Abstract
The intestinal environment harbors a large number of activated T cells, which are potentially inflammatory. To prevent inflammatory responses, intestinal T cells are controlled by various tolerogenic mechanisms, including T cell apoptosis. We investigated the expression mechanism and function of the purinergic receptor P2X7 in contraction of intestinal CD4+ effector T cells. We found that P2X7 up-regulation on CD4+ effector T cells is induced by retinoic acid through retinoic acid receptor α (RARα) binding to an intragenic enhancer region of the P2rx7 gene. P2X7 is highly expressed by most intestinal αβ and γδ T cells, including Th1 and Th17 cells. The intestinal effector T cells are effectively deleted by P2X7 activation-dependent apoptosis. Moreover, P2X7 activation suppressed T cell-induced colitis in Rag1−/− mice. The data from vitamin A-deficient and P2rx7−/− mice indicate that the retinoic acid-P2X7 pathway is important in preventing aberrant build-up of activated T cells. We conclude that retinoic acid controls intestinal effector T cell populations by inducing P2X7 expression. These findings have important ramifications in preventing inflammatory diseases in the intestine.
Introduction
The intestinal immune system is in a state of constant activation due to the ample presence of foreign antigens and microbial products in the gut lumen. The majority of intestinal CD4+ T cells are activated cells, and many of these T cells recognize antigens generated by commensal bacteria.1 While intestinal effector T cells play important roles in regulating the gut microbiota and mounting immune responses to pathogens, activated T cells can mediate adverse inflammatory responses, leading to colitis, allergic responses or other chronic inflammatory diseases. To prevent inflammatory responses, the intestinal immune system must have effective tolerance mechanisms. Major mechanisms of immune tolerance in the intestine include generation and maintenance of FoxP3+ and/or IL-10+ regulatory T cells, induction of anergic lymphocytes, and disposal of excessive effector cells, the latter of which is called effector cell contraction.2, 3 T cell contraction is mediated by apoptotic signaling induced by activation-induced cell death (AICD) pathways mediated by FAS/FASL, perforin, TCR proximal kinases, reactive oxygen species (ROS), and P2X7 signaling.4–10
P2X7 is a purinergic receptor and adenosine triphosphate (ATP)-gated cation channel.11 P2X7 is activated by nicotinamide adenine dinucleotide (NAD)-induced adenosine diphosphate (ADP)-ribosylation, which is catalyzed by the enzyme ADP-ribosyltransferase (ART) 2 in rodents.12 P2X7 is also activated by high levels of extracellular ATP.13 Activation of P2X7 induces rapid influx of cations, intracellular signaling, and pore formation on the cell membrane for apoptosis.14 P2X7 is expressed by T cells, macrophages, mast cells, epithelial cells and neuronal cells.15–17 P2X7 activation can lead to inflammasome activation and cytokine expression in monocytic lineage cells.18–20 T cell subsets such as FoxP3+ T cells, cytotoxic T cells, and follicular helper T cells express P2X7 and are sensitive to P2X7-mediated cell death,4, 5, 21, 22 which can either suppress or enhance immunity depending on the function of each cell type. In humans, loss-of-function polymorphisms in the P2rx7 gene are linked to chronic lymphocytic leukemia and increased susceptibility to pathogens such as Mycobacterium tuberculosis.23, 24 It has been reported that naive/resting CD4+ T cells and retinoic acid (RA)-treated CD8+ T cells express P2X7,4, 25 but the expression mechanism and the function of P2X7 in intestinal T cell homeostasis remain poorly elucidated.
We studied the regulation mechanism of P2rx7 expression and the function of P2X7 in regulating effector T cells, particularly Th1 and Th17 cells, in the intestine. Here, we report that RA induces P2X7 expression in Th1 and Th17 cells in the intestine through activating an RA-responsive enhancer region in the mouse P2rx7 gene. P2X7 deficiency leads to aberrant expansion of Th1 and Th17 cells in the small intestine. NAD-dependent ADP-ribosylation of P2X7 induces the contraction of intestinal Th1 and Th17 cell populations in the steady state and during active immune responses to bacterial pathogens. NAD treatment also depleted inflammatory effector T cells and suppressed tissue inflammation in the intestine. Our results provide a regulatory mechanism for P2X7 expression in effector T cells and identify a role for the RA-induced P2X7 in control of inflammatory T cells in the intestine.
Results
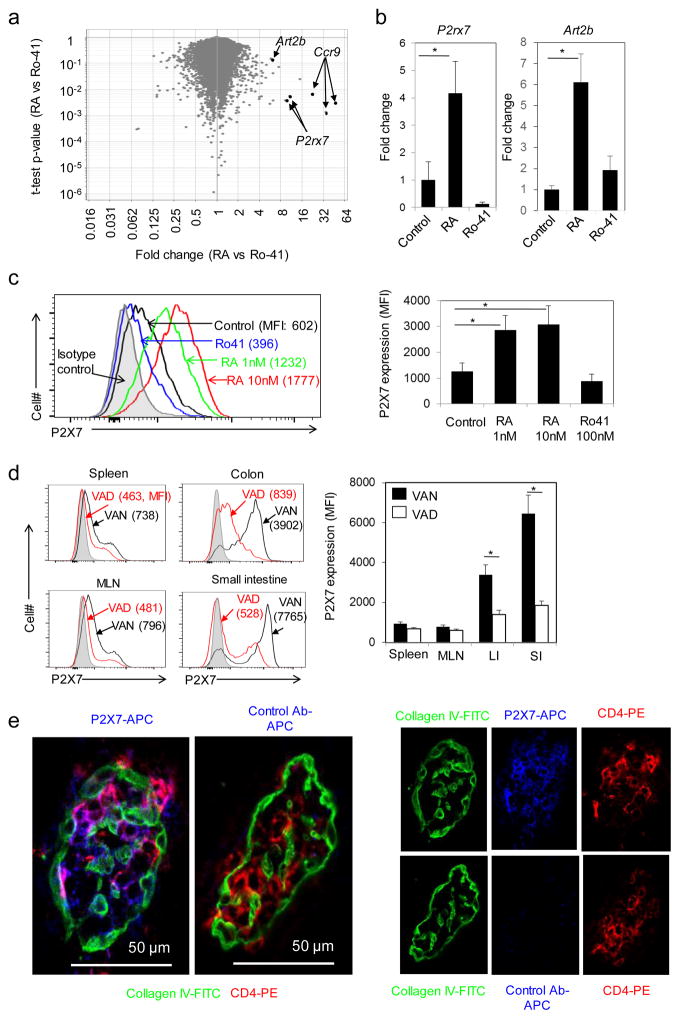
RA induces the expression of P2rx7 and Art2b in intestinal CD4+ T cells
Transcriptome analysis of cultured mouse CD4+ T cells revealed that P2rx7 expression is induced by RA but suppressed by an RARα antagonist, Ro41-5253 (Figure 1a). A follow-up qRT-PCR examination confirmed that RA greatly induced P2rx7 expression, whereas the RARα antagonist Ro41-5253 suppressed its expression in cultured CD4+ T cells (Figure 1b). Along with P2rx7, the expression of the gene for the ADP-ribosyltransferase (ART2.2), Art2b, was also induced by RA (Figure 1b). Utilizing a highly sensitive 3-step antibody staining method, we also found that RA induces P2X7 protein expression on the surface of activated CD4+ T cells (Figure 1c). To further study the impact of RA on P2X7 expression in vivo, we utilized vitamin A-deficient (VAD) mice and examined P2X7 expression by CD4+ T cells in the small intestine, colon, MLN, and spleen in vivo. We found that small intestinal (SI) and large intestinal (LI) CD4+ T cells highly expressed P2X7 whereas those in lymphoid tissues expressed P2X7 only at basal levels (Figure 1d). Importantly, the P2X7 expression on intestinal CD4+ T cells was greatly decreased in VAD mice (Figure 1d), indicating a positive role of vitamin A in P2X7 expression by CD4+ T cells. Immunofluorescence staining revealed that most CD4+ T cells in the lamina propria (LP), along with intraepithelial T cells, expressed P2X7 in intestinal villi (Figure 1e).
Figure 1. RA induces P2X7 expression in CD4+ T cells in vitro and in vivo.
