Summary
Laboratory and clinical studies are essential to the advancement of sciences. However, a significant gap exists between the research findings and clinical practice. Therefore, research findings can be of little importance if their outcome cannot be directly or indirectly applied to everyday clinical care or readily translated. This paper focuses on how we can shorten the gap between the generation of new knowledge and their implementation into everyday clinical care. A new model is discussed where clinicians are the ones generating the research idea are paired with researchers. They collaborate on studies whose results are readily applicable to everyday practice. Partnering with health providers on studies that address everyday clinical research questions is a potential solution to speed up the translation of the research findings. Generating clinically applicable results can better improve the health of the public. Quoting Dr. Lawrence W. Green: “If we want more evidence-based practice, we need more practice-based evidence.” This paper presents the practice-based research model as a solution to address this knowledge gap.
Introduction
It is an honor to be the recipient of the Buonocore Memorial lecture and to once more celebrate his findings at the Academy of Operative Dentistry annual meeting. Dr Michael Buonocore believed in making a difference in patients' lives, challenged existing paradigms, and was a forward thinker who just over 50 years ago revolutionized how we think today about prevention and restoration.1 With the concept of adhesive dentistry, he gave another dimension to how we restore teeth today, and as a result, dentists can propose minimal intervention dentistry that ultimately benefits patient's health. That is where I would like to get started: on patient's health.
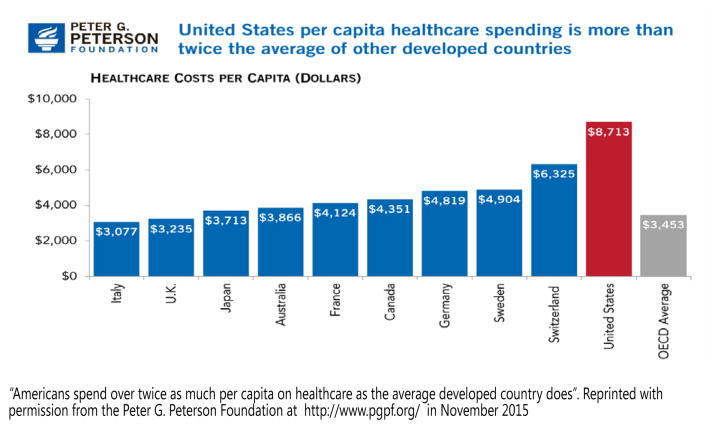
The cost of health care in the United States has been consistently higher than other developed countries, and it has dramatically increased in the last decade.2 The Peter G. Peterson Foundation is an American foundation established in 2008 by Peter G. Peterson, former US Secretary of Commerce. It works to find fiscal solutions to help secure the country's economic growth. According to government projections, health care expenditures are projected to climb to 22% by 2039. Americans currently pay about twice as much per capita on health care as other leading nations. The annual cost per capita has remained high, approaching $9000 for the last four years (Figure 1). Therefore, one would expect that because the United States spends significant funds on health care that the life expectancy would be higher. Unfortunately, that is not the case, and the life expectancy in the United States is still below several leading countries.3
Figure 1.
Bar graph illustrating the per capita health care costs in the United States and several leading countries.
Significant time and money has been spent in biomedical research in the United States4 and worldwide. We have accumulated a significant number of clinical and in vitro study results. Despite the immense amount of new knowledge, health in the United States is still below our expectation and below several industrialized countries. Several reasons need to be considered; however, we can focus on the following three. 1) A significant delay exists between the generation of new knowledge and its application into the medical/dental practicing community where it is delivered to patients. It takes an average of between 17 and 24 years to translate study findings to routine clinical practice.5 2) Too often, the study results are not immediately applied to everyday clinical care (ie, the results cannot be applied to benefit the patient's health).5-7 3) There is insufficient research that is evidence based on clinical practice for clinicians to make the correct choice during their decision-making process.8 It is estimated that as little as 8% of clinical practice is based on peer-reviewed and critically appraised evidence.9,10
One example that has been my research interest is the treatment of defective restorations. It is one of the most frequent problems encountered by general practitioners today and accounts for more than 50% of all the treatment performed in general dental practice.11-13 Several in vitro and clinical studies have shown that removal of the existing restoration will significantly reduce sound tooth structure, resulting in subsequently larger dental restorations.14-17 Additionally, the removal of existing restorations may cause further trauma on the tooth with possible dentinal/pulpal response to thermal, chemical, or mechanical stimuli, depending on the size and depth of the existing restored site.18-20 The consequence of replacing existing restorations could alter the outcome of the tooth and result in additional cost and time of treatment. All of these issues have a negative effect on patients. Two separate groups of investigators21-26 through clinical studies have concluded that the repair of defective restorations is a viable treatment option that increased the longevity of the original restoration. Despite the results of the clinical studies involving the repair of restorations and several schools including the teaching of repair of restorations in their curriculum,27-30 most clinicians still do not routinely consider the repair or sealing of defective restorations as a viable treatment option,31-34 and patients who may be eligible for repair of restorations are not offered this alternative treatment. One study published by the Dental Practice-Based Research Network (PBRN) in the United States involving close to 10,000 restorations (9875 restorations in 7502 patients) concluded that 75% of clinicians chose replacement over repair of defective restorations.35-37 We also learned that dentists' decision and