Abstract
Enteropathogenic Escherichia coli (EPEC) strains deliver effector proteins Tir, EspB, Map, EspF, EspH, and EspG into host cells to induce brush border remodeling and produce attaching and effacing (A/E) lesions on small intestinal enterocytes. In this study, the role of individual EPEC effectors in brush border remodeling and A/E lesion formation was investigated with an in vitro human small intestinal organ culture model of EPEC infection and specific effector mutants. tir, map, espB, and espH mutants produced “footprint” phenotypes due to close bacterial adhesion but subsequent loss of bacteria; an espB mutant and other type III secretion system mutants induced a “noneffacing footprint” associated with intact brush border microvilli, whereas a tir mutant was able to efface microvilli resulting in an “effacing footprint”; map and espH mutants produced A/E lesions, but loss of bacteria resulted in a “pedestal footprint.” An espF mutant produced typical A/E lesions without associated microvillous elongation. An espG mutant was indistinguishable from the wild type. These observations indicate that Tir, Map, EspF, and EspH effectors play a role in brush border remodeling and production of mature A/E lesions.
Strains of enteropathogenic Escherichia coli (EPEC), an important pediatric diarrheal pathogen, colonize the small bowel and produce characteristic attaching and effacing (A/E) lesions on small intestinal enterocytes characterized by localized destruction of brush border microvilli, intimate bacterial attachment, and cytoskeletal accretion beneath intimately attached bacteria. Actin polymerization beneath bacteria frequently results in bacteria sitting on raised pedestal-like structures (23, 32). EPEC strains employ a type III secretion system (TTSS) to deliver effector virulence proteins into host cells leading to A/E lesion formation and diarrheal disease (9). Genes encoding A/E lesion formation map to the LEE (locus of enterocyte effacement) pathogenicity island (28) and within the LEE, Tir, EspB, Map, EspF, EspH, and EspG are known to be translocated into host cells, although only Tir and EspB have been shown to be essential for A/E lesion formation (8, 17, 19, 29, 37). Also essential is surface expression of the bacterial adhesion molecule, intimin (10).
Tir is the translocated transmembrane adaptor protein which links extracellular EPEC to the cell cytoskeleton; the extracellular domain of Tir binds intimin (10), while the intracellular amino and carboxy termini interact with a number of cytoskeletal proteins (13, 16). Intimin-Tir interaction triggers Tir tyrosine phosphorylation and recruitment of Nck, N-WASP, and Arp2/3, resulting in actin polymerization and pedestal formation (2). EspB is both a functional component of the TTSS (translocator protein) and an effector protein targeted to the host cell cytosol, where it modulates the cell actin cytoskeleton (35, 36, 39); its role as a translocator makes it essential for translocation of other effectors and thus for A/E lesion formation. EspB from the closely related enterohemorrhagic E. coli (EHEC) has been shown to bind and recruits α-catenin to the EHEC pedestal (26). Map is targeted to and interferes with mitochondrial function but also promotes rapid filopodia formation in a Cdc42-dependent manner (18, 19). EspF is involved in disruption of the tight junction (TJ) barrier, possibly through manipulation of the actin cytoskeleton (30); it also plays a role in EPEC-induced host cell death (5). The function of EspG is not known, although homology with Shigella VirA, which interacts with tubulin and causes microtubule instability, suggests EspG may play a similar role in EPEC infection (8, 40). EspH is a modulator of the host actin cytoskeleton affecting filopodia and pedestal formation (37). Thus, a number of EPEC effectors have been shown to modulate the host cytoskeleton and may be important in the events leading to A/E lesion formation. The aim of this study was to define the role of EPEC effectors in brush border remodeling and A/E lesion formation with an in vitro human intestinal organ culture (IVOC) model of EPEC infection (23) and defined effector protein mutants.
Wild-type EPEC strains colonize human intestinal mucosa, induce gross brush border remodeling, and produce A/E lesions.
Normal pediatric duodenal mucosal biopsies taken with informed consent and ethical approval were maintained in organ culture and infected for 8 h with overnight Luria broth cultures of wild-type EPEC strain E2348/69 and defined E2348/69 mutants (Table 1), as previously described (23). After 8 h, biopsies were thoroughly washed, fixed in 3% glutaraldehyde, processed for scanning electron microscopy (20), and examined in a Philips XL30 scanning electron microscope. Due to limitations of the human intestinal tissue available, each strain could be examined only twice. Nevertheless, the results presented were reproducible in both assays and are representative of the phenotypes observed.
TABLE 1.
Strains used in this study
| Strain | Genotype | Phenotype
|
Reference | |||
|---|---|---|---|---|---|---|
| BFP | Intimin | Tira | A/E lesionsb | |||
| E2348/69 | Wild-type EPEC isolate (O127:H6) | + | + | + | + | 27 |
| UMD901 | bfpA mutant | − | + | + | + | 41 |
| CVD452 | escN mutant | + | + | − | − | 14 |
| UMD864 | espB mutant | + | + | − | − | 7 |
| ICC171 | escF mutant | + | + | − | − | 38 |
| CVD206 | eae (intimin) mutant | + | − | + | − | 6 |
| E2348/69 tir | tir mutant | + | + | − | − | 17 |
| E2348/69 map | map mutant | + | + | + | + | 19 |
| UMD874 | espF mutant | + | + | + | + | 5 |
| E2348/69 espG | espG mutant | + | + | + | + | 8 |
| E2348/69 espH | espH mutant | + | + | + | + | 37 |
Tir translocation into host cells.