(a) A volcano plot for genes up- or down-regulated by RA (10 nM) versus RAR antagonist (Ro41-5253, 100 nM) in activated CD4+ T cells. (b) Expression levels of P2x7 and Art2b mRNA in CD4+ T cells activated in the presence of RA or Ro41-5253. Relative expression levels of P2rx7 and Art2b mRNA are shown. (c) Expression of surface P2X7 protein on CD4+ T cells activated in the presence of RA or Ro41-5253. Mean fluorescence intensity (MFI) of P2X7 staining determined by flow cytometry is shown. Naive CD4+ T cells were cultured with concanavalin A (a, c) or anti-CD3/CD28 (b) in the presence of IL-2 and RA (or Ro41-5253) for 3 (a, b) or 5 (c) days. (d) CD4+ T cells from the spleen, mesenteric lymph node (MLN), the lamina propria (LP) of the small intestine (SI), and the LP of the large intestine (LI) of VAN and VAD mice were examined for P2X7 expression by flow cytometry. (e) Expression of P2X7 by T cells in intestinal villi. Confocal microscopy was performed on fluorescent antibody-stained frozen sections of SI tissues (250× original magnification). Representative and combined data (n=3 for b, c, d; n=5 for e) are shown. All error bars indicate SEM. *Significant differences from control or between two groups.
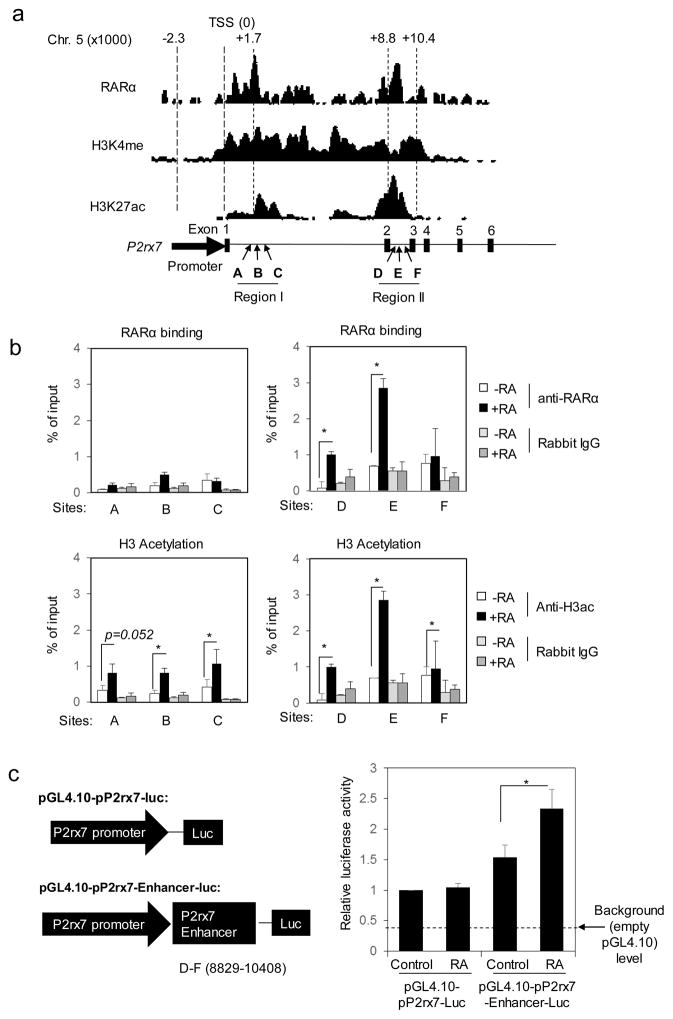
The sensitivity of the P2rx7 gene to RA is regulated by an intragenic enhancer region
RA induces gene expression by activating RAR-RXR receptors that bind RA-responsive elements (RAREs) on many genes. Analysis of published ChIP-Seq data26 indicates the presence of two major intragenic RARα binding regions (I and II) in the mouse P2rx7 gene (Figure 2a). However, the putative P2rx7 promoter region did not have any significant RARα binding activity. The RARα binding regions had epigenetic modifications such as H3K4me and H3K27Ac, which are consistent with high transcriptional activity.27 T cell activation in the presence of RA induced RARα binding and H3 acetylation on region II (Figure 2b). The enhancer activity of region II, which is located between exon 2 and 3, was tested in primary CD4+ T cells by a luciferase reporter assay. RA-dependent transcriptional reporter activity was detected when region II was ligated downstream of the P2rx7 promoter in the luciferase reporter plasmid (Figure 2c). Therefore, this region has an RA-dependent enhancer activity and is referred to as “the RA-responsive P2rx7 enhancer.”
Figure 2. An enhancer region in the P2X7 gene has binding sites for RARα and makes the P2X7 gene responsible to RA.
(a) The structure of P2rx7 promoter and enhancer regions along with RARα binding, H3K4 methylation, and H3K27 acetylation. (b) RARα binding and H3 acetylation at putative P2rx7 enhancer regions. A ChIP assay was performed using anti-RARα and anti-acetylated H3 on CD4+ naive T cells activated with anti-CD3/CD28 for 3 days in the presence of RA or Ro41-5253. (c) The transcriptional activity of the P2rx7 enhancer region was determined with a luciferase reporter assay. Reporter plasmids were transfected into activated CD4+ T cells, cultured for 6 hours in the presence or absence of RA, and assayed for luciferase activity. Relative luciferase units (RLU) normalized by PGL4-P2rx7 control levels are shown. Combined data from 3–6 independent experiments are shown. *Significant differences between indicated groups.
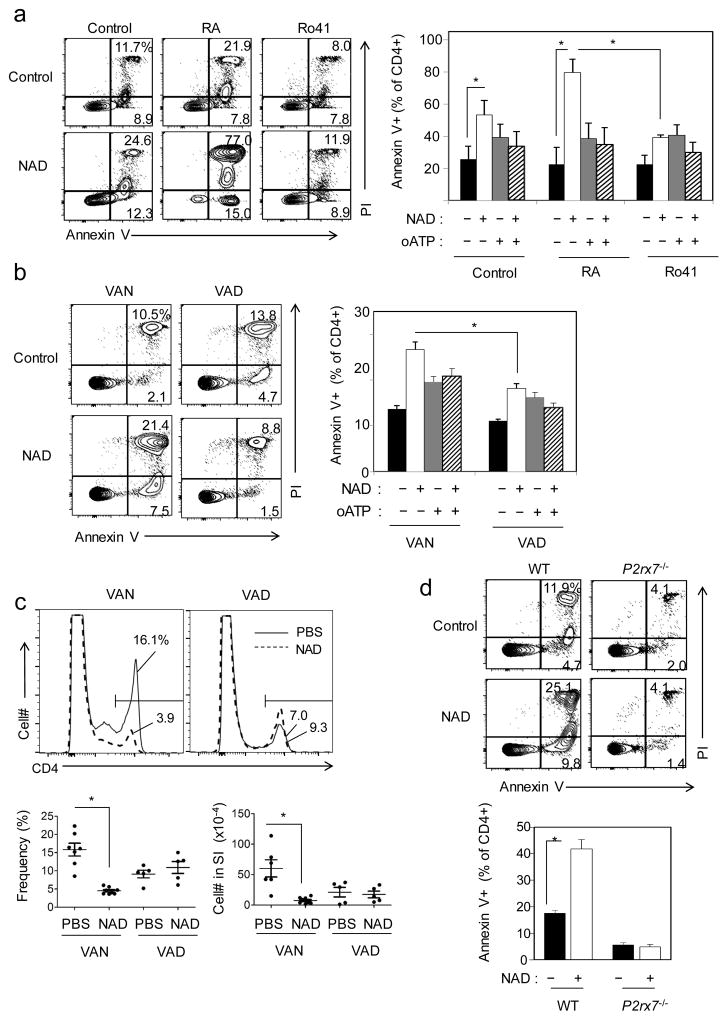
RA makes CD4+ T cells susceptible to NAD-induced apoptosis in a P2X7-dependent manner
P2X7 activation on T cells induces phosphatidylserine exposure and apoptosis.14 Because of the differential expression of P2X7 by RA- and Ro41-5253-treated T cells, we compared their sensitivity to NAD-induced apoptosis. RA-treated CD4+ T cells were highly sensitive to NAD-induced apoptosis, whereas Ro41-5253-treated T cells were insensitive to NAD (Figure 3a). This dependence on RA was observed on CD4+ T cells, activated with different T cell activators such as concannavalin A (Figure 3a) and OVA323–339 (not shown). oATP (an irreversible antagonist for P2X7) effectively blocked the NAD-induced apoptosis. Moreover, the CD4+ T cells, isolated from the MLN of VAN mice, were significantly more susceptible to NAD-induced apoptosis than their counterparts from VAD mice (Figure 3b). Next, we examined the sensitivity of intestinal T cells to NAD-induced apoptosis in vivo following i.v. injection of NAD into mice. The CD4+ T cells of the SI of VAN mice were effectively depleted following NAD injection, while those in VAD mice were resistant to NAD-induced cell death (Figure 3c). While wild type T cells, induced for P2X7 expression with RA in vitro, were sensitive to NAD-induced apoptosis, P2rx7−/− CD4+ T cells were resistant (Figure 3d). These results indicate that RA induces the expression of functional P2X7 on intestinal CD4+ T cells and P2X7 activation depletes intestinal CD4+ T cells.
