Abstract
Background
Empirically derived and tested models are necessary to develop effective, holistic interventions to improve positive health outcomes in adolescents and young adults (AYA) with cancer, yet few exist. This paper is the second of two papers reporting on evaluation of the Resilience in Illness Model (RIM) as a predictive model to guide positive health research and practice.
Objective
To report the confirmatory model evaluation of the RIM.
Methods
A confirmatory evaluation of RIM was done using baseline data from a sample of 113 AYA aged 11 to 24 years who were undergoing hematopoietic stem cell transplant and enrolled in a randomized controlled trial of a behavioral intervention to enhance resilience. Data were analyzed using latent variable structural equation modeling.
Results
Goodness-of-fit indices supported RIM as a confirmed model and accounted for large amounts of variance in the outcomes of self-transcendence (62%) and resilience (72%), and in three of five mediators, specifically social integration (74%), courageous coping (80%), and hope-derived meaning (87%) as well as small to moderate amounts of variance in the remaining mediators of defensive coping (1%) and family environment (35%).
Conclusions
Findings establish the RIM as a plausible predictive framework for explaining ways AYA with cancer transcend their illness and achieve resilience resolution, and for guiding intervention studies in this population. Additional research is needed to explore RIM's transferability based on stage of illness, other chronic diseases, and cultural diversity.
Implications for Practice
Results support the RIM as an appropriate guide for developing and evaluating interventions to foster positive adjustment in AYA with cancer.
Adolescents and young adults (AYA) with cancer have markedly poorer outcomes throughout their cancer journey, compared to children and older adults. 1 The well documented challenges these AYA face include, but are not limited to, symptom distress, uncertainty, infertility, fear of recurrence, spiritual and existential distress, social isolation, problems with family communication and relationships, disruptions to developmental tasks (e.g. intimacy and independence), and traumatic stress symptoms. 2-7 Information and support services to address AYA concerns and challenges are lacking, and there are few well designed and tested interventions. 2, 3, 8 Between 1988 and 2015, only 12 controlled intervention studies targeting AYA were reported, and of these only 7 were guided by an explicit theoretical framework. 9, 10
In addition to the unmet needs of AYA with cancer, there are few empirically derived and tested models to guide research for this population. 11 Such models are necessary to develop effective, holistic interventions aimed at improving AYA positive health outcomes. To explain how positive health is fostered in AYA, the Resilience in Illness Model (RIM) was developed through a series of qualitative and quantitative studies, using data from AYA with cancer and other chronic conditions. 12-15 This paper is the second of two papers reporting on evaluation of the RIM as a predictive model to guide research and practice. 13
In the first paper (Part 1), we described evaluation of the exploratory RIM, hereafter referred to as E-RIM. 13 To increase confidence in the ability of RIM to predict and guide intervention and outcomes research, it is important to evaluate how well the model is replicated in a different sample. This paper reports evaluation of the confirmatory RIM, hereafter referred to as C-RIM, using a sample of 113 AYA with cancer and recruited at the consenting stage of hematopoietic stem cell transplant (HSCT) to participate in a randomized clinical trial of a therapeutic music video intervention. 16 The data obtained for use in this study was funded by the National Institute of Nursing Research (R01NR008583) and the National Cancer Institute as a Children's Oncology Group study ANUR0631 (R01NR008583; U10CA180886; UG1CA189955; U10CA098543; U10CA095861).
The Resilience in Illness Model
A detailed description of RIM development, exploratory evaluation, and listing of latent variables with definitions of RIM concepts are described in Part 1. Briefly, RIM was developed from a positive health perspective to gain understanding of factors that contribute to AYA positive adjustment to chronic illness. The final best-fitting E-RIM consisted of two risk factors, illness-related distress (uncertainty and symptom distress) and defensive coping (avoidant, fatalistic, and emotive coping); five protective factors including spiritual perspective (one's self-defined spiritual beliefs and practices), social integration (perceived support from friends and healthcare providers), family environment (adaptability, cohesion, perceived strengths), hope-derived meaning, and courageous coping (optimistic, confrontive, and supportant coping); and two outcome factors self-transcendence, measured as activities and perspectives individuals engage in to expand their boundaries; and resilience (the process of identifying or developing resources and strengths to flexibly manage stressors to gain a sense of confidence/mastery, self-transcendence, and self-esteem). The E-RIM accounted for large amounts of variance for the two outcome variables (63% for self-transcendence, 67% for resilience resolution) and one mediating variable (76% for hope-derived meaning) and small to moderate amounts of variance (18 – 52 %) for the mediating variables of defensive coping, family environment, and social integration.
DESIGN AND METHODS
For the C-RIM, the study design was a cross-sectional theory evaluation, using baseline data obtained prior to AYA assignment to experimental or low dose control intervention conditions in our randomized controlled trial. 16 Hypotheses for the C-RIM were based on the final E-RIM. 13 We hypothesized two outcomes, resilience and self-transcendence, and regarding these outcomes, we hypothesized: (a) self-transcendence will be directly influenced by courageous coping, illness-related distress and spiritual perspective, and indirectly influenced by defensive coping, family environment, and social integration; and, (b) resilience resolution will be directly influenced by courageous coping and hope-derived meaning, and indirectly influenced by defensive coping family environment, social integration, illness-related distress, and spiritual perspective.
