This population-based survey study examines changes in the lifetime prevalence, patterns, and associated demographics of heroin use and use disorder from 2001-2002 to 2012-2013 among the nationally representative respondents to the Epidemiologic Survey on Alcohol and Related Conditions.
Key Points
Question
Did a change occur in the prevalence, course, and associated demographics of heroin use and heroin use disorder from 2001-2002 to 2012-2013?
Findings
In this population-based survey study of 79 402 respondents, the prevalence of heroin use (1.61% vs 0.33%) and related disorder (0.69% vs 0.21%) was significantly higher in 2012-2013 than in 2001-2002, with greater increases among white individuals. The proportion of individuals reporting initiation of nonmedical use of prescription opioids before heroin use increased across time among white users only.
Meaning
The use of prescription opioids may have contributed to the greater increase in the prevalence of heroin use and related disorder observed among white individuals.
Abstract
Importance
Heroin use is an urgent concern in the United States. Little is know about the course of heroin use, heroin use disorder, and associated factors.
Objective
To examine changes in the lifetime prevalence, patterns, and associated demographics of heroin use and use disorder from 2001-2002 to 2012-2013 in 2 nationally representative samples of the US adult general population.
Design, Setting, and Participants
This survey study included data from 43 093 respondents of the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) and 36 309 respondents of the 2012-2013 NESARC-III. Data were analyzed from February 2 to September 15, 2016.
Main Outcomes and Measures
Lifetime heroin use and DSM-IV heroin use disorder.
Results
Among the 79 402 respondents (43.3% men; 56.7% women; mean [SD] age, 46.1 [17.9] years), prevalence of heroin use and heroin use disorder significantly increased from 2001-2002 to 2012-2013 (use: 0.33% [SE, 0.03%] vs 1.6% [SE, 0.08%]; disorder: 0.21% [SE, 0.03%] vs 0.69% [SE, 0.06%]; P < .001). The increase in the prevalence of heroin use was significantly pronounced among white (0.34% [SE, 0.04%] in 2001-2002 vs 1.90% [SE, 0.12%] in 2012-2013) compared with nonwhite (0.32% [SE, 0.05%] in 2001-2002 vs 1.05% [SE, 0.10%] in 2012-2013; P < .001) individuals. The increase in the prevalence of heroin use disorder was more pronounced among white individuals (0.19% [SE, 0.03%] in 2001-2002 vs 0.82% [SE, 0.08%] in 2012-2013; P < .001) and those aged 18 to 29 (0.21% [SE, 0.06%] in 2001-2002 vs 1.0% [0.17%] in 2012-2013; P = .01) and 30 to 44 (0.20% [SE, 0.04%] in 2001-2002 vs 0.77% [0.10%] in 2012-2013; P = .03) years than among nonwhite individuals (0.25% [SE, 0.04%] in 2001-2002 vs 0.43% [0.07%] in 2012-2013) and older adults (0.22% [SE, 0.04%] in 2001-2002 vs 0.51% [SE, 0.07%] in 2012-2013). Among users, significant differences were found across time in the proportion of respondents meeting DSM-IV heroin use disorder criteria (63.35% [SE, 4.79%] in 2001-2001 vs 42.69% [SE, 2.87%] in 2012-2013; P < .001). DSM-IV heroin abuse was significantly more prevalent among users in 2001-2002 (37.02% [SE, 4.67%]) than in 2012-2013 (19.19% [SE, 2.34%]; P = .001). DSM-IV heroin dependence among users was similar in 2001-2002 (28.22% [SE, 3.95%]) and in 2012-2013 (25.02% [SE, 2.20%]; P = .48). The proportion of those reporting initiation of nonmedical use of prescription opioids before initiating heroin use increased across time among white individuals (35.83% [SE, 6.03%] in 2001-2002 to 52.83% [SE, 2.88%] in 2012-2013; P = .01).
Conclusions and Relevance
The prevalence of heroin use and heroin use disorder increased significantly, with greater increases among white individuals. The nonmedical use of prescription opioids preceding heroin use increased among white individuals, supporting a link between the prescription opioid epidemic and heroin use in this population. Findings highlight the need for educational campaigns regarding harms related to heroin use and the need to expand access to treatment in populations at increased risk for heroin use and heroin use disorder.
Introduction
Heroin is an urgent concern in the United States.1,2 Risks associated with heroin use and addiction include mortality,3,4 overdose,1,5,6 infectious diseases,1,7 and impaired psychological status and social relationships.8 Increases in serious consequences of heroin use, including overdoses,9 emergency department visits,10 and public drug abuse treatment,11 have led to widespread concerns about a heroin epidemic.6 Although studies have addressed the link between use of prescription opioids (POs) and heroin,1,2,12,13,14,15 most information on trends in US adult heroin use is indirect, obtained through studies of its sequelae.10,11
Studies of trends in the consequences of heroin use, such as overdoses, are important. However, these studies do not provide information about underlying trends in the population burdens of heroin use and related disorders in US adults or in the characteristics and patterns of use among heroin users. For such trends, national survey data are needed. The National Survey on Drug Use and Health (NSDUH) is a potential source of such information. However, other than brief summaries,1,16,17 little has been published from NSDUH on trends in heroin use. Apart from the NSDUH, no studies known to us have addressed time trends in heroin consumption among US representative samples, including change over time in the prevalence of lifetime heroin use and heroin use disorders overall or patterns and characteristics of heroin use and related disorders among users (eg, age at onset, use frequency, disorder severity, types of abuse, or dependence symptoms endorsed). Using US adult national surveys conducted during 2001-2002 and 2012-2013, we addressed the following questions. First, did prevalence of lifetime heroin use and related disorders increase? Second, did demographic characteristics associated with lifetime heroin use and heroin use disorders change? Third, did patterns, severity, and substance comorbidity of heroin use and related disorders change?
Methods
Study Design and Participants
We obtained data from the following 2 nationally representative face-to-face household surveys of adults 18 years and older residing in households and group quarters18,19: the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (n = 43 093), and the 2012-2013 NESARC-III (n = 36 309). NESARC and NESARC-III used similar multistage probability sampling designs with oversampling for Hispanic, black, and (in NESARC-III) Asian individuals.19,20,21 Survey weights were used to adjust for differential probabilities of participant selection and household and person-level nonresponse and adjusted sample margins to match key demographic distributions (eg, age, sex, and race) of each target population.19,22 NESARC and NESARC-III used computer-assisted interviews and highly trained interviewers. Response rates in NESARC (60.1%) and NESARC-III (81.0%) were comparable to those of other national surveys.23,24 Interviewer quality assurance methods were similar across surveys.22 The US Census Bureau and US Office of Management and Budget conducted a full ethical review and approved all protocols and study consent procedures for 2001-2002 NESARC. The 2012-2013 NESARC-III protocols and study consent procedures were approved by the institutional review boards of Westat and the National Institutes of Health. Respondents gave written informed consent and were compensated for participation.