Figure 3. RA increases CD4+ T cell sensitivity to NAD-induced cell death in vitro and in vivo.
(a) RA-treated CD4+ T cells are more susceptible than Ro41-treated CD4+ T cells to NAD-induced cell death. Naive CD4+ T cells were cultured with concanavalin A in the presence of IL-2 and RA (or Ro41-5253) for 4–5 days. The cells were treated with NAD (100 μM) or control media for 2 hours, and the frequency of apoptotic CD4+ cells was determined by annexin V and PI staining. (b) MLN CD4+ T cells isolated from VAD mice were relatively more resistant than those from VAN mice to NAD-induced cell death. (c) P2X7+ SI CD4+ T cells were preferentially depleted by NAD-induced cell death in vivo. Mice were injected i.v. with NAD (10 mg/mouse), and numbers of CD4+ T cells were determined by flow cytometry twenty hours after the NAD injection. (d) P2rx7−/− cells are resistant to NAD-induced cell death. Cultured CD4+ T cells from WT and P2rx7−/− mice were treated with NAD as in (a). Representative and combined data (n=3 for a, b, d; n=5 for c) are shown. *Significant differences between indicated groups.
Polymorphisms in the P2rx7 gene in C57BL/6 and BALB/c mice have been reported, leading to functional differences in P2X7 activity.28 Because of this polymorphism, we also examined P2X7 expression and function in regulating T cells in BALB/c mice. We found that the T cells from BALB/c mice expressed P2X7 in response to RA and were equally sensitive to NAD-induced apoptosis (Supplementary Figure 1a–d).
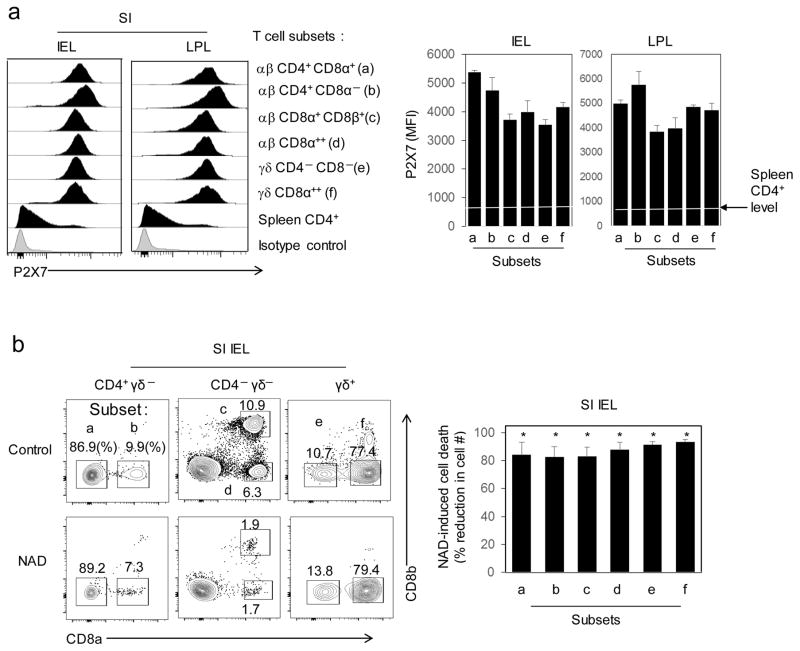
There are many αβ and γδ T cell subsets in the LP and intraepithelial compartments. We studied P2X7 expression by CD4 and/or CD8-expressing αβ and γδ T cell subsets in the SI LP and intraepithelial compartments. We found that all of the αβ (CD4+CD8α+, CD4+CD8α−, CD8α+CD8β+, and CD8α++) and γδ (CD8α++ and CD8− CD4−) T cell subsets highly expressed P2X7 and were susceptible to NAD-induced cell death (Figure 4a, b).
Figure 4. P2X7 expression and NAD-induced cell death of αβ and γδ T cell subsets in LP and intraepithelial compartments.
(a) Expression of P2X7 by various αβ and γδ T cell subsets in LP and intraepithelial compartments. (b) NAD-induced cell death of intestinal αβ and γδ T cell subsets. Mice were injected i.v. with NAD (10 mg/mouse), and numbers of CD4+ T cells were determined by flow cytometry twenty hours after the NAD injection. Representative and combined data (n=4 for a; n=8 for b) are shown. *Significant differences from control mice.
Antigenically stimulated memory/effector, but not naïve, CD4+ T cells preferentially express P2X7
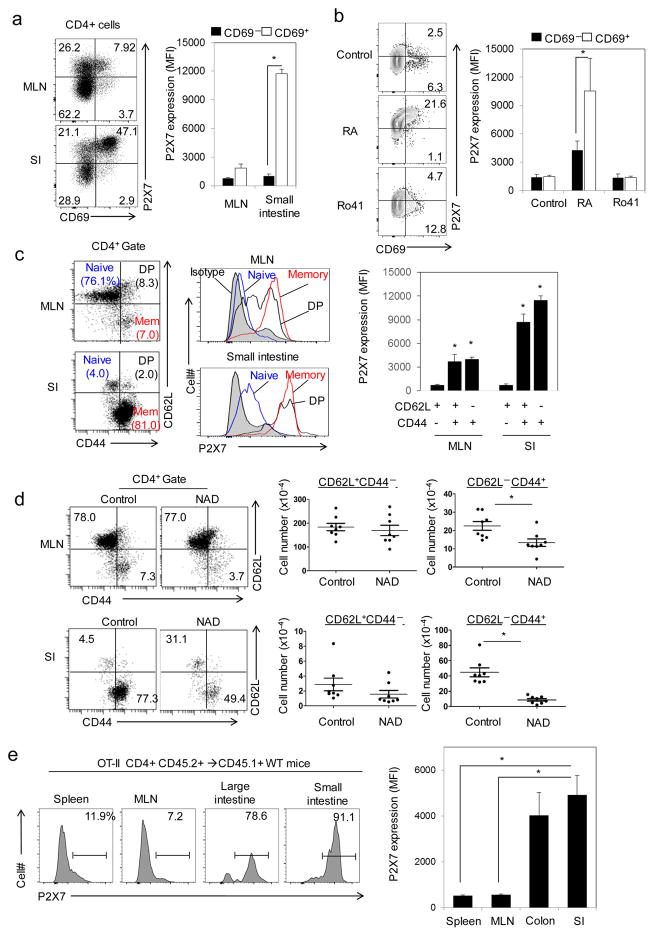
It has been proposed that naive or resting CD4+ T cells preferentially express P2X7 and are the main target of NAD-induced cell death.25 However, our data indicate that P2X7 expression is induced by RA on intestinal T cells, the majority of which are memory or effector T cells. Therefore, we closely examined the P2X7 expression by resting versus activated cells based on CD69 expression and naive versus memory/effector-like T cells based on CD62L/CD44 expression. P2X7 expression on SI CD4+ T cells was concentrated on CD69+ activated T cells compared to CD69− CD4+ cells (Figure 5a). Similarly, CD69+ CD4+ cells, generated in culture in the presence of RA, expressed higher levels of P2X7 than did CD69− CD4+ cells (Figure 5b). Moreover, P2X7 expression highly correlated with the expression of the memory/effector T cell marker CD44 and was negligible on CD62L+ CD44− naive-like CD4+ T cells (Figure 5c). In line with the pattern of P2X7 expression, NAD injection effectively depleted memory/effector CD62L− CD44+ CD4+ T cells but not naive type CD62L+CD44− CD4+ T cells (Figure 5d). Because it was previously reported that FoxP3+ T cells highly express P2X7,22 we also examined P2X7 expression by FoxP3+ T cells. For CD62L+ CD44− naive types, P2X7 expression was higher on FoxP3+ T cells, whereas it was higher on CD44+ FoxP3− memory T cells compared to CD44+ FoxP3+ memory T cells (Supplementary Figure 2a). In culture, RA induced P2X7 expression both in FoxP3− and FoxP3+ CD4+ T cells (Supplementary Figure 2b). In support of the findings, reanalysis of publicly available transcriptome data (GSE15907) for P2rx7 revealed that CD4+ CD44+ CD122+ memory T cells, but not CD4+ CD62L+ naive T cells, highly expressed this gene (Supplementary Figure 3).