Setting and Sample
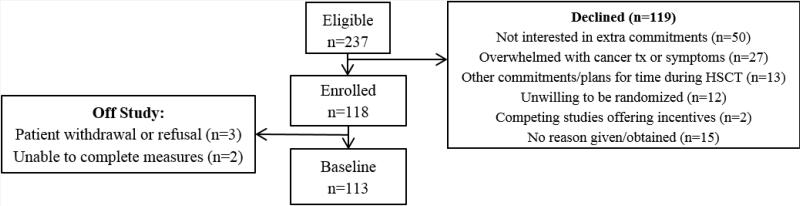
The parent study was conducted at eight sites that included 9 pediatric hospitals affiliated with the Children's Oncology Group and 3 adult hospitals affiliated with 3 of the pediatric hospitals. Participant inclusion criteria were: (a) AYA aged 11 through 24 years; (b) diagnosed with cancer and consented to receive an allogeneic or autologous stem cell transplant that required a myeloablative regimen; and (c) able to read and speak English. Exclusion criteria were: (a) having a cancer that does not usually occur in AYA populations; (b) cognitive impairments making it difficult to complete data collection instruments; and, (c) being married and/or having children. Figure 1 describes participant recruitment and accrual outcomes. Reasons for declining participation were consistent with published literature on AYA recruitment to RCT studies. 17 Demographic information for the sample is presented in Table 1. The participants, aged 11 to 24 years (M=17.3, SD=3.8), were primarily male (58%) with 83% Non-Hispanic and 58.4% Caucasian. The most common primary cancer diagnosis was leukemia (46.4%) and grouping disease status into high and low risk categories, 55% had were high risk.
Figure 1.
Recruitment
Table 1.
Baseline Demographics
| Demographics | n | Mean/% |
|---|---|---|
| Age (mean (SD); range) | 113 | 17.3 (3.8); 11-24 |
| Gender (%) | 113 | |
| Female | 42.5 | |
| Male | 57.5 | |
| Hispanic (%) | 113 | |
| No | 83.2 | |
| Yes | 16.8 | |
| Race (%) | 113 | |
| African-American | 10.6 | |
| White | 58.4 | |
| More than one race | 20.4 | |
| Othera | 6.2 | |
| Unknown or not reported | 4.4 | |
| Currently attend school (%) | 111 | |
| No | 32.4 | |
| Yes | 67.6 | |
| Level of school completed (%) | 111 | |
| Grade school | 31.5 | |
| High school | 44.1 | |
| College | 24.3 | |
| Household income (%) | 113 | |
| <$25,000 | 18.6 | |
| $25,000-$75,000 | 41.6 | |
| >$75,000 | 27.4 | |
| Unknown or not reported | 12.4 | |
| Religious activity participation (%) | 112 | |
| Inactive or infrequent | 51.8 | |
| Occasional or regular | 48.2 | |
| Employment status (%) | 112 | |
| Full-time | 7.1 | |
| Part-time | 12.5 | |
| Not employed | 80.4 | |
| Primary diagnosis (%) | 112 | |
| Leukemia | 46.4 | |
| Lymphoma | 25.0 | |
| Solid tumor | 28.6 | |
| Transplant type (%) | 112 | |
| Autologous | 40.2 | |
| Allogeneic/Syngeneic | 59.8 | |
| Disease status at transplant (%) | 111 | |
| Low risk | 54.1 | |
| High risk | 45.9 | |
Includes American Indian, Alaskan Native, Asian, Native Hawaiian, Pacific Islander and other race.
Measures
The same 20 measures used for the E-RIM evaluation listed in Table 2 were used for the C-RIM. These measures and their psychometric properties are fully described in the E-RIM manuscript, Part 1, Table 3.13 Internal consistency reliabilities (Cronbach's α) for the C-RIM measures are reported in Table 2. Cronbach's α coefficients were in an acceptable range (.75 to .94) for all measures with the exception of 3 sub-scales that each had a small number of items (i.e., 4 -5 items). As expected, Cronbach's α coefficients for these subscales were lower (.60 to .65). Construct validity of the measures in the context of AYA with cancer enrolled in this study is supported based on hypothesized intercorrelations (Table 3) and the final confirmatory measurement model (Figure 2).
Table 2.
Manifest Variables and Psychometric Properties from Baseline (N=113)
| Latent Variable/Manifest Variable | Number of items | Possible range | Mean (SD) | High score indicates greater (or more) ... | Cronbach's alpha |
|---|---|---|---|---|---|
| Illness-Related Distress | |||||
| Symptom distress | 11 | 1-5 | 1.8 (0.6) | symptom distress | .82 |
| Uncertainty in illness | 28 | 1-5 | 2.3 (0.5) | uncertainty | .89 |
| Social Integration | |||||
| Perceived social support from health care providers | 20 | 1-5 | 3.7 (0.6) | perceived support-provider | .90 |
| Perceived social support from friends | 20 | 1-5 | 4.1 (0.6) | perceived support-friends | .90 |
| Perceived social support from family | 20 | 1-5 | 4.0 (0.7) | perceived support-family | .91 |
| Spiritual Perspective | |||||
| Spirituality-practices frequency | 4 | 1-6 | 4.0 (1.5) | spirituality | .87 |
| Spirituality-beliefs | 6 | 1-6 | 4.5 (1.3) | spirituality | .94 |
| Family Environment | |||||
| Family cohesion | 16 | 1-5 | 3.7 (0.6) | cohesion | .89 |
| Family adaptability | 14 | 1-5 | 3.4 (0.6) | adaptability | .83 |
| Family communication-problem* | 10 | 1-5 | 3.2 (0.7) | communication | .82 |
| Family communication-open* | 10 | 1-5 | 4.0 (0.7) | communication | .90 |
| Family strengths | 12 | 1-5 | 3.7 (0.6) | family strength | .83 |
| Coping-Defensive | |||||
| Emotive/evasive coping | 18 | 0-3 | 1.2 (0.5) | emotive/evasive coping | .79 |
| Coping-Positive | |||||
| Confrontive coping | 10 | 0-3 | 1.4 (0.6) | confrontive coping | .80 |
| Optimistic coping | 9 | 0-3 | 2.1 (0.6) | optimistic coping | .75 |
| Supportant coping | 5 | 0-3 | 1.7 (0.6) | supportant coping | .60 |
| Hope-Derived Meaning | |||||
| Expectancy/interconnectedness | 4 | 1-5 | 4.3 (0.6) | hope | .65 |
| Positive readiness | 4 | 1-5 | 4.3 (0.6) | hope | .62 |
| Outcomes | |||||
| Self-transcendence | 15 | 1-4 | 3.3 (0.4) | self-transcendence | .75 |
| Resilience resolution | 15 | 1-6 | 5.1 (0.6) | resilience | .81 |
Mother and father measurements were combined into a single mean score.
