Abstract
Influenza virus causes a respiratory disease in human that can progress to lung injury with fatal outcome. The interleukin (IL)-36 cytokines are newly described IL-1 family cytokines that promote inflammatory responses via binding to the IL-36 receptor (IL-36R). The mechanism of expression and the role of IL-36 cytokines is poorly understood. Here, we investigated the role of IL-36 cytokines in modulating the innate inflammatory response during influenza virus-induced pneumonia in mice. The intranasal administration of influenza virus upregulated IL-36α mRNA and protein production in the lungs. In vitro, influenza virus-mediated IL-36α but not IL-36γ is induced and secreted from alveolar epithelial cells (AECs) through both a caspase-1 and caspase-3/7 dependent pathway. IL-36α was detected in microparticles shed from AECs and promoted the production of pro-inflammatory cytokines and chemokines in respiratory cells. IL-36R deficient mice were protected from influenza virus-induced lung injury and mortality. Decreased mortality was associated with significantly reduced early accumulation of neutrophils and monocytes/macrophages, activation of lymphocytes, production of pro-inflammatory cytokines and chemokines and permeability of the alveolar-epithelial barrier in despite impaired viral clearance. Taken together, these data indicate that IL-36 ligands exacerbate lung injury during influenza virus infection.
Keywords: Influenza virus, IL-36 receptor ligands, IL-36 receptor, Microparticles, Lung injury
Introduction
Influenza virus induced pneumonia and resultant acute respiratory distress syndrome (ARDS) are associated with high mortality in critical care patients.1 High viral load, excessive pro-inflammatory cytokines and chemokine expression and robust inflammatory cells influx into the lungs are associated with disease severity in influenza virus infection.2,3, 4 Imbalance between viral pathogenicity and host immune response is believed to contribute to influenza virus-induced respiratory failure.
Interleukin (IL)-36 cytokines, including three agonist proteins IL-36α, IL-36β, and IL-36γ, along with the antagonist protein IL-36Ra, are novel members of IL-1 family of cytokines. IL-36 agonists bind the same receptor complex, consisting of the IL-36 receptor (IL-36R) and IL-1receptor accessory protein (IL-1RAcP), a protein which is shared with the IL-1 receptor and the IL-33 receptor. Binding to this complex stimulates inflammatory signals through nuclear factor-κB and mitogen-activated protein kinase.5 The IL-36 agonists similarly induce pro-inflammatory cytokines and chemokines and contribute to neutrophils accumulation, dendritic cell activation and polarization of T helper 1 and IL-17 producing T cells.5, 6, 7 IL-36 cytokines are expressed by keratinocytes and other epithelial cells, as well as macrophages and monocytes. Conversely, IL-36R is widely expressed throughout the body.5 It was well characterized that IL-36 cytokines are involved in the pathogenesis of human psoriasis8, 9 and animal models of skin inflammation.10, 11 However, little is known about the role of IL-36 cytokines in the lung. Transcript products of IL-36γ have been shown to be upregulated in bronchial epithelial cells by stimulation of pro-inflammatory cytokines, bacteria, and viral associated molecular patterns.12,13 Intratracheal administration of IL-36α or IL-36γ in mice induce a rapid influx of neutrophils into the lungs and the expression of pro-inflammatory cytokines and chemokines.14, 15 These previous findings suggest that IL-36 cytokines may play an important role in host defense against respiratory pathogens and contribute to leukocyte recruitment during infection. To date, no studies have investigated IL-36 cytokines in the host defense against influenza virus or as mediators of virus-induced lung injury.
Secretion mechanism of IL-36 cytokines from stimulated cells is not well understood. IL-36 cytokines, like other IL-1 family cytokines, lack a signal peptide and do not utilize a classical endoplasmic reticulum-to-Golgi secretion pathway, requiring alternative mechanisms for their release. Extracellular adenosine triphosphate (ATP) has been shown to be necessary for the secretion of intracellularly produced IL-36 cytokines. 8, 16, 17 Stimulation of P2×7 receptor by extracellular ATP induced NOD-like receptor family, pyrin containing 3 (NLRP3) inflammasome activation and caspase-1-dependent processing and release of IL-1β and IL-18.18 Moreover, P2×7 signaling induces the release of extracellular microvesicles or microparticles (MPs), and secreted IL-1β and IL-18 is packaged within MPs.19, 20 MPs are membrane-bound vesicles ranging in size from 0.1–1 micron released by a variety of cells. MPs contain proteins, bioactive lipids, nucleic acid and organelles and are recognized to be a biomarker and effector of cell-to-cell signaling in inflammatory diseases.21 We have recently shown that IL-36γ protein shed from macrophages stimulated with bacteria and ATP was detected within MPs. 22 However, the role and secretion mechanism of IL-36 cytokines in the pathogenesis of lung inflammation is unknown.
