Abstract
Objective
To characterize the causes of marked elevation of C-reactive protein (CRP) levels, investigate patient outcomes, and examine factors that might influence the CRP response.
Design
Health records were used to retrospectively determine patient characteristics, diagnoses, and outcomes over a 2-year period (2012 to 2013).
Setting
A large referral centre in Moncton, NB.
Participants
Adult inpatients and outpatients with a CRP level above 100 mg/L.
Main outcome measures
Differences among the CRP distributions of various diagnosis categories were examined using Kruskal-Wallis tests, and factors affecting outcomes were examined using Fisher exact tests.
Results
Over the 2-year period, 1260 CRP levels (839 patients; 3.1% of all tests) were above 100 mg/L (range 100.1 to 576.0 mg/L). The mean age was 63 years (range 18 to 101) and 50.2% of patients were men. Infection was the most prevalent cause (55.1%), followed by rheumatologic diseases (7.5%), multiple causes (5.6%), other inflammatory conditions (5.4%), malignancy (5.1%), drug reactions (1.7%), and other conditions (2.0%). A diagnosis could not be established in 17.6% of cases. On average, infections caused higher peak CRP levels (W = 34 519, P < .001) and infection was present in 88.9% of cases with CRP levels greater than 350 mg/L. Rheumatologic causes were associated with only 5.6% of CRP levels above 250 mg/L. The overall mortality was 8.6% and was higher in patients with malignancy (37.0%), multiple diagnoses (21.0%), and leukopenia (20.7%, P = .002).
Conclusion
Most patients had infections and the proportion of patients with infections increased with the level of CRP, although many diagnoses were associated with markedly elevated CRP levels. These data could help guide health care professionals in the evaluation and management of these patients.
Résumé
Objectif
Déterminer les causes des niveaux très élevés de la protéine C réactive (PCR), leurs conséquences pour le patient et les facteurs qui peuvent influencer cette réponse de la PCR.
Type d’étude
On a utilisé des dossiers de santé pour déterminer rétrospectivement les caractéristiques, les diagnostics et les résultats des patients sur une période de 2 ans (2012 à 2013).
Contexte
Un important centre de référence à Moncton, au Nouveau-Brunswick.
Participants
Des patients adultes externes ou hospitalisés présentant un niveau de PCR supérieur à 100 mg/L.
Principaux paramètres à l’étude
On a utilisé des tests de Krustal-Wallis pour établir des catégories de diagnostic selon le niveau de la PCR, ainsi que des tests exacts de Fisher pour les facteurs susceptibles d’influencer les issues.
Résultats
Au cours des 2 années de l’étude, on a trouvé 1260 niveaux de PCR (839 patients; 3,1 % de tous les tests) qui dépassaient 100 mg/L (entre 100,1 et 576,0 mg/L). L’âge moyen des patients était de 63 ans (entre 18 et 101 ans) et 50,2 % étaient des hommes. L’infection était la cause la plus courante (5,1 %), suivie par les maladies rhumatismales (7,5 %), la comorbidité (5,6 %), d’autres maladies inflammatoires (5,4 %), les cancers (5,1 %), certaines réactions médicamenteuses (1,7 %) et d’autres problèmes de santé (2,0 %). Dans 17,6 % des cas, on n’a pu établir de diagnostic. En moyenne, c’est l’infection qui a entraîné les plus hauts pics de PCR (W = 34 519, P < .001), et cette condition était présente dans 88,9 % des cas où le niveau de PCR dépassait 350 mg/L. Les causes d’ordre rhumatologique ne représentaient que 5,6 % des niveaux supérieurs à 250 mg/L. Dans l’ensemble, la mortalité était de 8,6 %, et elle était plus élevée dans les cas de cancer (37,0 %), de comorbidité (21,0 %) et de leucopénie (20,7 %, P = .002).
Conclusion
La plupart des patients avaient une infection, et plus le niveau de PCR était élevé, plus cette proportion augmentait, et ce, même si on trouvait des niveaux très élevés de PCR dans plusieurs autres conditions. Les présents résultats pourraient être utiles aux professionnels de la santé qui doivent évaluer et traiter ces patients.
