Population in Countries Receiving Surveyb | % of Population in all UN-Recognized Countriesc | |
|---|---|---|---|---|---|---|---|---|
| Overall | 200 | 7248 | 130 | 6778 | 125 (96) | 6754 | 99.6 | 93 |
| ISN regions | ||||||||
| Africa | 54 | 1156 | 37 | 969 | 35 (95) | 964 | 99 | 83 |
| Middle East | 14 | 225 | 13 | 223 | 13 (100) | 223 | 100 | 99 |
| Latin America | 25 | 608 | 18 | 571 | 17 (94) | 560 | 98 | 92 |
| North and East Asia | 7 | 1602 | 6 | 1577 | 6 (100) | 1577 | 100 | 98 |
| South Asia | 8 | 1707 | 5 | 1673 | 5 (100) | 1673 | 100 | 98 |
| OSEA | 25 | 671 | 13 | 661 | 13 (100) | 661 | 100 | 99 |
| East and Central Europe | 20 | 209 | 19 | 207 | 17 (89) | 199 | 96 | 95 |
| NIS and Russia | 11 | 281 | 6 | 223 | 6 (100) | 223 | 100 | 79 |
| Western Europe | 22 | 429 | 11 | 318 | 11 (100) | 318 | 100 | 74 |
| North America | 14 | 362 | 2 | 356 | 2 (100) | 356 | 100 | 398 |
| World Bank income groups | ||||||||
| Low | 31 | 631 | 18 | 405 | 18 (100) | 405 | 100 | 64 |
| Lower middle | 52 | 2862 | 35 | 2789 | 34 (97) | 2786 | 99.9 | 97 |
| Upper middle | 53 | 2370 | 35 | 2313 | 32 (91) | 2293 | 99 | 97 |
| High | 63 | 1386 | 41 | 1271 | 40 (98) | 1270 | 99.9 | 92 |
| Not classified | 1 | 0.02 | 1 | 0.02 | 1 (100) | 0.02 | 100 | 100 |
Abbreviations: ISN, International Society of Nephrology; NIS, newly independent states; OSEA, Oceania and South East Asia; UN, United Nations.
The percentage was calculated as total No. of countries that completed the survey/total No. of countries that received the survey.
The proportion was calculated as total population for countries that completed the survey/total population for countries that received the survey.
The proportion was calculated as total population for countries that completed the survey/total population in all UN-recognized countries.
Table 2. Respondent Affiliations Included in the Survey.
| Total No. of Respondentsa | No. of Respondents Per Country, Median (Interquartile Range)c | Respondent Affiliation, No. (%) | ||||
|---|---|---|---|---|---|---|
| Nephrologists | Other Physicians | Administrators/Policy Makers | Otherb | |||
| Overall | 289d | 2 (1-3) | 247 (85) | 10 (3) | 16 (6) | 16 (6) |
| ISN regions | ||||||
| Africa | 58 | 1 (1-2) | 42 (73) | 4 (7) | 6 (10) | 6 (10) |
| Middle East | 32 | 3 (2-3) | 29 (91) | 1 (3) | 1 (3) | 1 (3) |
| Latin America | 50 | 2 (1-3) | 50 (100) | 0 | 0 | 0 |
| North and East Asia | 31 | 6 (2-8) | 29 (94) | 0 | 1 (3) | 1 (3) |
| South Asia | 12 | 2 (2-3) | 10 (84) | 1 (8) | 1 (8) | 0 |
| OSEA | 39 | 2 (1-4) | 31 (79) | 2 (5) | 3 (8) | 3 (8) |
| East and Central Europe | 27 | 1 (1-2) | 26 (96) | 1 (4) | 0 | 0 |
| NIS and Russia | 12 | 1.5 (1-2) | 7 (59) | 0 | 4 (33) | 1 (8) |
| Western Europe | 21 | 2 (1-3) | 17 (81) | 1 (5) | 0 | 3 (14) |
| North America | 7 | 3.5 (3-4) | 6 (86) | 0 | 0 | 1 (14) |
| World Bank income groups | ||||||
| Low | 30 | 2 (1-2) | 22 (73) | 4 (13) | 2 (7) | 2 (7) |
| Lower middle | 68 | 2 (1-3) | 50 (73) | 4 (6) | 10 (15) | 4 (6) |
| Upper middle | 83 | 2 (1-3) | 76 (92) | 1 (1) | 4 (5) | 2 (2) |
| High | 107 | 2 (1-3.5) | 98 (92) | 1 (1) | 0 | 8 (7) |
| Not classified | 1 | 1 (1-1) | 1 (100) | 0 | 0 | 0 |
Abbreviations: ISN, International Society of Nephrology; NIS, newly independent states; OSEA, Oceania and South East Asia.
Total number of respondents to the survey, overall and by ISN regions and World Bank income groups.
Other types of stakeholders (eg, nurses, community health officers).
Median and interquartile range of respondents per country.
Overall number of individual respondents among 337 contacted (individual response rate of 85.8%).
Country Readiness, Capacity, and Response to CKD and AKI
Access to Essential Medicines and Technologies
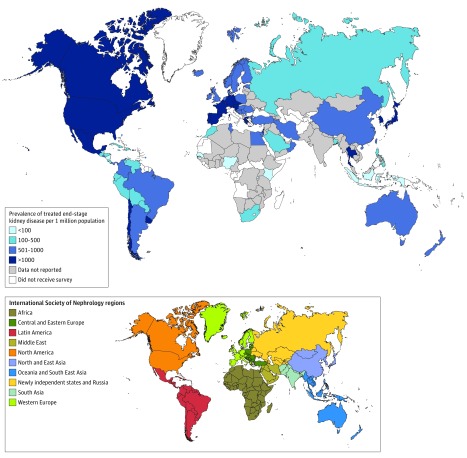
There were variations across ISN regions (n = 10) and World Bank income groups (n = 4) in the prevalence of treated end-stage renal disease represented by kidney replacement therapy (kidney replacement therapy: hemodialysis, peritoneal dialysis, and kidney transplantation), with the highest prevalence in developed regions in comparison with developing nations (Figure 1). The reported availability and access to essential medicines for CKD care and technologies also showed significant variations across regions and countries (eAppendix 2 in the Supplement). Among all countries (n=125 responding), 119 (95%), 95 (76%), and 94 (75%) had facilities for hemodialysis, long-term peritoneal dialysis, and kidney transplantation, respectively; 100% of high-income countries had such facilities. In contrast, 33 (94%), 16 (45%), and 12 (34%) countries in Africa had facilities for hemodialysis, long-term peritoneal dialysis, and kidney transplantation, respectively (eAppendix 2).
Figure 1. Global Prevalence of Treated End-Stage Renal Disease Per 1 Million Population.
The map depicts the prevalence of treated kidney failure per 1 million population based on individual country data. Data not available indicates that data were either not known or not provided on the questionnaire for countries that received the survey.
Health Systems Financing
The number of countries (n=118 responding) that reported complete public funding (completely free care at the point of delivery covered by the government) for chronic hemodialysis, long-term peritoneal dialysis, and kidney transplantation were 50 (42%), 48 (51%), and 46 (49%), respectively (Table 3). Overall, 45 (39%) and 34 (49%) countries reported complete public funding for hemodialysis and peritoneal dialysis, respectively, in the acute setting (Table 4). The public funding structures for all forms of kidney replacement therapy (hemodialysis, peritoneal dialysis, and kidney transplantation) were less common in the low- and lower middle–income countries (Table 3 and Table 4). There was significant variation across regions in access to medications for kidney care. For instance, no country from the low-income and lower middle–income categories reported complete public funding for medications for nondialysis CKD care (including angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, other antihypertensive agents, statins, and glucose-lowering agents) (Table 5 and eAppendix 2 in the Supplement). In contrast, 12 (32%) and 10 (32%) high- and upper middle–income nations reported complete public funding for medications in nondialysis CKD care (Table 5).