In the current study, we hypothesized that IL-36 cytokines and their receptor, IL-36R, can contribute to the pathogenesis of influenza virus-induced lung injury. Influenza virus infection in mice resulted in the selective upregulation of IL-36α, but not IL-36β and γ, in the lungs. IL-36α was secreted by alveolar epithelial cells (AECs) in MPs, exosomes (EXs), and directly into the extracellular milieu in response to influenza virus, and AEC-derived MPs directly stimulate cytokine and chemokine production in pulmonary macrophages (PMs) in-vitro in an IL-36R dependent fashion. As compared to WT controls, IL-36R−/− mice display decreased early accumulation and activation of inflammatory cells, production of pro-inflammatory cytokines and chemokines, and reduced alveolar-epithelial barrier leak, which is associated with reduced mortality in response to influenza virus challenge. Taken together, these data demonstrate for the first time an important role of IL-36R ligands in the pathogenesis of influenza virus-induced lung injury.
Results
IL-36α is selectively induced in the lungs during influenza virus infection
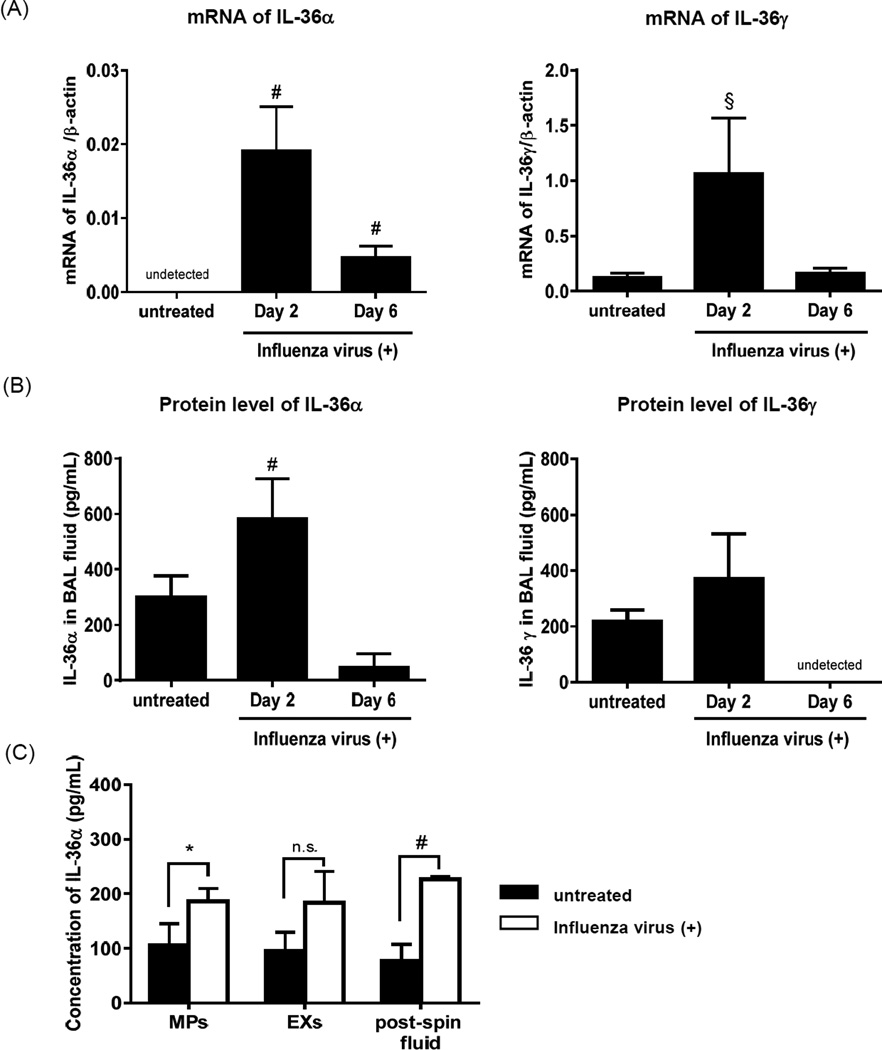
We first examined the transcript products of IL-36 cytokines in the lungs of wild-type (WT) C57B/6 mice infected with influenza virus (Influenza A/Puerto Rico/8/34 virus). Both IL-36α and IL-36γ mRNA levels were significantly elevated in lung at day 2 after influenza administration, and this increase in IL-36α mRNA, but not IL-36γ mRNA, persisted through day 6 (Fig 1A). Conversely, IL-36β mRNA was not detected in influenza virus infected lungs (data not shown). The protein levels of IL-36α in bronchoalveolar lavage fluid (BALF), but not IL-36γ, were significantly higher at day 2 compared with untreated mice (Fig 1B).
FIGURE 1. Expression of IL-36 cytokines in lung of WT mice infected with influenza virus.
(A) Transcript products of IL-36α (left panel) and IL-36γ (right panel) in the lungs of untreated, day 2 and day 6 after influenza virus infection. mRNA was analyzed by real-time PCR. (B) Protein expression of IL-36α (left panel) and IL-36γ (right panel) in BAL was quantified by ELISA. (C) MPs and EXs in BAL fluid were isolated by three step centrifugation. Production of IL-36α in MPs, EXs and post-spin fluid in which MPs and EXs fractions were removed were measured by ELISA. Data are shown as means ± SD of 5 mice/group. *p<0.05, # p <0.01, § p <0.001, significant compared with untreated mice or as indicated.