Assessments
Heroin Use and DSM-IV Use Disorder
The National Institute on Alcohol Abuse and Alcoholism Alcohol Use Disorder and Associated Disabilities Interview Schedule IV (AUDADIS-IV), a fully structured diagnostic interview designed for use by nonclinician interviewers after structured training, was used to assess substance use and psychiatric disorders according to DSM-IV criteria. In NESARC-III, the AUDADIS-5 was used to assess substance use and DSM-IV25 and DSM-526 criteria for substance use disorders.
Lifetime heroin use (ever vs never used heroin) was measured in both surveys and was included as a binary (yes or no) variable in our analyses. The reliability and validity of AUDADIS DSM-IV substance use disorder diagnoses have been well documented.27,28,29,30,31,32,33,34,35,36,37,38,39,40 We combined abuse and dependence because the criteria reflect a single disorder rather than 2 conditions.41 Symptom items (n = 30) that assessed DSM-IV heroin use disorder (abuse and dependence) in the NESARC and NESARC-III were virtually identical. However, 4 items were slightly reworded and 1 abuse item appeared in the NESARC but not the NESARC-III, whereas a different abuse item appeared in the NESARC-III but not the NESARC. Comparisons between DSM-IV heroin use disorder diagnoses with and without the additional questions yielded virtually identical prevalences (NESARC: 0.69% vs 0.68%; NESARC-III: 0.21% vs 0.21%), with corresponding near perfect or perfect concordance (κ = 0.998 and κ = 1.00, respectively), suggesting that these trivial differences could not account for the substantial differences in prevalence between the surveys.
Patterns of Heroin Use
Variables included age at first use, period of use (before the past 12 months only, past 12 months only, or both periods) and frequency of use during the heaviest-use period (every day or nearly every day or other). Heroin use disorder included use disorder overall, abuse, dependence, the abuse and dependence criteria, driving under the influence of heroin, and the number of lifetime heroin disorder criteria (0-1, 2-3, 4-5, and ≥6).
Other Substance Use
Lifetime use of other substances (sedatives or tranquilizers, stimulants, marijuana, cocaine or crack, hallucinogens, inhalants, POs, and other substances) on one’s own was included and measured identically across surveys. Because PO use is of special interest, we created a variable indicating whether nonmedical PO (NMPO) use among heroin users was initiated before heroin use.
Demographic Data
Demographic characteristics, measured identically across surveys, included sex (male or female), age (18-29, 30-44, or ≥45 years), educational level (less than high school, high school, or some college or more), race/ethnicity (non-Hispanic white vs nonwhite [non-Hispanic black, Hispanic, Asian or Pacific Islander, or Native American]), marital status (unmarried; married or living as married; or widowed, separated, or divorced), urbanicity (in metropolitan statistical areas or other), region (Northeast, Midwest, South, or West, coded according to US Census definitions based on the location of participants’ residences), and federal poverty level (<100% [below poverty level], 100%-200%, and >200%). Federal poverty level was determined by family income and size and by federal poverty guidelines.42
Statistical Analysis
Data were analyzed from February 2 to September 15, 2016. We combined NESARC and NESARC-III data to conduct repeated cross-sectional analyses, as was done previously to examine other trends in these surveys.22,43,44 We added a variable representing the survey from which the participant was included. Weighted prevalences were produced for full samples and by subgroups.
We conducted 3 sets of analyses. First, using separate models for each heroin outcome (lifetime use or lifetime use disorder) to estimate whether prevalences differed between surveys, we modeled survey year as associated with the outcome. Second, with logistic regression models, we tested associations between demographic variables and heroin use or heroin use disorder. Then, to test whether associations between demographic characteristics and the outcomes differed between surveys, we added an interaction term between the survey year and each demographic variable to all models. To assess differential associations on the prevalence scale, we first estimated prevalence differences between strata of the demographic variables (eg, male and female respondents) within each survey. We tested whether these prevalence differences differed between surveys (eg, male and female respondents in NESARC vs male and female respondents in NESARC-III) using pairwise t tests for independent samples. We estimated these prevalences and their SEs from model-predicted log-odds, back-transformed to the prevalence scale.45
Third, we estimated the distributions of variables corresponding to various aspects of severity and patterns of heroin use among heroin users in each survey. To test whether these distributions differed significantly between survey years, we used Wald χ2 tests (categorical variables) or Wald F tests (continuous variables), with P < .05 indicating significance. We used SUDAAN software (version 11.0.1)46 to incorporate the weights and complex design features of the surveys. Unless otherwise indicated, data are expressed as prevalence (SE).
Results
Lifetime Heroin Use, Heroin Use Disorder, and Demographic Characteristics
The sample included 79 402 respondents (43.3% men; 56.7% women; mean [SD] age, 46.1 [17.9] years) of the NESARC and NESARC-III. Lifetime prevalence of heroin use increased from 2001-2002 (0.33% [0.03%]) to 2012-2013 (1.61% [0.08%]) overall and among all subgroups: 18 to 29 years of age (0.26% [0.07%] to 1.81% [0.21%]; P = .09), 30 to 44 years of age (0.36% [0.06%] to 1.75% [0.17%]; P = .21), and 45 years or older (0.35% [0.05%] to 1.46% [0.11%]). Past-year prevalence of heroin use also increased from 2001-2002 (0.03% [0.01%) to 2012-2013 (0.21% [0.03%]; P < .001).
Lifetime prevalence of heroin use disorder increased significantly from 2001-2002 (0.21% [0.03%]) to 2012-2013 (0.69% [0.06%]) overall and among all subgroups: 18 to 29 years of age (0.21% [0.06%] to 1.01% [0.17%]; P = .01), 30 to 44 years of age (0.20% [0.04%] to 0.77% [0.10%]; P = .03), and 45 years or older (0.22% [0.04%] to 0.51% [0.07%]). Increases in use and use disorder remained significant between surveys when adjusted by lifetime NMPO. Among men, prevalence of heroin use (0.52% [0.05%] to 2.41% [0.15%]) and use disorder (0.32% [0.04%] to 1.04% [0.11%]) increased more than among women (0.16% [0.03%] to 0.86% [0.07%] and 0.11% [0.03%] to 0.36% [0.40%], respectively; P < .001). In 2001-2002, white and nonwhite individuals had similar prevalences of heroin use (0.34% [0.04%] and 0.32% [0.05%], respectively); in 2012-2013, heroin use was significantly higher among white (1.90% [0.12%]) than nonwhite (1.05% [0.10%]; P < .001) individuals. Heroin use and use disorder increased more among previously married (0.48% [0.08%] to 2.33% [0.19%]; P < .001; and 0.30% [0.06%] to 0.88% [0.10%]; P = .01; respectively) and unmarried (0.51% [0.09%] to 2.29% [0.21%] and 0.38% [0.08%] to 1.30% [0.17%], respectively) than among married (0.23% [0.04%] to 1.10% [0.10%]; P < .001; and 0.13% [0.03%] to 0.38% [0.06%]; P = .002 respectively) respondents. Similar findings were observed among those with educational levels of less than high school (0.41% [0.09%] to 2.01% [0.23%]; P = .03; and 0.24% [0.07%] to 0.87% [0.16%]; P = .08; respectively) and no more than high school (0.39% [0.07%] to 2.15% [0.19%]; P = .003; and 0.29% [0.06%] to 1.11% [0.14%]; P = .003; respectively) compared with those who attained higher educational levels (0.28% [0.04%] to 1.30% [0.10%] and 0.16% [0.03%] to 0.47% [0.06%], respectively). For heroin use only, prevalence significantly increased among respondents at less than 100% of the federal poverty level (0.44% [0.11%] to 2.42% [0.22%]; P < .001) and those at 100% to 200% of the poverty level (0.42% [0.08%] to 1.95% [0.18%]; P = .008) compared with those not in poverty (0.28% [0.03%] to 1.22% [0.10%]) (Figure 1, Table 1, Table 2, and eTables 1 and 2 in the Supplement).