Table 3. Funding for Chronic Kidney Replacement Therapy Provision, Overall and by ISN Regions and World Bank Income Groups.
| No. of Responding Countries | No. (%) of Responding Countries | ||||||
|---|---|---|---|---|---|---|---|
| Publicly Funded by Government Free at the Point of Delivery | Publicly Funded by Government But With Some Fees at the Point of Delivery | Mix of Public and Private Funding Systems | Solely Private and Out of Pocket | Solely Private Through Health Insurance Providers | Multiple Funding Systemsa | ||
| Hemodialysis | |||||||
| Overall | 118 | 50 (42) | 14 (12) | 41 (35) | 2 (2) | 0 | 11 (9) |
| ISN regions | |||||||
| Africa | 33 | 10 (30) | 7 (21) | 12 (37) | 1 (3) | 0 | 3 (9) |
| Middle East | 13 | 9 (69) | 1 (8) | 1 (8) | 0 | 0 | 2 (15) |
| Latin America | 15 | 3 (20) | 0 | 11 (73) | 0 | 0 | 1 (7) |
| North and East Asia | 6 | 0 | 3 (50) | 2 (33) | 0 | 0 | 1 (17) |
| South Asia | 5 | 0 | 1 (20) | 3 (60) | 0 | 0 | 1 (20) |
| OSEA | 13 | 1 (8) | 2 (15) | 7 (54) | 1 (8) | 0 | 2 (15) |
| East and Central Europe | 16 | 14 (87) | 0 | 2 (13) | 0 | 0 | 0 |
| NIS and Russia | 6 | 4 (66) | 0 | 1 (17) | 0 | 0 | 1 (17) |
| Western Europe | 9 | 7 (78) | 0 | 2 (22) | 0 | 0 | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 | 0 | 0 |
| World Bank income groups | |||||||
| Low | 17 | 3 (18)b | 4 (24) | 6 (34) | 2 (12) | 0 | 2 (12) |
| Lower middle | 32 | 7 (21) | 6 (19) | 14 (44) | 0 | 0 | 5 (16) |
| Upper middle | 31 | 18 (59) | 0 | 11 (35) | 0 | 0 | 2 (6) |
| High | 38 | 22 (58) | 4 (11) | 10 (26) | 0 | 0 | 2 (5) |
| Peritoneal Dialysis | |||||||
| Overall | 95 | 48 (51) | 11 (12) | 28 (29) | 1 (1) | 0 | 7 (7) |
| ISN regions | |||||||
| Africa | 17 | 6 (35) | 4 (24) | 6 (35) | 0 | 0 | 1 (6) |
| Middle East | 11 | 7 (64) | 2 (18) | 0 | 1 (9) | 0 | 1 (9) |
| Latin America | 15 | 4 (27) | 0 | 11 (73) | 0 | 0 | 0 |
| North and East Asia | 6 | 0 | 4 (66) | 1 (17) | 0 | 0 | 1 (17) |
| South Asia | 5 | 1 (20) | 1 (20) | 2 (40) | 0 | 0 | 1 (20) |
| OSEA | 9 | 1 (11) | 0 | 6 (67) | 0 | 0 | 2 (22) |
| East and Central Europe | 15 | 14 (93) | 0 | 1 (7) | 0 | 0 | 0 |
| NIS and Russia | 6 | 5 (83) | 0 | 0 | 0 | 0 | 1 (17) |
| Western Europe | 9 | 8 (89) | 0 | 1 (11) | 0 | 0 | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 | 0 | 0 |
| World Bank income groups | |||||||
| Low | 6 | 0 | 2 (33) | 3 (50) | 0 | 0 | 1 (17) |
| Lower middle | 22 | 6 (27) | 3 (14) | 10 (45) | 1 (5) | 0 | 2 (9) |
| Upper middle | 29 | 17 (58) | 2 (7) | 8 (28) | 0 | 0 | 2 (7) |
| High | 38 | 25 (66) | 4 (11) | 7 (18) | 0 | 0 | 2 (5) |
| Kidney Transplantation | |||||||
| Overall | 93 | 46 (49) | 10 (11) | 28 (30) | 1 (1) | 0 | 8 (9) |
| ISN regions | |||||||
| Africa | 12 | 4 (33) | 1 (8) | 4 (33) | 1 (8) | 0 | 2 (18) |
| Middle East | 13 | 6 (46) | 4 (31) | 0 | 0 | 0 | 3 (23) |
| Latin America | 15 | 2 (13) | 0 | 12 (80) | 0 | 0 | 1 (7) |
| North and East Asia | 6 | 0 | 5 (83) | 0 | 0 | 0 | 1 (17) |
| South Asia | 5 | 0 | 0 | 5 (100) | 0 | 0 | 0 |
| OSEA | 9 | 3 (33) | 0 | 5 (56) | 0 | 0 | 1 (11) |
| East and Central Europe | 16 | 16 (100) | 0 | 0 | 0 | 0 | 0 |
| NIS and Russia | 6 | 5 (83) | 0 | 1 (17) | 0 | 0 | 0 |
| Western Europe | 9 | 8 (89) | 0 | 1 (11) | 0 | 0 | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 | 0 | 0 |
| World Bank income groups | |||||||
| Low | 2 | 1 (50) | 0 | 1 (50) | 0 | 0 | 0 |
| Lower middle | 24 | 4 (17) | 3 (13) | 13 (53) | 1 (4) | 0 | 3 (13) |
| Upper middle | 29 | 15 (52) | 2 (7) | 9 (31) | 0 | 0 | 3 (10) |
| High | 38 | 26 (69) | 5 (13) | 5 (13) | 0 | 0 | 2 (5) |
Abbreviations: ISN, International Society of Nephrology; NIS, newly independent states; OSEA, Oceania and South East Asia.
Involving government, nongovernmental organizations, and communities.
Low-income countries offering long-term hemodialysis free of cost were Chad, Gambia, and Guinea.
Table 4. Funding for Acute Kidney Replacement Therapy Provision, Overall and by ISN Regions and World Bank Income Groups.