Table 3.
Intercorrelations and Level of Significance among SMART Manifest Variables (n=113)
| Scale | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Symptom Distress | --- | ||||||||||||||||||
| 2. Uncertainty in Illness | .30 | ||||||||||||||||||
| 3. Spirituality-Frequency | .12 | −.09 | |||||||||||||||||
| 4. Spirituality-Belief | −.00 | −.05 | .75 | ||||||||||||||||
| 5. Support-Provider | .01 | −.35 | .19 | .21 | |||||||||||||||
| 6. Support-Friend | −.18 | −.37 | .19 | .10 | .34 | ||||||||||||||
| 7. Support-Family | −.14 | −.31 | .22 | .27 | .36 | .41 | |||||||||||||
| 8. Family Cohesion | −.16 | −.29 | .25 | .33 | .29 | .26 | .75 | ||||||||||||
| 9. Family Adaptability | −.11 | −.29 | .23 | .32 | .28 | .31 | .76 | .82 | |||||||||||
| 10. Family Comm-Prob | −.07 | −.23 | .24 | .19 | .25 | .31 | .60 | .52 | .62 | ||||||||||
| 11. Family Comm-Open | −.13 | −.22 | .24 | .30 | .37 | .28 | .75 | .66 | .71 | .69 | |||||||||
| 12. Family Strengths | −.28 | −.28 | .20 | .27 | .20 | .25 | .74 | .76 | .75 | .65 | .69 | ||||||||
| 13. Emotive/Evasive Coping | .19 | .03 | .19 | .11 | −.02 | .02 | −.06 | −.05 | .07 | −.16 | −.11 | −.11 | |||||||
| 14. Confrontive Coping | .04 | −.32 | .39 | .32 | .33 | .37 | .31 | .30 | .40 | .23 | .20 | .19 | .51 | ||||||
| 15. Optimistic Coping | .04 | −.40 | .35 | .33 | .29 | .41 | .31 | .27 | .32 | .19 | .20 | .24 | .36 | .65 | |||||
| 16. Supportant Coping | .18 | −.11 | .52 | .50 | .30 | .30 | .34 | .27 | .30 | .19 | .26 | .23 | .18 | .55 | .61 | ||||
| 17. Derived Meaning: Expect/Interconnect | −.24 | −.32 | .33 | .51 | .28 | .36 | .33 | .38 | .33 | .16 | .24 | .32 | −.05 | .27 | .37 | .47 | |||
| 18. Derived Meaning: Positive Readiness | −.17 | −.39 | .35 | .38 | .27 | .33 | .36 | .33 | .37 | .25 | .26 | .31 | .08 | .41 | .40 | .44 | .57 | ||
| 19. Resilience in Illness | −.33 | −.35 | .31 | .48 | .26 | .25 | .26 | .33 | .26 | .14 | .18 | .28 | −.01 | .30 | .39 | .36 | .63 | .49 | |
| 20. Self-Transcendence | −.30 | −.37 | .25 | .38 | .27 | .31 | .32 | .33 | .33 | .19 | .37 | .33 | −.04 | .30 | .40 | .35 | .50 | .37 | .45 |
Figure 2.
Measurement model
Procedures
Institutional Review Board approval for the parent study was obtained at each site prior to approaching potential participants. Baseline data were obtained following informed written consent from AYA > 17 years or assent from AYA < 18 years with parental consent. The timeframe for baseline data collection ranged from 30 days prior to AYA admission to 1 week after admission. This timeframe encompasses the pre-transplant phase, when AYA physical symptom distress is usually less severe. Data were collected in a quiet, in-hospital or clinic setting by Certified Research Associates or healthcare professionals with a graduate degree. All evaluators completed a two-day training seminar on study-specific data collection procedures prior to collecting data. Participants entered their responses directly into a secure web-based data collection site developed specifically for this study. 18 During data collection sessions, an evaluator was present the entire time to answer questions and assist with technology issues. Time to complete baseline data collection ranged from 60-90 minutes. Several strategies (e.g. evaluator training and masking, audio-recording of sessions; secure computer data entry done by the AYA) were used to insure evaluation integrity procedures. 19
Data Analyses
We used MPLUS software to perform C-RIM confirmatory factor analysis (CFA) and structural equation modeling (SEM). In addition, we used the robust version of maximum likelihood estimation, in which estimated standard errors and statistical tests are robust to violations of normality assumptions. 20 Criteria for goodness of fit were evaluated using the comparative fit index (CFI) between .92 and .99, standardized root mean square residual (SRMR) < .08, and root mean square error of approximation (RMSEA) between .06 to .09. 21 Modifications to the models were explored using the MPLUS indices for adding paths, and p-values for dropping paths to achieve the best-fitting model. 20
RESULTS
Confirmatory measurement model
Initial analysis of CFA revealed that the data fit the C-RIM reasonably well (Figure 2; CFI = 0.92, SRMR = .06, and RMSEA = .07). The 90% confidence interval for the RMSEA fit statistic (.06, .09) indicated that the estimation precision of the model was very good, despite a significant chi-square of 222.73 with 136 degrees of freedom and p < .0001. Using MPLUS indices and theory to guide decision making, 14, 15 eleven modified versions of the measurement model were investigated (e.g., two subscales of the uncertainty in illness scale were used as indicators of illness-related distress; instead of a combined score, emotive and evasive coping subscales were used as separate indicators of defensive coping; fatalistic coping was added as an indicator of defensive coping; and, religious activity was added as a third indicator of spiritual perspective).