bias will actually affect the restoration longevity.35 A survival analysis of posterior restorations using an insurance claims database concludes that patients who change dentists are far more likely to have restorations replaced than if they do not.38 An interesting finding is that most patients accept the repair of defective restorations. In another practice-based study involving close to 10,000 restorations and 200 clinicians, we assessed the behavioral aspect of patient satisfaction and found out that overall patient satisfaction was higher when the defective restoration was repaired compared with replaced.39,40 Another study by the Network assessed the outcome of almost 6000 restorations that had been repaired vs replaced after 12 months by 195 dentists. The results showed that repaired restorations were less likely to need an aggressive treatment than restorations that had been replaced. Overall, the failure rate was low (n=378 [−6%]). When the restoration required additional treatment after the one-year follow-up, it was less likely to need a replacement, a root canal treatment, or an extraction if the restoration had been repaired (74%) rather than if it had been replaced (85%). In other words, although some repaired restorations failed, the failure was not catastrophic, it was a “friendly failure”: a failure that could be repaired.37
Paradigm Shift
Despite all the efforts to study the treatment of defective restorations and ways to improve the longevity of the tooth and existing restoration through clinical studies, clinicians still do not routinely consider the repair of defective restorations as a viable treatment option. Therefore, a knowledge gap exists between the generation of new knowledge and its application to routine clinical care. How do we bridge the gap between research and clinical practice? How do we make sure that the topics being researched are of interest or will benefit the majority of the public at large? How do we make sure that once research findings become available that they will actually be implemented in dental and medical practices? These questions must be addressed if we hope to improve health while reducing costs.
Taxpayers and the public are very interested in immediate benefits from research investment.41 Search engines have been created an easy way for the public to access the results generated from federally funded research (eg, http://www.ncbi.nlm.nih.gov/pubmed; http://www.nidcr.nih.gov/oralhealth/; http://www.webmd.com/; http://www.healthline.com/; and http://www.nidcr.nih.gov/research/ResearchResults/NewsReleases/). The committee for economic development concluded that “increased public access accelerates progress in science by speeding up and broadening diffusion of knowledge” and “increased public-access policies should be judged by their impact on the society and the development of high-quality scientific research.” This opportunity for patients to access new results may lead patients to choose providers who rapidly implement research findings. A way to speed up the implementation of the research findings into clinical practice is to involve practitioners in the research process. That opportunity now exists with the creation of practice-based research (PBR). The commitment from the National Institute of Health (NIH) to fund PBR consolidates and attests where research efforts are headed (http://www.nidcr.nih.gov/research/ResearchResults/NewsReleases/CurrentNewsReleases/NDPBRN.htm and https://www.dentistry.ucla.edu/events/research-symposium-0).42-44
PBR is done by a teamwork approach: an effort in which clinicians and investigators work together to address clinical research questions that will ultimately benefit patient's health.45 Dental practice-based research is conducted by dentists who are affiliated to investigate research questions and to share experiences and expertise. The dentists provide dental care to the public and are affiliated with an academic center that serves as the administrative base. The research is done by practitioners in and about the “real world” of dental practice, where the majority of the population receives its dental care. Practice-based research is not a new concept. It was introduced by the medical field back in 1970s. In 2012, AHRQ (Agency for Healthcare Research and Quality), US Department of Health & Human Services, identified more than 150 primary care PBRNs operating across the United States with more than 55,000 clinicians in more than 17,000 locations, serving approximately 46 million patients. Today, there are more than 170 networks registered at the AHRQ website.43
A handicap in most in vitro and some clinical studies is the translation of the research findings to everyday clinical practice. One limiting factor of traditional institutional-based clinical study is the lack of generalizability and external validity.46 The result findings may not be readily applicable to everyday patients. Even if the findings are applicable to the everyday patient care, it takes time to translate the research results to everyday clinical practice. PBR addresses these obstacles in two ways: 1) it generates evidence-based knowledge with good external validity (the results apply to populations involved in the study (ie, the evidence comes directly from the end user, “the everyday patient”); and 2) PBR speeds up the adoption of the research findings by dentists who participated in the study. Passive absorption of knowledge usually does not work or works slowly.5 In PBR, clinicians are involved in the entire research process from its inception: asking the clinical questions, gathering the research findings, and being involved in its dissemination. As the practitioner is involved in the research process, it is more likely that he or she will implement the research findings into their routine delivery of clinical care.