Assessed in HEp-2 cells by the fluorescence actin staining test (22).
Uninfected mucosa appeared uniformly smooth, although individual microvilli were not clearly resolved due to the presence of the brush border glycocalyx; no adherent bacteria were present in uninfected control tissue (Fig. 1a). After an 8-h infection with wild-type EPEC E2348/69, a good percentage of the mucosal surface was colonized by A/E bacteria (Fig. 1b). Brush border microvilli were now clearly resolved, and there was typical brush border remodeling with gross microvillous elongation particularly around the periphery of bacterial microcolonies and microvillous effacement where bacteria had produced A/E lesions (Fig. 1c). Three-dimensional bacterial microcolonies typical of localized adherence seen in tissue culture cell adhesion assays were not seen—only two-dimensional colonies of A/E bacteria. Cells without adherent bacteria appeared normal and were indistinguishable from uninfected tissue. These observations obtained with pediatric tissue are typical of those previously described for adult tissue (23). Typical EPEC strains possess a large EPEC adherence factor (EAF) plasmid which encodes a bundle-forming pilus (BFP) involved in interactions between bacteria and in adhesion to host cells (3, 11). An identical pattern of mucosal colonization to that of the wild type was seen with an E2348/69 bfpA mutant strain UMD901(Table 1) (Fig. 1d), except that this strain, in the absence of BFP production, was less efficient than the wild type at colonizing the mucosal surface, as we previously demonstrated for an EAF plasmid-cured derivative of E2348/69 (23).
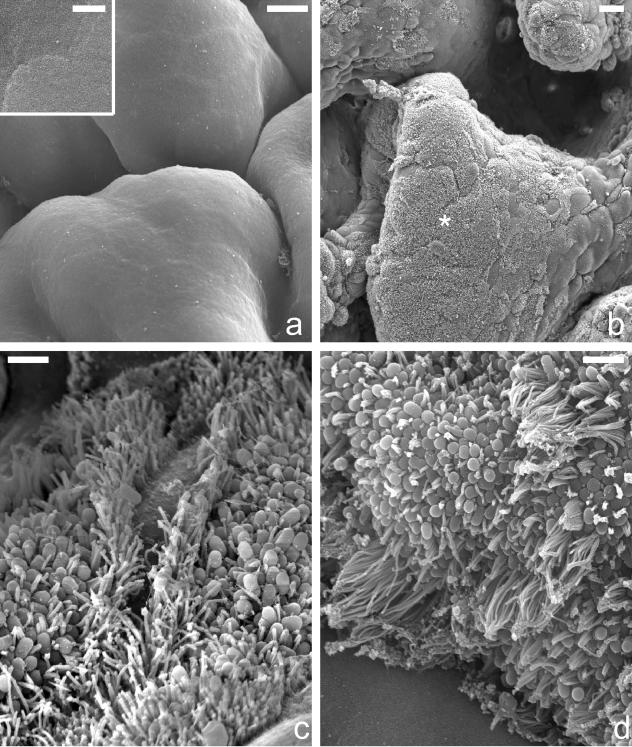
FIG. 1.
Scanning electron micrographs showing uninfected duodenal mucosa (a) and mucosa infected for 8 h with wild-type E2348/69 (b and c) and E2348/69 bfpA mutant strain UMD901 (d). Control tissue displayed a uniformly smooth mucosal surface with the outline of individual enterocytes visible, although even at high power, brush border microvilli were not resolved (a, inset); uninfected mucosa lacked any adherent bacteria (a). Following an 8-h infection with E2348/69, a large percentage of the mucosal surface was colonized by adherent bacteria (b, asterisk). Adherent bacteria had produced A/E lesions, and there was gross microvillous elongation, particularly around the periphery of bacterial microcolonies (c). Similar features were seen with the bfpA mutant strain (d). Size bars: a, 5 μm (inset, 0.5 μm); b, 10 μm; c and d, 1 μm.
EPEC strains lacking intimin are able to induce brush border remodeling but unable to form A/E lesions.