C-reactive protein (CRP) level has widely replaced erythrocyte sedimentation rate (ESR) as a marker of inflammation, infection, and tissue damage. There are various important differences between CRP level and ESR, including the enhanced responsiveness and specificity of CRP test results. C-reactive protein levels rise more quickly than ESR (increasing within 2 hours and peaking at 48 hours) and are less affected by anemia, pregnancy, and elevated protein levels.1 As well, the range of CRP measurements is more than 5 times that of ESR. While there is an abundance of literature on the importance of low elevations of CRP levels,2,3 there is a paucity of studies, other than in disease-specific states, on the importance of high elevations of CRP levels. The causes of markedly elevated CRP levels in the general population have not been well established and it is unknown whether there are CRP levels at or above which certain diagnoses are more likely. This uncertainty might pose problems for clinicians who are tasked with triaging and investigating these patients. This study provides an initial step toward characterizing the causes and outcomes of markedly elevated CRP levels and examines factors that might influence the CRP response.
METHODS
Study population
We retrospectively reviewed all adult cases (18 years of age and older) with markedly elevated CRP levels (more than 10 times the upper limit of normal [10 mg/L]4 or > 100 mg/L*) of both inpatients and outpatients at a large community and regional referral hospital in Moncton, NB, over a 2-year period (2012 to 2013). All principal medical and surgical subspecialties, except transplant and cardiac surgery, are offered at this centre (and thus no key adult population is excluded).
Data collection
Health records were used to determine patient characteristics, diagnoses, and outcomes. Various data were recorded, including demographic characteristics (age, sex, location of patient, and usual health authority), the setting in which the test was ordered (outpatient services, emergency department, or inpatient services), as well as initial CRP level (> 100 mg/L), peak CRP level, clinical and laboratory information, medications, outcome, duration and level of care required, and diagnosis. Outcomes were determined during hospitalization at the time of the markedly elevated CRP level (long-term mortality was not considered owing to the possibility of unrelated causes). Clinical information of interest included temperature (highest value within 2 days of the initial markedly elevated CRP level), admitting diagnosis and comorbidities (especially pre-existing cancer, diabetes mellitus, chronic obstructive pulmonary disease, chronic kidney disease, immunosuppression, connective tissue disease, and congestive heart failure). Laboratory results recorded were white blood cell count (both at the time of the initial markedly elevated CRP value and the peak value), ESR (at the time of the initial markedly elevated CRP level), microbiology results, medical imaging findings, and pathology results. Furthermore, the specific diagnoses were classified into 1 of the following categories: infection, rheumatologic causes, inflammatory causes (excluding rheumatologic causes), malignancy, drug reactions, other causes, and multiple diagnoses. Where there was neither a definitive stated diagnosis nor a conclusive laboratory, radiographic, or histologic diagnosis, the cause for the elevated CRP level was considered uncertain.
C-reactive protein level was measured using the Abbott Architect c16000 multichannel analyzer.
Statistical analysis
Descriptive and frequency statistics were generated to illustrate each diagnostic group’s characteristics. Medians and interquartile ranges are presented for non-normally distributed variables. Differences between diagnosis categories on CRP distributions were examined using nonparametric statistics (eg, Kruskal-Wallis test and Wilcoxon rank sum test) with α set to .05. Potential differences between factors related to outcomes (eg, white blood cell count and body temperature) were examined using the Fisher exact test.
Horizon Health Network’s Research Ethics Board approved this study protocol, and patient consent was obtained only when there was telephone contact.
RESULTS
Study population
Over the 2-year period, 40 843 CRP levels were measured, and 1260 (839 patients, 3.1% of all tests) were above 100 mg/L (range 100.1 to 576.0 mg/L). Of these patients, the mean age was 63 years (range 18 to 101 years) and 50.2% were men. Overall, 22.9% of the CRP tests with markedly elevated results were ordered for outpatients, whereas 35.9% were ordered in the emergency department and 41.1% were ordered for inpatients. Erythrocyte sedimentation rate was normal (< 20 mm/h) in 24 of 481 patients (5.0%) for whom it was documented.
Causes of markedly elevated CRP levels
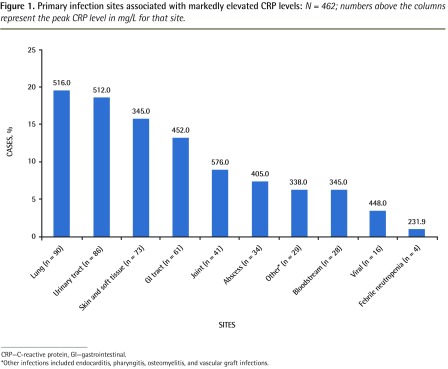
Most patients (55.1%) in this study had a diagnosis of infection. The proportion of cases caused by infection increased at higher CRP levels, and 88.9% of those presenting with a CRP level above 350 mg/L had an infection. Figure 1 outlines the most common infection sites.