Confirmatory structural model
The C-RIM factor analysis (CFA) presented in Figure 2 was used as the basis for testing the C-RIM structural equation model (SEM) in Figure 3. The data fit the C-RIM SEM reasonably well (CFI = 0.92, SRMR = .07, and RMSEA = .07 with a 90% CI = .05, .09). Consistent with the E-RIM, the full C-RIM accounted for high levels of variance: 72% of resilience resolution and 62% of self-transcendence. Based on these confirmed findings, to distinguish resilience as process from resilience as outcome, the latent outcome variable previously labeled “resilience” was changed to “resilience resolution.” In the C-RIM, variance of the proximal outcomes accounted for large to moderate amounts of courageous coping (80%), hope-derived meaning (87%), and social integration (74%) and small to moderate amounts of family environment (35%) and defensive coping (1%).
Figure 3.
Confirmed structural equation modeling
DISCUSSION
Findings indicated that the hypothesized C-RIM measurement model and full model fit reasonably well with baseline data of AYA undergoing stem cell transplant. Consistent with the E-RIM, the C-RIM accounted for high levels of variance in the distal outcomes of resilience resolution and self-transcendence and proximal outcomes of courageous coping, hope-derived meaning and social integration. Path differences between the E-RIM and C-RIM were anticipated due to substantive differences in the samples, including time since diagnosis and position in the cancer trajectory (i.e., newly diagnosed, relapsed, beginning stem cell transplant regimen, survivorship, end-of-life). The E-RIM included a heterogeneous sample of AYA across the cancer trajectory, on and off treatment, and with good and poor prognoses. In contrast, the C-RIM sample included only AYA beginning the process of receiving a stem cell transplant regimen. Comparison of the E-RIM and C-RIM suggests that various time points and illness circumstances influences illness-related distress, emotional availability of family and friends, coping, and hope-derived meaning. Regardless of the differences in paths across models, especially considering differences between the samples across studies, findings establish the RIM as a predictive framework that accounts for ways AYA with cancer transcend their illness and achieve resilience. The C-RIM study results support the RIM as an appropriate guide for developing and evaluating interventions to foster positive adjustment in AYA with cancer.
Resilience Redefined
Based on the E-RIM and C-RIM findings, and to distinguish resilience as process from resilience as outcome, we revised the definition of resilience presented in Part 1 as follows.
In the context of illness resilience as a process is defined as the degree to which individuals identify, develop, and/or engage protective resources (i.e., spiritual perspective, social integration, family environment, courageous coping, and hope-derived meaning) to flexibly manage illness-related stressors (i.e., illness-related distress and defensive coping) in order to achieve the two-fold outcomes, resilience resolution and self-transcendence.
In the context of illness, resilience resolution is defined as the degree to which individuals: (a) gain a sense of mastery, accomplishment and competency related to managing the illness situation; (b) are motivated to continue to maintain and improve the situation and help and inspire others; and, (c) acknowledge and accept that the illness experience contributes to, but does not predominately define oneself as a person.
This revised definition of resilience resolution closely aligns with the illness resolution described in Haase's qualitative research on courage in chronically ill adolescents, which was the basis of the Resilience in Illness measure developed to support the RIM. 14
Juxtaposition of Illness-related Distress and Spiritual Perspective as Key Influences
The juxtaposition of illness-related distress (i.e., symptom distress and illness uncertainty) and spiritual perspective (i.e., spiritual beliefs and practices) in relation to other protective and risk factors is highly compelling. Specifically, the RIM paths indicate when illness-related distress is high and/or not well-managed, the potential for AYA to successfully transcend the illness experience is likely to be significantly diminished, and the protective factors of courageous coping and social integration are likely to be less effective. Conversely, the paths indicate that when AYA have a strong spiritual perspective, resilience resolution and ability to transcend the illness are likely to be enhanced, even in the midst of illness-related distress; and, family environment, hope-derived meaning, and courageous coping are likely to be enhanced as protective factors.
Management of Illness-Related Distress
The significant direct negative paths between illness-related distress (uncertainty and symptom distress) and courageous coping, social integration, and self-transcendence underscore the importance of attending to symptoms and uncertainty as a top priority of care providers. The RIM indicates AYA will have difficulty self-transcending when illness-related distress is high and/or not well-managed. This finding is supported by other research showing strong relationships between symptom distress, uncertainty, and traumatic stress symptoms in AYA with cancer. 22-26
Uncertainty management
Although uncertainty management interventions are promising in adult populations, there remains a great need for interventions tailored to the unique developmental needs of AYA. 22, 27 Several intervention approaches are possible. First, the level of uncertainty of newly diagnosed AYA could be assessed, and then addressed and monitored as their cancer and treatment status change. To manage the uncertainty, AYA require information specific to their cancer trajectory, provided in amounts and at times that are appropriate to their age and coping skills, and in formats that are appealing and accessible. 27 Perhaps the most obvious and important intervention strategy to decrease uncertainty is increased skillful communication by healthcare providers that is timely, developmentally appropriate, and empathically delivered regarding diagnosis, prognosis, and what to expect during their treatment course. 24 Because cancer-related information is often complex, ambiguous, and emotionally difficult, providing written information and/or directing AYA to age-relevant information sources, such as web-sites, may be a helpful component of an uncertainty intervention. To take in, understand, make decisions about, and act on information relevant to their cancer journey, interventions designed to support effective expression and communication of their thoughts and emotions are needed. There is evidence that uncertainty in AYA and families also may be alleviated through social support and the expression of feelings in ways that are comfortable for AYA, such as through music and therapies.28-31 Lastly, research with childhood cancer survivors indicates that, although uncertainty can be a source of distress, when it is well attended to, it can also be a catalyst for growth, greater awareness of life purpose, development of confidence, resilience, and optimism. 28
Symptom Management
It is often difficult to assess and manage symptoms in AYA. Toxicities experienced by AYA are often more severe than those experienced by children receiving identical treatment regimens. 32 Additional research is needed to understand the differences in pharmacological responses for AYA, develop ways to assess AYA symptoms and symptom clusters, and most importantly, develop AYA specific symptom management strategies. 33, 34 Because it is often difficult to assess symptom distress in AYA, innovative strategies to obtain symptom distress information from AYA are needed, and palliative care experts should be consulted early for assessment and management of symptoms.