Figure 1. Lifetime Heroin Use in the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) and the 2012-2013 NESARC-III.
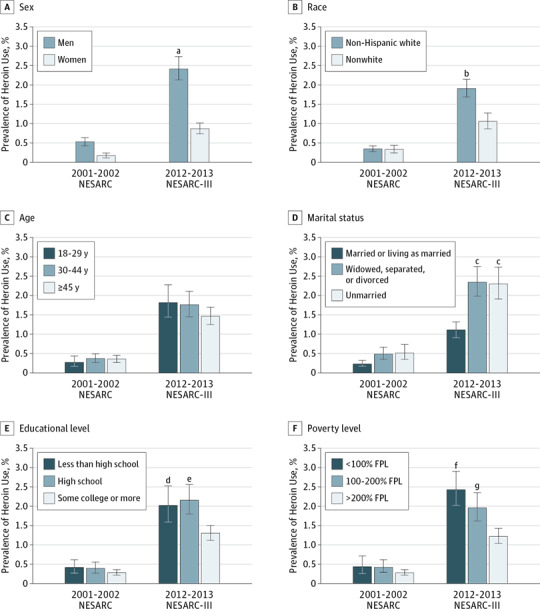
Differences in prevalences across variable categories in NESARC are compared with differences in prevalences in NESARC-III. FPL indicates federal poverty level. Error bars indicate 95% CIs.
aP < .001, compared with women.
bP < .001, compared with nonwhite.
cP < .001, compared with married or living as married.
dP = .03, compared with some college or more.
eP = .003, compared with some college or more.
fP < .001, compared with greater than 200% FPL.
gP = .008, compared with greater than 200% FPL.
Table 1. Heroin Use and Demographic Correlates in the 2001-2002 NESARC and the 2012-2013 NESARC-III.
| Variable | Unadjusted Lifetime Heroin Use | ||||
|---|---|---|---|---|---|
| 2001-2002 NESARC (n = 43 093) |
2012-2013 NESARC-III (n = 36 309) |
P Valuea | |||
| Prevalence (SE), % | PD (SE), % | Prevalence (SE), % | PD (SE), % | ||
| Overall | 0.33 (0.03) | NA | 1.61 (0.08) | NA | NA |
| Sex | |||||
| Male | 0.52 (0.05) | 0.36 (0.06) | 2.41 (0.15) | 1.55 (0.17) | <.001 |
| Female | 0.16 (0.03) | 1 [Reference] | 0.86 (0.07) | 1 [Reference] | 1 [Reference] |
| Race/ethnicity | |||||
| Non-Hispanic white | 0.34 (0.04) | 0.02 (0.06) | 1.90 (0.12) | 0.85 (0.17) | <.001 |
| Nonwhiteb | 0.32 (0.05) | 1 [Reference] | 1.05 (0.10) | 1 [Reference] | 1 [Reference] |
| Age, y | |||||
| 18-29 | 0.26 (0.07) | −0.09 (0.08) | 1.81 (0.21) | 0.35 (0.24) | .09 |
| 30-44 | 0.36 (0.06) | 0.01 (0.08) | 1.75 (0.17) | 0.29 (0.21) | .21 |
| ≥45 | 0.35 (0.05) | 1 [Reference] | 1.46 (0.11) | 1 [Reference] | 1 [Reference] |
| Marital status | |||||
| Married or living as married | 0.23 (0.04) | 1 [Reference] | 1.10 (0.10) | 1 [Reference] | 1 [Reference] |
| Widowed, separated, or divorced | 0.48 (0.08) | 0.25 (0.09) | 2.33 (0.19) | 1.23 (0.22) | <.001 |
| Unmarried | 0.51 (0.09) | 0.28 (0.10) | 2.29 (0.21) | 1.19 (0.25) | <.001 |
| Educational level | |||||
| Less than high school | 0.41 (0.09) | 0.12 (0.10) | 2.01 (0.23) | 0.71 (0.25) | .03 |
| High school | 0.39 (0.07) | 0.11 (0.08) | 2.15 (0.19) | 0.85 (0.23) | .003 |
| Some college or more | 0.28 (0.04) | 1 [Reference] | 1.30 (0.10) | 1 [Reference] | 1 [Reference] |
| Poverty levelc | |||||
| <100% FPL | 0.44 (0.11) | 0.16 (0.12) | 2.42 (0.22) | 1.20 (0.26) | <.001 |
| 100%-200% FPL | 0.42 (0.08) | 0.14 (0.09) | 1.95 (0.18) | 0.74 (0.20) | .008 |
| >200% FPL | 0.28 (0.03) | 1 [Reference] | 1.22 (0.10) | 1 [Reference] | 1 [Reference] |
| Urbanicity | |||||
| Rural | 0.23 (0.07) | 1 [Reference] | 1.28 (0.18) | 1 [Reference] | 1 [Reference] |
| Urban | 0.36 (0.04) | 0.12 (0.08) | 1.70 (0.09) | 0.42 (0.20) | .17 |
| Region | |||||
| Northeast | 0.38 (0.09) | 1 [Reference] | 1.54 (0.21) | 1 [Reference] | 1 [Reference] |
| Midwest | 0.22 (0.05) | −0.16 (0.10) | 1.54 (0.19) | 0 (0.28) | .59 |
| South | 0.32 (0.05) | −0.06 (0.10) | 1.60 (0.13) | 0.06 (0.24) | .66 |
| West | 0.42 (0.07) | 0.05 (0.11) | 1.74 (0.14) | 0.21 (0.25) | .57 |
Abbreviations: FPL, federal poverty level; NA, not applicable; NESARC, National Epidemiologic Survey on Alcohol and Related Conditions; PD, prevalence difference.
Calculated as the difference in PDs (back-transformed from predicted marginal log-odds).
Nonwhite includes non-Hispanic black, Hispanic, Asian or Pacific Islanders, or Native American.
Determined by family income and family size using the federal poverty guidelines published annually by the US Department of Health and Human Services. Individuals or families making less than 100% of the FPL are considered to be below the poverty level.