We have recently shown that IL-36γ protein released from primary PMs stimulated with Streptococcus pneumoniae was primarily packaged within MPs and exosomes (EXs). We therefore examined whether IL-36α in BAL fluid post influenza virus challenge was present in MPs and EXs. To assess this, BAL was performed at day 3 after flu administration, then MPs and/or EXs in BAL fluid were isolated by three step centrifugation.22 IL-36α was detected by ELISA within the MPs, EXs, and post-spin fluid fraction, and was significantly higher in the MP and post-spin fractions in influenza virus infected mice as compared with untreated mice (Fig 1C)
IL-36α is released from influenza virus stimulated AECs through caspase-1 and caspase-3/7 dependent pathways
Respiratory epithelial cells and macrophages are important innate immune cells during influenza virus infection. To determine the primary cellular source of IL-36α during influenza, primary AECs and PMs isolated from WT mice were incubated with various doses of influenza virus. LPS stimulation was used as a control immune activator. Treatment with LPS induced IL-36α mRNA in both AECs and PMs. Though the expression level of IL-36α mRNA was significantly elevated in influenza virus-treated AECs in a dose dependent manner, IL-36α mRNA was not induced in PMs by influenza virus (Fig 2A). Heat killed (fusion inhibiting) influenza virus failed to induce IL-36α mRNA in AECs (data not shown). Incubation with ultraviolet (UV)-inactivated influenza virus (replication inhibiting) induced IL-36α mRNA in AECs, its level was significantly lower as compared to live virus (Supplemental figure 1A).
FIGURE 2. Mechanisms of IL-36α protein synthesis and secretion from AEC in response to influenza virus, TLR-3, and TLR-7 agonists.
(A) Primary AECs (right panel) and PMs (left panel) isolated from WT mice were treated with LPS (1mg/ml) or different dose of influenza virus (MOI 10–0.1). After 24 h incubation, expression of IL-36α mRNA was analyzed by real-time PCR. (B, C) AECs were treated with poly (I:C) (25µg/ml), R843 (25µg/ml), both poly (I:C) (25µg/ml)and R843 (25µg/ml), influenza virus (MOI 10) or LPS (1µg/ml). (B) After 24 h incubation, expression of IL-36α mRNA was analyzed by real-time PCR.
(C) The protein levels of IL-36α in CM were measured by ELISA. (E, F) AECs were pretreated with Caspase-1 (20µM) or Caspase-3/7 (100 µM) inhibitor 1h before influenza virus stimulation. After 24 h incubation, IL-36α mRNA (E) and protein production in CM (F) was analyzed. Data (means ± SD) are representative of two independent experiments. *p<0.05, # p<0.01, §p<0.001, ¶ p <0.0001, n.s. not significant, compared with medium only or as indicated.
Two distinct toll-like receptors (TLRs)-3 and TLR-7 recognize the double stranded and single stranded viral RNA of influenza virus, respectively, within endosomes and play key roles in the innate immune responses against virus. 23 To examine whether these pathogen recognition receptors contribute to induction and secretion of IL-36α, we first compared mRNA expression of IL-36α in AECs treated with the TLR-3 agonist poly (I:C); the TLR-7 agonist R843; the combination of poly (I:C) plus R843; influenza virus; or LPS. Unlike a previous study,17 treatment with poly (I:C) alone did not induce IL-36α mRNA. Conversely, treatment with R843 alone enhanced expression of IL-36α mRNA, and its level tended to be enhanced by co-stimulation with poly (I:C) treatment (Fig 2B). To evaluate secretion of IL-36α protein, IL-36α was measured in culture medium (CM) by ELISA. The production of IL-36α was significantly elevated in AECs treated with live influenza virus or with the combination of poly (I:C) plus R843, but not poly (I:C) or R843 alone (Fig 2C). These data suggest that both TLR-3 and TLR-7 signaling were required for secretion of IL-36α by AECs. Moreover, we did not observe secretion of IL-36α by AECs incubated with UV-inactivated influenza virus (Supplemental figure 1B). These data indicate that viral replication is required for maximal induction and secretion of IL-36α from virus-infected AECs.
We next investigated the influence of influenza-induced caspase-1 and caspase-3/7 activation on induction and secretion of IL-36α. Influenza virus has previously been shown to induce the expression of IL-1 like family members such as IL-1β and IL-18 in respiratory cells by a caspase-1 dependent manner.18 Moreover, the secretion of IL-36 cytokines from stimulated cells has been shown to require extracellular ATP treatment (which activates caspase-1) 8, 16, 17 or caspase-3/7 activity. 17 We confirmed that live influenza virus activated caspase-1 and caspase-3/7 in AECs (Supplement figure 2C, 2D). While treatment with caspase-3/7 inhibitor did not alter IL-36α mRNA levels (Fig 2D), the secretion of IL-36α in CM was significantly reduced by caspase-3/7 inhibitor (Fig 2E). Alternatively, caspase-1 inhibition suppressed both mRNA and extracellular protein expression of IL-36α (Fig 2D, 2E). These data indicated that live influenza virus induced caspase-1 activation contributed to induction of IL-36α, whereas caspase-3/7 was required for the secretion of IL-36α from AECs. Interestingly, we did not observe apoptosis of AECs at the 24 h post infection (as determined by Annexin V+ staining), a time point in which IL-36α was detected in conditioned media (data not shown), suggesting that caspase-1 and caspase-3/7 activity, but not cell death, is required for the induction and secretion of IL-36α in influenza virus-infected AECs.