| No. of Responding Countries | No. (%) of Responding Countries | ||||||
|---|---|---|---|---|---|---|---|
| Publicly Funded by Government Free at the Point of Delivery | Publicly Funded by Government But With Some Fees at the Point of Delivery | Mix of Public and Private Funding Systems | Solely Private and Out of Pocket | Solely Private Through Health Insurance Providers | Multiple Funding Systemsa | ||
| Acute Hemodialysis | |||||||
| Overall | 116 | 45 (39) | 22 (19) | 41 (35) | 1 (1) | 0 | 7 (6) |
| ISN regions | |||||||
| Africa | 32 | 10 (32) | 9 (28) | 9 (28) | 1 (3) | 0 | 3 (9) |
| Middle East | 13 | 6 (46) | 1 (8) | 4 (31) | 0 | 0 | 2 (15) |
| Latin America | 15 | 2 (13) | 0 | 13 (87) | 0 | 0 | 0 |
| North and East Asia | 6 | 0 | 4 (66) | 1 (17) | 0 | 0 | 1 (17) |
| South Asia | 5 | 0 | 1 (20) | 4 (80) | 0 | 0 | 0 |
| OSEA | 13 | 2 (15) | 4 (31) | 6 (46) | 0 | 0 | 1 (8) |
| East and Central Europe | 16 | 14 (88) | 1 (6) | 1 (6) | 0 | 0 | 0 |
| NIS and Russia | 5 | 3 (60) | 1 (20) | 1 (20) | 0 | 0 | 0 |
| Western Europe | 9 | 7 (78) | 1 (11) | 1 (11) | 0 | 0 | 0 |
| North America | 2 | 1 (50) | 0 | 1 (50) | 0 | 0 | 0 |
| World Bank income groups | |||||||
| Low | 16 | 4 (25)b | 5 (32) | 5 (31) | 1 (6) | 0 | 1 (6) |
| Lower middle | 32 | 5 (16) | 10 (31) | 14 (44) | 0 | 0 | 3 (9) |
| Upper middle | 30 | 16 (53) | 1 (3) | 11 (37) | 0 | 0 | 2 (7) |
| High | 38 | 20 (52) | 6 (16) | 11 (29) | 0 | 0 | 1 (3) |
| Acute Peritoneal Dialysis | |||||||
| Overall | 70 | 34 (49) | 11 (16) | 19 (27) | 3 (4) | 0 | 3 (4) |
| ISN regions | |||||||
| Africa | 11 | 3 (27) | 2 (18) | 4 (37) | 1 (9) | 0 | 1 (9) |
| Middle East | 7 | 5 (72) | 1 (14) | 0 | 0 | 0 | 1 (14) |
| Latin America | 14 | 4 (29) | 1 (7) | 7 (50) | 2 (14) | 0 | 0 |
| North and East Asia | 4 | 0 | 4 (100) | 0 | 0 | 0 | 0 |
| South Asia | 5 | 1 (20) | 0 | 4 (80) | 0 | 0 | 0 |
| OSEA | 6 | 1 (17) | 2 (33) | 2 (33) | 0 | 0 | 1 (17) |
| East and Central Europe | 11 | 10 (91) | 1 (9) | 0 | 0 | 0 | 0 |
| NIS and Russia | 4 | 4 (100) | 0 | 0 | 0 | 0 | 0 |
| Western Europe | 6 | 5 (83) | 0 | 1 (17) | 0 | 0 | 0 |
| North America | 2 | 1 (50) | 0 | 1 (50) | 0 | 0 | 0 |
| World Bank income groups | |||||||
| Low | 4 | 0 | 0 | 3 (75) | 1 (25) | 0 | 0 |
| Lower middle | 17 | 7 (41) | 3 (18) | 5 (29) | 0 | 0 | 2 (12) |
| Upper middle | 22 | 13 (59) | 2 (9) | 6 (27) | 1 (5) | 0 | 0 |
| High | 27 | 14 (51) | 6 (22) | 5 (19) | 1 (4) | 0 | 1 (4) |
Abbreviations: ISN, International Society of Nephrology; NIS, newly independent states; OSEA, Oceania and South East Asia.
Involving government, nongovernmental organizations, and communities.
Low-income countries offering acute hemodialysis free of cost were Chad, Gambia, Mozambique, and Tanzania.
Table 5. Access to Medications and Reimbursement Plans, Overall and by ISN Regions and World Bank Income Groups.
| No. of Responding Countries | No. (%) of Responding Countries | ||||||
|---|---|---|---|---|---|---|---|
| Publicly Funded by Government Free at the Point of Delivery | Publicly Funded by Government But With Some Fees at the Point of Delivery | Mix of Public and Private Funding Systems | Solely Private and Out of Pocket | Solely Private Through Health Insurance Providers | Multiple Funding Systemsa | ||
| Nondialysis Chronic Kidney Disease | |||||||
| Overall | 118 | 22 (19) | 22 (19) | 51 (42) | 9 (8) | 1 (1) | 13 (11) |
| ISN regions | |||||||
| Africa | 32 | 1 (3) | 8 (25) | 12 (37) | 6 (19) | 0 | 5 (16) |
| Middle East | 13 | 3 (23) | 2 (15) | 5 (39) | 1 (8) | 0 | 2 (15) |
| Latin America | 16 | 2 (13) | 0 | 12 (75) | 0 | 1 (6) | 1 (6) |
| North and East Asia | 6 | 1 (17) | 2 (33) | 2 (33) | 0 | 0 | 1 (17) |
| South Asia | 5 | 0 | 0 | 4 (80) | 0 | 0 | 1 (20) |
| OSEA | 13 | 1 (8) | 2 (15) | 8 (62) | 2 (15) | 0 | 0 |
| East and Central Europe | 16 | 11 (69) | 4 (25) | 1 (6) | 0 | 0 | 0 |
| NIS and Russia | 6 | 1 (17) | 0 | 3 (50) | 0 | 0 | 2 (33) |
| Western Europe | 9 | 2 (22) | 4 (45) | 2 (22) | 0 | 0 | 1 (11) |
| North America | 2 | 0 | 0 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||||
| Low | 17 | 0 | 3 (18) | 5 (29) | 5 (29) | 0 | 4 (24) |
| Lower middle | 32 | 0 | 7 (22) | 15 (46) | 4 (13) | 1 (3) | 5 (16) |
| Upper middle | 31 | 10 (32) | 2 (6) | 17 (56) | 0 | 0 | 2 (6) |
| High | 38 | 12 (32) | 10 (26) | 14 (37) | 0 | 0 | 2 (5) |
| Dialysis | |||||||
| Overall | 118 | 26 (22) | 29 (25) | 46 (38) | 8 (7) | 1 (1) | 8 (7) |
| ISN regions | |||||||
| Africa | 32 | 2 (6) | 9 (28) | 11 (34) | 6 (19) | 0 | 4 (13) |
| Middle East | 13 | 5 (39) | 4 (31) | 2 (15) | 0 | 0 | 2 (15) |
| Latin America | 16 | 3 (19) | 0 | 12 (75) | 0 | 1 (6) | 0 |
| North and East Asia | 6 | 0 | 3 (50) | 2 (33) | 0 | 0 | 1 (17) |
| South Asia | 5 | 0 | 0 | 4 (80) | 1 (20) | 0 | 0 |
| OSEA | 13 | 0 | 4 (30) | 8 (62) | 1 (8) | 0 | 0 |
| East and Central Europe | 16 | 12 (75) | 4 (25) | 0 | 0 | 0 | 0 |
| NIS and Russia | 6 | 1 (17) | 0 | 4 (66) | 0 | 0 | 1 (17) |
| Western Europe | 9 | 3 (33) | 5 (56) | 1 (11) | 0 | 0 | 0 |
| North America | 2 | 0 | 0 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||||
| Low | 17 | 0 | 4 (24) | 6 (35) | 5 (29) | 0 | 2 (12) |
| Lower middle | 32 | 0 | 7 (22) | 18 (57) | 3 (9) | 1 (3) | 3 (9) |
| Upper middle | 31 | 13 (42) | 4 (13) | 12 (39) | 0 | 0 | 2 (6) |
| High | 38 | 13 (34) | 14 (37) | 10 (26) | 0 | 0 | 1 (3) |
| Kidney Transplantation | |||||||
| Overall | 118 | 35 (30) | 22 (18) | 35 (30) | 18 (15) | 1 (1) | 7 (6) |
| ISN regions | |||||||
| Africa | 32 | 5 (16) | 3 (9) | 6 (19) | 14 (43) | 0 | 4 (13) |
| Middle East | 13 | 7 (54) | 3 (23) | 0 | 0 | 0 | 3 (23) |
| Latin America | 16 | 4 (25) | 0 | 11 (69) | 0 | 1 (6) | 0 |
| North and East Asia | 6 | 0 | 3 (50) | 3 (50) | 0 | 0 | 0 |
| South Asia | 5 | 0 | 0 | 4 (80) | 1 (20) | 0 | 0 |
| OSEA | 13 | 1 (8) | 2 (15) | 7 (54) | 3 (23) | 0 | 0 |
| East and Central Europe | 16 | 13 (81) | 3 (19) | 0 | 0 | 0 | 0 |
| NIS and Russia | 6 | 4 (66) | 1 (17) | 1 (17) | 0 | 0 | 0 |
| Western Europe | 9 | 1 (11) | 7 (78) | 1 (11) | 0 | 0 | 0 |
| North America | 2 | 0 | 0 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||||
| Low | 17 | 0 | 1 (6) | 3 (18) | 10 (58) | 0 | 3 (18) |
| Lower middle | 32 | 6 (19) | 4 (13) | 12 (37) | 7 (22) | 1 (3) | 2 (6) |
| Upper middle | 31 | 15 (49) | 3 (10) | 11 (35) | 1 (3) | 0 | 1 (3) |
| High | 38 | 14 (37) | 14 (37) | 9 (23) | 0 | 0 | 1 (3) |
Abbreviations: ISN, International Society of Nephrology; NIS, newly independent states; OSEA, Oceania and South East Asia.