Spiritual Perspective
The RIM indicates spiritual perspective a strong protective factor for AYA, their family and friends, and it may serve as a counterbalance to illness-related distress. Despite the potential beneficial influence of spiritual perspective on outcomes, there is a paucity of research on spirituality in general and specifically for AYA. 35-37 This significant influence of spiritual perspective is supported by the National Consensus Project Guidelines and National Quality Preferred Practices for Spiritual Domain Guidelines encouraging provision of spiritual care as a fundamental component of compassionate, patient-centered, and developmentally appropriate care; 36 however, additional research is needed on ways to appropriately implement the guidelines for AYA. Additional AYA-specific research needs include: 1) evaluation and, if necessary, adaptation of existing theories of spirituality for their relevance to AYA, or development of AYA specific theories; 2) use of mixed methods approaches to provide a holistic perspective of spirituality in AYA; 3) research on AYA spiritual perspectives in the context of illness (e.g., how spiritual perspectives influence or are influenced by the illness experience); 4) interventions that help AYA express their spiritual perspectives in the context of illness; and, 5) development of measures of spiritual perspective that are based on AYA perceptions. 35
Social Integration and Family Environment
In the C-RIM, both social integration (i.e., the support AYA receive from friends and healthcare providers) and family environment (i.e., the ways families perceive their family, communicate, adapt, and are cohesive) serve as protective factors that foster hope-derived meaning and courageous coping. The influence of AYA's social network, including family, friends and connected healthcare providers is well supported in the literature; 7, 38 however, based on the C-RIM, the influence of these two factors on courageous coping, hope-derived meaning, and resilience may be mitigated when illness-related distress is high, such as during HSCT. In addition, for AYA to benefit from these protective factors, they may require assistance to maintain social relationships, inform others about their condition, deal with feeling different, and keep up with school activities. 39 A predominant theme in qualitative studies of AYA is the nature of the provider/patient relationship and the importance of connectedness. 14, 40, 41 In general, adults often struggle to effectively communicate with AYA and there are few effective interventions available that help adults learn ways to open and sustain communication with AYA about what is important to them—what their hopes, values, beliefs, and concerns are, especially related to the cancer. 10 To enact their protective roles, additional intervention research is needed on ways to help families, friends, and healthcare providers effectively care for themselves so they remain emotionally available to the AYA. Recently, there is increased attention on helping healthcare providers learn effective ways to communication that expresses emotional support for AYA, 42, 43 which has been linked to better treatment compliance and reduced depression and anxiety in AYA with cancer. 44
Interactions of Defensive and Courageous Coping
Defensive ways of coping (i.e., avoidant, emotive, and fatalistic) are most often used when a situation, such as a diagnosis of cancer or high symptom distress, is appraised as a threat. Based on stress/coping literature, defensive ways of coping are usually sustained until adequate time and resources are available to address the source of threat and/or to develop context-specific courageous coping skills to manage the threat.45 Examples of context-specific courageous coping skills for cancer are: learning more about the cancer; reframing the cancer experience from an insider perspective; adapting previous or learning new coping strategies to deal with cancer-related concerns, treatments, and procedures; and, learning comfortable ways to share cancer-related experiences with healthcare providers, family or friends. 40, 46 The RIM supports coping literature that indicates without development of courageous ways of coping over time, defensive ways of coping may become problematic, leading to risk-taking behaviors, withdrawal, and depression. 47, 48 The RIM also indicates prolonged defensive coping may be a barrier to transcendence or resilience resolution, ultimately affecting quality of life.
Hope-derived Meaning as a Pathway to Resilience Resolution
The C-RIM indicates hope-derived meaning is influenced by spiritual perspective, social integration and family environment. These three protective factors may be promising intervention targets to foster resilience resolution through hope-derived meaning. Research to understand the ways to foster hope-derived meaning directly and through these protective factors is needed. The Self-Sustaining Process Model provides a useful framework for fostering hope through self-reflection on several hope-fostering and sustaining thought processes that are congruent with the RIM (e.g. Spiritual--“God will take care of me”; Social Integration and Family Environment-“Others have hope for me”; Optimistic Courageous Coping-Knowledge of survivors).49, 50 Because AYA may have difficulty verbally communicating their experiences of coping, creative arts therapies, such music therapy interventions, offer promising alternative, effective ways to help AYA learn new and positive ways to cope with the cancer experience. 16
Study Limitations
Two study limitations identified for the E-RIM also apply to the C-RIM, specifically: 1) self-report scales that raise questions of distortion of recall, lack of objectivity, and social desirability; and, 2) cross sectional data. These limitations should be weighed in light of the importance of self-report measures as a way to describe experiences. Concerns regarding social desirability were likely negligible, given that in this study: measures had normal distribution patterns; there were very little missing data; and qualitative interview data from parents and AYA participating indicate the measures were not burdensome. A third limitation, unique to this study, was our use of a homogenous sample of AYA being admitted for HSCT. Although the homogeneity of our study sample can be viewed as a limitation, it also allowed us to examine pathways in the RIM that may vary across the cancer treatment trajectory and with treatment severity.