Figure 5. T cell activation in the presence of RA in vitro or in the gut-tissue environment in vivo induces P2X7 expression and increases sensitivity to NAD-induced cell death.
(a) Expression of P2X7 by CD69+ versus CD69− CD4+ T cells in SI LP and MLN. (b) Expression of P2X7 by CD69+ versus CD69− CD4+ T cells activated in vitro with RA or Ro41-5253 and concanvalin A. Naive OTII CD4+ T cells were activated for 4–5 days in the presence of CD11c+ splenocytes and OVA323–339. (c) Expression of P2X7 by naive and memory/effector-like CD4+ T cell subsets distinguished by CD44 and CD62L expression. (d) Comparison of gut naive and memory/effector CD4+ T cell subsets for their sensitivity to NAD-induced cell death. (e) Antigenic stimulation induces P2X7 on CD4+ T cells preferentially in the small and large intestines. CD45.1+ mice were transferred i.v. with naive CD45.2+ OT-II T cells and immunized i.g. with ovalbumin. Representative and combined data (n=5 for a, n=3 for b, n=6 for c, n=7 for d, n=7 for e) are shown. *Significant differences from the first groups or between indicated groups.
We, next, investigated if antigen stimulation drives P2X7 expression on intestinal CD4+ T cells in vivo. We adoptively transferred ovalbumin-specific OT-II T cells into CD45.1 congenic mice and intragastrically immunized these mice with ovalbumin. The P2X7 expression on CD4+ T cells was induced by ovalbumin, and the OT-II P2X7+ cells were detected in the SI and LI but rarely in spleen and MLN (Figure 5e), indicating that antigen stimulation in the intestinal environment is required for robust induction of P2X7 expression by T cells.
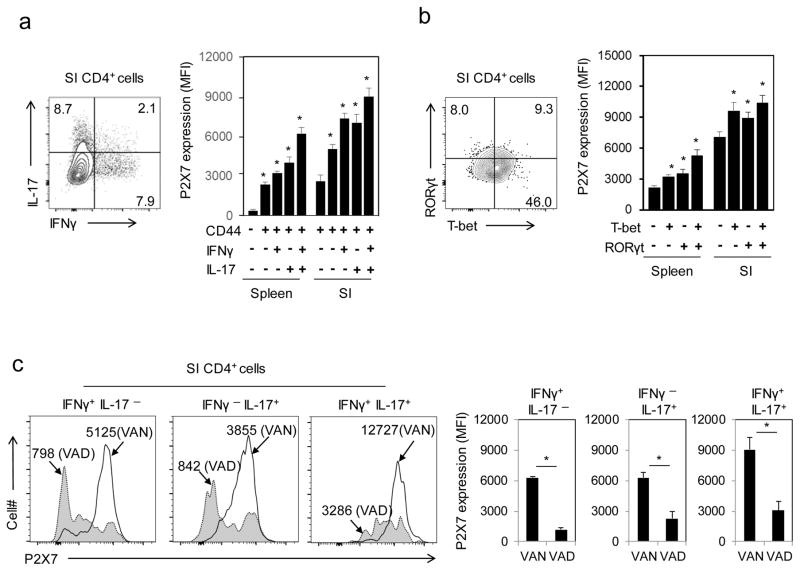
P2X7 controls the size of Th1 and Th17 cell populations in the intestine
Th1 and Th17 cells are major CD4+ memory/effector T cell subsets in the intestine. Because of the preferential expression of P2X7 by memory/effector T cells in the intestine, we examined P2X7 expression by Th1 and Th17 cells. SI Th1 and Th17 cells highly expressed P2X7 (Figure 6a), which suggests that these effector T cells are likely to be the major targets of P2X7-mediated apoptosis. In support of this, high positive correlations were found between the expression of P2X7 and T-bet or RORγt, the master transcription factors for Th1 or Th17 cells (Figure 6b). The P2X7 expression by intestinal Th1 and Th17 cells was decreased in the VAD compared to the VAN condition (Figure 6c). Moreover, RA induced P2X7 expression on in vitro-generated Th1, Th17, and Th2 cells (Supplementary Figure 4). These results identify intestinal Th1 and Th17 cells as potential targets of P2X7-mediated apoptosis.
Figure 6. Intestinal Th1 and Th17 effector cells preferentially express P2X7 in a RA or vitamin A-dependent manner.
(a) P2X7 expression by IFN-γ/IL-17-expressing CD44+ versus non-IFN-γ/IL-17-expressing CD44+ CD4+ cells. (b) Correlation between P2X7 and RORγt or T-bet expression in intestinal T cells. Expression of P2X7, T-bet and RORγt by CD4+ T cells isolated from indicated tissues of C57BL/6 mice was examined. (c) P2X7 expression by Th1 and Th17 cells in the spleen and SI of VAN and VAD mice. Representative and combined data (n=7 for a, n=6 for b and c) are shown. *Significant differences from the first groups or between two groups.
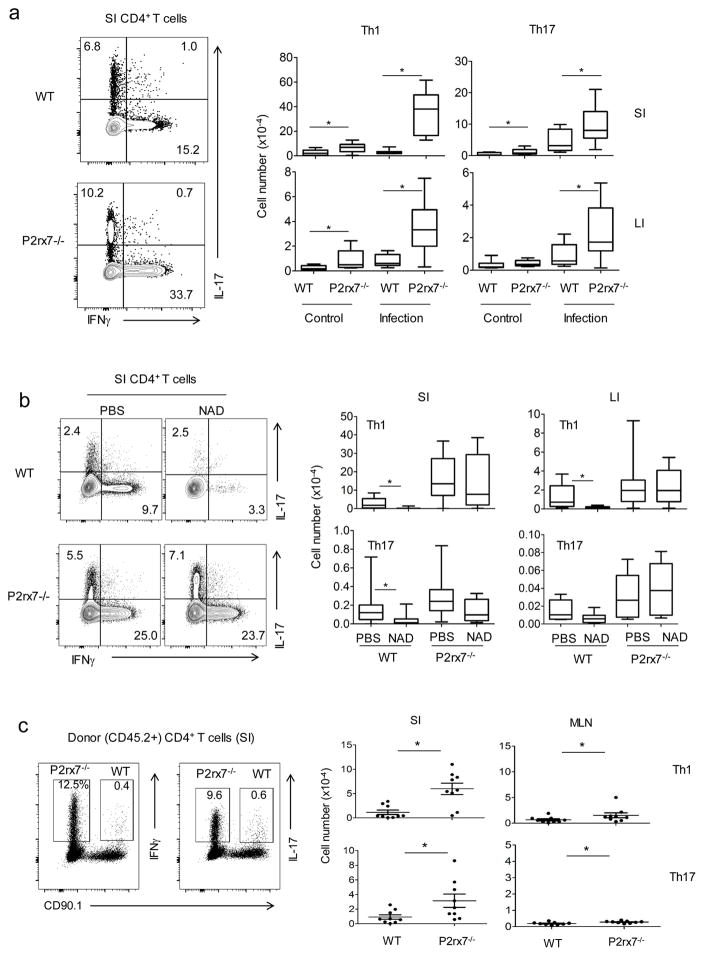
A potential function of P2X7 in the intestine is to induce apoptosis of excessive Th1 and Th17 cells. If this is the case, P2X7 deficiency would increase the numbers of Th1 and Th17 cells in the intestine. To test this hypothesis, we examined the size of Th1 and Th17 cell populations in WT versus P2rx7−/− mice during the steady state and infection by C. rodentium. The absolute numbers of Th1 cells in the SI were significantly increased in P2X7-deficient mice in the steady state and this change was even more pronounced during infection by C. rodentium (Figure 7a). The numbers of Th17 cells were also increased in the SI and LI of P2X7-defcieint mice. Interestingly, the abnormal increase of effector T cells was also observed in the MLN and spleen during infection (Supplementary Figure 5a). It was also noted that P2X7 expression by CD4+ memory/effector cells was increased at variable levels in secondary lymphoid tissues and LI during infection (Supplementary Figure 5b). We, next, administered NAD into WT and P2rx7−/− mice to determine if Th1 and Th17 cells are effectively depleted in the intestine. NAD injection depleted intestinal Th1 and Th17 cells in WT, but hardly in P2rx7−/−, mice following NAD administration or upon NAD treatment ex vivo (Figure 7b and Supplementary Figure 6a). In line with the data, Th1, Th17, and Th2 cells, generated in vitro in the presence of RA, were effectively depleted by NAD (Supplementary Figure 6b, c, d).