Figure 1.
Primary infection sites associated with markedly elevated CRP levels: N = 462; numbers above the columns represent the peak CRP level in mg/L for that site.
CRP—C-reactive protein, GI—gastrointestinal.
*Other infections included endocarditis, pharyngitis, osteomyelitis, and vascular graft infections.
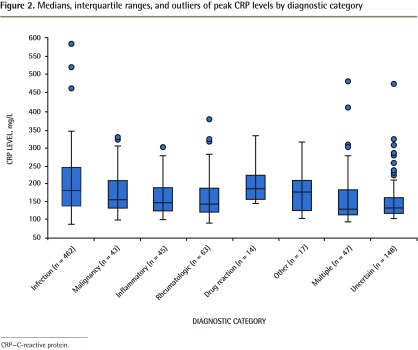
In addition, there were several noninfectious causes of markedly elevated CRP levels (Table 1) and each of these categories accounted for less than 8% of the total cases (with the exception of uncertain causes). The proportions of noninfectious causes remained relatively stable up to a CRP level of 350 mg/L, above which only 2 of the 18 patients did not have infection. We were unable to define a threshold to exclude certain diagnoses (Figure 2).
Table 1.
Causes of markedly elevated CRP levels: N = 839 patients.
| DIAGNOSIS | PATIENTS, N (%) |
|---|---|
| Infection | 462 (55.1) |
| Inflammatory | 45 (5.4) |
| Rheumatologic | 63 (7.5) |
| Malignancy | 43 (5.1) |
| Drug reaction | 14 (1.7) |
| Multiple* | 47 (5.6) |
| Uncertain | 148 (17.6) |
| Other | 17 (2.0) |
CRP—C-reactive protein.
Of the 47 patients who had multiple diagnoses, 46 also had infection.
Figure 2.
Medians, interquartile ranges, and outliers of peak CRP levels by diagnostic category
CRP—C-reactive protein.
There was a significant difference in CRP level distributions between diagnosis categories. On average, those with infection had higher peak CRP levels (W = 34 519, P < .001).
Noninfectious causes of markedly elevated CRP levels
Some of the specific noninfectious diagnoses are shown in Tables 2 and 3. The category of malignancy (n = 43) consisted predominantly of solid tumours (n = 18 malignancies were hematologic), with lung (n = 7) and colon (n = 6) neoplasms being most common.
Table 2.
Noninfectious diagnoses and associated peak CRP values
| DIAGNOSIS | NO. OF PATIENTS | PEAK CRP LEVEL, mg/L |
|---|---|---|
| Rheumatologic | 63 | 361.0 |
| Solid tumour | 25 | 325.0 |
| Pericarditis | 20 | 277.0 |
| Inflammatory bowel disease | 21 | 203.2 |
| Hematologic malignancy | 18 | 321.0 |
| Drug reaction | 14 | 321.0 |
| COPD exacerbation | 5 | 312.9 |
COPD—chronic obstructive pulmonary disease, CRP—C-reactive protein.
Table 3.
Unusual causes of markedly elevated CRP levels
| DIAGNOSIS | NO. OF PATIENTS | PEAK CRP LEVEL, mg/L |
|---|---|---|
| Venous thrombosis | 2 | 247.9 |
| Bowel obstruction | 2 | 218.0 |
| Gastrointestinal ischemia | 2 | 123.0 |
| Ischemic extremity | 1 | 118.0 |
| Rhabdomyolysis | 1 | 183.0 |
| Hematoma | 1 | 136.0 |
CRP—C-reactive protein.
Of the inflammatory conditions (n = 45), most were due to pericarditis (20 cases, CRP range 114.0 to 277.0 mg/L) or inflammatory bowel disease (21 cases, CRP range 100.6 to 203.2 mg/L). A few cases were due to pancreatitis (CRP range 124.0 to 296.0 mg/L).
There were 63 cases with rheumatologic causes. For comparison, during the same time period as the study, our rheumatology clinic alone had 212 visits for crystal-induced arthritis, 4978 visits for inflammatory arthritis, 346 visits for polymyalgia rheumatica, and 297 visits for either antineutrophil cytoplasmic antibody–associated vasculitis or giant cell arteritis (data not shown). Very few of these cases had CRP levels above 100 mg/L. Rheumatologic causes were associated with only 5.6% of CRP levels above 250 mg/L. In this study, crystal-induced arthritis accounted for 69.2% of rheumatologic cases with CRP levels above 250 mg/L, and septic arthritis was more common than any rheumatologic pathogenesis (Table 4). Of note, only 2 patients with systemic lupus erythematosus (SLE) had marked CRP elevations, and both had pericarditis.