Intimin was the first protein shown to be essential for A/E lesion formation (15). Intimate EPEC adhesion and pedestal formation involves interaction between bacterial intimin and translocated and membrane-inserted Tir. The E2348/69 intimin mutant CVD206 (Table 1) still possesses nonintimate adhesins and a functional TTSS and can adhere to and translocate effectors into host cells, including Tir, but is unable to form intimate bacterial adhesion and A/E lesions (3, 6). In this study, virtually no adherent CVD206 bacteria were seen after an 8-h infection, although large areas of mucosa that had undergone some brush border remodeling were evident: mucosa with elongated brush border microvilli could be seen, and, in some areas of such modified mucosa, regions of microvillous effacement were present (Fig. 2). Such features were never seen on uninfected mucosa, on mucosa infected for 8 h with a commensal E. coli strain, or on mucosa incubated with culture medium from an 8-h CVD206 infection from which the bacteria had been removed, indicating that they were probably caused by CVD206 bacteria. This conclusion is supported by observations from short IVOC infections in which bacteria primed as ready to produce A/E lesions (4) were incubated with mucosal biopsies in suspension on a rotary mixer (3). Following a 1.5-h IVOC infection, CVD206 bacteria were seen adhering to the mucosa in small microcolonies and had induced localized microvillous remodeling but without intimate attachment or A/E lesions (Fig. 2, inset) (3). These observations are consistent with CVD206 being able to adhere to the mucosa initially, probably via BFP (3), and translocate effectors which induce microvillous elongation and effacement. In the absence of intimin-Tir interaction and A/E lesion formation, BFP-mediated bacterial dispersal (1, 25) would then explain the lack of adherent bacteria seen after 8 h.
FIG. 2.
Scanning electron micrographs showing duodenal mucosa infected for 8 h and 1.5 h (inset) with intimin (eae) mutant strain CVD206. After 8 h, virtually no adherent bacteria were seen, although areas of mucosa with elongated brush border microvilli could be seen and, in some areas of such remodeled mucosa, regions of microvillous effacement appeared to be present (asterisk). Adherent CVD206 bacteria were present following a short 1.5-h infection, and these were associated with areas of brush border remodeling (inset). Size bars, 0.5 μm.
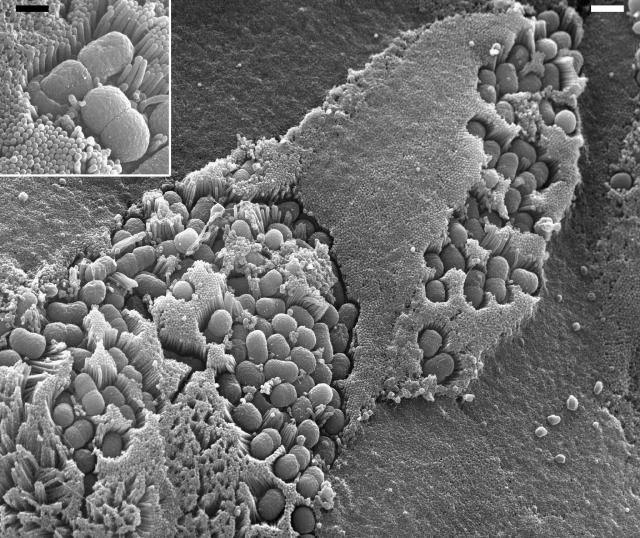
EPEC strains deficient in type III secretion adhere and produce a noneffacing bacterial footprint.
Mutants deficient in critical components of the EPEC TTSS do not produce a functional translocation apparatus (24, 38) and are therefore unable to translocate effectors into the host cell to produce A/E lesions. They do, however, produce BFP and express surface intimin. Three TTSS mutants lacking EscN, EscF, and EspB (Table 1) were examined in 8-h IVOC assays, and these strains produced a new adherence phenotype that we have termed a “noneffacing footprint” (Fig. 3). Some bacteria showed close adherence to the mucosal surface, although this could not be intimin-Tir intimate adherence, since Tir is not being translocated; other bacteria, however, appeared to have come away from the surface, leaving a bacterial footprint which clearly outlined the shape of the bacterium (Fig. 3). To form this type of footprint, there has been limited elongation of some brush border microvilli around the bacterium, but this appears quite distinct from the gross microvillous elongation seen with wild-type EPEC. In this phenotype, the tips of brush border microvilli are clearly resolved, showing that no effacement has taken place. To produce a footprint presumably requires interaction between molecules covering the bacterial surface and receptors on the host cell surface. Although an intimin mutant, CVD206, appeared to be similarly able to efface brush border microvilli, its inability to produce a bacterial footprint suggests that intimin may be important. Under the infection conditions being used, intimin is the major protein expressed on the bacterial surface (21), and since no Tir has been translocated into the host cell membrane, such a footprint might indicate interaction between intimin and a host cell intimin receptor. Numerous pieces of evidence have indicated the presence of a host cell intimin receptor (10), and one putative receptor is nucleolin. First demonstrated to bind intimin γ of EHEC (33), nucleolin was recently shown to bind EPEC intimins α and β with the same affinity, albeit lower avidity than binding to Tir (34). Whatever the nature of this bacterium-cell interaction, removal of bacteria to reveal a footprint would suggest that the interaction is not particularly strong. We have previously shown that EPEC strains expressing intimin but lacking other initial attachment factors such as BFP and a functional TTSS are unable to adhere to brush border cells (3). Lack of a functional TTSS in these strains suggests that BFP may also be important to promote initial attachment prior to the more close attachment seen in the noneffacing footprint.