Figure 7. P2rx7−/− mice have aberrantly expanded populations of Th1 and Th17 cells in the steady state and during active immune responses.
(a) Frequencies and absolute numbers of Th1 and Th17 cells in the intestine of WT and P2rx7−/− mice in the steady state and during C. rodentium infection. Mice were examined 2 weeks after infection with C. rodentium. (b) Sensitivity of SI WT versus P2rx7−/− Th1 and Th17 cells to NAD-induced cell death. (c) Th1 and Th17 populations following competitive bone marrow repopulation. A 1:1 mixture of Thy1.1+ CD45.2+ WT and Thy 1.2+ CD45.2+ P2rx7−/− BM were transplanted into lethally irradiated CD45.1+ congenic mice. The mice were sacrificed 9 weeks post-BM transfer. The boxes and bars respectively represent the 25–75th and 0–100th percentile data ranges. Representative and combined data (n=11–14 for a; n=12 for b) are shown. *Significant differences between two groups.
We further performed a competitive repopulation study for WT and P2rx7−/− bone marrow (BM) cells to create mice that have both WT and P2rx7−/− hematopoietic cells in the same hosts. The SI had abnormal expansion of P2rx7−/− Th1 and Th17 cells compared to their WT counterparts in the same host (Figure 7c). Similar differences were observed in the MLN but the differences were relatively smaller. These results indicate that P2X7 is required to prevent the excessive buildup of Th1 and Th17 cell in the intestine.
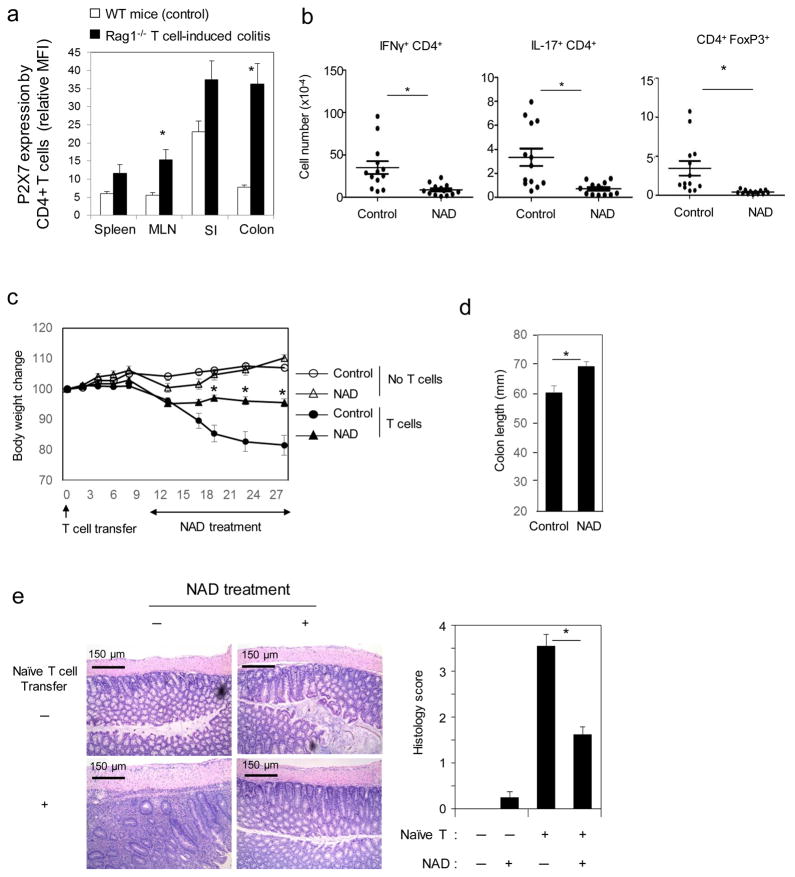
NAD administration restrained inflammatory intestinal Th1 and Th17 cells and suppressed colitis
To gain insights into the role of P2X7 in regulating inflammatory T cells in the intestine, we next examined P2X7 expression by CD4+ T cells in the T cell-induced colitis in Rag1−/− mice. P2X7 expression was up-regulated in both the SI and LI of T cell-transferred Rag1−/− mice (Figure 8a). The P2X7 expression levels on inflammatory intestinal T cells in Rag1−/− mice were significantly higher than that of normal intestinal T cells in control C57BL/6 mice. Particularly, the expression of P2X7 by CD4+ T cells in the LI of Rag1−/− mice was particularly high. This indicates a potentially important role for the P2X7 pathway in reining in inflammatory T cells. To test this hypothesis, we injected NAD into T cell-transferred Rag1−/− mice. Repeated NAD treatment depleted greater than ~90% of Th1 in the colitis model (Figure 8b). Moreover, minor populations such as Th17 and FoxP3+ cells were also depleted. NAD injection suppressed weight loss, inflammation-related colon contraction, and tissue inflammation (Figure 8c, d, e).
Figure 8. NAD administration depletes inflammatory T cells and suppresses colitis in Rag1−/− mice.
(a) Expression of P2X7 by CD4+ T cells in Rag1−/− mice following the transfer of naive CD4+ T cells. (b) Numbers of Th1 and Th17 cells in in Rag1−/− mice following injection of NAD or PBS. (c) NAD suppressed colitis-associated weight loss. (d) NAD suppressed T cell-induced colitis-associated colon shortening in Rag1−/− mice. (e) NAD suppressed tissue inflammation in the distal colon. H&E staining and histological assessment were performed. Mice were sacrificed at 4 weeks after naive T cell transfer. Representative and combined data (n=5 for a, n=13 for b, c, d, e) are shown. *Significant differences from control groups or between two groups.
Discussion
The results of this study reveal an important role of vitamin A metabolites in regulating intestinal effector T cells through P2X7 up-regulation. We identified an enhancer region that makes the murine P2rx7 gene sensitive to RA. RA-induced P2X7 is required to restrain the size of effector T cell populations in the intestine. This function of P2X7 is important in suppressing the overpopulation of effector T cells in intestinal tissues and, therefore, has the potential to prevent T cell–induced inflammatory diseases in the intestine.
It has been unclear when and how P2X7 is up-regulated on CD4+ T cells during T cell differentiation. Early studies suggested that CD4+ T cells in peripheral lymph nodes are sensitive to P2X7-induced cell death.14, 29 A key question is if there is any specificity in P2X7 expression in terms of cell type, differentiation stage, and tissue location. We systematically compared P2X7 expression by naive and memory/effector CD4+ T cell populations in the intestine and lymphoid tissues. Naive CD4+ T cells hardly expressed P2X7 but memory and effector CD4+ T cells highly expressed P2X7. Moreover, there were differences among organs (i.e. intestine versus lymphoid tissues) in P2X7 expression by T cells. In the steady state, CD4+ T cells in the SI most highly express P2X7, which is followed by those of the LI. In contrast, relatively fewer CD4+ T cells in lymphoid tissues expressed P2X7. Moreover, it was Th1 and Th17 cells that expressed P2X7 most highly in the intestine. Thus, P2X7 expression is developmentally and tissue-specifically regulated in CD4+ T cells.