Table 2. DSM-IV Heroin Use Disorder and Demographic Correlates in the 2001-2002 NESARC and the 2012-2013 NESARC-III.
| Variable | Unadjusted Lifetime DSM-IV Heroin Use Disordera | ||||
|---|---|---|---|---|---|
| 2001-2002 NESARC (n = 43 093) |
2012-2013 NESARC-III (n = 36 309) |
P Valueb | |||
| Prevalence, (SE), % | PD (SE), % | Prevalence (SE), % | PD (SE), % | ||
| Overall | 0.21 (0.03) | NA | 0.69 (0.06) | NA | NA |
| Sex | |||||
| Male | 0.32 (0.04) | 0.21 (0.05) | 1.04 (0.11) | 0.68 (0.12) | <.001 |
| Female | 0.11 (0.03) | 1 [Reference] | 0.36 (0.04) | 1 [Reference] | 1 [Reference] |
| Race | |||||
| Non-Hispanic white | 0.19 (0.03) | −0.06 (0.05) | 0.82 (0.08) | 0.38 (0.11) | <.001 |
| Nonwhite | 0.25 (0.04) | 1 [Reference] | 0.43 (0.07) | 1 [Reference] | 1 [Reference] |
| Age, y | |||||
| 18-29 | 0.21 (0.06) | −0.01 (0.07) | 1.01 (0.17) | 0.49 (0.19) | .01 |
| 30-44 | 0.20 (0.04) | −0.02 (0.05) | 0.77 (0.10) | 0.25 (0.11) | .03 |
| ≥45 | 0.22 (0.04) | 1 [Reference] | 0.51 (0.07) | 1 [Reference] | 1 [Reference] |
| Marital status | |||||
| Married or living as married | 0.13 (0.03) | 1 [Reference] | 0.38 (0.06) | 1 [Reference] | 1 [Reference] |
| Widowed, separated, or divorced | 0.30 (0.06) | 0.18 (0.06) | 0.88 (0.10) | 0.50 (0.11) | .01 |
| Unmarried | 0.38 (0.08) | 0.25 (0.09) | 1.30 (0.17) | 0.92 (0.19) | .002 |
| Educational level | |||||
| Less than high school | 0.24 (0.07) | 0.08 (0.07) | 0.87 (0.16) | 0.40 (0.16) | .08 |
| High school | 0.29 (0.06) | 0.12 (0.07) | 1.11 (0.14) | 0.64 (0.16) | .003 |
| Some college or more | 0.16 (0.03) | 1 [Reference] | 0.47 (0.06) | 1 [Reference] | 1 [Reference] |
| Poverty levelc | |||||
| <100% FPL | 0.40 (0.11) | 0.25 (0.11) | 1.14 (0.16) | 0.64 (0.17) | .05 |
| 100%-200% FPL | 0.26 (0.06) | 0.11 (0.06) | 0.79 (0.12) | 0.29 (0.12) | .19 |
| >200% FPL | 0.15 (0.03) | 1 [Reference] | 0.50 (0.06) | 1 [Reference] | 1 [Reference] |
| Urbanicity | |||||
| Rural | 0.13 (0.04) | 1 [Reference] | 0.53 (0.12) | 1 [Reference] | 1 [Reference] |
| Urban | 0.23 (0.03) | 0.11 (0.05) | 0.73 (0.06) | 0.19 (0.13) | .53 |
| Region | |||||
| Northeast | 0.25 (0.08) | 1 [Reference] | 0.77 (0.15) | 1 [Reference] | 1 [Reference] |
| Midwest | 0.14 (0.04) | −0.11 (0.09) | 0.71 (0.13) | −0.05 (0.20) | .78 |
| South | 0.23 (0.04) | −0.02 (0.09) | 0.71 (0.09) | −0.06 (0.18) | .84 |
| West | 0.22 (0.05) | −0.03 (0.09) | 0.57 (0.11) | −0.20 (0.19) | .43 |
Abbreviations: FPL, federal poverty level; NA, not applicable; NESARC, National Epidemiologic Survey on Alcohol and Related Conditions; PD, prevalence difference.
DSM-IV heroin use disorder refers to DSM-IV drug abuse or dependence.
Calculated as the difference in PDs (back-transformed from predicted marginal log-odds).
Determined by family income and family size using the federal poverty guidelines published annually by the US Department of Health and Human Services. Individuals or families making <100% of the FPL are considered to be below the poverty level.
Lifetime Heroin Use Disorders and Heroin Use Patterns Among Lifetime Users
Lifetime prevalence of heroin use disorder among users decreased significantly from 2001-2002 (63.35% [4.79%]) to 2012-2013 (42.69% [2.87%]; P < .001). Although the prevalence of dependence and most of its criteria were stable across both surveys, DSM-IV heroin abuse was significantly less prevalent among users in 2012-2013 (19.19% [2.34%]) than in 2001-2002 (37.02% [4.67%]; P = .001), as were all 4 DSM-IV abuse criteria. These included role failure (21.40% [1.86%] vs 43.03% [4.89%]; P < .001), physically hazardous use (31.79% [2.54%] vs 47.46% [4.60%]; P = .005), legal problems (12.99% [1.91%] vs 23.58% [4.02%]; P = .02), and use persistence despite recurrent social problems (30.92% [2.50%] vs 52.10% [5.03%]; P < .001) (Figure 2 and Table 3).
Figure 2. DSM-IV Heroin Use Disorder in the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) and the 2012-2013 NESARC-III.
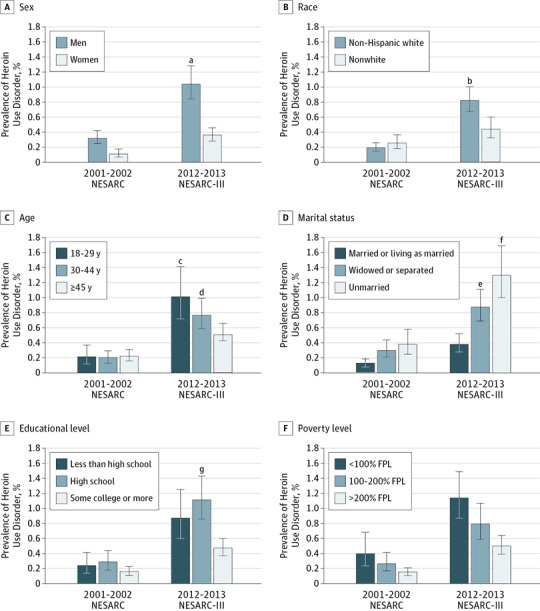
Differences in prevalences across variable categories in NESARC are compared with differences in prevalences in NESARC-III. Error bars indicate 95% CIs.
aP < .001, compared with women.
bP < .001, compared with nonwhite.
cP = .01, compared with 45 years or older.
dP = .03, compared with 45 years or older.
eP = .01, compared with married or living as married.
fP = .002, compared with married or living as married.
gP = .003, compared with some college or more.