Involving government, nongovernmental organizations, and communities.
Health Service Delivery
Globally, infrastructure available for kidney care was reported to be good/above average in 48 (39%) and excellent in 11 (9%) countries for AKI. For CKD, 46 (38%) countries were rated good/above average and 9 (7%) were rated excellent (eTable 1 in the Supplement). Reports of extremely poor or poor/below average infrastructure for AKI and CKD care were highest in Africa and South Asia and lowest in Western Europe and North America (eTable 1). Pertaining to services used for monitoring CKD, measurement of serum creatinine reported with estimated glomerular filtration rate (eGFR) was described as always or usually available at the primary and secondary care levels in only 21 (18%) or 23 (19%) and 43 (40%) or 25 (23%) countries, respectively (Table 6, Table 7, and eAppendix 3 in the Supplement). Pathological services for renal biopsy were always available at the secondary care level for 27 (23%) countries but were otherwise rarely or never available in 28 (24%) and 16 (14%) countries, respectively (Table 7 and eAppendix 3).
Table 6. Availability of Services for Chronic Kidney Disease Monitoring and Management at Primary Care Level.
| No. of Responding Countries | Availability, No. (%) of Responding Countries | ||||
|---|---|---|---|---|---|
| Always | Usually | Rarely | Never | ||
| Blood Pressure | |||||
| Overall | 119 | 75 (63) | 40 (34) | 4 (3) | 0 |
| ISN regions | |||||
| Africa | 33 | 15 (45) | 16 (49) | 2 (6) | 0 |
| Middle East | 13 | 9 (70) | 2 (15) | 2 (15) | 0 |
| Latin America | 16 | 12 (75) | 4 (25) | 0 | 0 |
| North and East Asia | 6 | 1 (17) | 5 (83) | 0 | 0 |
| South Asia | 5 | 3 (60) | 2 (40) | 0 | 0 |
| OSEA | 13 | 8 (62) | 5 (38) | 0 | 0 |
| East and Central Europe | 16 | 14 (87) | 2 (13) | 0 | 0 |
| NIS and Russia | 6 | 4 (67) | 2 (33) | 0 | 0 |
| Western Europe | 9 | 7 (78) | 2 (22) | 0 | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 8 (47) | 8 (47) | 1 (6) | 0 |
| Lower middle | 33 | 16 (49) | 15 (45) | 2 (6) | 0 |
| Upper middle | 31 | 23 (74) | 8 (26) | 0 | 0 |
| High | 38 | 28 (73) | 9 (24) | 1 (3) | 0 |
| Blood Glucose | |||||
| Overall | 119 | 48 (40) | 50 (42) | 19 (16) | 2 (2) |
| ISN regions | |||||
| Africa | 33 | 9 (27) | 10 (30) | 12 (37) | 2 (6) |
| Middle East | 13 | 6 (46) | 6 (46) | 1 (8) | 0 |
| Latin America | 16 | 7 (44) | 7 (44) | 2 (12) | 0 |
| North and East Asia | 6 | 0 | 6 (100) | 0 | 0 |
| South Asia | 5 | 1 (20) | 2 (40) | 2 (40) | 0 |
| OSEA | 13 | 4 (31) | 8 (61) | 1 (8) | 0 |
| East and Central Europe | 16 | 10 (63) | 5 (31) | 1 (6) | 0 |
| NIS and Russia | 6 | 2 (33) | 4 (67) | 0 | 0 |
| Western Europe | 9 | 8 (89) | 1 (11) | 0 | 0 |
| North America | 2 | 1 (50) | 1 (50) | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 4 (24) | 3 (18) | 8 (46) | 2 (12) |
| Lower middle | 33 | 9 (27) | 16 (49) | 8 (24) | 0 |
| Upper middle | 31 | 12 (39) | 17 (55) | 2 (6) | 0 |
| High | 38 | 23 (60) | 14 (37) | 1 (3) | 0 |
| Serum Creatinine | |||||
| Serum creatinine with eGFR reporting | |||||
| Overall | 119 | 21 (18) | 23 (19) | 48 (40) | 27 (23) |
| ISN regions | |||||
| Africa | 33 | 1 (3) | 4 (12) | 15 (46) | 13 (39) |
| Middle East | 13 | 1 (8) | 3 (23) | 7 (54) | 2 (15) |
| Latin America | 16 | 2 (13) | 4 (25) | 7 (43) | 3 (19) |
| North and East Asia | 6 | 0 | 2 (33) | 3 (50) | 1 (17) |
| South Asia | 5 | 1 (20) | 0 | 3 (60) | 1 (20) |
| OSEA | 13 | 2 (15) | 3 (23) | 6 (47) | 2 (15) |
| East and Central Europe | 16 | 8 (49) | 3 (19) | 3 (19) | 2 (13) |
| NIS and Russia | 6 | 0 | 1 (17) | 2 (33) | 3 (50) |
| Western Europe | 9 | 5 (56) | 2 (22) | 2 (22) | 0 |
| North America | 2 | 1 (50) | 1 (50) | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 0 | 0 | 7 (41) | 10 (59) |
| Lower middle | 33 | 3 (9) | 2 (6) | 18 (55) | 10 (30) |
| Upper middle | 31 | 4 (13) | 9 (29) | 12 (39) | 6 (19) |
| High | 38 | 14 (36) | 12 (32) | 11 (29) | 1 (3) |
| Serum creatinine without eGFR reporting | |||||
| Overall | 119 | 31 (26) | 46 (39) | 32 (27) | 10 (8) |
| ISN regions | |||||
| Africa | 33 | 5 (15) | 10 (30) | 12 (37) | 6 (18) |
| Middle East | 13 | 5 (38) | 5 (38) | 3 (24) | 0 |
| Latin America | 16 | 4 (25) | 9 (56) | 3 (19) | 0 |
| North and East Asia | 6 | 0 | 5 (83) | 1 (17) | 0 |
| South Asia | 5 | 1 (20) | 1 (20) | 2 (40) | 1 (20) |
| OSEA | 13 | 3 (23) | 3 (23) | 5 (39) | 2 (15) |
| East and Central Europe | 16 | 7 (44) | 4 (25) | 4 (25) | 1 (6) |
| NIS and Russia | 6 | 1 (17) | 5 (83) | 0 | 0 |
| Western Europe | 9 | 5 (56) | 2 (22) | 2 (22) | 0 |
| North America | 2 | 0 | 2 (100) | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 1 (6) | 4 (24) | 5 (29) | 7 (41) |
| Lower middle | 33 | 5 (15) | 13 (40) | 13 (39) | 2 (6) |
| Upper middle | 31 | 9 (29) | 18 (58) | 4 (13) | 0 |
| High | 38 | 16 (42) | 11 (29) | 10 (26) | 1 (3) |
| Radiology Services | |||||
| Overall | 119 | 17 (14) | 38 (32) | 48 (41) | 16 (13) |
| ISN regions | |||||
| Africa | 33 | 5 (15) | 5 (15) | 14 (43) | 9 (27) |
| Middle East | 13 | 1 (8) | 3 (23) | 6 (46) | 3 (23) |
| Latin America | 16 | 3 (19) | 3 (19) | 9 (56) | 1 (6) |
| North and East Asia | 6 | 1 (17) | 1 (17) | 4 (66) | 0 |
| South Asia | 5 | 1 (20) | 1 (20) | 3 (60) | 0 |
| OSEA | 13 | 0 | 6 (46) | 6 (46) | 1 (8) |