Although a well-conducted randomized clinical trial (RCT) is typically the most scientifically rigorous design for clinical studies, it is not always the best design to help move scientific evidence promptly into routine clinical practice. A key advantage of most PBRN studies is that they intentionally do not use highly selected samples, but instead enroll consecutive patients for whom certain treatment options would be appropriate. In that manner, they maximize the generalizability of conclusions made about treatment effectiveness. They also allow for an analysis of the process of care, such as determining which patients are offered treatment by clinicians and which patients choose to accept it, a possibility precluded in a RCT design.
The benefit of PBR supersedes the notion of access to large number of patients. Besides the diversity of patient population, it is in PBR where “effectiveness can be measured, where new clinical questions arise, and where readiness to change and adopt new treatments can be studies and addressed.”45 It is also “where the interface between patients and their physicians can be explored and medical care improved.”45 Two main points are critical for the success of PBR: 1) it needs to address questions that practicing clinicians judge to be important with the potential the results could improve clinical practice; and 2) the research must be feasible in most busy clinical practices.
What drives clinicians to participate in PBR? According to multiple testimonies over the 11 years of the existence of the Dental PBRN in the United States, participants reported that they 1) desire interaction with other colleagues in the dental field; 2) want to belong to a community or entity, 3) have a desire to give back to the profession, and 4) want to know the answers to everyday clinical questions.47 Participants seek evidence-based answers to clinical questions and do not want to rely on biased opinions. Most information that is directed to clinicians is manufacturer driven, and bias is a major concern. The desire to be a part of a community that values answers informed by high-quality research drives most clinicians to join PBR.
Because networking with colleagues is important to practitioners, it is important that PBR allow an environment that fosters these interactions. One strategy is annual or semiannual meetings in which interaction with fellow practitioners is promoted. In those meetings, time is set aside for discussion among colleagues about the research results, including how to best implement the results into practice.
We discovered at the end of one of our interactive meetings that a significant number of practitioners actually changed how they practice as a result of the interactive discussion with their fellow clinicians. The improvement was toward using more prevention to treat dental caries and delaying the surgical treatment process in certain instances, according to the latest evidence-based research results.48,49 We learned that a highly interactive meeting with fellow practitioner-investigators could be an effective mean to apply scientific findings into clinical practice, as clinicians reported that they would change how they treat patients as a result of being engaged in the scientific process. This “change in intention” is consistent with the health change theory, which suggests that this step is a prelude to the subsequent next step, which is the actual implementation of change in the practice.50,51
Another benefit to the clinician's career of participating in a PBR network is that it provides clinicians an opportunity to present the research findings at national and international meetings. This is a benefit not only to the clinicians, but also for the research community in which the paper is being presented, as researchers and academicians get to hear from a clinician working in everyday practice about their experiences. PBR promotes interaction of researchers and academicians with their fellow practitioners and another opportunity to be a part of the research and educational processes.
One of the biggest challenges of practice-based research is to coordinate all the parts involved in the research process. We have learned that a lot can be accomplished when we have an organized teamwork approach. The academic institution provides a framework for the development of practice-based research, creating opportunities and resources for all those involved to be a part of the research process, but this would be meaningless if it did not have the involvement of the teams in the offices as the gathering of the research data takes place by the clinician and the dental team.
There are various steps involved in the PBR research process, from idea generation by the clinician (through the development of the study concept) all the way to the study launching (Figure 2). After a study concept is approved by both the executive committee and National Institute of Dental and Craniofacial Research (NIDCR) Clinical Studies Group, a study team is formed composed of statistician, one or more research investigators, private practitioner(s), research coordinator, a data manager staff, and a principal investigator. The study team will then develop and submit a complete clinical protocol using the NIDCR clinical study protocol template.52 After the approval of the complete protocol, the Coordinating Center will support the study team in the development of all required study startup documents, such as the Operations documents, Statistical Analysis Plan, Manual of Procedures, and Case Report Forms, using the NIDCR Toolkit templates.53 Once all the forms are completed and approved, the study is implemented in the offices that agreed to participate and that had completed the training requirement for participation in in-office research.
Figure 2.