Table 3. Patterns of Heroin Use Among Lifetime Heroin Users in the the 2001-2002 NESARC and the 2012-2013 NESARC-III.
| Variable | Prevalence (SE), %a | P Value | |
|---|---|---|---|
| 2001-2002 NESARC | 2012-2013 NESARC-III | ||
| Age at first use, mean (SD), y | 21.80 (0.67) | 22.82 (0.39) | .19 |
| Period of heroin use | |||
| Past 12 mo only | 2.02 (1.42) | 3.23 (1.11) | .52 |
| Before past 12 mo only | 90.73 (3.46) | 86.17 (2.18) | |
| Both | 7.24 (3.27) | 10.61 (1.84) | |
| Period of heroin use disorder | |||
| Past 12 mo only | 3.20 (2.25) | 2.18 (1.08) | .47 |
| Before past 12 mo only | 88.86 (5.20) | 83.02 (3.38) | |
| Both | 7.94 (4.85) | 14.80 (3.29) | |
| Frequency of heroin use in lifetime | |||
| No. of times | 1039.69 | 649.4 | .05 |
| 1-5 times | 38.97 (4.78) | 31.97 (2.25) | <.001 |
| 6-100 times | 9.91 (2.63) | 24.29 (2.17) | |
| >100 times | 51.12 (5.00) | 43.73 (2.45) | |
| Frequency of use during heaviest period | |||
| Daily | 36.35 (4.78) | 30.04 (2.51) | .35 |
| Less than daily but monthly or more | 22.61 (3.96) | 29.02 (2.72) | |
| Less than monthly | 41.04 (4.90) | 40.94 (2.72) | |
| Frequency of use during heaviest period | |||
| Daily or near daily | 39.11 (4.77) | 37.01 (2.45) | .70 |
| Less than daily or near daily | 60.89 (4.77) | 62.99 (2.45) | |
| DSM-IV heroin use disorderb | 63.35 (4.79) | 42.69 (2.87) | <.001 |
| Heroin abuse | 37.02 (4.67) | 19.19 (2.34) | .001 |
| Heroin dependence | 28.22 (3.95) | 25.02 (2.20) | .48 |
| DSM-IV heroin abuse criteria | |||
| Role failure | 43.03 (4.89) | 21.40 (1.86) | <.001 |
| Physically hazardous use | 47.46 (4.60) | 31.79 (2.54) | .005 |
| Legal problems | 23.58 (4.02) | 12.99 (1.91) | .02 |
| Use persistence despite recurrent social problems | 52.10 (5.03) | 30.92 (2.50) | <.001 |
| DSM-IV heroin dependence criteria | |||
| Tolerance | 35.96 (5.14) | 31.42 (2.62) | .43 |
| Withdrawal | 41.20 (4.98) | 31.35 (2.55) | .09 |
| Larger amounts or longer | 37.65 (5.04) | 26.14 (2.20) | .04 |
| Persistent intention to quit | 50.40 (5.06) | 41.93 (2.66) | .14 |
| Time spent obtaining | 42.05 (4.94) | 32.93 (2.48) | .10 |
| Social or occupational dysfunction | 34.22 (5.06) | 25.10 (2.15) | .10 |
| Use persistence despite physical health problems due to heroin | 38.48 (4.95) | 29.38 (2.21) | .10 |
| DSM-IV heroin use disorder, No. of criteriab | |||
| 0-1 | 39.83 (5.00) | 55.16 (2.82) | .03 |
| 2-3 | 10.09 (2.67) | 12.50 (1.91) | |
| 4-5 | 8.54 (2.67) | 5.53 (1.34) | |
| ≥6 | 41.53 (5.09) | 26.81 (2.28) | |
| Driving under the influence of heroin, among heroin users | 42.1 (4.7) | 28.9 (2.2) | .01 |
| No history of any other drug use, among heroin users | 0.0 (0.0) | 2.1 (0.70) | .003 |
| NMPO use | 68.9 (4.5) | 76.0 (2.2) | .15 |
| Frequency of use during heaviest use period | |||
| Daily or near daily | 21.93 (4.14) | 33.54 (2.47) | .25 |
| 1-4 d/wk | 22.32 (4.72) | 16.38 (2.11) | |
| 1-3 times per mo | 9.51 (2.88) | 11.22 (1.70) | |
| <1 time per mo | 15.06 (2.97) | 13.63 (1.79) | |
| Proportion of lifetime heroin users in categories of frequency of NMPO use during heaviest use period | |||
| Daily or near daily | 31.87 (5.64) | 44.59 (3.01) | .25 |
| 1-4 d/wk | 32.43 (6.26) | 22.37 (2.76) | |
| 1-3 times per mo | 13.81 (4.11) | 14.91 (2.19) | |
| <1 time per mo | 21.88 (4.30) | 18.12 (2.30) | |
| Order of initiation of use | |||
| Before heroin | 38.16 (5.05) | 46.98 (2.50) | .20 |
| After heroin | 12.14 (3.00) | 15.73 (1.67) | |
| Coincident with heroin or unknown | 18.61 (4.01) | 13.29 (1.90) | |
| Use before heroin | |||
| Among nonwhite respondents | 44.12 (7.60) | 26.20 (3.95) | .04 |
| Among white respondents | 35.83 (6.03) | 52.83 (2.88) | .01 |
Abbreviations: NESARC, National Epidemiologic Survey on Alcohol and Related Conditions; NMPO, nonmedical prescription opioid.
Prevalences and their SEs are weighted and take into account the complex survey designs of the NESARC and the NESARC-III.
DSM-IV heroin use disorder refers to DSM-IV drug abuse or dependence.
The proportion of heroin users who reported no history of any other drug use increased between surveys (0 in 2001-2002 vs 2.10% [0.66%] in 2012-2013; P = .003) (Table 3). The proportion of those who ever drove under the influence of heroin decreased between surveys (42.07% [4.69%] vs 28.90% [2.18%]; P = .01). The proportion of individuals experiencing remission in heroin use and use disorder was similar in the 2001-2002 and 2012-2013 surveys (use, 90.73% [3.46%] vs 86.17% [2.18%]; P = .52; disorder, 88.86% [5.20%] vs 83.02% [3.38%]; P = .47). Frequency of NMPO use among individuals who used heroin and POs in their lifetime did not differ between surveys. In race-stratified analyses, white individuals were more likely to have initiated NMPO use before heroin (35.83% [6.03%] in 2001-2002 and 52.83% [2.88] in 2012-2013; P = .01), whereas nonwhite individuals were less likely to have initiated NMPO use before heroin (44.12% [7.60%] in 2001-2002 and 26.20% [3.95%] in 2012-2013; P = .04). A greater proportion of heroin users used heroin more than 100 times in 2001-2002 (51.12% [5.00%]) than in 2012-2013 (43.73% [2.45%]; P < .001).
Discussion
In the 2012-2013 NESARC-III, 1.61% of US adults had ever used heroin, and 0.69% had ever met criteria for a heroin use disorder. Extrapolation from these results indicates that in 2012-2013, approximately 3 800 000 US adults used heroin at some point in their lifetime and approximately 1 615 000 US adults ever met criteria for lifetime heroin use disorder. Between the 2001-2002 NESARC and the 2012-2013 NESARC-III, the prevalence of lifetime heroin use increased almost 5-fold and the prevalence of lifetime heroin use disorder increased approximately 3-fold. The increase in the prevalence of lifetime heroin use disorder represented approximately 1 127 000 additional individuals with heroin use disorder in 2012 relative to 2001. Despite the decreased risk for heroin use disorder among users, the large increase in users led to an overall increased prevalence of heroin use disorder in the adult population.