| East and Central Europe | 16 | 3 (19) | 9 (56) | 3 (19) | 1 (6) |
| NIS and Russia | 6 | 1 (17) | 3 (50) | 2 (33) | 0 |
| Western Europe | 9 | 2 (22) | 5 (56) | 1 (11) | 1 (11) |
| North America | 2 | 0 | 2 (100) | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 1 (6) | 1 (6) | 8 (47) | 7 (41) |
| Lower middle | 33 | 4 (12) | 8 (24) | 18 (55) | 3 (9) |
| Upper middle | 31 | 6 (19) | 10 (32) | 11 (36) | 4 (13) |
| High | 38 | 6 (16) | 19 (50) | 11 (29) | 2 (5) |
| Urinalysis (Qualitative Assays) | |||||
| Overall | 119 | 26 (22) | 54 (45) | 32 (27) | 7 (6) |
| ISN regions | |||||
| Africa | 33 | 5 (15) | 11 (33) | 13 (40) | 4 (12) |
| Middle East | 13 | 2 (15) | 10 (77) | 1 (8) | 0 |
| Latin America | 16 | 3 (19) | 6 (38) | 6 (37) | 1 (6) |
| North and East Asia | 6 | 0 | 4 (67) | 2 (33) | 0 |
| South Asia | 5 | 2 (40) | 2 (40) | 1 (20) | 0 |
| OSEA | 13 | 2 (16) | 5 (38) | 5 (38) | 1 (8) |
| East and Central Europe | 16 | 7 (44) | 7 (44) | 1 (6) | 1 (6) |
| NIS and Russia | 6 | 1 (17) | 2 (33) | 3 (50) | 0 |
| Western Europe | 9 | 4 (44) | 5 (56) | 0 | 0 |
| North America | 2 | 0 | 2 (100) | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 3 (18) | 4 (24) | 7 (41) | 3 (18) |
| Lower middle | 33 | 5 (16) | 13 (39) | 13 (39) | 2 (6) |
| Upper middle | 31 | 4 (13) | 18 (58) | 7 (23) | 2 (6) |
| High | 38 | 14 (37) | 19 (50) | 5 (13) | 0 |
| UACR or UPCR Measurement | |||||
| Overall | 119 | 9 (8) | 29 (24) | 52 (44) | 29 (24) |
| ISN regions | |||||
| Africa | 33 | 0 | 4 (12) | 11 (33) | 18 (55) |
| Middle East | 13 | 0 | 6 (46) | 6 (46) | 1 (8) |
| Latin America | 16 | 3 (19) | 5 (31) | 5 (31) | 3 (19) |
| North and East Asia | 6 | 0 | 0 | 6 (100) | 0 |
| South Asia | 5 | 0 | 1 (20) | 4 (80) | 0 |
| OSEA | 13 | 1 (8) | 3 (23) | 7 (54) | 2 (15) |
| East and Central Europe | 16 | 2 (13) | 2 (13) | 9 (55) | 3 (19) |
| NIS and Russia | 6 | 0 | 1 (17) | 3 (50) | 2 (33) |
| Western Europe | 9 | 3 (33) | 5 (56) | 1 (11) | 0 |
| North America | 2 | 0 | 2 (100) | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 0 | 0 | 3 (18) | 14 (82) |
| Lower middle | 33 | 1 (3) | 4 (12) | 18 (55) | 10 (30) |
| Upper middle | 31 | 3 (10) | 8 (26) | 16 (51) | 4 (13) |
| High | 38 | 5 (13) | 17 (45) | 15 (39) | 1 (3) |
Abbreviations: eGFR, estimated glomerular filtration rate; ISN, International Society of Nephrology; NIS, newly independent states; OSEA, Oceania and South East Asia; UACR, urine albumin:creatinine ratio; UPCR, urine protein:creatinine ratio.
Table 7. Availability of Services for Chronic Kidney Disease Monitoring and Management at Secondary or Tertiary Care Levels.
| No. of Responding Countries | Availability, No. (%) of Responding Countries | ||||
|---|---|---|---|---|---|
| Always | Usually | Rarely | Never | ||
| Blood Pressure | |||||
| Overall | 119 | 106 (89) | 13 (11) | 0 | 0 |
| ISN regions | |||||
| Africa | 33 | 27 (82) | 6 (18) | 0 | 0 |
| Middle East | 13 | 13 (100) | 0 | 0 | 0 |
| Latin America | 16 | 15 (94) | 1 (6) | 0 | 0 |
| North and East Asia | 6 | 3 (50) | 3 (50) | 0 | 0 |
| South Asia | 5 | 5 (100) | 0 | 0 | 0 |
| OSEA | 13 | 12 (92) | 1 (8) | 0 | 0 |
| East and Central Europe | 16 | 16 (100) | 0 | 0 | 0 |
| NIS and Russia | 6 | 5 (83) | 1 (17) | 0 | 0 |
| Western Europe | 9 | 8 (89) | 1 (11) | 0 | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 14 (82) | 3 (18) | 0 | 0 |
| Lower middle | 33 | 28 (85) | 5 (15) | 0 | 0 |
| Upper middle | 31 | 29 (94) | 2 (6) | 0 | 0 |
| High | 38 | 35 (92) | 3 (8) | 0 | 0 |
| Blood Glucose | |||||
| Overall | 119 | 83 (70) | 35 (29) | 1 (1) | 0 |
| ISN regions | |||||
| Africa | 33 | 18 (55) | 14 (42) | 1 (3) | 0 |
| Middle East | 13 | 12 (92) | 1 (8) | 0 | 0 |
| Latin America | 16 | 14 (87) | 2 (13) | 0 | 0 |
| North and East Asia | 6 | 1 (17) | 5 (83) | 0 | 0 |
| South Asia | 5 | 4 (80) | 1 (20) | 0 | 0 |
| OSEA | 13 | 7 (54) | 6 (46) | 0 | 0 |
| East and Central Europe | 16 | 15 (94) | 1 (6) | 0 | 0 |
| NIS and Russia | 6 | 3 (50) | 3 (50) | 0 | 0 |
| Western Europe | 9 | 7 (78) | 2 (22) | 0 | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 10 (59) | 7 (41) | 0 | 0 |
| Lower middle | 33 | 17 (52) | 15 (45) | 1 (3) | 0 |
| Upper middle | 31 | 25 (81) | 6 (19) | 0 | 0 |
| High | 38 | 31 (82) | 7 (18) | 0 | 0 |
| Serum Creatinine | |||||
| Serum creatinine with eGFR reporting | |||||
| Overall | 108 | 43 (40) | 25 (23) | 25 (23) | 15 (14) |
| ISN regions | |||||
| Africa | 33 | 7 (21) | 6 (18) | 8 (24) | 12 (37) |
| Middle East | 13 | 5 (38) | 5 (38) | 3 (24) | 0 |
| Latin America | 5 | 2 (40) | 1 (20) | 1 (20) | 1 (20) |
| North and East Asia | 6 | 1 (17) | 4 (66) | 1 (17) | 0 |
| South Asia | 5 | 0 | 2 (40) | 2 (40) | 1 (20) |
| OSEA | 13 | 6 (46) | 3 (23) | 4 (31) | 0 |
| East and Central Europe | 16 | 11 (68) | 2 (13) | 2 (13) | 1 (6) |
| NIS and Russia | 6 | 2 (33) | 1 (17) | 3 (50) | 0 |
| Western Europe | 9 | 7 (78) | 1 (11) | 1 (11) | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 2 (12) | 1 (6) | 3 (18) | 11 (64) |
| Lower middle | 29 | 5 (17) | 9 (31) | 13 (45) | 2 (7) |
| Upper middle | 27 | 10 (37) | 10 (37) | 5 (19) | 2 (7) |
| High | 35 | 26 (75) | 5 (14) | 4 (11) | 0 |
| Serum creatinine without eGFR reporting | |||||
| Overall | 117 | 68 (58) | 40 (34) | 7 (6) | 2 (2) |
| ISN regions | |||||
| Africa | 32 | 9 (28) | 19 (60) | 3 (9) | 1 (3) |