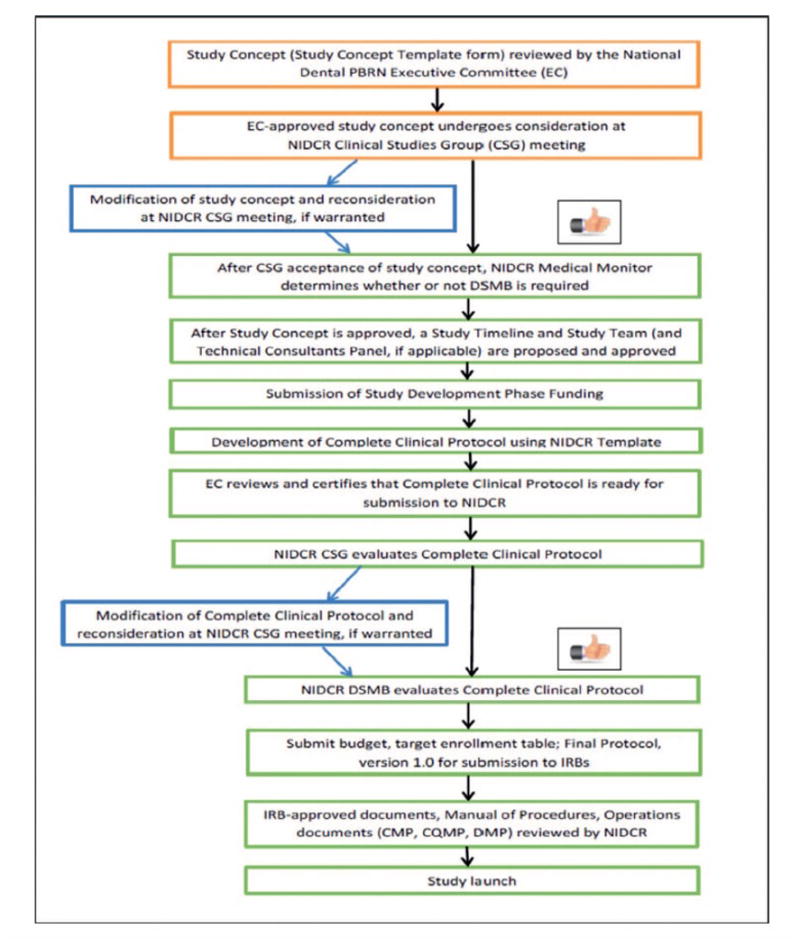
Example of a diagram illustrating the steps from study concept to study launch by the National Dental PBRN funded by the NIH-NIDCR (http://www.nationaldentalpbrn.org/study%20development.php).
Throughout the 11 years of existence of the dental PBR in the United States, we learned that patients' attitudes toward participation in dental research and experience with the delivery of care were valuable. We generated valuable results in the studies that had patient participation, ie, not only the attrition rate on survey studies was low, but also the overall response was positive. One behavioral science study involving 8000 patients asked patients about their dental office experience and their satisfaction with the dental procedure received.39,40 Because we wanted to make sure that the anesthesia had worn off when patients responded the questionnaire (so that the report would be most unbiased), patients had to respond no sooner than 24 hours, which meant that they would have left the office when they responded. The research group had some concern if patients would remember to respond to the questionnaire and mail it accordingly 24 hours later. We were pleasantly surprised with a 78% patient response rate. According to dentists' report, patients enjoyed being a part of the research process and appreciated the fact that the dental office was involved in research. Although there was some compensation for patients to participate (a $10 gift card), some patients returned the card back to the research as they felt it was “their responsibility to contribute to science.”
We also learned that it is fundamental for clinicians to be a part of the dissemination of the research findings. In fact, we learned that clinicians may respond more positively to findings presented by other clinician rather than by academic researchers. Therefore, close to 70% of publications and presentations from the National Dental Network include at least one full-time practicing clinician as a coauthor.54,55 The roles of the clinicians have ranged from presenters, to coauthors, to lead authors. It is our impression that when a clinician working in the field presents the data, there seems to have a more positive interaction between the presenter and the audience. There is a higher sense of ownership and experience that is shared as opposed to a researcher who may understand the clinician's experiences, but is not participating in the daily routine of the dental office.
Another approach to communicate with clinicians about research findings, particularly those who participate in studies is to summarize their individual study results and to compare them with other practitioners working in their region and network-wide (ie, nationally). The careful analysis of their individual study results creates opportunities for them to reflect on their decision-making process and quality of care and if applicable consider a change in their practice pattern. Therefore, the Network will provide a summary of the research findings to those participating in the research process. The findings have bar graphs and/or tables illustrating the research results and a sentence summarizing it.