Research and Clinical Implications
Here we describe implications of the RIM for assessment and management of risk and protective factors. Addressing illness-related distress is crucial throughout the cancer continuum, from diagnosis through survivorship or end-of-life; however, when AYA are on active treatment--receiving chemotherapy, radiation, and/or HSCT, even the most skilled clinicians struggle to manage the symptom distress and uncertainty of their patients and families. According to the RIM, enhancing protective factors can potentially offset illness-related distress and help AYA self-transcend and attain resilience resolution.
Research Implications
Researchers should consider using the RIM to identify gaps in knowledge and to develop interventions to address both risk and protective factors in the RIM relevant to AYA. Research is needed on ways protective factors can best be assessed and fostered to help AYA self-transcend the cancer experience and achieve resilience resolution. Future research on the model should systematically assess RIM factors longitudinally over time, beginning at diagnosis and at key times in the cancer trajectory, such as following cancer response evaluations and relapse. In addition, researchers are encouraged to consider the Children's Oncology Group (COG) Nursing Discipline Committee's adapted RIM to guide research with a broader population of pediatric cancer patients and families.51
Clinical Implications
Clinicians are encouraged to identify best practices for each protective factor. Following are just a few suggestions for clinical actions targeting RIM protective factors that could be incorporated into an AYA plan of care.
-
(a)
Spiritual Perspective. Enhance spiritual care by routinely and systematically assessing and addressing spiritual distress (e.g., despair/hopelessness, need for reconciliation, anger at God) and meeting spiritual needs (e.g., ask about spiritual beliefs and practices and supporting their use). 35, 36
-
(b)
Hope-derived Meaning. Foster realistic hope by providing clear and accurate information about the cancer prognosis and treatment options and by encouraging reflection on experiences among AYA, family, and friends, focusing on what is meaningful and important to them in the midst having cancer.
-
(c)
Social Integration. Acknowledge the difficulty of missing out with friends and facilitate AYA efforts to stay connected with friends and other cancer survivors as sources of support.39 Foster connectedness by encouraging healthcare providers to use strategies that foster a sense of connectedness, such as being watchful and attentive to the AYA's unique needs; displaying a willingness to foster a relationship; using humor; and communicating in a way that conveys respect, and assuring respectful care that supports AYA autonomy to the fullest extent possible.
-
(d)
Assess and address family distress, so parents can be emotionally available to their AYA. Help parents learn active listening skills to communicate with their AYA through active listening.
-
(e)
Evaluate the repertoire of coping skills AYAs have and use, assisting them to evaluate the effectiveness of any defensive coping strategies while working to enhance positive coping skills. Specifically, assist AYA to: acquire needed information about their cancer and treatments; gain an optimistic perspective (e.g., through upward and downward comparisons of AYA who are doing well and not doing well); and feel comfortable asking for support from others.
In closing, the RIM has promising research and clinical implications for reducing risk and enhancing positive health and well-being. While it is beyond the scope of this paper to comprehensively discuss all the potential ways the RIM may be used to guide research and practice, the RIM does provide a “big picture” view of ways to address both risk and protective factors. Researchers may find the RIM a useful guide for designing interventions and to identify meaningful measures and outcomes to target. The RIM may also facilitate clinicians’ efforts to systematically adopt a holistic approach to care for AYA with cancer.
Acknowledgments
Funding: National Institute of Nursing Research R01NR008583; National Cancer Institute [Children's Oncology Group NCTN Operations Center Grant (U10CA180886); NCORP Grant (UG1CA189955); Chair's Grant (U10CA098543); and CCOP Grant (U10CA095861)]
Footnotes
The authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.Shaw PH, Reed DR, Yeager N, Zebrack B, Castellino SM, Bleyer A. Adolescent and young adult (AYA) oncology in the United States: A specialty in its late adolescence. J Pediatr Hematol Oncol. 2015;37(3):161–169. doi: 10.1097/MPH.0000000000000318. [DOI] [PubMed] [Google Scholar]
- 2.Smith AW, Parsons HM, Kent EE, et al. Unmet support service needs and health-related quality of life among adolescents and young adults with cancer: The AYA HOPE Study. Front Oncol. 2013;3:75. doi: 10.3389/fonc.2013.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keegan TH, Lichtensztajn DY, Kato I, et al. Unmet adolescent and young adult cancer survivors information and service needs: a population-based cancer registry study. J Cancer Surviv. 2012;6(3):239–250. doi: 10.1007/s11764-012-0219-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Docherty SL, Kayle M, Maslow GR, Santacroce SJ. The adolescent and young adult with cancer: A developmental life course perspective. Semin Oncol Nurs. 2015;31(3):186–196. doi: 10.1016/j.soncn.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Linder LA, Ameringer S, Baggott C, et al. Measures and methods for symptom and symptom cluster assessment in adolescents and young adults withcCancer. Semin Oncol Nurs. 2015;31(3):206–215. doi: 10.1016/j.soncn.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Kwak M, Zebrack BJ, Meeske KA, et al. Prevalence and predictors of post-traumatic stress symptoms in adolescent and young adult cancer survivors: a 1-year follow-up study. Psychooncology. 2013;22(8):1798–1806. doi: 10.1002/pon.3217. [DOI] [PubMed] [Google Scholar]
- 7.Zebrack B, Isaacson S. Psychosocial care of adolescent and young adult patients with cancer and survivors. J Clin Oncol. 2012;30(11):1221–1226. doi: 10.1200/JCO.2011.39.5467. 10. [DOI] [PubMed] [Google Scholar]
- 8.Zebrack BJ, Block R, Hayes-Lattin B, et al. Psychosocial service use and unmet need among recently diagnosed adolescent and young adult cancer patients. Cancer. 2013;119(1):201–214. doi: 10.1002/cncr.27713. [DOI] [PubMed] [Google Scholar]
- 9.Sansom-Daly UM, Peate M, Wakefield CE, Bryant RA, Cohn RJ. A systematic review of psychological interventions for adolescents and young adults living with chronic illness. Health Psychol. 2012;31(3):380–393. doi: 10.1037/a0025977. [DOI] [PubMed] [Google Scholar]
- 10.Phillips CR, Davis LL. Psychosocial interventions for adolescents and young adults with cancer. Semin Oncol Nurs. 2015;31(3):242–250. doi: 10.1016/j.soncn.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 11. [April 14, 2016];Medicine Io. Proceedings National Cancer Policy Forum/LIVESTRONG Workshop on Addressing the needs of adolescents and young adults with cancer. Available at: http://www.nationalacademies.org/hmd/Activities/Disease/NCPF/2013-JUL-15.aspx.