| Middle East | 13 | 13 (100) | 0 | 0 | 0 |
| Latin America | 16 | 10 (62) | 6 (38) | 0 | 0 |
| North and East Asia | 6 | 3 (50) | 3 (50) | 0 | 0 |
| South Asia | 5 | 3 (60) | 2 (40) | 0 | 0 |
| OSEA | 12 | 6 (50) | 5 (42) | 1 (8) | 0 |
| East and Central Europe | 16 | 12 (75) | 2 (13) | 1 (6) | 1 (6) |
| NIS and Russia | 6 | 5 (83) | 1 (17) | 0 | 0 |
| Western Europe | 9 | 5 (56) | 2 (22) | 2 (22) | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 2 (12) | 12 (70) | 2 (12) | 1 (6) |
| Lower middle | 31 | 16 (52) | 13 (42) | 2 (6) | 0 |
| Upper middle | 31 | 24 (77) | 7 (23) | 0 | 0 |
| High | 38 | 26 (68) | 8 (21) | 3 (8) | 1 (3) |
| UACR or UPCR Measurement | |||||
| Overall | 118 | 32 (27) | 47 (40) | 28 (24) | 11 (9) |
| ISN regions | |||||
| Africa | 32 | 2 (6) | 8 (25) | 14 (44) | 8 (25) |
| Middle East | 13 | 5 (38) | 8 (62) | 0 | 0 |
| Latin America | 16 | 4 (25) | 10 (62) | 2 (13) | 0 |
| North and East Asia | 6 | 1 (17) | 4 (66) | 0 | 1 (17) |
| South Asia | 5 | 0 | 3 (60) | 2 (40) | 0 |
| OSEA | 13 | 4 (31) | 4 (31) | 5 (38) | 0 |
| East and Central Europe | 16 | 7 (44) | 4 (25) | 4 (25) | 1 (6) |
| NIS and Russia | 6 | 1 (17) | 3 (49) | 1 (17) | 1 (17) |
| Western Europe | 9 | 6 (67) | 3 (33) | 0 | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 0 | 1 (6) | 10 (59) | 6 (35) |
| Lower middle | 33 | 3 (9) | 15 (46) | 13 (39) | 2 (6) |
| Upper middle | 30 | 9 (30) | 14 (47) | 4 (13) | 3 (10) |
| High | 38 | 20 (52) | 17 (45) | 1 (3) | 0 |
| Radiology Services (Ultrasound) | |||||
| Overall | 119 | 68 (57) | 45 (38) | 6 (5) | 0 |
| ISN regions | |||||
| Africa | 33 | 13 (39) | 16 (49) | 4 (12) | 0 |
| Middle East | 13 | 12 (92) | 1 (8) | 0 | 0 |
| Latin America | 16 | 8 (50) | 8 (50) | 0 | 0 |
| North and East Asia | 6 | 3 (50) | 3 (50) | 0 | 0 |
| South Asia | 5 | 3 (60) | 2 (40) | 0 | 0 |
| OSEA | 13 | 5 (38) | 6 (47) | 2 (15) | 0 |
| East and Central Europe | 16 | 12 (75) | 4 (25) | 0 | 0 |
| NIS and Russia | 6 | 4 (67) | 2 (33) | 0 | 0 |
| Western Europe | 9 | 6 (67) | 3 (33) | 0 | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 5 (29) | 9 (53) | 3 (18) | 0 |
| Lower middle | 33 | 15 (45) | 16 (49) | 2 (6) | 0 |
| Upper middle | 31 | 19 (62) | 11 (35) | 1 (3) | 0 |
| High | 38 | 29 (76) | 9 (24) | 0 | 0 |
| Pathology Services (Renal Biopsy) | |||||
| Overall | 118 | 27 (23) | 47 (39) | 28 (24) | 16 (14) |
| ISN regions | |||||
| Africa | 32 | 1 (3) | 6 (19) | 13 (40) | 12 (38) |
| Middle East | 13 | 4 (31) | 8 (61) | 1 (8) | 0 |
| Latin America | 16 | 2 (13) | 11 (68) | 2 (13) | 1 (6) |
| North and East Asia | 6 | 1 (17) | 3 (50) | 2 (33) | 0 |
| South Asia | 5 | 0 | 4 (80) | 1 (20) | 0 |
| OSEA | 13 | 3 (23) | 3 (23) | 5 (39) | 2 (15) |
| East and Central Europe | 16 | 9 (56) | 4 (25) | 2 (13) | 1 (6) |
| NIS and Russia | 6 | 0 | 4 (67) | 2 (33) | 0 |
| Western Europe | 9 | 5 (56) | 4 (44) | 0 | 0 |
| North America | 2 | 2 (100) | 0 | 0 | 0 |
| World Bank income groups | |||||
| Low | 17 | 0 | 3 (18) | 5 (29) | 9 (53) |
| Lower middle | 32 | 1 (3) | 12 (37) | 15 (47) | 4 (13) |
| Upper middle | 31 | 3 (10) | 18 (57) | 7 (23) | 3 (10) |
| High | 38 | 23 (60) | 14 (37) | 1 (3) | 0 |
Abbreviations: eGFR, estimated glomerular filtration rate; ISN, International Society of Nephrology; NIS, newly independent states; OSEA, Oceania and South East Asia; UACR, urine albumin:creatinine ratio; UPCR, urine protein:creatinine ratio.
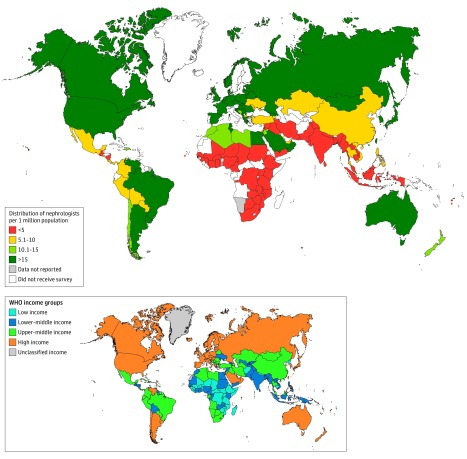
Health Workforce
Respondents from countries were asked to provide estimates of the number of trained nephrologists, as defined by the relevant regulatory authorities, and provide an opinion regarding shortage (yes/no) of the workforce required for kidney care delivery. There was a low reported nephrology workforce density (≤10 per 1 million population) for several countries in the Africa, North and East Asia, and South Asia regions as well as in parts of Latin America (Figure 2). There were also wide disparities in the number of nephrologists across countries and regions. For instance, 9 of the 10 countries with the lowest numbers of nephrologists were in sub-Saharan Africa (eFigure 1A in the Supplement), whereas the countries with the highest number of nephrologists were from several regions, with Lithuania, Taiwan, and Japan reporting the highest numbers of nephrologists per 1 million population (eFigure 1B in the Supplement). Overall, there were frequent reported shortages of the various categories of other health care workers. Most countries had reported shortages of vascular access coordinators, transplant coordinators, social workers, renal pathologists, nurse practitioners, nephrologists, dieticians, dialysis technicians, dialysis nurses, and counselors and psychologists (Figure 2C). In contrast, fewer countries reported shortages of pharmacists, laboratory technicians, and primary care physicians (Figure 2C). By region, shortages of other health care clinicians were more common in Africa, the Middle East, Latin America, South Asia, North and East Asia, OSEA, and East and Central Europe (eTable 2 in the Supplement). For example, 28 (85%) countries in Africa had reported shortages of nephrologists compared with only 2 (20%) countries in Western Europe with reported shortages of this category of workforce (eTable 2).