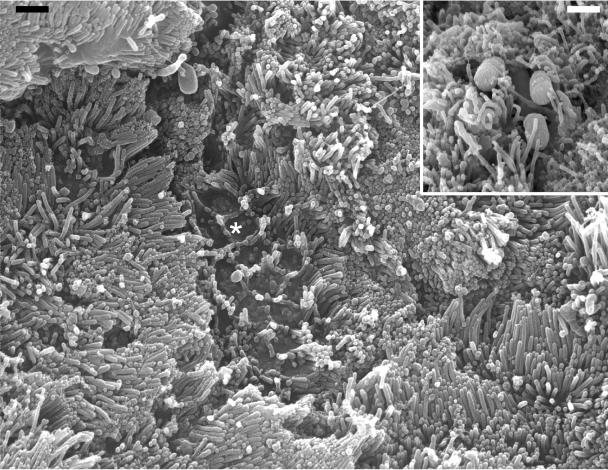
FIG. 3.
Scanning electron micrographs showing duodenal mucosa infected for 8 h with TTSS mutant strains CVD452 (escN) (a) and ICC171 (escF) (b). Some bacteria adhered closely to the mucosal surface, but other bacteria had come away, leaving a bacterial footprint associated with noneffaced microvilli, the tips of which were clearly resolved in areas of bacterial attachment; microvilli were not resolved in adjacent uninfected areas of mucosa (b, asterisk). Size bars, 0.5 μm.
Brush border microvilli are not usually clearly resolved by scanning electron microscopy due to the presence of the brush border glycocalyx (Fig. 1a). Interestingly, with these TTSS mutants, it was noticeable that noneffaced microvilli at the site of bacterial attachment were now clearly resolved but were not resolved on a closely adjacent mucosal surface (Fig. 3b, asterisk) which appeared like normal uninfected mucosa. A similar effect was seen with an E2348/69 espF mutant (see below). These observations suggest that adherent EPEC cells may have the ability to remove the brush border glycocalyx, something that might be required to facilitate intimin interaction with Tir during A/E lesion formation or intimin interaction with a host cell receptor as postulated here.
EPEC strains deficient in Tir produce an effacing bacterial footprint.
Tir is the translocated transmembrane adaptor protein which links extracellular EPEC to the cell cytoskeleton and is the only EPEC effector reported to be essential for A/E lesion formation. Hence, in the absence of Tir, EPEC cannot form an intimate intimin-Tir interaction or induce pedestal formation. In an 8-h IVOC infection, a Tir mutant adhered to the brush border and induced remodeling, including microvillous effacement at the site of bacterial attachment, although gross microvillous elongation was not apparent; other bacteria, however, appeared to have come away from the brush border surface, leaving a bacterial footprint (Fig. 4). This footprint, however, was distinct from the noneffacing footprint described above for some TTSS mutants in that brush border microvilli had been effaced at the site of bacterial attachment, leaving a hollow structure devoid of microvilli which outlined the shape of the bacterium (Fig. 4, inset). Consequently, we have termed this phenotype an “effacing bacterial footprint.” This footprint phenotype is independent of Tir but consistent with a requirement for effector protein translocation to induce microvillous effacement; as with the TTSS mutants, the actual footprint could indicate interaction between surface intimin and a host cell intimin receptor.
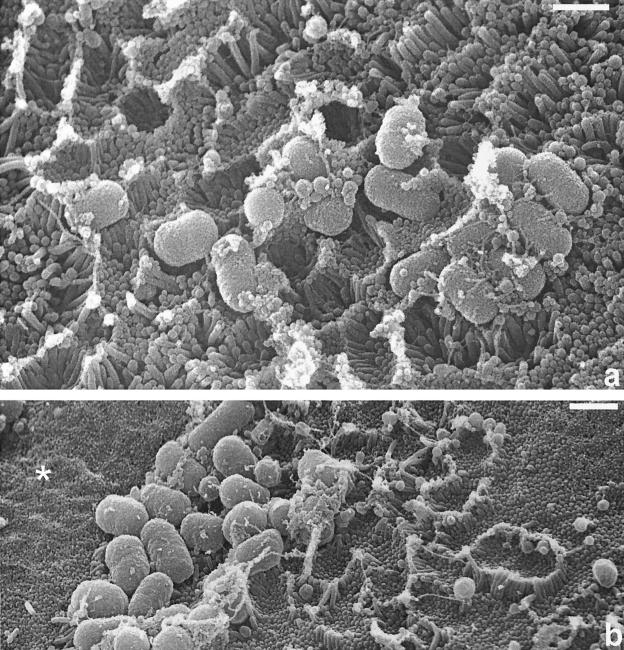
FIG. 4.
Scanning electron micrographs showing duodenal mucosa infected for 8 h with an E2348/69 tir mutant strain. Some bacteria adhered closely to the mucosal surface, but other bacteria had come away, leaving a bacterial footprint associated with cavities of effaced brush border microvilli (inset). Size bar, 0.5 μm (inset, 0.2 μm).
EPEC strains deficient in Map and EspH produce a pedestal footprint.