The increases that we show in lifetime heroin use and use disorder are consistent with increases in heroin outcomes in several other studies during the same period. The NSDUH showed a 62.5% increase in the rates of heroin use and a 90% increase (from 1.0 to 1.9 per 1000 population) in the rates of past-year heroin use disorder.17 In addition, mortality associated with heroin overdoses increased 47 by 26% from 2000 to 2013-2014.48 Data from the Treatment Episode Data Sets show an increase in admissions due to heroin as the primary drug from 15% in 2003 to 19% in 2013.11 Our study expands on prior investigations by presenting change over time in the US national prevalence of lifetime heroin use and use disorders overall and among users by investigating patterns of use and characteristics associated with heroin use and related disorders.
Increases in heroin use and related disorders were particularly prominent among white individuals, leading to a significant race gap in lifetime heroin use by 2012-2013, consistent with other sources.17,49,50,51 In 2001-2002, only approximately one-third of white heroin users reported NMPO use before first using heroin, whereas in 2012-2013, more than half of white heroin users reported using NMPO before heroin. In contrast, fewer nonwhite users reported using POs before heroin in the 2012-2013 than in 2001-2002 periods. This demographic shift is parallel to increases in NMPOs use since 2002, which has occurred disproportionally among white individuals2,49,50,51 and could be attributed to the disparities in prescribing opioids to white patients, as shown in a meta-analysis.52 Increased availability and lower heroin prices in recent years may have contributed to increased heroin use.17,49,53,54 In the past decade, NMPO users have been at higher risk than nonusers for initiation of heroin use.51,55,56,57 We explored the association of lifetime heaviest frequency of NMPO use with the risk for heroin use in both surveys. Not surprisingly, the risk increased as frequency of NMPO use increased. However, the increase in the prevalence of heroin use occurred across NMPO use frequency categories in NESARC-III compared with NESARC, suggesting that factors other than increasingly frequent NMPO use contributed to the increase in heroin use in adults in the 2012-2013 period. Differential increases in lifetime heroin use among white adults persisted even after controlling for potential differential increases in lifetime NMPO use. Heroin use appears to have become more socially acceptable among suburban and rural white individuals, perhaps because its effects seem so similar to those of widely available POs.13 All these factors could contribute to increased prevalence of heroin use and use disorder among white users.
The sex gap in lifetime heroin use and use disorder widened from the 2001-2002 to 2012-2013 periods; use among men increased more than among women. Similar results were reported using NSDUH data.16,57 Changes in the heroin sex gap are consistent with those for marijuana.58,59 Changes in exposure to risk factors for heroin may explain the widening heroin sex gap. For example, men may have been more affected by economic stressors than women (eg, low manufacturing employment rates60 leading to greater increases in male heroin use).
Although heroin use is now more widespread among individuals of all socioeconomic strata (Table 1 and eTable 1 in the Supplement) and among those with stronger bonds to social institutions,61 relative increases in heroin use and use disorder across time were greater among less educated and poorer individuals. These trends are concerning because increases in the prevalence of heroin use and use disorder have been occurring among vulnerable individuals who have few resources to overcome problems associated with use.62,63 No differences in prevalence of heroin use were found by age. However, in NESARC-III, the prevalence of heroin use disorders was significantly higher among younger than older aged (≥45 years) groups.
The proportion of heroin users with a lifetime heroin use disorder decreased between the 2 surveys, primarily owing to decreases in DSM-IV abuse criteria. Some subgroups of heroin users (those with greater resources and infrequent users) might be less likely to develop milder abuse symptoms. However, if the prevalence of heroin use continues to increase, the numbers of those with heroin use disorders will likely increase as well.
No NESARC participants and 2.1% of NESARC-III participants reported that heroin was the only illicit drug they had used. Although this result may seem surprising, it is consistent with reports that some individuals transition from use of POs to heroin with no history of other drug use besides POs.49
Limitations and Strengths
NESARC and NESARC-III lacked biological testing for substances and excluded homeless and incarcerated individuals. Including these populations would likely increase the overall prevalence of heroin use and use disorder.64,65 Because overall66 and drug-related67,68 adult incarceration rates did not increase during the decade between surveys, they should be comparable in covering heroin users in the adult general population, and reports of time trends are unlikely to be biased. The AUDADIS-5 interviewers were not clinicians, but a NESARC-III validation substudy comparing AUDADIS and clinician diagnoses of lifetime heroin use disorder showed nearly identical prevalence and good concordance.69 The NESARC-III response rate was acceptable (60.1%) but lower than the NESARC rate (81.0%). Weighting that compensated for nonresponse facilitated comparisons between the surveys. Surveys with lower response rates may miss more substance abusers,70 potentially leading to lower prevalence. If this occurred in NESARC-III, the NESARC and NESARC-III differences reported herein may underestimate the true differences. In addition, employers of NESARC and NESARC-III interviewers were different (Census and Westat, respectively); whether this difference affected participant responses is unknown. However, NESARC and NESARC-III were presented to respondents as voluntary surveys conducted under the auspices of the US government, possibly mitigating this difference. The validity of increases shown between NESARC and NESARC-III is supported by their coherence with the other aforementioned studies, which show increases in heroin-related variables during the same period (eg, overdoses, treatment). Also, the study did not examine NESARC and NESARC-III differences by DSM-5 severity levels. The DSM-5 heroin use disorder criteria, published in 2013, were not known in 2001, and not all DSM-5 criteria were included in the 2001-2002 NESARC. Finally, NESARC surveys only provide assessments at 2 points, and we do not have information on fluctuations and trends in heroin use and related disorder between both periods.
We focused on associations with lifetime use, lifetime disorder, and patterns of lifetime disorder across time, which are important population parameters, particularly for very rare conditions such as heroin outcomes in the general population. For very rare conditions (eg, any heroin outcome in the general population), examining lifetime cases may be the only way to determine demographic and clinical correlates and patterns of use during the life course, which simply cannot be estimated from small numbers of survey participants with current heroin use or use disorders. Furthermore, lifetime heroin use prevalence represents the burden on a population of a highly risky behavior for which sequelae often persist even after cessation of use of that particular drug.
Limitations are balanced by numerous strengths, including use of AUDADIS in both surveys and assessment of more than 79 000 participants. Study data provide unique information on time trends during a period when changes associated with heroin use patterns occurred (eg, increase in white users, lower prevalence of heroin use disorder in recent years).13,49 Study findings provide context for further investigation of how demographic, clinical, and other risk factors for heroin use and heroin use disorders may have changed over time. Continued monitoring of such time trends is an important public health priority.