Figure 2. Global Distribution of Nephrologists Per 1 Million Population.
The map depicts global distribution of nephrologists per 1 million population by country and region. Data not available indicates that data were either not known or not provided on the questionnaire for countries that received the survey.
Health Information Systems
Countries were asked to provide data on the availability of registries (surveillance and monitoring systems) for kidney replacement therapy and nondialysis CKD and AKI. The prevalence of treated end-stage renal disease was comparatively low in some regions compared with others (Figure 1). For instance, Africa, the Middle East, and South Asia had low prevalence of treated end-stage renal disease in comparison with North America and Western Europe (where the prevalence was generally above 1000 per 1 million population) (Figure 1). Overall, only 9 (7.7%) and 8 (6.8%) countries reported having registries for nondialysis CKD and AKI, respectively (eFigure 2 and eAppendix 3 in the Supplement). There was wide variation in the presence of kidney replacement therapy registries across regions, with most countries reporting having dialysis registries and fewer reporting having kidney transplant registries, particularly in Africa, the Middle East, and South Asia (eFigure 2 and eAppendix 3). Dialysis and kidney transplant registries were most commonly available in Western Europe, North and East Asia, North America, and East and Central European countries (eFigure 2 and eAppendix 3).
Leadership and Governance
Specific national strategies for improving the care of patients with CKD were reported as present in only 19 countries (17%) (eTable 3 in the Supplement). There were variations in the availability of 1 or more of the various strategies (national position paper, identification tools, incentives, etc) for improving identification of AKI across regions; 59 countries (51%) had none of these strategies (eTable 4 in the Supplement).
Response of the Nephrology Community (Guidelines and Advocacy for Kidney Care)
The majority of countries reported access predominantly to international guidelines compared with national guidelines. Access to international CKD and AKI management guidelines was reported in 60 (52%) and 52 (45%) countries, respectively (eTable 5 in the Supplement). Thirty-one countries (27%) reported availability of national guidelines for CKD (eTable 5). In contrast, only 8 countries (7%) reported access to national guidelines for AKI. Presence of CKD and AKI advocacy groups were limited in most regions and were more common for CKD than for AKI (eFigure 3 and eAppendix 3 in the Supplement).
Capacity for Research and Development
Respondents rated their involvement with different phases of clinical trials and observational research studies (available infrastructure, trained workforce, ethical frameworks, etc). Low capacity for participation in different aspects of clinical trials was frequently reported, especially in developing countries and regions (eAppendix 3 in the Supplement). For example, only 33 (28%) and 46 (40%) countries overall could participate in phase 1 and phase 2 clinical trials, respectively (eTable 6 and eAppendix 3 in the Supplement). Western Europe and North America reported the highest capacity to participate in all phases of clinical trials (eTable 6 and eAppendix 3). For instance, all countries in these 2 regions reported capacity to participate in phase 3 and 4 trials in contrast to only 5 (17%) and 4 (13%) in Africa, respectively (eTable 6). Although most countries described some capacity to conduct or participate in observational cohort studies, Africa and Middle East countries reported no capacity to participate in transplantation cohort studies (eTable 6). Institutional ethics approval was the most common study approval type in most countries overall and across most regions (eTable 6).
Discussion
To our knowledge, this is the first systematic assessment of the global capacity for kidney care in terms of the key building blocks of a functional health system and readiness of countries and regions to enhance such care. There were significant gaps reported in services, facilities, and workforce in some countries and regions. Most countries in Africa described no facilities for peritoneal dialysis or kidney transplantation. Few countries reported complete public funding for kidney replacement therapy services and medications for CKD care (including dialysis and transplantation); there was a large private contribution toward payment for kidney replacement therapy services and medications reported particularly in countries across the Africa, South Asia, and OSEA regions. Even though the infrastructure available for AKI and CKD care was mostly rated as average or above average, survey responses suggested that measurement of serum creatinine with eGFR was common at the primary care level in only a few countries. Availability of pathological services for kidney biopsy was described as very low. Overall, there was a reported shortage of nephrology workforce and other workforce categories in many settings. There was limited availability of health information systems (renal registries), particularly for nondialysis CKD and AKI. National or regional strategies for improving CKD and AKI care were present in only a few countries, with wide variations across regions on the reported availability and access to care guidelines. The presence of CKD and AKI advocacy groups was reported as limited in most regions and was more common for AKI than for CKD, with more than two-thirds of countries reporting absence of capacity to participate in clinical research.
The status of kidney health care as suggested by this study indicates that the health systems of many countries face substantial challenges in closing the large gaps that are reported to currently exist in meeting the health needs of people with AKI and CKD around the world. First, the reported limited availability of and public funding for AKI and CKD care (kidney replacement therapy technologies, essential medicines, service delivery and infrastructures, kidney disease detection), particularly in low- and lower middle–income countries, call for strategies at global, regional, and national levels to make these care components accessible and affordable to the burgeoning populace with kidney disease. While community-based kidney disease prevention, identification, and treatment programs represent an important low-cost strategy with the potential for significant public health benefits, the present study found that most countries reported inadequate CKD detection and surveillance systems to achieve this goal. For example, the ability to quantitatively measure serum creatinine with eGFR reporting and proteinuria even at secondary care levels was “always” possible in only 7 (21%) and 2 (6%) African countries, respectively. Furthermore, peritoneal dialysis tended to be relatively underutilized in resource-poor countries, even though this mode is generally considered a less expensive and technically less demanding form of kidney replacement therapy that is particularly suited to low- and lower–middle income countries challenged by limited finances, limited nephrology workforce, and geographical barriers. Developing low-cost kidney disease detection programs (integrated with other noncommunicable disease strategies) and low-cost dialysis programs in resource-limited settings requires building partnerships among industry, international health agencies, and governments, as occurred with the establishment of low-cost chronic disease management programs in Africa.
A second challenge is the limited availability of reliable surveillance systems reported for both AKI and CKD across countries and regions, which is a major impediment to designing and implementing effective interventions to close the identified gaps in infrastructures and services. Policy decisions at national and international levels are required to support development of functional information systems across the broad spectrum of kidney diseases and to track and monitor burden, treatment, and related outcomes.
A third key challenge is the limited workforce capacity reported in most countries and regions, especially dialysis nurses, laboratory workers, dietitians, transplant coordinators, and nephrologists. Because health care workforce availability is a prerequisite for effective AKI and CKD management programs and policies, the challenge of health care professional shortages will require a concerted response from major national and international stakeholders.
Fourth, the limited capacity reported in most regions and countries to undertake clinical research calls for more investment and a targeted research agenda to improve understanding of kidney disease burden, process of care, outcomes monitoring, and testing of novel interventions, particularly in low- and lower middle–income countries.
The key strengths of the GKHA Project were the development of the study protocol and survey instrument, which followed a well-validated conceptual framework assessing capacity for other chronic diseases based on the widely applied WHO health system building blocks. The survey had high external validity, involving 125 countries and including very good coverage across regions and income levels. Data were reviewed for accuracy and validity by regional and national stakeholders knowledgeable of the local context across regions and countries. Furthermore, the findings were corroborated and validated via triangulation with secondary data sources based on a review of published and other literature at country levels (provided by survey respondents and other sources). In addition, a future survey using similar methods may provide assessments of improvements or declines in global kidney health care status.
The GKHA Project and this study also have several limitations. The use of a questionnaire survey, although an important source of information, was potentially subjective and highly dependent on the knowledge, expertise, and perceptions of the respondents. Furthermore, there are no internationally agreed on or recommended benchmarks for health care workforce densities, and therefore, precise definition of what constitutes a health worker shortage is likely to vary considerably between different countries. The survey questions were limited to only face validity and were reliant on respondents answering fairly and representing the status of services in their country accurately. To address these potential problems, respondents with a range of kidney care knowledge, expertise, and regional representation were carefully selected in liaison with the ISN regional boards. There was potential for social desirability bias to have influenced some responses, which was mitigated by corroborating findings with regional leaders as well as secondary data sources. The study also did not take into account some important dimensions of health systems, such as quality, efficiency, accessibility, geographic distribution, and within-country heterogeneity (particularly between urban and rural regions).