A key finding of this study is the identification of an enhancer region in the mouse P2rx7 gene, which induces the gene in response to RA. RA is highly produced by dendritic cells and epithelial cells in the intestine, particularly in the SI.30 RA has pleiotropic functions in regulating the immune system.31, 32 RA affects the differentiation and function of T cells and other cell types,26, 33–37 and induces gut-homing receptors for T cell migration into the intestines.33, 35, 37 By inducing gut-homing receptors, RA populates the intestine with antigen-experienced effector T cells. While this promotes intestinal immunity, the same function can cause over-population of effector T cells and tissue inflammation. Our transcriptome analysis of RA-treated T cells indicates that P2X7 is co-expressed by T cells that express gut homing receptors such as CCR9 and Itg-α4. This indicates that gut-homing CD4+ T cells are a target of P2X7-mediated apoptosis. It has been reported that RA induces P2X7 expression in intraepithelial CD8+ T cells.4 Our data indicate that most αβ and γδ T cell subsets in intestinal LP and intraepithelial compartments express P2X7 and are susceptible to NAD-induced cell death. Therefore, the RA-P2X7 pathway is likely to affect most T cell subsets in the intestine.
The intestinal tissues harbor many effector T cells reactive to commensal bacteria and dietary antigens. ATP and NAD, the two P2X7-activating metabolites, are released from stressed or activated cells, which are generated following tissue damage and inflammatory responses. ATP can be also produced by the gut microbiota or host cells upon stimulation with commensal bacteria and pathogens.38, 39 Our results indicate that intestinal effector T cells are restrained by the P2X7-mediated apoptosis in the steady state and during inflammatory responses. This is supported by the abnormally expanded Th1 and Th17 cell populations in P2X7-deficient mice, particularly during active immune responses such as infection or inflammatory responses. In support of our findings, it has been reported that P2X7-deficient mice suffer from more severe inflammatory responses compared to WT mice following infection with Toxoplasma gondii or during an experimental inflammatory response in the CNS.40, 41 This is further supported by our data that NAD administration effectively depleted inflammatory Th1 and Th17 cells and suppressed the T cell-induced colitis into Rag1−/− mice. Thus, P2X7 controls the size of activated T cell populations in the intestine.
P2X7 is also expressed by mouse and human FoxP3+ Tregs.22, 42 For example, Aswad et al. reported that spleen Tregs express P2X7 and are more susceptible to NAD or ATP-induced apoptosis compared to non-Tregs.22 It is true that Tregs in secondary lymphoid tissues such as spleen and lymph nodes express P2X7 at levels higher than that by non-Tregs. This is due to the fact that even naive-like Tregs express P2X7 at medium levels, whereas conventional non-Treg naive CD4+ T cells hardly express P2X7. In the small intestine, however, non-Treg effector T cells express P2X7 at levels higher than Tregs. RA induces P2X7 also in FoxP3+ T cells. Therefore, RA-induced P2X7 expression probably affects both effector T cells and Tregs in the intestine. Because Tregs express P2X7 even at the naive stage, Tregs may depend less on RA in P2X7 expression than non-Tregs. We observed also that antigen stimulation is required to induce P2X7 expression in naive CD4+ T cells. Thus, the results of our study expand the role of P2X7 to memory/effector T cells, including Th1 and Th17 effector T cells. A recent study revealed that P2X7 controls the function of Tfh cells in Peyer’s patches.5 In this regard, Tfh cells are also effector CD4+ T cells, specialized in helping B cells.
In summary, effector T cells, including Th1 and Th17 cells, are effectively restrained by P2X7-dependent apoptosis in the intestine. RA induces the expression of P2X7 and ART2.2 in activated CD4+ T cells producing effector cytokines. RA induces P2X7 expression through RARα binding to an enhancer region between exon 2 and 3 on the P2rx7 gene for epigenetic modification and enhanced gene expression. We conclude that RA, the key factor that promotes T cell migration to the intestine for immunity, also plays a significant role in containing the activity of various effector T cells in the intestine. We suggest that this pathway provides a negative feedback loop in the intestinal immune network to suppress aberrant T cell activity and inflammatory diseases.
Methods
Animals and diet
All experiments with animals in this study were approved by the Purdue Animal Care and Use Committee (PACUC). P2rx7−/− mice (stock # 005576) and Rag1−/− C57BL/6 mice (stock number 002216) were purchased from the Jackson Laboratory (Bar Harbor, ME). Vitamin A-deficient (VAD) and vitamin A-normal (VAN) mice were generated by feeding late-term (15–16 days post coitus) pregnant females with AIN-93G custom diet containing retinyl acetate at 2,500 IU/kg of diet for VAN or 0 IU/kg of diet for VAD respectively (TD. 07267 and TD. 00158, Harlan Teklad, Indianapolis, IN). The weaned mice were kept on the same diet for at least 10 weeks prior to experiments.
Infection and induction of colitis
Wild type (WT) and P2rx7−/− C57BL/6 mice (6 weeks old, sex-matched males or females) were infected i.g. with C. rodentium (109 colony forming unit/mouse). Rag1−/− C57BL/6 mice were injected i.p. with naive CD4+ T cells (5×105 cells/mouse) to induce colitis. Mice were monitored for weight change and sacrificed 2 or 4 weeks later. The colon was histologically examined after hematoxylin and eosin staining. Colitis scores were assessed based on levels of leukocyte infiltration, loss of normal crypt structure, and mucosae hyperplasia on a scale of 4 by two different researchers. When indicated, NAD (20 mg; Sigma Aldrich, St. Louis, MO) was injected i.p. every 12 hours.
Bone Marrow or T cell transfer
Recipient mice were subjected to lethal γ-irradiation (1,050 rads) and reconstituted i.v. with bone marrow cells from WT and P2rx7−/− mice (4×106 cells each). Mice were examined 9 weeks after bone marrow transplantation. CD4+ naive T cells (2×106 cells/mouse), isolated from CD45.2+ OT-II mice, were transferred i.v. into CD45.1+ mice and then immunized i.g. with OVA323–339 (10 μg, Sigma Aldrich, St. Louis, MO) and cholera toxin (10 μg, Sigma Aldrich) on day 1 and 14. Mice were sacrificed 5 days after the immunization.
Cell isolation and culture
Naive CD4+ T cells, isolated as previously described,37 were cultured in complete RPMI-1640 medium supplemented with either regular or charcoal-treated fetal bovine serum. The cells were activated with concanavalin A (1.5 μg/ml, Sigma Aldrich, St. Louis, MO), OVA323–339 (for DO11.10 Rag2−/− CD4+ T cells), or plate bound anti-CD3 antibody (0.2–2 μg/ml) and soluble anti-CD28 antibody (2 μg/ml) (BioXcell, Lebanon, NH) with hIL-2 (100 U/ml) for 3–5 days. Th1, Th17 and Tregs were cultured as previously described.33, 37 Cytokines were purchased from either BioLegend (San Diego, CA) or PeproTech (Rocky Hill, NJ). T cells were cultured with RA (all-trans RA, 1–10 nM) or Ro41-5253 (100 or 500 nM, Sigma Aldrich).
Flow cytometry
Cells were stained with anti-P2X7 (clone Hano43, AbD Serotec), anti-rat IgG2b (clone MRG2b-85), PerCP/Cy5.5 or PE-Cy7 conjugated streptavidin, anti-CD4 (clone RM4-5), anti-IFNγ (clone XMG1.2), anti-IL17 (clone TC11-18H10.1), anti-FoxP3 (clone FJK-16s), anti-CD44 (clone IM7), anti-CD69 (clone H1.2F3), anti-CD62L (clone MEL-14), anti-RORγt (clone AFKJS-9), and/or anti-Tbet (clone eBio-4B10). Most antibodies were purchased from BioLegend or eBioscience. For detection of P2X7 on T cells, cells were sequentially stained with anti-P2X7 antibody, biotin-anti-rat IgG2b, and fluorochrome-conjugated streptavidin. Intracellular staining of cytokines and other antigens were performed as described previously.33
Assessment of NAD-induced T cell apoptosis
Cultured CD4+ T cells or cells isolated from the mesenteric lymph nodes (MLN) or small intestine (SI) were treated with NAD (β-Nicotinamide adenine dinucleotide hydrate, Sigma-Aldrich, 100–200 μM) for 2 hours in complete cRPMI-1640. When indicated, cells were pre-treated with periodate-oxidized ATP (oATP, a P2X7 receptor antagonist, 1 mM, Sigma Aldrich) for 2 hours before the NAD treatment. Cells were then washed twice with ice cold PBS, and then stained with antibodies to CD4, CD44, IFNγ, and IL-17. When indicated, Annexin V and PI staining was performed in Annexin V binding buffer (BioLegend). To assess the short-term depletion effect of NAD on CD4+ T cells in vivo, mice were injected i.v. with NAD (10 mg) and sacrificed 2 or 20 hours later. The results obtained at 2 and 20-hour time points were similar and all data shown in this report were obtained at the 20-hour time point.