Table 4.
Patients with rheumatologic diagnoses whose CRP levels remained above different cutoffs: Septic arthritis was considered an infection but its results are shown here for comparison.
| DIAGNOSIS | NO. AT PEAK CRP LEVEL | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| > 100 mg/L | > 150 mg/L | > 200 mg/L | > 250 mg/L | > 300 mg/L | > 350 mg/L | > 400 mg/L | > 500 mg/L | |
| Septic arthritis | 41 | 27 | 19 | 11 | 6 | 3 | 3 | 1 |
| Rheumatologic | ||||||||
| • Crystal-induced arthritis | 25 | 12 | 5 | 5 | 3 | 1 | 0 | 0 |
| • Vasculitis | 10 | 6 | 2 | 2 | 1 | 0 | 0 | 0 |
| • Rheumatoid arthritis | 10 | 3 | 2 | 0 | 0 | 0 | 0 | |
| • Other inflammatory arthritis | 10 | 4 | 1 | 1 | 0 | 0 | 0 | 0 |
| • Polymyalgia rheumatica | 6 | 2 | 1 | 0 | 0 | 0 | 0 | 0 |
| • SLE* | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
CRP—C-reactive protein, SLE—systemic lupus erythematosus.
The 2 patients with SLE both had isolated pericarditis.
Uncertain causes of markedly elevated CRP levels
A definitive diagnosis could not be established in 17.6% of patients (although they only accounted for 7.1% of patients with a CRP level > 200 mg/L) and these patients tended to have better outcomes. Of this subset, 75.0% were outpatients and 19.6% were from outside the zone of our health authority. Overall, 75.6% of outpatients from our zone with markedly elevated CRP levels had no information documented on their hospital outpatient charts around the time of the test. We did not review the primary care physicians’ medical charts. Telephone contact was made with some patients, but this yielded little additional diagnostic information.
Factors influencing the CRP response
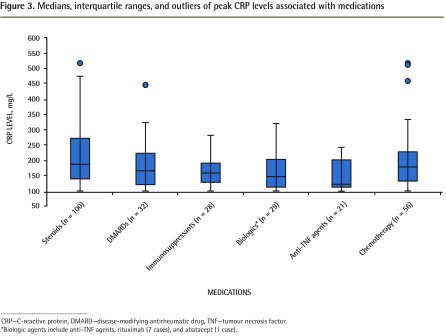
There was no significant correlation between peak CRP level and age, sex, or the presence of comorbidities. Anti–tumour necrosis factor (TNF) biologic agents appeared to be associated with a blunted CRP response (Figure 3). Few patients were being treated with these agents and there was substantial overlap in medications, so no statistically significant conclusions could be made. In addition, there were no patients taking either tocilizumab or ustekinumab who presented with markedly elevated CRP levels. No other medications appeared to affect the CRP response.
Figure 3.
Medians, interquartile ranges, and outliers of peak CRP levels associated with medications
CRP—C-reactive protein, DMARD—disease-modifying antirheumatic drug, TNF—tumour necrosis factor.
*Biologic agents include anti-TNF agents, rituximab (7 cases), and abatacept (1 case).
Outcomes
A total of 567 patients (67.6%) were admitted to hospital, 72 of whom were treated in the intensive care unit. While most patients with rheumatologic or uncertain causes were treated as outpatients, most patients with other diagnoses were hospitalized (Table 5).
Table 5.
Outcomes of patients based on diagnostic category
| DIAGNOSIS | HOSPITALIZED | MORTALITY, % | ||
|---|---|---|---|---|
|
| ||||
| ADMITTED, % | MEAN NO. OF DAYS | INTENSIVE CARE, % | ||
| Infection (n = 462) | 77.9 | 10.0 | 10.0 | 9.0 |
| Rheumatologic (n = 63) | 41.2 | 7.6 | 1.6 | 0.0 |
| Malignancy (n = 43) | 83.7 | 18.5 | 7.0 | 37.0 |
| Drug reaction (n = 14) | 71.4 | 8.4 | 14.0 | 0.0 |
| Multiple (n = 47) | 93.6 | 15.0 | 6.0 | 21.0 |
| Inflammatory (n = 45) | 88.9 | 9.0 | 20.0 | 4.0 |
| Other (n = 17) | 88.2 | 13.6 | 12.0 | 6.0 |
| Uncertain (n = 148) | 25.0 | 9.0 | 2.0 | 1.0 |
The overall mortality rate was 8.6% and was higher in patients with malignancy (37.0%), multiple diagnoses (21.0%), and leukopenia (20.7%, P = .002) (Table 6).