- 12.Haase JE. The adolescent resilience model as a guide to interventions. J Pediatr Oncol Nurs. 2004;21(5):289–299. doi: 10.1177/1043454204267922. discussion 300-304. [DOI] [PubMed] [Google Scholar]
- 13.Haase JE, Kintner EK, Monahan PO, Robb SL. The resilience in illness model, part 1: exploratory evaluation in adolescents and young adults with cancer. Cancer Nurs. 2014;37(3):E1–12. doi: 10.1097/NCC.0b013e31828941bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haase JE. Components of courage in chronically ill adolescents: a phenomenological study. ANS Adv Nurs Sci. 1987;9(2):64–80. doi: 10.1097/00012272-198701000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Haase JE, Heiney SP, Ruccione KS, Stutzer C. Research triangulation to derive meaning-based quality-of-life theory: Adolescent resilience model and instrument development. Int J Cancer Suppl. 1999;12:125–131. doi: 10.1002/(sici)1097-0215(1999)83:12+<125::aid-ijc22>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 16.Robb SL, Burns DS, Stegenga KA, et al. Randomized clinical trial of therapeutic music video intervention for resilience outcomes in adolescents/young adults undergoing hematopoietic stem cell transplant: a report from the Children's Oncology Group. Cancer. 2014;120(6):909–917. doi: 10.1002/cncr.28355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hendricks-Ferguson VL, Cherven BO, Burns DS, et al. Recruitment strategies and rates of a multi-site behavioral intervention for adolescents and young adults with cancer. J Pediatr Health Care. 2012 doi: 10.1016/j.pedhc.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Musick BS, Robb SL, Burns DS, et al. The development and use of a web-based data management system for a randomized clinical trial of adolescents and young adults. CIN: Computers, Informatics, Nursing. 2011;29(6):337–343. doi: 10.1097/NCN.0b013e3181fcbc95. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phillips-Salimi CR, Donovan Stickler MA, Stegenga K, Lee M, Haase JE. Principles and strategies for monitoring data collection integrity in a multi-site randomized clinical trial of a behavioral intervention. Research in Nursing & Health. 2011;34(4):362–371. doi: 10.1002/nur.20440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muthen LK, Muthen BO. Mplus User's Guide. 5th ed. Muthen & Muthen; Los Angeles: 1998-2007. [Google Scholar]
- 21.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Convential criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- 22.Santacroce SJ, Lee YL. Uncertainty, posttraumatic stress, and health behavior in young adult childhood cancer survivors. Nurs Res. 2006;55(4):259–266. doi: 10.1097/00006199-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Santacroce SJ. Parental uncertainty and posttraumatic stress in serious childhood illness. J Nurs Scholarsh. 2003;35(1):45–51. doi: 10.1111/j.1547-5069.2003.00045.x. [DOI] [PubMed] [Google Scholar]
- 24.Fortier MA, Batista ML, Wahi A, Kain A, Strom S, Sender LS. Illness uncertainty and quality of life in children with cancer. J Pediatr Hematol Oncol. 2013;35(5):366–370. doi: 10.1097/MPH.0b013e318290cfdb. [DOI] [PubMed] [Google Scholar]
- 25.Stewart JL, Mishel MH, Lynn MR, Terhorst L. Test of a conceptual model of uncertainty in children and adolescents with cancer. Res Nurs Health. 2010;33(3):179–191. doi: 10.1002/nur.20374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kwak M, Zebrack BJ, Meeske KA, et al. Prevalence and predictors of post-traumatic stress symptoms in adolescent and young adult cancer survivors: a 1-year follow-up study. Psychooncology. 2012 doi: 10.1002/pon.3217. [DOI] [PubMed] [Google Scholar]
- 27.Decker CL, Haase JE, Bell CJ. Uncertainty in adolescents and young adults with cancer. Oncol Nurs Forum. 2007;34(3):681–688. doi: 10.1188/07.ONF.681-688. [DOI] [PubMed] [Google Scholar]
- 28.Parry C. Embracing uncertainty: An exploration of the experiences of childhood cancer survivors. Qual Health Res. 2003;13(2):227–246. doi: 10.1177/1049732302239600. [DOI] [PubMed] [Google Scholar]
- 29.Bradt J, Potvin N, Kesslick A, et al. The impact of music therapy versus music medicine on psychological outcomes and pain in cancer patients: a mixed methods study. Support Care Cancer. 2015;23(5):1261–1271. doi: 10.1007/s00520-014-2478-7. [DOI] [PubMed] [Google Scholar]
- 30.Robb SL. Coping and chronic illness: Music therapy for children and adolescents with cancer. In: Robb SL, editor. Music therapy in pediatric healthcare: Research and evidence-based practice. American Music Therapy Association; Silver Spring, MD: 2003. pp. 101–136. [Google Scholar]