Influenza virus induced IL-36α from AECs is contained within MPs
As shown previously, a percentage of IL-36α in BAL was secreted within MPs during influenza virus infection (Fig 1C), and the secretion of IL-36α from AECs was dependent upon influenza virus-induced activation of caspase-3/7 (Fig 2, 2E). We next examined whether IL-36α secreted from influenza virus-treated AECs was packaged within extracellular vesicles. AECs were treated with or without influenza virus for 48h, then MPs and EXs isolated from CM by three step centrifugation. Although there was no difference of number of MPs released by influenza virus-treated AECs as compared to vehicle-treated cells, the size of MPs shed from influenza virus-treated AECs were larger than that from untreated AECs (Fig 3A). On the other hand, no difference was observed in the number and size of EXs between the two groups. As shown Fig 3B, the quantity of IL-36α protein contained within influenza virus-induced MPs was > 2 fold higher than that of MPs recovered from uninfected cells, whereas no difference in IL-36α levels was observed in EXs and post spin fluid (Fig 3C). To address the size difference in MPs shed from influenza virus infected cells as compared to untreated control, we examined whether or not influenza virus was contained within MPs. MPs were isolated from CM with or without influenza virus treated AECs by ultracentrifugation and then washed twice to remove virus binding to the surface of MPs. Immunoblotting showed the presence of both IL-36α and influenza virus M2 protein within MPs from influenza-infected AECs (Fig. 3D), and virus contained with these MPs could be grown in MDCK cells (Fig. 3E).
FIGURE 3. IL-36α released from influenza virus stimulated AECs contained within MPs.
AECs were treated with or without influenza virus for 48h incubation, and then MPs and EXs were isolated from CM by three step differential centrifugation. (A) MPs and EXs were identified as Annexin V positive cells. The size of MPs (left panel) and EXs (right panel) was assessed by flow cytometry for size relative to submicron calibration beads. (B) The protein expression of IL-36α in MPs, EXs and post-spin fluid was detected by western blotting. Arrows showed the expression of IL-36α at 18kDa (Upper panel). Lower panel showed β-actin at 42 kDa. (C) The production of IL-36α in MPs, EXs and post-spin fluid were measured by ELISA. Data are shown as means ± SD. *p<0.05, n.s. not significant as indicated. (D, E) MPs isolated from CM were washed twice to remove surface bound virus. The protein expression of IL-36α and influenza virus M2 antigen in MPs were detected by Western blotting. Arrow shows the expression of IL-36α at 18kDa (Upper panel), influenza virus M2 antigen at 15kDa (Middle panel) and β-actin at 42 kDa (Lower panel) (D). MPs were cultured with MDCK cells (E). MPs (UT): MPs from untreated AECs, MP (IV): MPs from influenza virus-treated AECs.
IL-36R−/− mice were protected from influenza virus-induced lung injury and mortality
To examine whether IL-36R–mediated signaling is involved in the host response against influenza infection, WT IL-36R−/− were inoculated intranasally with 2LD50 dose of influenza virus, survival and body weight change assessed out to 14 day. Because IL-36 cytokine have previously been shown to enhance the expression of other IL-36 family members, 11 and we observed upregulation of IL-36γ mRNA in lungs of influenza virus infected mice at day 2, we included IL-36γ−/− as an additional control group. Body weight was not significantly different among the three groups (Fig 4A). However, all of WT and IL-36γ−/− mice were dead within 11 days post infection, whereas 50% of IL-36R−/− mice survived beyond day 14 post infection (Fig 4B). We next examined viral clearance after influenza virus challenge by quantitating lung viral titers in WT and IL-36R−/− mice on day 2 and 6 after infectious challenge. There was no difference in viral titers observed between WT and IL-36R−/− mice at day 2 (Fig 4C, left panel). However, by day 6 there was a 10-fold higher viral burden in IL-36R−/− mice as compared to infected WT mice (Fig 4C, right panel).
FIGURE 4. Effect of IL-36R gene deletion on mortality, viral clearance and lung injury in influenza virus infection in-vivo.