Map and EspH have both been implicated in filopodia formation and modulation of the host cell actin cytoskeleton in undifferentiated epithelial cells (18, 37). Since filopodia formation occurs rapidly on bacterial contact with cells, we examined Map and EspH mutants (Table 1) after short 1.5-h as well as 8-h IVOC infections. Little or no adhesion and brush border remodeling was observed after 1.5 h (data not shown), and so any role of these effectors in rapid brush border remodeling events could not be assessed. However, after 8 h, Map and EspH mutants both induced brush border remodeling and produced what appeared to be typical A/E lesions (Fig. 5). However, there were some differences from the wild-type strain in that elongation of noneffaced microvilli, particularly in the EspH mutant, appeared to be attenuated and some bacteria that had clearly formed pedestals had come away, leaving a third type of bacterial footprint, which we have termed a “pedestal footprint.” Clearly defined pedestal structures had formed, but the overlying bacterium was no longer present (Fig. 5, insets). We have never seen pedestal footprints with wild-type E2348/69, suggesting there is something defective with A/E lesions produced by the Map and EspH mutants. These mutants might express reduced surface intimin or translocate reduced amounts of Tir, resulting in a weaker intimin-Tir interaction, but this was not apparent following fluorescence imaging of intimin and Tir in infected HEp-2 cells (data not shown). More likely, based on their recognized cytoskeleton-modulating effects (18, 37), Map and EspH effectors might, in some way, be modulating Tir interaction with the cytoskeleton, which in turn modulates Tir-intimin interaction.
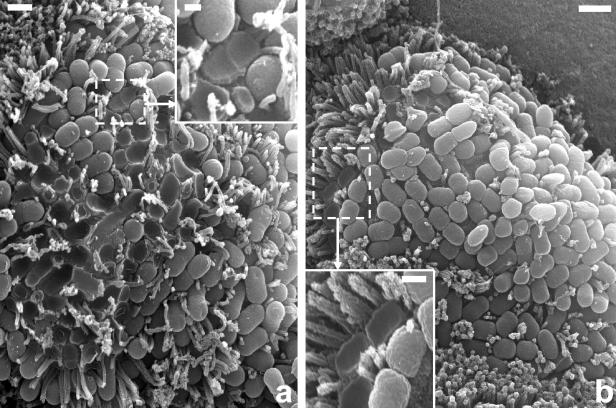
FIG. 5.
Scanning electron micrographs showing duodenal mucosa infected for 8 h with E2348/69 map (a) and espH (b) mutant strains. Both strains induced microvillous effacement and formed A/E lesions, although unlike the wild type, some bacteria had come away from what appeared to be perfectly formed pedestals (a and b, insets). Size bars: a and b, 0.5 μm (insets, 0.2 μm).
EPEC strains deficient in EspG are indistinguishable from the wild type.
The function of EspG is unclear, although, like VirA in Shigella, it might function in modulation of the microtubule cytoskeleton (40). In an 8-h IVOC infection, an EspG mutant (Table 1) produced brush border remodeling and A/E lesions typical of wild-type E2348/69 (Fig. 6). EspG is not required for A/E lesion formation in undifferentiated cells (8), but it is possible that it might play a role in A/E lesion formation in intestinal epithelial brush border cells but was not seen in this study because of genetic redundancy. Some EPEC strains, including E2348/69, possess the EspC pathogenicity islet which encodes Orf3, a homologue of EspG (8). It is now becoming clear that EPEC strains possess additional non-LEE-encoded effectors that are delivered to host cells (12). Translocated Orf3 could therefore be compensating for the lack of EspG, thus resulting in an EspG mutant behaving like the wild type.
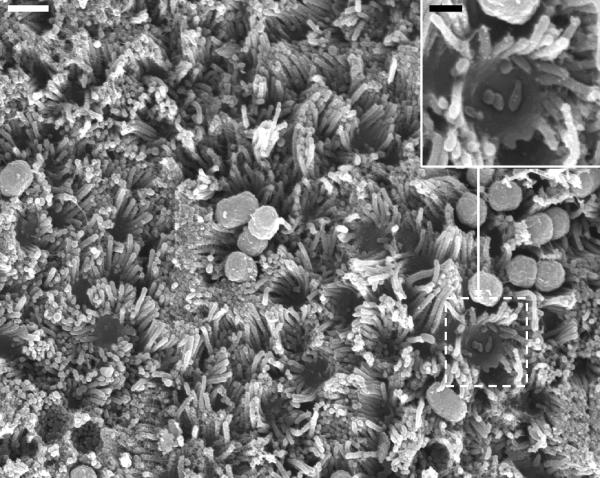
FIG. 6.
Scanning electron micrograph showing duodenal mucosa infected for 8 h with an E2348/69 espG mutant strain. Bacteria produced A/E lesions and brush border remodeling indistinguishable from that of wild-type strain E2348/69. Size bar, 0.5 μm.