Chromatin Immunoprecipitation (ChiP) assay
RARα binding and histone 3 (H3) acetylation sites on the P2rx7 gene were identified by analyzing publicly available ChiP-seq data (GSE60356) with Integrated Genome Browser (IGB Bioinformatics Application Note). To determine RA-dependent regulation of RARα binding and H3 acetylation sites on the P2rx7 gene, a ChiP assay was performed with the SimpleChiP® kit (Cell Signaling Technologies, Danvers, MA) using the primers described in Supplementary Table 1. Immunoprecipitation was performed using rabbit control IgG or polyclonal antibody to h/mRAR α (Santa Cruz Biotech, Santa Cruz, CA) or acetylated H3 (Millipore, Temecula, CA). Eluted DNA was analyzed by qRT-PCR using primers described in Supplementary Table 1.
Transfection and reporter assay
The 2.3 kb P2rx7 promoter and 1.6 kb enhancer regions (−2337 to −1 and +8828 to +10409 from TSS, respectively) were amplified with primers shown in Supplementary Table 1 and cloned into pGL4.10 (Promega, Madison, WI). CD4+ T cells (3x106) were activated for 2 days with anti-CD3/CD28 antibodies and transfected using the Mouse T Cell Nucleofector® Kit (Lonza, Allendale, NJ). Transfected cells were cultured for 6 h in cRPMI with charcoal treated FBS (10%) with or without RA (20 nM) before measuring luciferase activity with the Luciferase Reporter kit (Promega). Transfection efficiency in T cells was assessed by qPCR of transfected plasmids 2 days after transfection.
Confocal microscopy
SI tissues (ileum) was harvested from C57BL/6 mice (7 weeks-old) and frozen in Tissue-Tek OCT Compound (Sakura Finetek, Torrance, CA). Tissue blocks were cut into 8 μm-sections, fixed in acetone and stained with antibodies to mP2X7 (Hano43), CD4 (RM4-5) and CD69 (H1.2F3). The images were obtained with a Leica SP5 II confocal system.
Quantitative real-time PCR and microarray data analyses
Total RNA was extracted with TRIzol (Invitrogen, Grand Island, NY), and cDNA synthesis was performed with the High-Capacity cDNA Reverse Transcription Kit (Invitrogen). Quantitative real-time PCR was performed with Maxima® SYBR Green/ROX qPCR Master Mix (Thermo Scientific, Grand Island, NY) using the primers described in Supplementary Table 1. β-actin expression was also measured for data normalization. Microarray data (GSE20500 and GSE15907) were described previously.43, 44 All plots were made with the multiplot module of GenePattern.
Statistics
Statistical significance of differences between indicated groups was obtained by Student’s t-test and two-way analysis of variance (ANOVA). P values <0.05 were considered significant. Error bars in all figures indicate SEM.
Supplementary Material
Acknowledgments
We thank JH Park (Purdue University) for his helpful input. This study was supported, in part, by grants from National Multiple Sclerosis Society and NIH (R01AI074745, R01DK076616, 1S10RR02829, R01AI080769, and R01AI121302) to CK.
Footnotes
Conflict of interest: None
Disclosure: All authors declare no conflict of interest.
Author contribution: SH performed experiments, analyzed data, and prepared most of the figures with experimental contributions from LF and MK. CK conceived the project and obtained funding; analyzed data and drafted the manuscript with SH.
References
- 1.Yang Y, Torchinsky MB, Gobert M, Xiong H, Xu M, Linehan JL, et al. Focused specificity of intestinal TH17 cells towards commensal bacterial antigens. Nature. 2014;510(7503):152–156. doi: 10.1038/nature13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marrack P, Scott-Browne J, MacLeod MK. Terminating the immune response. Immunological reviews. 2010;236:5–10. doi: 10.1111/j.1600-065X.2010.00928.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKinstry KK, Strutt TM, Swain SL. Regulation of CD4+ T-cell contraction during pathogen challenge. Immunological reviews. 2010;236:110–124. doi: 10.1111/j.1600-065X.2010.00921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heiss K, Janner N, Mahnss B, Schumacher V, Koch-Nolte F, Haag F, et al. High sensitivity of intestinal CD8+ T cells to nucleotides indicates P2X7 as a regulator for intestinal T cell responses. Journal of immunology. 2008;181(6):3861–3869. doi: 10.4049/jimmunol.181.6.3861. [DOI] [PubMed] [Google Scholar]
- 5.Proietti M, Cornacchione V, Rezzonico Jost T, Romagnani A, Faliti CE, Perruzza L, et al. ATP-gated ionotropic P2X7 receptor controls follicular T helper cell numbers in Peyer’s patches to promote host-microbiota mutualism. Immunity. 2014;41(5):789–801. doi: 10.1016/j.immuni.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 6.Rissiek B, Haag F, Boyer O, Koch-Nolte F, Adriouch S. ADP-ribosylation of P2X7: a matter of life and death for regulatory T cells and natural killer T cells. Current topics in microbiology and immunology. 2015;384:107–126. doi: 10.1007/82_2014_420. [DOI] [PubMed] [Google Scholar]
- 7.Hildeman DA, Mitchell T, Teague TK, Henson P, Day BJ, Kappler J, et al. Reactive oxygen species regulate activation-induced T cell apoptosis. Immunity. 1999;10(6):735–744. doi: 10.1016/s1074-7613(00)80072-2. [DOI] [PubMed] [Google Scholar]
- 8.Brenner D, Krammer PH, Arnold R. Concepts of activated T cell death. Critical reviews in oncology/hematology. 2008;66(1):52–64. doi: 10.1016/j.critrevonc.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Sharma V, Delgado M, Ganea D. Granzyme B, a new player in activation-induced cell death, is down-regulated by vasoactive intestinal peptide in Th2 but not Th1 effectors. Journal of immunology. 2006;176(1):97–110. doi: 10.4049/jimmunol.176.1.97. [DOI] [PubMed] [Google Scholar]
- 10.Strasser A, Jost PJ, Nagata S. The many roles of FAS receptor signaling in the immune system. Immunity. 2009;30(2):180–192. doi: 10.1016/j.immuni.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khakh BS, North RA. P2X receptors as cell-surface ATP sensors in health and disease. Nature. 2006;442(7102):527–532. doi: 10.1038/nature04886. [DOI] [PubMed] [Google Scholar]
- 12.Adriouch S, Bannas P, Schwarz N, Fliegert R, Guse AH, Seman M, et al. ADP-ribosylation at R125 gates the P2X7 ion channel by presenting a covalent ligand to its nucleotide binding site. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2008;22(3):861–869. doi: 10.1096/fj.07-9294com. [DOI] [PubMed] [Google Scholar]
- 13.Trabanelli S, Ocadlikova D, Gulinelli S, Curti A, Salvestrini V, Vieira RP, et al. Extracellular ATP exerts opposite effects on activated and regulatory CD4+ T cells via purinergic P2 receptor activation. Journal of immunology. 2012;189(3):1303–1310. doi: 10.4049/jimmunol.1103800. [DOI] [PubMed] [Google Scholar]
- 14.Seman M, Adriouch S, Scheuplein F, Krebs C, Freese D, Glowacki G, et al. NAD-induced T cell death: ADP-ribosylation of cell surface proteins by ART2 activates the cytolytic P2X7 purinoceptor. Immunity. 2003;19(4):571–582. doi: 10.1016/s1074-7613(03)00266-8. [DOI] [PubMed] [Google Scholar]
- 15.Rissiek B, Haag F, Boyer O, Koch-Nolte F, Adriouch S. P2X7 on Mouse T Cells: One Channel, Many Functions. Frontiers in immunology. 2015;6:204. doi: 10.3389/fimmu.2015.00204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dubyak GR. P2X7 receptor regulation of non-classical secretion from immune effector cells. Cellular microbiology. 2012;14(11):1697–1706. doi: 10.1111/cmi.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Di Virgilio F, Ferrari D, Falzoni S, Chiozzi P, Munerati M, Steinberg TH, et al. P2 purinoceptors in the immune system. Ciba Foundation symposium. 1996;198:290–302. doi: 10.1002/9780470514900.ch17. discussion 302–295. [DOI] [PubMed] [Google Scholar]