Table 6.
Outcomes of patients based on initial WBC count
| SAMPLE | HOSPITALIZED, % | MORTALITY, % |
|---|---|---|
| Leukopenia (n = 29) | 86.2 | 20.7* |
| Normal WBC count (n = 297) | 61.6 | 8.4 |
| Leukocytosis (n = 510) | 71.4 | 8.0 |
| Overall (n = 836) | 67.7 | 8.6 |
WBC—white blood cell.
Significant at P = .002 using Fisher exact test.
DISCUSSION
This study examined a large number of patients with markedly elevated CRP levels in a general population. While there were many causes of markedly elevated CRP levels, infection was the most common (particularly at higher CRP levels) and was present in 88.9% of patients with CRP levels above 350 mg/L. There was a significant difference in the CRP distributions between infection and other causes, although the Kruskal-Wallis test does not identify at what level there is a difference. Rheumatologic conditions have better outcomes and account for a small proportion of cases of markedly elevated CRP levels, with septic arthritis being more common than any of the others. Furthermore, mortality was increased with malignancy, multiple diagnoses, and leukopenia. Medications did not appear to affect the CRP response, with the possible exception of anti-TNF agents (and no patients were treated with tocilizumab or ustekinumab). Finally, there were 2 patients with SLE (both of whom had pericarditis) and ESR was normal in 5.0% of cases.
The results of this study might have various clinical implications. Based on our findings, the primary focus of clinicians presented with a markedly elevated CRP level should be to rule out infection. While crystal-induced arthritis was the most common rheumatologic cause, septic arthritis was even more common, emphasizing the need for joint aspiration. It is important to recognize that a variety of noninfectious conditions are also potential causes, and particular attention should be given to patients presenting with leukopenia, malignancies, and multiple diagnoses, owing to their association with worse prognoses. The presence of pericarditis in the patients with SLE is consistent with the observation that the CRP response is suppressed in SLE except in the setting of serositis or infection.5 We speculate that in the 24 cases with normal ESRs, the CRP test was done very early after the onset of illness, possibly before the ESR had enough time to increase. The potentially lowered CRP levels associated with anti-TNF agents and the lack of patients treated with tocilizumab (an interleukin-6 inhibitor) might follow from the fact that interleukin-6 and TNF-α are important drivers of CRP production. Correspondingly, it is possible that physicians might underestimate the risk of infection in patients taking certain biologic agents. In addition to certain biologic agents and SLE, there might be other conditions that suppress CRP production, such as advanced liver disease.6
A previous study had looked at patients with extreme elevations (> 500 mg/L) of CRP.7 While the characteristics of the institution were different (a large European tertiary care centre), the findings were similar. A total of 88% of their cases were caused by infection, which is consistent with our findings for CRP levels above 350 mg/L, and 71% had predisposing or debilitating comorbidities. Even severely immunosuppressed patients could mount a marked inflammatory response. Their mortality rate was higher (36% overall), particularly for patients with active cancer (61%) and neutropenia (73%), and was not affected by the maximal CRP level. Our study examined a broader range of elevated CRP levels in an attempt to better characterize the causes and outcomes of patients with markedly elevated CRP levels. Certain publications have suggested that there is a limited differential diagnosis for markedly elevated CRP levels, primarily severe infections and rheumatologic causes (vasculitis or severe arthritis).8 We were unable to define a CRP threshold above which certain diagnoses could be excluded, although we were able to show that infections typically present with the highest CRP levels and generated higher CRP levels on average.
Limitations
There are a number of limitations to our study. This was a retrospective review. Some clinical information was unobtainable owing to incomplete documentation, particularly for outpatients and those outside our health region or province. This resulted in a relatively high proportion of cases with CRP levels below 200 mg/L being classified as uncertain diagnoses. Moreover, there were insufficient numbers in some subgroups to draw firm conclusions about factors influencing the CRP response and patient outcomes. In addition, we are unable to comment on associations and outcomes in cases with less than markedly elevated CRP levels. Finally, we cannot exclude the possibility that there are factors other than those considered in this study that drive or suppress the CRP response.