Conclusions
The prevalences of heroin use and use disorder have increased significantly in the US adult general population since the beginning of this millennium. Of note, increases have been greatest among men, white individuals, those with low income and educational levels, and, for heroin use disorder, younger individuals. To curb the heroin epidemic, particularly among younger adults, collective prevention and intervention efforts may be most effective.71 Promising examples include expansion of access to medication-assisted treatment (including methadone hydrochloride, buprenorphine hydrochloride, or injectable naltrexone hydrochloride), educational programs in schools and community settings,72 overdose prevention training in concert with comprehensive naloxone hydrochloride distribution programs,73 and consistent use of prescription drug monitoring programs that implement best practices by prescribers.74,75 Efforts may be most efficient if concentrated in states acutely affected by the opioid epidemic, as noted in President Obama’s Comprehensive Addiction Recovery Act signed in July 2016.71 Although many parallels have been identified between increases in the PO epidemic and in heroin use and its consequences, NMPO use has decreased recently, whereas heroin use and related disorders continue to increase.17,49 Understanding these diverging trends is an important public health challenge that must be met to halt further increases.
eTable 1. Heroin Use and Demographic Correlates in NESARC (2001-2002) and NESARC-III (2012-2013)
eTable 2. DSM-IV Heroin Use Disorder and Demographic Correlates in NESARC (2001-2002) and NESARC-III (2012-2013)
References
- 1.Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(2):154-163. [DOI] [PubMed] [Google Scholar]
- 2.Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314(14):1468-1478. [DOI] [PubMed] [Google Scholar]
- 3.Darke S, Marel C, Mills KL, Ross J, Slade T, Tessson M. Years of potential life lost amongst heroin users in the Australian Treatment Outcome Study cohort, 2001-2015. Drug Alcohol Depend. 2016;162:206-210. [DOI] [PubMed] [Google Scholar]
- 4.Lopez-Quintero C, Roth KB, Eaton WW, et al. Mortality among heroin users and users of other internationally regulated drugs: a 27-year follow-up of users in the Epidemiologic Catchment Area Program household samples. Drug Alcohol Depend. 2015;156:104-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martins SS, Sampson L, Cerdá M, Galea S. Worldwide prevalence and trends in unintentional drug overdose: a systematic review of the literature. Am J Public Health. 2015;105(11):e29-e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention . Today’s Heroin Epidemic: More People at Risk, Multiple Drugs Abused. https://www.cdc.gov/vitalsigns/heroin/index.html. Updated July 7, 2015. Accessed June 15, 2016.
- 7.Rondinelli AJ, Ouellet LJ, Strathdee SA, et al. Young adult injection drug users in the United States continue to practice HIV risk behaviors. Drug Alcohol Depend. 2009;104(1-2):167-174. [DOI] [PubMed] [Google Scholar]
- 8.Yen CN, Wang CS, Wang TY, Chen HF, Chang HC. Quality of life and its correlates among heroin users in Taiwan. Kaohsiung J Med Sci. 2011;27(5):177-183. [DOI] [PubMed] [Google Scholar]
- 9.Csete J, Kamarulzaman A, Kazatchkine M, et al. Public health and international drug policy. Lancet. 2016;387(10026):1427-1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Center for Behavioral Health Statistics and Quality . Drug Abuse Warning Network Methodology Report, 2011 Update. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality . Treatment Episode Data Set (TEDS): 2003-2013. National Admissions to Substance Abuse Treatment Services. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [Google Scholar]
- 12.Muhuri PK, Gfroerer JC, Davies C. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States. CBHSQ Data Review. http://archive.samhsa.gov/data/2k13/DataReview/DR006/nonmedical-pain-reliever-use-2013.pdf. Published August 2013. Accessed October 16, 2016.
- 13.Cicero TJ, Kuehn BM. Driven by prescription drug abuse, heroin use increases among suburban and rural whites. JAMA. 2014;312(2):118-119. [DOI] [PubMed] [Google Scholar]
- 14.Cicero TJ, Ellis MS. Nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(13):1295-1296. [DOI] [PubMed] [Google Scholar]
- 15.Cicero TJ, Ellis MS, Harney J. Shifting patterns of prescription opioid and heroin abuse in the United States. N Engl J Med. 2015;373(18):1789-1790. [DOI] [PubMed] [Google Scholar]
- 16.Ihongbe TO, Masho SW. Prevalence, correlates and patterns of heroin use among young adults in the United States. Addict Behav. 2016;63:74-81. [DOI] [PubMed] [Google Scholar]
- 17.Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users—United States, 2002-2013. MMWR Morb Mortal Wkly Rep. 2015;64(26):719-725. [PMC free article] [PubMed] [Google Scholar]
- 18.Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(4):361-368. [DOI] [PubMed] [Google Scholar]
- 20.Grant BF, Moore TC, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 21.Grant BF, Amsbary M, Chu A, et al. Source and Accuracy Statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2014. [Google Scholar]
- 22.Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the United States Between 2001-2002 and 2012-2013. JAMA Psychiatry. 2015;72(12):1235-1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Substance Abuse and Mental Health Services Administration . Results From the 2012 National Survey on Drug Use and Health: Summary of National Findings, Appendix B: Statistical Methods and Measurement. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- 24.Adams PF, Kirzinger WK, Martinez ME; National Center for Health Statistics . Summary health statistics for US adults: National Health Interview Survey, 2012. Vital Health Stat 2013;10(259). [PubMed] [Google Scholar]
- 25.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 26.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 27.Canino G, Bravo M, Ramírez R, et al. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol. 1999;60(6):790-799. [DOI] [PubMed] [Google Scholar]
- 28.Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule–Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend. 1997;47(3):171-185. [DOI] [PubMed] [Google Scholar]
- 29.Cottler LB, Grant BF, Blaine J, et al. Concordance of DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug Alcohol Depend. 1997;47(3):195-205. [DOI] [PubMed] [Google Scholar]
- 30.Grant BF. DSM-IV, DSM-III-R, and ICD-10 alcohol and drug abuse/harmful use and dependence, United States, 1992: a nosological comparison. Alcohol Clin Exp Res. 1996;20(8):1481-1488. [DOI] [PubMed] [Google Scholar]
- 31.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71(1):7-16. [DOI] [PubMed] [Google Scholar]
- 32.Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39(1):37-44. [DOI] [PubMed] [Google Scholar]
- 33.Nelson CB, Rehm J, Ustün TB, Grant B, Chatterji S. Factor structures for DSM-IV substance disorder criteria endorsed by alcohol, cannabis, cocaine and opiate users: results from the WHO reliability and validity study. Addiction. 1999;94(6):843-855. [DOI] [PubMed] [Google Scholar]
- 34.Pull CB, Saunders JB, Mavreas V, et al. Concordance between ICD-10 alcohol and drug use disorder criteria and diagnoses as measured by the AUDADIS-ADR, CIDI and SCAN: results of a cross-national study. Drug Alcohol Depend. 1997;47(3):207-216. [DOI] [PubMed] [Google Scholar]
- 35.Ustün B, Compton W, Mager D, et al. WHO Study on the reliability and validity of the alcohol and drug use disorder instruments: overview of methods and results. Drug Alcohol Depend. 1997;47(3):161-169. [DOI] [PubMed] [Google Scholar]
- 36.Vrasti R, Grant BF, Chatterji S, et al. Reliability of the Romanian version of the alcohol module of the WHO Alcohol Use Disorder and Associated Disabilities: Interview Schedule–Alcohol/Drug-Revised. Eur Addict Res. 1998;4(4):144-149. [DOI] [PubMed] [Google Scholar]
- 37.Grant B, Harford TC, Dawson DA, Chou PS, Dufour M, Pickering R. Prevalence of DSM-IV alcohol abuse and dependence: United States, 1992. NIAAA Epidemiology Bull. 1994;18(3):243-248. [PMC free article] [PubMed] [Google Scholar]
- 38.Grant BF. Comorbidity between DSM-IV drug use disorders and major depression: results of a national survey of adults. J Subst Abuse. 1995;7(4):481-497. [DOI] [PubMed] [Google Scholar]
- 39.Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV Version. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- 40.Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44(2-3):133-141. [DOI] [PubMed] [Google Scholar]
- 41.Hasin DS, O’Brien CP, Auriacombe M, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834-851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thompson RG Jr, Alonzo D, Hu MC, Hasin DS. Substance use disorders and poverty as prospective predictors of adult first-time suicide ideation or attempt in the United States [published online July 16, 2016]. Community Ment Health J. doi:10.1007/s10597-016-0045-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saha TD, Kerridge BT, Goldstein RB, et al. Nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder in the United States. J Clin Psychiatry. 2016;77(6):772-780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grant BF, Saha TD, Ruan WJ, et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. JAMA Psychiatry. 2016;73(1):39-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171(5):618-623. [DOI] [PubMed] [Google Scholar]
- 46.Research Triangle Institute . SUDAAN Language Manual, Release 11.0. Research Triangle Park, NC: Research Triangle Institute; 2012. [Google Scholar]
- 47.Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309(7):657-659. [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention . Vital Signs: Today’s Heroin Epidemic—More People at Risk, Multiple Drugs Abused. https://www.cdc.gov/vitalsigns/heroin/. Updated July 7, 2015. Accessed December 28, 2016.