Conclusions
This survey demonstrated significant interregional and intraregional variability in the current capacity for kidney care across the world, including important gaps in services and workforce. Assuming the responses accurately reflect the status of kidney care in the respondent countries, these findings may be useful to inform efforts to improve the quality of kidney care worldwide.
eFigure 1. Global Availability of Nephrology Workforce
eFigure 2. Availability of Renal Registries by Region
eFigure 3. Presence of Advocacy Group for Kidney Care
eTable 1. Assessment of Healthcare Infrastructure Available for Providing Kidney Care
eTable 2. In Your Opinion, Is There a Shortage of Any of the Following Providers in Your Country? (By Region)
eTable 3. Does Your Country Have a National Strategy for Improving the Care of CKD Patients?
eTable 4. Does Your Country Have a National Strategy for Improving the Identification of AKI?
eTable 5. Access to Clinical Practice Guidelines for Kidney Care
eTable 6. Capacity and Availability of Regulatory Framework for Clinical Research
eAppendix 1. Study Questionnaire
eAppendix 2. Access to RRT, Medication Funding and Workforce Capacity
eAppendix 3. Services for CKD Care, Information Systems, Advocacy Structures, and Capacity for Clinical Trials
References
- 1.Bello AK, Levin A, Manns BJ, et al. ; Kidney Health for Life Initiative . Effective CKD care in European countries: challenges and opportunities for health policy. Am J Kidney Dis. 2015;65(1):15-25. [DOI] [PubMed] [Google Scholar]
- 2.Radhakrishnan J, Remuzzi G, Saran R, et al. ; CDC-CKD Surveillance Team; European CKD Burden Consortium; CKD.QLD Group . Taming the chronic kidney disease epidemic: a global view of surveillance efforts. Kidney Int. 2014;86(2):246-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Couser WG, Remuzzi G, Mendis S, Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80(12):1258-1270. [DOI] [PubMed] [Google Scholar]
- 4.Palmer S, Vecchio M, Craig JC, et al. Prevalence of depression in chronic kidney disease: systematic review and meta-analysis of observational studies. Kidney Int. 2013;84(1):179-191. [DOI] [PubMed] [Google Scholar]
- 5.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296-1305. [DOI] [PubMed] [Google Scholar]
- 6.Wang HE, Gamboa C, Warnock DG, Muntner P. Chronic kidney disease and risk of death from infection. Am J Nephrol. 2011;34(4):330-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levey AS, de Jong PE, Coresh J, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011;80(1):17-28. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland: WHO Press; 2014. [Google Scholar]
- 9.Huffman MD, Perel P, Beller GA, et al. World Heart Federation Emerging Leaders Program: an innovative capacity building program to facilitate the 25 × 25 goal. Glob Heart. 2015;10(4):229-233. [DOI] [PubMed] [Google Scholar]
- 10.Moran AE, Roth GA, Narula J, Mensah GA. 1990-2010 Global Cardiovascular Disease Atlas. Glob Heart. 2014;9(1):3-16. [DOI] [PubMed] [Google Scholar]
- 11.Perico N, Remuzzi G. Acute kidney injury in poor countries should no longer be a death sentence: the ISN “0 by 25” Project. Ann Nutr Metab. 2015;66(suppl 3):42-44. [DOI] [PubMed] [Google Scholar]
- 12.Sacco RL, Roth GA, Reddy KS, et al. The heart of 25 by 25: achieving the goal of reducing global and regional premature deaths from cardiovascular diseases and stroke: a modeling study from the American Heart Association and World Heart Federation. Circulation. 2016;133(23):e674-e690. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization Universal Health Coverage: Supporting Country Needs http://www.who.int/contracting/UHC_Country_Support.pdf. Accessed April 14, 2017.
- 14.Guariguata L, Whiting D, Weil C, Unwin N. The International Diabetes Federation Diabetes Atlas methodology for estimating global and national prevalence of diabetes in adults. Diabetes Res Clin Pract. 2011;94(3):322-332. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Geneva, Switzerland: WHO Press; 2010. [Google Scholar]
- 16.Leowski J, Krishnan A. Capacity to control noncommunicable diseases in the countries of South-East Asia. Health Policy. 2009;92(1):43-48. [DOI] [PubMed] [Google Scholar]
- 17.Chapman AL, Hadfield M, Chapman CJ. Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb. 2015;45(3):201-205. [DOI] [PubMed] [Google Scholar]
- 18.Stevens GA, Alkema L, Black RE, et al. ; GATHER Working Group . Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet. 2016;388(10062):e19-e23. [DOI] [PubMed] [Google Scholar]
- 19.Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382(9888):260-272. [DOI] [PubMed] [Google Scholar]
- 20.White SL, Chadban SJ, Jan S, Chapman JR, Cass A. How can we achieve global equity in provision of renal replacement therapy? Bull World Health Organ. 2008;86(3):229-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teerawattananon Y, Luz A, Pilasant S, et al. How to meet the demand for good quality renal dialysis as part of universal health coverage in resource-limited settings? Health Res Policy Syst. 2016;14:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jha V, Arici M, Collins AJ, et al. Understanding kidney care needs and implementation strategies in low- and middle-income countries: conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int. 2016;90(6):1164-1174. [DOI] [PubMed] [Google Scholar]
- 23.Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015;313(8):837-846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson DW, Atai E, Chan M, et al. ; KHA-CARI . KHA-CARI guideline: early chronic kidney disease: detection, prevention and management. Nephrology (Carlton). 2013;18(5):340-350. [DOI] [PubMed] [Google Scholar]
- 25.Wouters OJ, O’Donoghue DJ, Ritchie J, Kanavos PG, Narva AS. Early chronic kidney disease: diagnosis, management and models of care. Nat Rev Nephrol. 2015;11(8):491-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karopadi AN, Mason G, Rettore E, Ronco C. Cost of peritoneal dialysis and haemodialysis across the world. Nephrol Dial Transplant. 2013;28(10):2553-2569. [DOI] [PubMed] [Google Scholar]
- 27.Pearce N, Ebrahim S, McKee M, et al. Global prevention and control of NCDs: limitations of the standard approach. J Public Health Policy. 2015;36(4):408-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Katz IJ, Gerntholtz T, Naicker S. Africa and nephrology: the forgotten continent. Nephron Clin Pract. 2011;117(4):c320-c327. [DOI] [PubMed] [Google Scholar]
- 29.Nuño R, Coleman K, Bengoa R, Sauto R. Integrated care for chronic conditions: the contribution of the ICCC Framework. Health Policy. 2012;105(1):55-64. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization Health Metrics Network: Framework and Standards for Country Health Information Systems. 2nd ed Geneva, Switzerland: WHO Press; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Global Availability of Nephrology Workforce
eFigure 2. Availability of Renal Registries by Region
eFigure 3. Presence of Advocacy Group for Kidney Care
eTable 1. Assessment of Healthcare Infrastructure Available for Providing Kidney Care
eTable 2. In Your Opinion, Is There a Shortage of Any of the Following Providers in Your Country? (By Region)
eTable 3. Does Your Country Have a National Strategy for Improving the Care of CKD Patients?
eTable 4. Does Your Country Have a National Strategy for Improving the Identification of AKI?
eTable 5. Access to Clinical Practice Guidelines for Kidney Care
eTable 6. Capacity and Availability of Regulatory Framework for Clinical Research
eAppendix 1. Study Questionnaire
eAppendix 2. Access to RRT, Medication Funding and Workforce Capacity
eAppendix 3. Services for CKD Care, Information Systems, Advocacy Structures, and Capacity for Clinical Trials