PBR is an excellent venue to foster international collaboration. Besides the exchange of information among clinicians and researchers, it explores the unique aspect that diversity of patient population and culture brings to the scientific process and discovery. The National Dental Network in the Unites States (http://www.nationaldentalpbrn.org/) favors global collaboration. At the request of the NIDCR Director, Dr Marta Somerman, the International Association of Dental Research Network workshop in Boston in 2015 included global/international collaboration as a discussion topic. The symposium had 20 guests from various countries with representation from most continents on the globe. Some discussion has already been initiated among some countries and ongoing work anticipates a fruitful collaboration.56-60
Future Plans and Conclusions
In conclusion, what does the future hold for clinicians and researchers? Three important key points to consider before formulating new research ideas: 1) research approaches and methods must be timely, relevant, nontraditional, and practical61; 2) traditional federally funded or corporate-funded research in academic institutions has significant value that can complement the studies that are conducted in PBRNs, but they must be innovative and readily applicable to survive in today's research climate; and 3) engaging clinicians in the research process will increase the potential for research that is relevant to daily practice and it will speed up the translation and dissemination of research findings that is fundamental to advancing population health. PBRNs can be an effective avenue for translation of research findings as participants serve as change agents.
Clinical Relevance.
Partnering with health providers on studies that address everyday clinical research questions through practice-based research is a potential solution to speed up the translation of research findings.
Acknowledgments
The author thanks The National Dental PBRN Collaborative Group, which includes practitioner, faculty, and staff investigators. The author also thanks Dr Gregg H. Gilbert and Dr D. Brad Rindal for their critical review and valuable suggestions related to this manuscript. This work was supported in part by National Institutes of Health Grants DE-16746, DE-16747, and DE-22516. Opinions and assertions contained herein are those of the author and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been fully explained.
Footnotes
Regulatory Statement: This study was conducted in accordance with all the provisions of the local human subjects oversight committee guidelines and policies of the University of Florida IRB 01. The approval code for this study is 161-2005.
Conflict of Interest: The author of this manuscript certifies that she has no proprietary, financial, or other personal interest of any nature or kind in any product, service, and/or company that is presented in this article.
References
- 1.Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. Journal of Dental Research. 1955;34(6):849–853. doi: 10.1177/00220345550340060801. [DOI] [PubMed] [Google Scholar]
- 2.Organization for Economic Co-operation and Development. Health spending (indicator) [January 19, 2016];2016 https://data.oecd.org/healthres/health-spending.htm.
- 3.University of California. Atlas in globe inequality. [January 19, 2016];2000 http://ucatlas.ucsc.edu/health.php.
- 4.Rockey S. Rock talk. National Institutes of Health, Office of Extramural Research. [January 19, 2016];2012 http://nexus.od.nih.gov/all/2012/02/03/our-commitment-to-supporting-the-next-generation/
- 5.Contopoulos-Ioannidis DG, Alexiou GA, Gouvias TC, Ioannidis JP. Life cycle of translational research for medical interventions. Science. 2008;321(5894):1298–1299. doi: 10.1126/science.1160622. [DOI] [PubMed] [Google Scholar]
- 6.Solberg LI, Elward KS, Phillips WR, Gill JM, Swanson G, Main DS, Yawn BP, Mold JW, Phillips RL, Jr, for the NAPCRG Committee on Advancing the Science of Family Medicine How can primary care cross the quality chasm? Annals of Family Medicine. 2009;7(2):164–169. doi: 10.1370/afm.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naik AD, Petersen LA. The neglected purpose of comparative-effectiveness research. New England Journal of Medicine. 2009;360(19):1929–1931. doi: 10.1056/NEJMp0902195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niederman R, Clarkson J, Richards D. Guest editorial: The affordable care act and evidence-based care. Journal of the American Dental Association. 2011;142(4):364–367. doi: 10.14219/jada.archive.2011.0177. [DOI] [PubMed] [Google Scholar]