- 49.Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7):821-826. [DOI] [PubMed] [Google Scholar]
- 50.Compton WM, Jones CM, Baldwin GT. Nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(13):1296. [DOI] [PubMed] [Google Scholar]
- 51.Martins SS, Santaella-Tenorio J, Marshall BD, Maldonado A, Cerdá M. Racial/ethnic differences in trends in heroin use and heroin-related risk behaviors among nonmedical prescription opioid users. Drug Alcohol Depend. 2015;151:278-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med. 2012;13(2):150-174. [DOI] [PubMed] [Google Scholar]
- 53.Drug Enforcement Administration . National Drug Threat Assessment Summary 2014 [publication DEA-DCT-DIR-002–15]. Washington, DC: US Department of Justice, Drug Enforcement Administration; 2015. [Google Scholar]
- 54.Unick G, Rosenblum D, Mars S, Ciccarone D. The relationship between US heroin market dynamics and heroin-related overdose, 1992-2008. Addiction. 2014;109(11):1889-1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Carlson RG, Nahhas RW, Martins SS, Daniulaityte R. Predictors of transition to heroin use among initially non-opioid dependent illicit pharmaceutical opioid users: a natural history study. Drug Alcohol Depend. 2016;160:127-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cerdá M, Santaella J, Marshall BD, Kim JH, Martins SS. Nonmedical prescription opioid use in childhood and early adolescence predicts transitions to heroin use in young adulthood: a national study. J Pediatr. 2015;167(3):605-12.e1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers—United States, 2002-2004 and 2008-2010. Drug Alcohol Depend. 2013;132(1-2):95-100. [DOI] [PubMed] [Google Scholar]
- 58.Carliner H, Mauro PM, Brown QL, et al. The widening gender gap in marijuana use prevalence in the U.S. during a period of economic change, 2002-2014. Drug Alcohol Depend. 2017;170(1):51-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age-period-cohort influences on trends in past year marijuana use in the US from the 1984, 1990, 1995 and 2000 National Alcohol Surveys. Drug Alcohol Depend. 2007;86(2-3):132-138. [DOI] [PubMed] [Google Scholar]
- 60.National Employment Law Project . The Low-Wage Recovery: Industry Employment and Wages Four Years Into the Recovery. New York, NY: National Employment Law Project; 2014. [Google Scholar]
- 61.Rigg KK, Monnat SM. Comparing characteristics of prescription painkiller misusers and heroin users in the United States. Addict Behav. 2015;51:106-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Martins S, Ko J, Kuwabara S, et al. The relationship of adult mental disorders to race, socioeconomic status, marital status, and urbanicity of residence. In: Eaton W, ed. Public Mental Health. New York, NY: Oxford University Press; 2012:151-200. [Google Scholar]
- 63.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078-15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nyamathi A, Salem BE, Farabee D, et al. Correlates of heroin and methamphetamine use among homeless male ex-jail and prison offenders. Addict Res Theory. 2014;22(6):463-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Karberg J, James D. Substance Dependence, Abuse, and Treatment of Jail Inmates, 2002. Washington, DC: US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2005. [Google Scholar]
- 66.Glaze LE, Kaeble D. Correctional Populations in the United States, 2013. Washington, DC: Department of Justice, Bureau of Justice Statistics; 2014. [Google Scholar]
- 67.Mauer M, King RA. 25-Year Quagmire: The War on Drugs and its Impact on American Society. Washington, DC: The Sentencing Project; 2007. [Google Scholar]
- 68.Carson EA. Prisoners in 2014. Washington, DC: Bureau of Justice Statistics; 2015. [Google Scholar]
- 69.Hasin DS, Greenstein E, Aivadyan C, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): procedural validity of substance use disorders modules through clinical re-appraisal in a general population sample. Drug Alcohol Depend. 2015;148:40-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhao J, Stockwell T, Macdonald S. Non-response bias in alcohol and drug population surveys. Drug Alcohol Rev. 2009;28(6):648-657. [DOI] [PubMed] [Google Scholar]
- 71.Williams AR, Bisaga A. From AIDS to opioids—how to combat an epidemic. N Engl J Med. 2016;375(9):813-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Spoth R, Trudeau L, Shin C, et al. Longitudinal effects of universal preventive intervention on prescription drug misuse: three randomized controlled trials with late adolescents and young adults. Am J Public Health. 2013;103(4):665-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Leichtling GJ, Irvine JM, Hildebran C, Cohen DJ, Hallvik SE, Deyo RA. Clinicians’ use of prescription drug monitoring programs in clinical practice and decision-making [published online October 29, 2016]. Pain Med. pii:pnw251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Patrick SW, Fry CE, Jones TF, Buntin MB. Implementation of prescription drug monitoring programs associated with reductions in opioid-related death rates. Health Aff (Millwood). 2016;35(7):1324-1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Heroin Use and Demographic Correlates in NESARC (2001-2002) and NESARC-III (2012-2013)
eTable 2. DSM-IV Heroin Use Disorder and Demographic Correlates in NESARC (2001-2002) and NESARC-III (2012-2013)