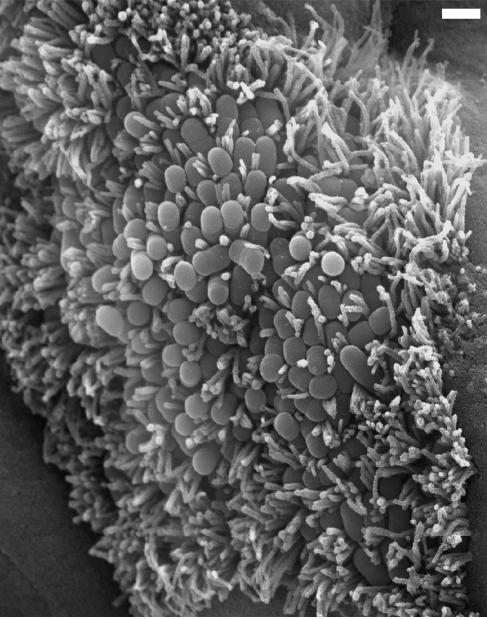
EPEC strains deficient in EspF do not induce microvillous elongation.
EspF has been implicated in disruption of cell TJs but not in A/E lesion formation (30). In an 8-h IVOC infection, an EspF mutant (Table 1) produced typical A/E lesions with localized effacement of brush border microvilli (Fig. 7). However, with this mutant the remaining noneffaced microvilli were highly uniform in length, which is very different from that observed with wild-type E2348/69-infected cells, in which microvilli are frequently highly elongated; microvilli in EspF mutant-infected cells were typical of normal brush border microvilli, although looking at Fig. 7 one might get the impression that the microvilli of infected cells are elongated compared to those of adjacent uninfected cells. This is because, as we have previously shown, EPEC-infected cells become raised above the level of surrounding uninfected cells (23), giving the impression that normal microvilli of infected cells are elongated. These observations suggest that EspF might play a role in brush border remodeling in addition to its role in modulating TJ structure and function (31).
FIG. 7.
Scanning electron micrograph showing duodenal mucosa infected for 8 h with an E2348/69 espF mutant strain. This strain colonized the mucosa and produced typical A/E lesions (inset). Noticeably, infected cells were raised above the surrounding uninfected mucosa and uneffaced microvilli were all uniformly long and not elongated; microvillous tips were also resolved in infected cells compared to adjacent uninfected cells. Size bar, 0.5 μm (inset, 0.2 μm).
While this study has identified some interesting new intestinal brush border phenotypes associated with intimin, TTSS, and effector protein mutants, the study failed to identify distinct functions associated with individual effector proteins in relation to the brush border remodeling events that occur during A/E lesion formation. This probably reflects the fact that, with single-gene-knockout mutants, one is not observing the effects of a single effector protein but rather the net effect of the remaining effectors. The identification of specific effector functions in brush border remodeling could be precluded because of genetic redundancy, multifunctionality, and the coordinate effects of different effectors (18).
Acknowledgments
We thank the Department of Paediatric Gastroenterology, Birmingham Children’s Hospital, for providing mucosal biopsies and Jim Kaper, Michael Donnenberg, Simon Elliott, Brendan Kenny, and Ilan Rosenshine for E2348/69 mutants.
This work was supported by the Wellcome Trust.
Editor: A. D. O'Brien
REFERENCES
- 1.Bieber, D., S. W. Ramer, C. Y. Wu, W. J. Murray, T. Tobe, R. Fernandez, and G. K. Schoolnik. 1998. Type IV pili, transient bacterial aggregates, and virulence of enteropathogenic Escherichia coli. Science 280:2114-2118. [DOI] [PubMed] [Google Scholar]
- 2.Campellone, K. G., and J. M. Leong. 2003. Tails of two Tirs: actin pedestal formation by enteropathogenic E. coli and enterohemorrhagic E. coli O157:H7. Curr. Opin. Microbiol. 6:82-90. [DOI] [PubMed] [Google Scholar]
- 3.Cleary, J., L.-C. Lai, R. K. Shaw, A. Straatman-Iwanowska, M. S. Donnenberg, G. Frankel, and S. Knutton. 2004. Enteropathogenic Escherichia coli (EPEC) adhesion to intestinal epithelial cells: role of bundle-forming pili (BFP), EspA filaments and intimin. Microbiology 150:527-538. [DOI] [PubMed] [Google Scholar]
- 4.Collington, G. K., I. W. Booth, and S. Knutton. 1998. Rapid modulation of electrolyte transport in Caco-2 cell monolayers by enteropathogenic Escherichia coli (EPEC) infection. Gut 42:200-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crane, J. K., B. P. McNamara, and M. S. Donnenberg. 2001. Role of EspF in host cell death induced by enteropathogenic Escherichia coli. Cell Microbiol. 3:197-211. [DOI] [PubMed] [Google Scholar]
- 6.Donnenberg, M. S., and J. B. Kaper. 1991. Construction of an eae deletion mutant of enteropathogenic Escherichia coli by using a positive-selection suicide vector. Infect. Immun. 59:4310-4317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donnenberg, M. S., J. Yu, and J. B. Kaper. 1993. A second chromosomal gene necessary for intimate attachment of enteropathogenic Escherichia coli to epithelial cells. J. Bacteriol. 175:4670-4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elliott, S. J., E. O. Krejany, J. L. Mellies, R. M. Robins-Browne, C. Sasakawa, and J. B. Kaper. 2001. EspG, a novel type III system-secreted protein from enteropathogenic Escherichia coli with similarities to VirA of Shigella flexneri. Infect. Immun. 69:4027-4033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frankel, G., A. D. Phillips, I. Rosenshine, G. Dougan, J. B. Kaper, and S. Knutton. 1998. Enteropathogenic and enterohaemorrhagic Escherichia coli: more subversive elements. Mol. Microbiol. 30:911-921. [DOI] [PubMed] [Google Scholar]