Weight loss (A) and survival rate (B) were assessed daily following influenza virus infection. Each group consisted of 6–12 mice. (C) Virus titers was assessed on day 2 and day 6 after infection (n=8 per each group). (D) Lung histopathological analysis was performed on day 2 and day 7 after infection. H&E-stained lung tissue at magnification of X200 (upper) and X400 (lower). Arrow showed neutrophils around bronchus. (E) The lung injury scores of lung sections from infected-WT and IL-36R−/− mice at day 7 were evaluated as previously described (n=6 per each group). Lung injury scoring system parameters include the presence ofneutrophils in the alveolar space (i), neutrophils in the interstitial space (ii), hyaline membranes (iii), proteinaceous debris filling the airspaces (iv) and alveolar septal thickening (v). At least 20 random regions were scored 0–2 independently and the final lung injury score was calculated as below; score = [(20 × i) + (14 × ii) + (7 × iii) + (7 × iv) + (2 × v)] / (number of fields × 100). (F) Lung permeability was quantified by albumin concentration in BAL fluid from 2 and 6 day after infection (n=4 per each group). Data (means± SD) are representative of two independent experiment. * p <0.05, ¶ p <0.0001, n.s.:not significant, compared with infected in WT mice or as indicated.
Histological examination of lungs on day 2 post influenza virus administration revealed accumulation of neutrophils in a peribronchial distribution in WT mice, and no difference in inflammatory cells influx into alveolar space between WT and IL-36R−/− mice at that time point. At day 7 in WT mice, there was massive infiltration of neutrophils not only into the intra-alveolar septa but into the alveolus, as well as alveolar hemorrhage, alveolar septa edema and proteinaceous debris in the alveolar space. These inflammatory changes were strikingly attenuated in IL-36R−/− mice. We quantified the histological changes of tissue injury using a standardized lung injury scoring system. 24 The lung injury score was significantly lower in IL-36R−/− mice as compared to infected WT mice (Fig 4E). We next assessed the permeability of the alveolar-capillary membrane by measurement of albumin concentration in BAL fluid. At day 6, albumin levels in BAL fluid were significantly reduced in IL-36R−/− mice compared to WT mice. Reduced alveolar permeability in influenza virus infected IL-36R−/− mice was associated with a significant decrease in TUNEL positive apoptotic cells in IL-36R−/− mice compared with WT mice (Supplement figure 2A and 2B). These data suggested that IL-36R ligands contributed to pathogenesis of lung injury and mortality induced by influenza virus despite a beneficial role in viral clearance.
Reduced lung leukocyte influx and activation in IL-36R−/− mice during influenza virus infection
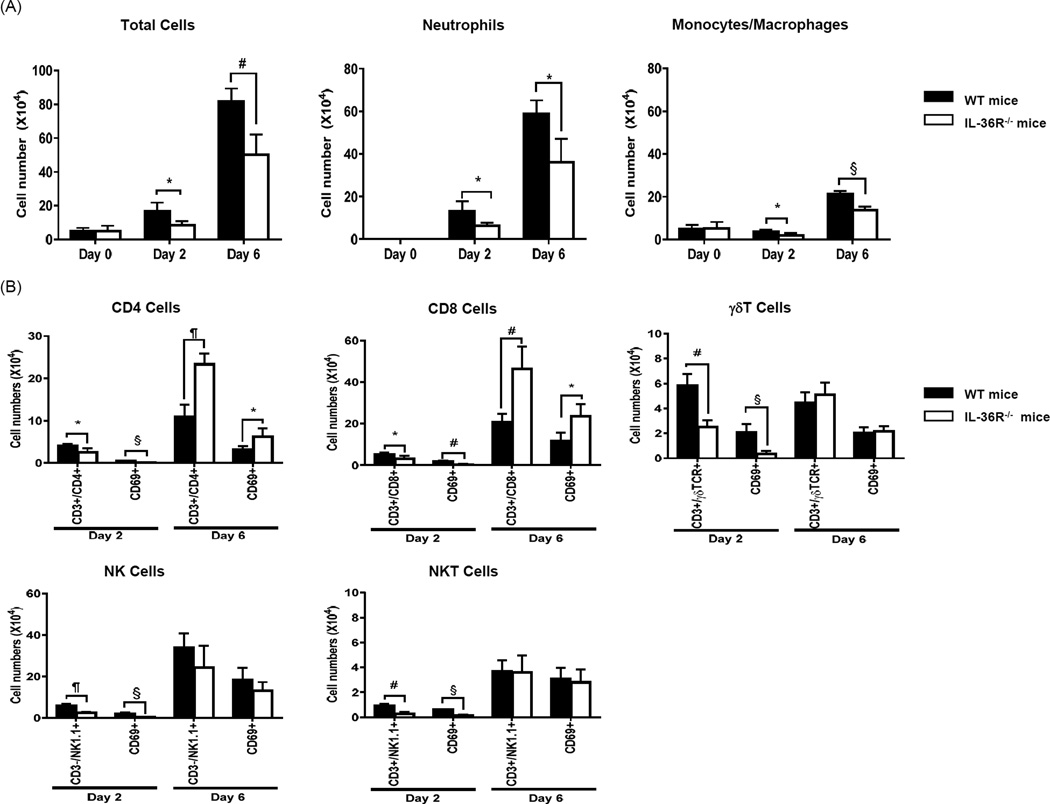
We next quantified differences in lung inflammatory cell accumulation in WT and IL-36R−/− mice during influenza virus infection. No difference in number of total BAL leukocyte and proportion of monocytes/macrophages were observed in uninfected WT and IL-36R−/− mice at baseline. After inoculation of influenza virus, total number of lung leukocytes in BAL fluid increased in a time-dependent manner (Fig 5A). At day 2 and day 6, the number of total leukocyte, neutrophils and monocytes/macrophages in BAL fluid was significantly reduced in IL-36R−/− mice as compared to their WT counterparts.