- 31.Potvin N, Bradt J, Kesslick A. Expanding perspective on music therapy for symptom management in cancer care. J Music Ther. 2015;52(1):135–167. doi: 10.1093/jmt/thu056. [DOI] [PubMed] [Google Scholar]
- 32.Bukowinski AJ, Burns KC, Parsons K, Perentesis JP, O'Brien MM. Toxicity of cancer therapy in adolescents and young Adults (AYAs). Semin Oncol Nurs. 2015;31(3):216–226. doi: 10.1016/j.soncn.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 33.Ameringer S, Erickson JM, Macpherson CF, Stegenga K, Linder LA. Symptoms and symptom clusters identified by adolescents and young adults with cancer using a symptom heuristics App. Res Nurs Health. 2015;38(6):436–448. doi: 10.1002/nur.21697. [DOI] [PubMed] [Google Scholar]
- 34.Erickson JM, Macpherson CF, Ameringer S, Baggott C, Linder L, Stegenga K. Symptoms and symptom clusters in adolescents receiving cancer treatment: a review of the literature. Int J Nurs Stud. 2013;50(6):847–869. doi: 10.1016/j.ijnurstu.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 35.Taylor EJ, Petersen C, Oyedele O, Haase J. Spirituality and spiritual care of adolescents and young adults with cancer. Semin Oncol Nurs. 2015;31(3):227–241. doi: 10.1016/j.soncn.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 36.Puchalski C, Ferrell B, Virani R, et al. Improving the quality of spiritual care as a dimension of palliative care: the report of the Consensus Conference. J Palliat Med. 2009 Oct;12(10):885–904. doi: 10.1089/jpm.2009.0142. [DOI] [PubMed] [Google Scholar]
- 37.Ferrell B. Meeting spiritual needs: what is an oncologist to do? J Clin Oncol. 2007;25(5):467–468. doi: 10.1200/JCO.2006.09.3724. [DOI] [PubMed] [Google Scholar]
- 38.Woodgate RL. The importance of being there: perspectives of social support by adolescents with cancer. J Pediatr Oncol Nurs. 2006;23(3):122–134. doi: 10.1177/1043454206287396. [DOI] [PubMed] [Google Scholar]
- 39.Phillips-Salimi CR, Haase JE, Kooken WC. Connectedness in the context of patient-provider relationships: A concept analysis. J Adv Nurs. 2012;68(1):230–245. doi: 10.1111/j.1365-2648.2011.05763.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hinds PS. Fostering coping by adolescents with newly diagnosed cancer. Seminars in Oncology Nursing. 2000;16(4):317–327. doi: 10.1053/sonu.2000.16590. discussion 328-336. [DOI] [PubMed] [Google Scholar]
- 41.Haase JE, Rostad M. Experiences of completing cancer therapy: Children's perspectives. Oncol Nurs Forum. 1994;21(9):1483–1492. discussion 1493-1484. [PubMed] [Google Scholar]
- 42.Mellblom AV, Korsvold L, Ruud E, Lie HC, Loge JH, Finset A. Sequences of talk about emotional concerns in follow-up consultations with adolescent childhood cancer survivors. Patient Educ Couns. 2016;99(1):77–84. doi: 10.1016/j.pec.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 43.Essig S, Steiner C, Kuehni CE, Weber H, Kiss A. Improving communication in adolescent cancer care: A multiperspective study. Pediatr Blood Cancer. 2016 doi: 10.1002/pbc.26012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ramphal R, Meyer R, Schacter B, Rogers P, Pinkerton R. Active therapy and models of care for adolescents and young adults with cancer. Cancer. 2011;117(10 Suppl):2316–2322. doi: 10.1002/cncr.26048. [DOI] [PubMed] [Google Scholar]
- 45.Lazarus RS, Folkman S. Stress, Appraisal and Coping. Springer; New York: 1984. [Google Scholar]
- 46.Decker C, Phillips CR, Haase JE. Information needs of adolescents with cancer. J Pediatr Oncol Nurs. 2004;21(6):327–334. doi: 10.1177/1043454204269606. [DOI] [PubMed] [Google Scholar]
- 47.Cooke L, Chung C, Grant M. Psychosocial care for adolescent and young adult hematopoietic cell transplant patients. J Psychosoc Oncol. 2011;29(4):394–414. [PMC free article] [PubMed] [Google Scholar]
- 48.Wells KJ, Booth-Jones M, Jacobsen PB. Do coping and social support predict depression and anxiety in patients undergoing hematopoietic stem cell transplantation? J Psychosoc Oncol. 2009;27(3):297–315. doi: 10.1080/07347330902978947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hinds P, Martin Janni. Hopefulness and the self sustaining process in adolescents with cancer. Nursing Research. 1988;37(6):336–340. [PubMed] [Google Scholar]
- 50.Ishibashi A, Ueda R, Kawano Y, Nakayama H, Matsuzaki A, Matsumura T. How to improve resilience in adolescents with cancer in Japan. Journal of Pediatric Oncology Nursing. 2010;27(2):73–93. doi: 10.1177/1043454209356786. [DOI] [PubMed] [Google Scholar]
- 51.Kelly KP, Hooke MC, Ruccione K, Landier W, Haase J. Children's Oncology Group nursing research framework. Semin Oncol Nurs. 2014;30(1):17–25. doi: 10.1016/j.soncn.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]