- 9.Ioannidis JP. Contradicted and initially stronger effects in highly cited clinical research. Journal of the American Medical Association. 2005;294(2):218–228. doi: 10.1001/jama.294.2.218. [DOI] [PubMed] [Google Scholar]
- 10.Antczak-Bouckoms A. Quality and effectiveness issues related to oral health. Medical Care. 1995;33(Supplement 11):123–142. doi: 10.1097/00005650-199511001-00012. [DOI] [PubMed] [Google Scholar]
- 11.Pink FE, Minden NJ, Simmonds S. Decisions of practitioners regarding placement of amalgam and composite restorations in general practice settings. Operative Dentistry. 1994;19(4):127–132. [PubMed] [Google Scholar]
- 12.Mjör IA, Moorhead JE, Dahl JE. Reasons for replacement of restorations in permanent teeth in general dental practice. International Dental Journal. 2000;50(6):360–366. doi: 10.1111/j.1875-595x.2000.tb00569.x. [DOI] [PubMed] [Google Scholar]
- 13.Simecek JW, Diefenderfer KE, Cohen ME. An evaluation of replacement rates for posterior resin-based composite and amalgam restorations in U.S Navy and Marine Corps recruits. Journal of the American Dental Association. 2009;140(2):200–209. doi: 10.14219/jada.archive.2009.0134. quiz 249. [DOI] [PubMed] [Google Scholar]
- 14.Gordan VV. In vitro evaluation of margins of replaced resin based composite restorations. Journal of Esthetic Dentistry. 2000;12(4):217–223. doi: 10.1111/j.1708-8240.2000.tb00223.x. [DOI] [PubMed] [Google Scholar]
- 15.Gordan VV. Clinical evaluation of replacement of Class V resin based composite restorations. Journal of Dentistry. 2001;29(7):485–488. doi: 10.1016/s0300-5712(01)00030-6. [DOI] [PubMed] [Google Scholar]
- 16.Gordan VV, Mondragon E, Shen C. Evaluation of the cavity design, cavity depth, and shade matching in the replacement of resin based composite restorations. Quintessence International. 2002;33(4):273–278. [PubMed] [Google Scholar]
- 17.Gordan VV, Shen C, Mjör IA. Marginal gap repair with flowable resin based composites. General Dentistry. 2004;52(5):390–394. [PubMed] [Google Scholar]
- 18.Hirata K, Nakashima M, Sekine I, Mukouyama Y, Kimura K. Dentinal fluid movement associated with loading of restorations. Journal of Dental Research. 1991;70(6):975–978. doi: 10.1177/00220345910700061301. [DOI] [PubMed] [Google Scholar]
- 19.Bissada NF. Symptomatology and clinical features of hypersensitive teeth. Archives of Oral Biology. 1994;39(Supplement):31S–32S. doi: 10.1016/0003-9969(94)90185-6. [DOI] [PubMed] [Google Scholar]
- 20.Brantley CF, Bader JD, Shugars DA, Nesbit SP. Does the cycle of rerestoration lead to larger restorations? Journal of the American Dental Association. 1995;126(10):1407–1413. doi: 10.14219/jada.archive.1995.0052. [DOI] [PubMed] [Google Scholar]
- 21.Gordan VV, Garvan CW, Blaser PK, Mondragon E, Mjor IA. A long-term evaluation of alternative treatments to replacement of resin-based composite restorations: Results of a seven-year study. Journal of the American Dental Association. 2009;140(12):1476–1484. doi: 10.14219/jada.archive.2009.0098. [DOI] [PubMed] [Google Scholar]
- 22.Gordan VV, Riley JL, III, Blaser PK, Mondragon E, Garvan CW, Mjor IA. Alternative treatments to replacement of defective amalgam restorations: Results of a 7-year clinical study. Journal of the American Dental Association. 2011;142(7):842–849. doi: 10.14219/jada.archive.2011.0274. [DOI] [PubMed] [Google Scholar]
- 23.Moncada G, Vildósola P, Fernandez E, Estay J, de Oliveira Júnior O, de Andrade M, Martin J, Mjor IA, Gordan VV. Longitudinal results of a 10-year clinical trial of repair of amalgam restorations. Operative Dentistry. 2015;40(1):34–43. doi: 10.2341/14-045-C. [DOI] [PubMed] [Google Scholar]
- 24.Moncada G, Fernandez E, Mena K, Martin J, Vildósola P, Oliveira Junior OB, Estay J, Mjör IA, Gordan VV. Seal, replacement or monitoring amalgam restorations with occlusal marginal defects? Results of a 10-year clinical trial. Journal of Dentistry. 2015;43(11):1371–1378. doi: 10.1016/j.jdent.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 25.Fernández E, Martín J, Vildósola P, Oliveira OB, Junior, Gordan VV, Mjor IA, Bersezio C, Estay J, de Andrade MF, Moncada G. Can repair increase the longevity of composite resins? Results of a 10-year clinical trial. Operative Dentistry. 2015;43(2):279–286. doi: 10.1016/j.jdent.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 26.Fernández E, Martín J, Vildósola P, Estay J, Oliveira OB, Junior, Gordan VV, Mjor IA, Gonzalez J, Loguercio A, Moncada G. Sealing composite with defective margins, good care or over treatment? Results of a 10 year clinical trial. Operative Dentistry. 2015;40(2):144–152. doi: 10.2341/14-143-C. [DOI] [PubMed] [Google Scholar]