FIGURE 5. Effect of IL-36R gene deletion on lung leukocytes influx and lymphocyte activation during influenza virus infection.
(A) BAL sample were collected at day 0, day 2 and day 6 after influenza virus infection and the number of total cell, neutrophils and monocytes and macrophages were count. (B) The number of CD4+ T cells, CD8+ T cells, NK cells, NKT cells and γδ T cells and CD69 positive lymphocytes was determined by flow cytometry. Lung digests were collected at day 2 and day 6 post-infection. Each group is consisted of 4 mice. Data (means ± SD) are representative of two independent experiments. * p<0.05, # p<0.01, § p<0.001, ¶ p<0.0001 as indicated.
Lymphocytes, especially CD8 T cells, contribute to influenza virus clearance during infection. Murine lymphocytes including CD4 T cells, CD8 T cells, NK cells and γδT cells express the IL-36 receptor, and IL-36 cytokines can directly influence activation and proliferation of selected T cell populations.25 We therefore examined the accumulation and activation of specific lymphocyte populations by flow cytometry. At day 2 of influenza virus infection, the numbers of CD4+ T cells, CD8+ T cells, NK cells, NKT cells, γδ T cells were significantly reduced in infected IL-36R−/− mice than in WT animals. Moreover, decreased numbers of activated lymphocyte populations, as identified by co-expression of activation marker CD69, were observed in IL-36R deficient mice. In contrast, total numbers and numbers of activated CD4+ and CD8+ T cell were considerably greater in IL-36R−/− mice than in WT mice at day 6 (Fig 5B).
IL-36R−/− mice exhibit reduced early cytokine and chemokine production during influenza virus infection
Cytokines and chemokines contribute to control of viral replication via activation of both myeloid and parenchymal cells. However, these cytokines can also contribute to pathophysiology in patients with severe influenza virus infection.26 Therefore, we examined whether IL-36R genetic deficiency altered cytokines/chemokine production during influenza virus infection. BAL samples were collected from influenza virus infected mice at day 2 and day 6. At day 2, BAL levels of IL-6, IL-17, KC/CXCL1 and IP-10/CXCL10 were significantly lower in IL-36R−/− mice compared to infected WT mice (Fig 6). By comparison, there was no difference in BALF IFN-γ, TNF-α and CCR2/MCP-1 levels (Supplemental Figure 2A) between WT and IL-36R−/− mice during the course of infection. No difference in the levels of cytokines/chemokines was noted at day 6.
FIGURE 6. Effect of IL-36R gene deletion on the production of pro-inflammatory cytokines and chemokines during influenza virus infection.
BAL sample were collected at day 0, day 2 and day 6 after influenza challange. Levels of immunoreactive TNF-α, IL-6, IFN-γ, IL-17, KC/CXCL1 and IP-10/CXCL10 were measured by ELISA. Each group is consisted of 4 mice. Data (means ± SD) are representative of two independent experiments. * p<0.05, # p<0.01 as indicated.
IL-36α enhanced cytokine/chemokine production from AECs and PMs
To examine whether IL-36α might promote the production of cytokines and chemokines by cells present within the alveolus in either an autocrine or paracrine fashion, primary AECs and PMs were isolated from WT and IL-36R−/− mice, then treated with mrIL-36α for 24h and the production of IL-6 and KC quantitated. Cells from IL-36R−/− mice were used as a control to exclude non-specific stimulation (e.g. LPS contamination). Treatment with rIL-36α induced the production of IL-6 and CXCL1/KC from WT AECs and PMs. This effect was dependent upon IL-36R signaling, as no induction of IL-6 and KC was observed in AECs and PMs isolated from IL-36R−/− mice (Fig 7A and 7B).
FIGURE 7. IL-36α induced production of cytokine and chemokines from primary AECs and PMs.
Primary AECs and PMs isolated from WT and IL-36R−/− mice were treated with recombinant IL-36α (100 ng/mL) for 24h (A–B). The production of IL-6 and KC by AECs (A) and PMs (B) were measured by ELISA. (C) AECs isolated from WT mice were treated with or without influenza virus. After 48h incubation, MPs were isolated by ultracentrifugation method. Primary PMs isolated from WT and IL-36R−/− mice were treated with influenza virus-mediated and untreated MPs for 24h. The production of IL-6 and KC in CM was measured by ELISA. rIL-36α: recombinant IL-36α, MPs (UT): MPs from untreated AECs, MP (IV): MPs from influenza virus-treated AECs. Data (means ± SD). * p<0.05, # p<0.01, § p<0.001, ¶ p<0.0001 compared with medium or as indicated as indicated.