Conclusion
This study examined the causes and outcomes of patients with markedly elevated CRP levels. The findings offer some guidance in the clinical management of such patients. It is important to note that several conditions can be associated with marked elevations of CRP levels, with infection being most common (particularly at extreme elevations). We could not distinguish between conditions based on the CRP level, but above 350 mg/L the cause was almost always infection. Further studies might lead to more conclusive results in some areas that were probed, such as a possible blunting of the CRP response by various biologic agents.
EDITOR’S KEY POINTS
This study examined a range of elevated C-reactive protein (CRP) levels to better characterize the causes and outcomes of markedly elevated CRP levels. The investigators were unable to define a CRP threshold above which certain diagnoses could be excluded, although they were able to show that infections typically presented with the highest CRP levels and generated higher CRP levels on average.
The primary focus of clinicians presented with a markedly elevated CRP level should be to rule out infection. Rheumatologic conditions have better outcomes and account for a small proportion of cases of markedly elevated CRP levels. While crystal-induced arthritis was the most common rheumatologic cause, septic arthritis was even more common, emphasizing the need for joint aspiration.
A variety of noninfectious conditions are also potential causes, and particular attention should be given to patients presenting with leukopenia, malignancies, and multiple diagnoses, owing to their association with worse prognoses.
POINTS DE REPÈRE DU RÉDACTEUR
Dans cette étude, les chercheurs ont examiné un éventail de niveaux élevés de la protéine C réactive (PCR) afin de préciser les causes et les conséquences des niveaux particulièrement élevés de PCR. Ils n’ont pas été en mesure de déterminer un niveau seuil au-delà duquel certains diagnostics pouvaient être exclus, mais ils ont pu démontrer qu’en moyenne, les infections présentaient généralement les niveaux les plus élevés de PCR et qu’elles généraient les niveaux moyens de PCR les plus élevés.
En présence d’un niveau très élevé de PCR, le clinicien devrait d’abord exclure la possibilité d’une infection. Les maladies rhumatismales ont des conséquences moins sévères et elles ne représentent qu’une faible proportion des cas de hausse importante de la PCR. Alors que la goutte était la cause rhumatismale la plus souvent responsable, l’arthrite septique était encore plus fréquente, ce qui souligne la nécessité de pratiquer une aspiration articulaire.
Diverses conditions non infectieuses sont aussi des causes potentielles, et il faudrait porter une attention particulière aux patients présentant une leucopénie, une affection maligne et des diagnostics multiples, en raison de leur association avec de plus mauvais pronostics.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Intuitive cutoffs in conventional units were used. To convert to SI units (nmol/L), multiply by 9.524.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340(6):448–54. doi: 10.1056/NEJM199902113400607. Erratum in: N Engl J Med 1999;340(17):1376. [DOI] [PubMed] [Google Scholar]
- 2.Koenig W, Löwel H, Baumert J, Meisinger C. C-reactive protein modulates risk prediction based on the Framingham score: implications for future risk assessment: results from a large cohort study in southern Germany. Circulation. 2004;109(11):1349–53. doi: 10.1161/01.CIR.0000120707.98922.E3. Epub 2004 Mar 15. [DOI] [PubMed] [Google Scholar]
- 3.Chaturvedi AK, Caporaso NE, Katki HA, Wong HL, Chatterjee N, Pine SR, et al. C-reactive protein and risk of lung cancer. J Clin Oncol. 2010;28(16):2719–26. doi: 10.1200/JCO.2009.27.0454. Epub 2010 Apr 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morley JJ, Kushner I. Serum C-reactive protein levels in disease. Ann N Y Acad Sci. 1982;389:406–18. doi: 10.1111/j.1749-6632.1982.tb22153.x. [DOI] [PubMed] [Google Scholar]
- 5.Gaitonde S, Samols D, Kushner I. C-reactive protein and systemic lupus erythematosus. Arthritis Rheum. 2008;59(12):1814–20. doi: 10.1002/art.24316. [DOI] [PubMed] [Google Scholar]
- 6.Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111(12):1805–12. doi: 10.1172/JCI18921. Erratum in: J Clin Invest 2003;112(2):299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vanderschueren S, Deeren D, Knockaert DC, Bobbaers H, Bossuyt X, Peetermans W. Extremely elevated C-reactive protein. Eur J Intern Med. 2006;17(6):430–3. doi: 10.1016/j.ejim.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 8.BC Biomedical Laboratories New MSP laboratory medicine funding agreement. Physicians’ Newsletter. 2010;XII(3):1–3. [Google Scholar]