- 27.Gordan VV, Mjör IA, Blum I, Wilson NHF. Teaching students the repair of resin based composite restorations: A survey of North American dental schools. Journal of the American Dental Association. 2003;134(3):317–323. doi: 10.14219/jada.archive.2003.0160. [DOI] [PubMed] [Google Scholar]
- 28.Blum IR, Lynch CD, Schreiver A, Heidemann D, Wilson NHF. Repair versus replacement of defective composite restorations in German dental schools. European Journal of Prosthodontics and Restorative Dentistry. 2011;19(2):56–61. [PubMed] [Google Scholar]
- 29.Blum IR, Lynch CD, Wilson NHF. Teaching of direct composite restoration repair in undergraduate dental schools in the United Kingdom and Ireland. European Journal of Dental Education. 2012;16(1):53–58. doi: 10.1111/j.1600-0579.2010.00674.x. [DOI] [PubMed] [Google Scholar]
- 30.Blum IR, Lynch CD, Wilson NHF. Teaching of the repair of defective composite restorations in Scandinavian dental schools. Journal of Oral Rehabilitation. 2012;39(3):210–216. doi: 10.1111/j.1365-2842.2011.02260.x. [DOI] [PubMed] [Google Scholar]
- 31.Gordan VV. Letter to the editor of the Journal of the American Dental Association. Journal of the American Dental Association. 2009;140(9):1078–1079. [Google Scholar]
- 32.Gordan VV, Garvan CW, Richman J, Fellows JL, Rindal DB, Qvist V, Heft MW, Williams OD, Gilbert GH, for The DPBRN Collaborative Group How dentists diagnose and treat defective restorations: Evidence from the Dental PBRN. Operative Dentistry. 2009;34(6):664–673. doi: 10.2341/08-131-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gordan VV. Letter to the editor of the Journal of the American Dental Association. Journal of the American Dental Association. 2010;141(3):248–252. [Google Scholar]
- 34.Gordan VV. Letter to the editor of the Journal of the American Dental Association for paper: Alternative treatments to replacement of defective amalgam restorations: Results of a 7-year clinical study. Journal of the American Dental Association. 2011;142:1336–1337. doi: 10.14219/jada.archive.2011.0274. [DOI] [PubMed] [Google Scholar]
- 35.Gordan VV, Riley JL, III, Geraldeli S, Rindal DB, Qvist V, Fellows JL, Kellum HP, Gilbert GH, for The DPBRN Collaborative Group Repair or replacement of defective restorations by dentists in the Dental PBRN. Journal of the American Dental Association. 2012;143(6):593–601. doi: 10.14219/jada.archive.2012.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gordan VV, Riley JL, III, Worley DC, Gilbert GH, for The DPBRN Collaborative Group Restorative material and other tooth-specific variables associated with the decision to repair or replace defective restorations: Findings from the Dental PBRN. Journal of Dentistry. 2012;40(5):397–405. doi: 10.1016/j.jdent.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gordan VV, Riley JL, III, Rindal DB, Qvist V, Fellows JL, Dilbone DA, Brotman SG, Gilbert GH, National Dental PBRN Collaborative Group Repair or replacement of restorations: A prospective cohort study by dentists in The National Dental PBRN. Journal of the American Dental Association. 2015;146(12):895–903. doi: 10.1016/j.adaj.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bogacki RE, Hunt RJ, del Aguila M, Smith WR. Survival analysis of posterior restorations using an insurance claims database. Operative Dentistry. 2002;27(5):488–492. [PubMed] [Google Scholar]
- 39.Riley JL, Gordan VV, Rindal DB, Fellows JL, Qvist V, Patel S, Foy P, Williams OD, Gilbert GH, for The DPBRN Collaborative Group Components of patient satisfaction with a dental restorative visit: Results from The Dental Practice-Based Research Network. Journal of the American Dental Association. 2012;143(9):1002–1010. doi: 10.14219/jada.archive.2012.0329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Riley JL, III, Gordan VV, Hudak-Boss S, Fellows J, Rindal DB, Gilbert GH, for The National Dental PBRN Collaborative Group Concordance between patient satisfaction and the dentist's view: Findings from the National Dental Practice-Based Research Network. Journal of the American Dental Association. 2014;145(4):355–362. doi: 10.14219/jada.2013.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Committee for Economic Development. The future of taxpayer-funded research: Who will control access to the results? Business group endorses greater public access. [February 2, 2016];2012 https://www.ced.org/pdf/The-Future-of-Taxpayer-Funded-Research.pdf.