Finally, using an in-vitro model of cell-to cell networking, we examined whether MPs released from influenza-infected AECs might stimulate the production of IL-6 and KC by PMs in an IL-36R–dependent fashion. AECs isolated from WT mice were treated with or without influenza virus for 48h, then MPs isolated from CM by ultracentrifugation. We next incubated primary PMs isolated from WT and IL-36R−/− mice with AECs-derived MPs. Because influenza virus-mediated MPs contained live influenza virus (Fig 3D and 3E), we first examined the production of IL-6 and KC in response to influenza virus between PMs isolated from WT and IL-36R−/− mice, and no differences were observed (data not shown). The induction of IL-6 and KC from PMs was significantly greater when incubated with MPs recovered from influenza virus-treated AECs as compared to MPs isolated from uninfected AEC. Moreover, we found that the MP-stimulated production of IL-6 and KC from PMs was IL-36R dependent, as MPs failed to induce cytokine production n PMs isolated from IL-36R−/− mice (Fig 7C).
Discussion
Influenza virus -induced lung injury is characterized by the disruption of the alveolar-capillary membranes and pulmonary edema.26 Both bronchial and alveolar epithelial cells play an important role in the immune response against influenza virus. If the host immune response and virus replication is not adequately control at infectious site, excessive inflammation can lead to epithelial cell death and tissue damage. In this study, we demonstrate that IL-36R ligands released from AECs and possibly other lung cells contribute to influenza virus-induced lung injury.
Influenza virus is single-stranded (ss) RNA virus, but produces double-stranded (ds) RNA intermediates during replication. TLR-3 and TLR-7 recognized ssRNA and dsRNA, respectively, and two distinct innate immune receptor-mediated signaling pathway, TLR-3-TRIF and TLR-7-MyD88, induced production of type-1 interferon or pro-inflammatory cytokines.27 We have previously demonstrated that the induction of IL-36γ in PMs by LPS and whole bacteria was MyD88 dependent.22 Our results indicate that TLR-4 and TLR-7, but not TLR-3, mediated the upregulation IL-36α mRNA in AECs (Fig 2B), and suggest that MyD88-, rather than TRIF signaling is required for induction of IL-36α message in AECs. It is known that secretion of IL-1β and IL-18 from influenza virus infected cells is depend on intracellular caspase-1 activity via NLRP-3 inflammasome components.27 We observed that treatment with a caspase-1 inhibitor suppressed IL-36α mRNA expression in response to influenza virus (Fig 2D), suggesting that induction of IL-36α mRNA in influenza virus infected AECs is regulated by caspase-1 activity. Previous studies have demonstrated that caspase-3/7 activation induced by either ATP8, 16 or TLR-317 signal was required for secretion of IL-36 cytokines. Our results are consistent with previous studies demonstrating the requirement for viral replication indicating a contribution of both TLR-7 and TLR-3 signal for maximal secretion of IL-36α.
MPs have been detected in patients with sepsis and ARDS. These structures are released from both apoptotic and activated cells in response to various stimuli such as LPS, cytokines and cellular stress. During sepsis, MPs have been associated with endothelial injury and vascular tone thorough pro-inflammatory pathways, pro-coagulation activity and both oxidative and nitrogen stress. 21 However, little is known regarding the role of pathogen-mediated MPs in infectious disease. We found that influenza virus-induced IL-36α was contained within MPs shed from AECs (Fig 3B and 3C), as well as MPs in BALF during influenza virus infection in-vivo (Fig 1C). Furthermore, IL-36α packaged within MPs enhanced the production of IL-6 and KC by PMs raising the possibility of autocrine and paracrine networking between cells within the alveolar space (Fig 7C). In addition, we found that live influenza virus was packaged within virus-induced MPs (Fig 3C and 3D). Thus, MPs containing both IL-36α and influenza virus together have the potential of amplifying inflammatory responses in the lungs, which in the setting of influenza infection results in adverse consequences.
We found that lung injury was mitigated in IL-36R−/− mice, as indicated by less albumin concentration (Fig 4F), histological lung injury score (Fig 4D and 4E) and lung epithelial cell apoptosis (Supplemental figure 2A and 2B). Reduction in lung injury in in IL-36R−/− mice was associated with significantly decreased early accumulation and activation of inflammatory cells, including monocytes, neutrophils, NK, and lymphocyte populations. Previous studies demonstrated that CCR2 positive exudative monocytes influx into alveolar space and contributed to lung epithelial cell damage through TRAIL mediated apoptosis after influenza virus infection.28, 29 However, we found no differences in the CCR2-ligand MCP-1 production or in the expression level of TRAIL mRNA in the lungs between influenza virus infected lungs of WT and IL-36R−/− mice (Supplemental figure 3A and 3B). Macrophages and monocytes express IL-36 receptor, and changes in macrophage activational state may be IL-36-dependent. However, there was no difference in NO activity, which is an activate marker of macrophages/monocytes, between two groups (Supplemental data 3C). These data suggest that the mechanism of reduced injury/apoptosis of lung epithelial cells in influenza virus infected IL-36R−/− mice is not due to differences in TRAIL mediated apoptosis.