- 10.Frankel, G., A. D. Phillips, L. R. Trabulsi, S. Knutton, G. Dougan, and S. Matthews. 2001. Intimin and the host cell—is it bound to end in Tir(s)? Trends Microbiol. 9:214-218. [DOI] [PubMed] [Google Scholar]
- 11.Giron, J. A., A. S. Ho, and G. K. Schoolnik. 1991. An inducible bundle-forming pilus of enteropathogenic Escherichia coli. Science 254:710-713. [DOI] [PubMed] [Google Scholar]
- 12.Gruenheid, S., I. Sekirov, N. A. Thomas, W. Deng, P. O'Donnell, D. Goode, Y. Li, E. A. Frey, N. F. Brown, P. Metalnikov, T. Pawson, K. Ashman, and B. B. Finlay. 2004. Identification and characterization of NleA, a non-LEE-encoded type III translocated virulence factor of enterohaemorrhagic Escherichia coli O157:H7. Mol. Microbiol. 51:1233-1249. [DOI] [PubMed] [Google Scholar]
- 13.Hartland, E. L., M. Batchelor, R. M. Delahay, C. Hale, S. Matthews, G. Dougan, S. Knutton, I. Connerton, and G. Frankel. 1999. Binding of intimin from enteropathogenic Escherichia coli to Tir and to host cells. Mol. Microbiol. 32:151-158. [DOI] [PubMed] [Google Scholar]
- 14.Jarvis, K. G., J. A. Giron, A. E. Jerse, T. K. McDaniel, M. S. Donnenberg, and J. B. Kaper. 1995. Enteropathogenic Escherichia coli contains a putative type III secretion system necessary for the export of proteins involved in attaching and effacing lesion formation. Proc. Natl. Acad. Sci. USA 92:7996-8000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jerse, A. E., J. Yu, B. D. Tall, and J. B. Kaper. 1990. A genetic locus of enteropathogenic Escherichia coli necessary for the production of attaching and effacing lesions on tissue culture cells. Proc. Natl. Acad. Sci. USA 87:7839-7843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kenny, B. 1999. Phosphorylation of tyrosine 474 of the enteropathogenic Escherichia coli (EPEC) Tir receptor molecule is essential for actin nucleating activity and is preceded by additional host modifications. Mol. Microbiol. 31:1229-1241. [DOI] [PubMed] [Google Scholar]
- 17.Kenny, B., R. DeVinney, M. Stein, D. J. Reinscheid, E. A. Frey, and B. B. Finlay. 1997. Enteropathogenic E. coli (EPEC) transfers its receptor for intimate adherence into mammalian cells. Cell 91:511-520. [DOI] [PubMed] [Google Scholar]
- 18.Kenny, B., S. Ellis, A. D. Leard, J. Warawa, H. Mellor, and M. A. Jepson. 2002. Co-ordinate regulation of distinct host cell signalling pathways by multifunctional enteropathogenic Escherichia coli effector molecules. Mol. Microbiol. 44:1095-1107. [DOI] [PubMed] [Google Scholar]
- 19.Kenny, B., and M. Jepson. 2000. Targeting of an enteropathogenic E. coli (EPEC) effector protein to host mitochondria. Cell Microbiol. 2:579-590. [DOI] [PubMed] [Google Scholar]
- 20.Knutton, S. 1995. Electron microscopical methods in adhesion. Methods Enzymol. 253:145-158. [DOI] [PubMed] [Google Scholar]
- 21.Knutton, S., J. Adu-Bobie, C. Bain, A. D. Phillips, G. Dougan, and G. Frankel. 1997. Down regulation of intimin expression during attaching and effacing enteropathogenic Escherichia coli adhesion. Infect. Immun. 65:1644-1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knutton, S., T. Baldwin, P. H. Williams, and A. S. McNeish. 1989. Actin accumulation at sites of bacterial adhesion to tissue culture cells: basis of a new diagnostic test for enteropathogenic and enterohemorrhagic Escherichia coli. Infect. Immun. 57:1290-1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Knutton, S., D. R. Lloyd, and A. S. McNeish. 1987. Adhesion of enteropathogenic Escherichia coli to human intestinal enterocytes and cultured human intestinal mucosa. Infect. Immun. 55:69-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Knutton, S., I. Rosenshine, M. J. Pallen, I. Nisan, B. C. Neves, C. Bain, C. Wolff, G. Dougan, and G. Frankel. 1998. A novel EspA-associated surface organelle of enteropathogenic Escherichia coli involved in protein translocation into epithelial cells. EMBO J. 17:2166-2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Knutton, S., R. K. Shaw, R. P. Anantha, M. S. Donnenberg, and A. A. Zorgani. 1999. The type IV bundle-forming pilus of enteropathogenic Escherichia coli undergoes dramatic alterations in structure associated with bacterial adherence, aggregation and dispersal. Mol. Microbiol. 33:499-509. [DOI] [PubMed] [Google Scholar]