- 42.Vannier DM, Somerman MJ. Guest editorial: Integrating the domains of dentistry and research A perspective from the National Institute of Dental and Craniofacial Research. Journal of the American Dental Association. 2016;147(2):77–79. doi: 10.1016/j.adaj.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 43.Hickner J, Green LA. Practice-based research networks (PBRNs) in the United States: Growing and still going after all these years. Commentary Journal of the American Board of Family Medicine. 2015;28(5):541–545. doi: 10.3122/jabfm.2015.05.150227. [DOI] [PubMed] [Google Scholar]
- 44.Glick M. Dr. Michael Glick, editor of the Journal of the American Dental Association, has a one-on-one conversation with guest editor NIDCR Director Martha Somerman on integrating dentistry and research. [February 4, 2016];2016 https://www.youtube.com/watch?v=DGEm4JEPZIU.
- 45.Westfall JM, Mold J, Fagnan L. Practice-based research—“Blue Highways” on the NIH roadmap. Journal of the American Medical Association. 2007;297(4):403–406. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- 46.Myers M. Qualitative research and the generalizability question: Standing firm with Proteus. [March 3, 2016];The Qualitative Report. 2000 http://www.nova.edu/ssss/QR/QR4-1/myers.html.
- 47.National Dental Practice Based Research Network. Testimonials of practitioners about their participation in the National Dental Network. [1/12/2016];2012 http://www.nationaldentalpbrn.org/testimonials.php.
- 48.Gilbert GH, Qvist V, Pihlstrom DJ, Foy PJ, Gordan VV. Change in stated clinical practice associated with participation in the DPBRN. General Dentistry. 2010;58(6):520–528. [PMC free article] [PubMed] [Google Scholar]
- 49.Rindal DB, Flottemesch TJ, Durand EU, Godlevsky OV, Schmidt A, Gesko DS, Gilbert GH, for the National Dental PBRN Collaborative Group Practice change toward better adherence to evidence-based treatment of early dental decay in the National Dental PBRN. Implementation Science. 2014;9:177. doi: 10.1186/s13012-014-0177-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Painter JE, Borba CPC, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: A systematic review. Annals of Behavior Medicine. 2008;35(3):358–362. doi: 10.1007/s12160-008-9042-y. [DOI] [PubMed] [Google Scholar]
- 51.Prochaska JO. Decision making in the transtheoretical model of behavior change. Medical Decision Making. 2008;28(6):845–849. doi: 10.1177/0272989X08327068. [DOI] [PubMed] [Google Scholar]
- 52.National Dental Practice Based Research Network. Study development guide and flow chart. [January 12, 2016];2016 http://www.nationaldentalpbrn.org/study-development.php.
- 53.National Institute of Dental and Craniofacial Research. Toolkit for clinical researchers by the National Institute of Dental and Craniofacial Research. [January 12, 2016];2016 http://www.nidcr.nih.gov/Research/toolkit/
- 54.Harris PA, McEdward DL, Brotman SG, Lease GM, Rindal DB, Gilbert GH, Gordan VV. Successfully engaging practitioners to present research. Journal of Dental Research. 2010;89CB Abstract 139335. [Google Scholar]
- 55.Harris PA, McEdward DL, Spoto JC, III, Harrison JR, Gilbert GH, Gordan VV, for The National DPBRN Collaborative Group Engagement of practitioners in presentation and publications: The National Dental PBRN. Journal of Dental Research. 2013;92A Abstract 174609. [Google Scholar]
- 56.Kakudate N, Sumida F, Matsumoto Y, Yokoyama Y, Riley J, III, Gilbert GH, Gordan VV. Dentist's decision to conduct caries risk assessment in Dental PBRN. Community Dentistry and Oral Epidemiology. 2015;43(2):128–134. doi: 10.1111/cdoe.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kakudate N, Sumida F, Matsumoto Y, Yokoyama Y, Gilbert GH, Gordan VV. Patient age and dentists' decisions about occlusal caries treatment thresholds. Operative Dentistry. 2014;39(5):473–480. doi: 10.2341/13-141-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kakudate N, Sumida F, Matsumoto Y, Manabe K, Gilbert GH, Gordan VV. Restorative treatment thresholds for proximal caries in dental PBRN. Journal of Dental Research. 2012;91(12):1202–1208. doi: 10.1177/0022034512464778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yokoyama Y, Kakudate N, Sumida F, Matsumoto Y, Gilbert GH, Gordan VV. Dentist's practice patterns regarding preventive dentistry: Results from a dental practice-based research network. BMJ. 2013;3(9):e003227. doi: 10.1136/bmjopen-2013-003227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yokoyama Y, Kakudate N, Sumida F, Matsumoto Y, Gilbert GH, Gordan VV. Dentists' dietary perception and practice patterns in a dental practice-based research network. PloS One. 2013;8(3):E59615. doi: 10.1371/journal.pone.0059615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Healthy People 2020. The result of a collaborative process among the U.S. Department of Health and Human Services (HHS) and other federal agencies, public stakeholders, and the advisory committee. [January 19, 2016];2014 http://www.healthypeople.gov/