- 18.Piccini A, Carta S, Tassi S, Lasiglie D, Fossati G, Rubartelli A. ATP is released by monocytes stimulated with pathogen-sensing receptor ligands and induces IL-1beta and IL-18 secretion in an autocrine way. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(23):8067–8072. doi: 10.1073/pnas.0709684105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franceschini A, Capece M, Chiozzi P, Falzoni S, Sanz JM, Sarti AC, et al. The P2X7 receptor directly interacts with the NLRP3 inflammasome scaffold protein. FASEB journal : official publication of the Federation of American Societies for Experimental Biology. 2015;29(6):2450–2461. doi: 10.1096/fj.14-268714. [DOI] [PubMed] [Google Scholar]
- 20.Kurashima Y, Amiya T, Nochi T, Fujisawa K, Haraguchi T, Iba H, et al. Extracellular ATP mediates mast cell-dependent intestinal inflammation through P2X7 purinoceptors. Nature communications. 2012;3:1034. doi: 10.1038/ncomms2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scheuplein F, Schwarz N, Adriouch S, Krebs C, Bannas P, Rissiek B, et al. NAD+ and ATP released from injured cells induce P2X7-dependent shedding of CD62L and externalization of phosphatidylserine by murine T cells. Journal of immunology. 2009;182(5):2898–2908. doi: 10.4049/jimmunol.0801711. [DOI] [PubMed] [Google Scholar]
- 22.Aswad F, Kawamura H, Dennert G. High sensitivity of CD4+CD25+ regulatory T cells to extracellular metabolites nicotinamide adenine dinucleotide and ATP: a role for P2X7 receptors. Journal of immunology. 2005;175(5):3075–3083. doi: 10.4049/jimmunol.175.5.3075. [DOI] [PubMed] [Google Scholar]
- 23.Gu BJ, Zhang W, Worthington RA, Sluyter R, Dao-Ung P, Petrou S, et al. A Glu-496 to Ala polymorphism leads to loss of function of the human P2X7 receptor. The Journal of biological chemistry. 2001;276(14):11135–11142. doi: 10.1074/jbc.M010353200. [DOI] [PubMed] [Google Scholar]
- 24.Fernando SL, Saunders BM, Sluyter R, Skarratt KK, Goldberg H, Marks GB, et al. A polymorphism in the P2X7 gene increases susceptibility to extrapulmonary tuberculosis. American journal of respiratory and critical care medicine. 2007;175(4):360–366. doi: 10.1164/rccm.200607-970OC. [DOI] [PubMed] [Google Scholar]
- 25.Adriouch S, Hubert S, Pechberty S, Koch-Nolte F, Haag F, Seman M. NAD+ released during inflammation participates in T cell homeostasis by inducing ART2-mediated death of naive T cells in vivo. Journal of immunology. 2007;179(1):186–194. doi: 10.4049/jimmunol.179.1.186. [DOI] [PubMed] [Google Scholar]
- 26.Brown CC, Esterhazy D, Sarde A, London M, Pullabhatla V, Osma-Garcia I, et al. Retinoic acid is essential for Th1 cell lineage stability and prevents transition to a Th17 cell program. Immunity. 2015;42(3):499–511. doi: 10.1016/j.immuni.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shlyueva D, Stampfel G, Stark A. Transcriptional enhancers: from properties to genome-wide predictions. Nature reviews Genetics. 2014;15(4):272–286. doi: 10.1038/nrg3682. [DOI] [PubMed] [Google Scholar]
- 28.Adriouch S, Dox C, Welge V, Seman M, Koch-Nolte F, Haag F. Cutting edge: a natural P451L mutation in the cytoplasmic domain impairs the function of the mouse P2X7 receptor. Journal of immunology. 2002;169(8):4108–4112. doi: 10.4049/jimmunol.169.8.4108. [DOI] [PubMed] [Google Scholar]
- 29.Haag F, Freese D, Scheublein F, Ohlrogge W, Adriouch S, Seman M, et al. T cells of different developmental stages differ in sensitivity to apoptosis induced by extracellular NAD. Developmental immunology. 2002;9(4):197–202. doi: 10.1080/10446670310001593514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Iwata M. Retinoic acid production by intestinal dendritic cells and its role in T-cell trafficking. Seminars in immunology. 2009;21(1):8–13. doi: 10.1016/j.smim.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 31.Kim CH. Retinoic acid, immunity, and inflammation. Vitamins and hormones. 2011;86:83–101. doi: 10.1016/B978-0-12-386960-9.00004-6. [DOI] [PubMed] [Google Scholar]
- 32.Hall JA, Grainger JR, Spencer SP, Belkaid Y. The role of retinoic acid in tolerance and immunity. Immunity. 2011;35(1):13–22. doi: 10.1016/j.immuni.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kang SG, Lim HW, Andrisani OM, Broxmeyer HE, Kim CH. Vitamin A metabolites induce gut-homing FoxP3+ regulatory T cells. Journal of immunology. 2007;179(6):3724–3733. doi: 10.4049/jimmunol.179.6.3724. [DOI] [PubMed] [Google Scholar]
- 34.Mucida D, Park Y, Kim G, Turovskaya O, Scott I, Kronenberg M, et al. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science. 2007;317(5835):256–260. doi: 10.1126/science.1145697. [DOI] [PubMed] [Google Scholar]
- 35.Iwata M, Hirakiyama A, Eshima Y, Kagechika H, Kato C, Song SY. Retinoic acid imprints gut-homing specificity on T cells. Immunity. 2004;21(4):527–538. doi: 10.1016/j.immuni.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 36.Hall JA, Cannons JL, Grainger JR, Dos Santos LM, Hand TW, Naik S, et al. Essential role for retinoic acid in the promotion of CD4(+) T cell effector responses via retinoic acid receptor alpha. Immunity. 2011;34(3):435–447. doi: 10.1016/j.immuni.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang C, Kang SG, HogenEsch H, Love PE, Kim CH. Retinoic acid determines the precise tissue tropism of inflammatory Th17 cells in the intestine. Journal of immunology. 2010;184(10):5519–5526. doi: 10.4049/jimmunol.0903942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Atarashi K, Nishimura J, Shima T, Umesaki Y, Yamamoto M, Onoue M, et al. ATP drives lamina propria T(H)17 cell differentiation. Nature. 2008;455(7214):808–812. doi: 10.1038/nature07240. [DOI] [PubMed] [Google Scholar]
- 39.Puhar A, Tronchere H, Payrastre B, Nhieu GT, Sansonetti PJ. A Shigella effector dampens inflammation by regulating epithelial release of danger signal ATP through production of the lipid mediator PtdIns5P. Immunity. 2013;39(6):1121–1131. doi: 10.1016/j.immuni.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 40.Miller CM, Zakrzewski AM, Robinson DP, Fuller SJ, Walker RA, Ikin RJ, et al. Lack of a Functioning P2X7 Receptor Leads to Increased Susceptibility to Toxoplasmic Ileitis. PloS one. 2015;10(6):e0129048. doi: 10.1371/journal.pone.0129048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen L, Brosnan CF. Exacerbation of experimental autoimmune encephalomyelitis in P2X7R−/− mice: evidence for loss of apoptotic activity in lymphocytes. Journal of immunology. 2006;176(5):3115–3126. doi: 10.4049/jimmunol.176.5.3115. [DOI] [PubMed] [Google Scholar]
- 42.Cortes-Garcia JD, Lopez-Lopez C, Cortez-Espinosa N, Garcia-Hernandez MH, Guzman-Flores JM, Layseca-Espinosa E, et al. Evaluation of the expression and function of the P2X7 receptor and ART1 in human regulatory T-cell subsets. Immunobiology. 2016;221(1):84–93. doi: 10.1016/j.imbio.2015.07.018. [DOI] [PubMed] [Google Scholar]
- 43.Heng TS, Painter MW Immunological Genome Project C. The Immunological Genome Project: networks of gene expression in immune cells. Nature immunology. 2008;9(10):1091–1094. doi: 10.1038/ni1008-1091. [DOI] [PubMed] [Google Scholar]
- 44.Kang SG, Park J, Cho JY, Ulrich B, Kim CH. Complementary roles of retinoic acid and TGF-beta1 in coordinated expression of mucosal integrins by T cells. Mucosal immunology. 2011;4(1):66–82. doi: 10.1038/mi.2010.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.