- 26.Kodama, T., Y. Akeda, G. Kono, A. Takahashi, K. Imura, T. Iida, and T. Honda. 2002. The EspB protein of enterohaemorrhagic Escherichia coli interacts directly with alpha-catenin. Cell Microbiol. 4:213-222. [DOI] [PubMed] [Google Scholar]
- 27.Levine, M. M., E. J. Bergquist, D. R. Nalin, D. H. Waterman, R. B. Hornick, C. R. Young, and S. Sotman. 1978. Escherichia coli strains that cause diarrhoea but do not produce heat-labile or heat-stable enterotoxins and are non-invasive. Lancet i:1119-1122. [DOI] [PubMed] [Google Scholar]
- 28.McDaniel, T. K., K. G. Jarvis, M. S. Donnenberg, and J. B. Kaper. 1995. A genetic locus of enterocyte effacement conserved among diverse enterobacterial pathogens. Proc. Natl. Acad. Sci. USA 92:1664-1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McNamara, B. P., and M. S. Donnenberg. 1998. A novel proline-rich protein, EspF, is secreted from enteropathogenic Escherichia coli via the type III export pathway. FEMS Microbiol. Lett. 166:71-78. [DOI] [PubMed] [Google Scholar]
- 30.McNamara, B. P., A. Koutsouris, C. B. O'Connell, J. P. Nougayrede, M. S. Donnenberg, and G. Hecht. 2001. Translocated EspF protein from enteropathogenic Escherichia coli disrupts host intestinal barrier function. J. Clin. Investig. 107:621-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muza-Moons, M. M., E. Schneeberger, and G. A. Hecht. 2004. Enteropathogenic Escherichia coli infection leads to appearance of aberrant tight junctions strands in the lateral membrane of intestinal epithelial cells. Cell. Microbiol. 6:783-793. [DOI] [PubMed] [Google Scholar]
- 32.Rothbaum, R. J., J. C. Partin, K. Saalfield, and A. J. McAdams. 1983. An ultrastructural study of enteropathogenic Escherichia coli infection in human infants. Ultrastruct. Pathol. 4:291-304. [DOI] [PubMed] [Google Scholar]
- 33.Sinclair, H. B., and A. D. O'Brien. 2002. Cell-surface localized nucleolin is a eukaryotic receptor for the adhesin intimin-gamma of enterohemorrhagic Escherichia coli O157:H7. J. Biol. Chem. 277:2876-2885. [DOI] [PubMed] [Google Scholar]
- 34.Sinclair, J. F., and A. D. O'Brien. 2004. Intimin types α, β, and γ bind to nucleolin with equivalent affinity but lower avidity than to the translocated intimin receptor. J. Biol. Chem. 279:33751-33758. [DOI] [PubMed] [Google Scholar]
- 35.Taylor, K. A., P. W. Luther, and M. S. Donnenberg. 1999. Expression of the EspB protein of enteropathogenic Escherichia coli within HeLa cells affects stress fibers and cellular morphology. Infect. Immun. 67:120-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Taylor, K. A., C. B. O'Connell, P. W. Luther, and M. S. Donnenberg. 1998. The EspB protein of enteropathogenic Escherichia coli is targeted to the cytoplasm of infected HeLa cells. Infect. Immun. 66:5501-5507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tu, X., I. Nisan, C. Yona, E. Hanski, and I. Rosenshine. 2003. EspH, a new cytoskeleton-modulating effector of enterohaemorrhagic and enteropathogenic Escherichia coli. Mol. Microbiol. 47:595-606. [DOI] [PubMed] [Google Scholar]
- 38.Wilson, R., R. K. Shaw, S. Daniell, I. Rosenshine, S. Aizawa, S. Knutton, and G. Frankel. 2001. Role of EscF, a putative needle-complex protein in the type III protein translocation system of enteropathogenic Escherichia coli. Cell Microbiol. 3:753-762. [DOI] [PubMed] [Google Scholar]
- 39.Wolff, C., I. Nisan, E. Hanski, G. Frankel, and I. Rosenshine. 1998. Protein translocation into HeLa cells by infecting enteropathogenic Escherichia coli. Mol. Microbiol. 28:143-155. [DOI] [PubMed] [Google Scholar]
- 40.Yoshida, S., E. Katayama, A. Kuwae, H. Mimuro, T. Suzuki, and C. Sasakawa. 2002. Shigella deliver an effector protein to trigger host microtubule destabilization, which promotes Rac1 activity and efficient bacterial internalization. EMBO J. 21:2923-2935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang, H. Z., and M. S. Donnenberg. 1996. DsbA is required for stability of the type IV pilin of enteropathogenic Escherichia coli. Mol. Microbiol. 21:787-797. [DOI] [PubMed] [Google Scholar]