A reduction in neutrophil influx was noted in the lungs of IL-36R deficient mice during influenza infection (Fig 5A). Exuberant recruitment and activation of neutrophils is considered to play a key role in progression of ALI/ARDS in several disease conditions. 30 In influenza infection, neutrophils have been shown to promote epithelial-endothelial barrier damage by the production of neutrophils extracellular traps 31, reactive oxygen species 32 and myeloperoxidase 33. In flu-induced ARDS patients, IL-17, CXCL8/ IL-8 and CXCL10/IP-10 have been shown to be elevated in serum and BALF and levels correlated with disease severity. 3, 34 IL-17 and CXC chemokines are known to be key mediators of neutrophil migration. In addition, neutrophils express CXCR3, and IP-10/CXCL10 can stimulate the respiratory burst in neutrophils.35 IL-17 is known to be responsible for upregulation of CXCR2 ligands such as KC 36 as well as the CXCR3 ligand IP-10.37 In murine influenza infection, both IL-17 receptor and IL-17A deficient mice showed increased survival rate and decreased lung injury, which occurred in association with reduced neutrophil accumulation. 38, 39 In addition, mice treated with IP-10 antibody and IP-10 KO mice attenuated the mortality of influenza virus induced lung injury.35, 40 We found that the early production of IL-17, KC and IP-10 at day 2 was significantly lower in IL-36R−/− mice as compared to influenza-infected WT mice. In influenza virus infection, the cellular source of IL-17 in the lungs is believed to be γδT cells.38, 41 These cells also express the IL-36 receptor, and stimulation with IL-36 cytokine directly promotes IFN-γ production.25 Importantly, we found that the absolute number of γδ T cells and CD69+ γδ T cells in the lungs are much lower in IL-36R−/− compared with WT at Day 2 post infection, which may account for attenuated production of IL-17 in IL-36R−/− mice after influenza virus infection. We also observed that IL-36α directly induces KC production from AECs and PMs (Fig 7A and 7B). Since murine neutrophils do not express the IL-36 receptor,42 IL-36R ligands are unlikely to directly mediate neutrophil accumulation and activation.
Of interest, we observed impaired viral clearance in IL-36R−/− mice. Our results are in line with the findings of others showing that influenza virus induced mortality does not necessarily correlate with lung viral clearance. 43,44, 45 A fine balance exists between optimal immune clearance of virus and immune-mediated lung tissue damage. PMN and exudate macrophages contribute to viral clearance, and reductions in these cell populations in IL-36R−/− mice may account for both attenuated lung injury responses and reduced viral clearance. A previous in vitro study demonstrated that IL-36γ directly promotes naïve CD8+ T cells proliferation and differentiation to effector CD8+ T cells, 25 thus IL-36 receptor ligands may be considered to contribute to virus clearance due to lymphocytes accumulation and antigen-specific activation at the infectious site. It is tempting to postulate that viral clearance was delayed in IL-36R−/− mice due to early reduction in the number of activated CD4+ and CD8+ T lymphocytes, cells known to contribute to viral clearance. On the other hand, at day 6 after infection, the number of total and CD69+ CD4+ and CD8+ T cells was much greater in IL-36R−/− mice. This paradoxical increase in CD4 and CD8 accumulation in IL-36R deficient mice at later time points remains unexplained. One possibility is that higher viral titers as a consequence of reduced early inflammatory cell accumulation (PMN, mononuclear cells) may drive lymphocyte accumulation/activation at later time points, which occurs in an IL-36 independent fashion. Finally, we observed reductions in number and activation of γδ T cells and more modest reductions in NK and NKT cells at early time points in IL-36R deficient mice, although the contribution of these cell populations to viral clearance and influenza-induced lung injury is less well defined. Regardless, our findings indicate that although IL-36 agonists promote antiviral clearance responses in the lung, they also promote deleterious lung injury culminating in death.
This study has some limitations. Most notably, we did not precisely identify the IL-36 receptor ligand responsible for the effects observed in our model. Because influenza infection did not stimulate IL-36γ secretion by virus infected AECs and PMs, and mortality in IL-36γ KO mice did not differ from WT mice during influenza virus infection, we speculate that IL-36α rather than IL-36γ plays a central role in influenza virus-induced lung injury. Unfortunately, the polyclonal IL-36α Ab generated for antigen detection was non-neutralizing and no IL-36α KO mice is yet available. In addition, there is some uncertainly as to cellular sources of IL-36α other than AECs in our model. A recent study demonstrated that neutrophils expressed IL-36 cytokines in a murine autoimmune encephalitis model.42
In conclusion, our findings indicate that IL-36 agonists released from AECs and almost certainly other lung cells play a pivotal role in influenza virus-induced lung injury. Further studies will focus on identifying IL-36R ligands in humans with influenza virus-induced lung injury and correlation with relevant clinical outcomes.
Materials and methods
Mice
Specific pathogen-free age- and sex-matched C57BL/6 mice were purchased from The Jackson Laboratory (Bar Harbor, ME, USA). IL-36R−/− mice on C57BL/6 background were provided by Jennifer Towne from Amgen (Thousand Oaks, CA, USA). 10 A colony of IL-36γ−/− mice bred on a C57BL/6 background was established at the University of Michigan (Ann Arbor, MI, USA). 22 All mice were housed in specific pathogen-free conditions within the University of Michigan Animal Care Facility. Animal studies were reviewed and approved by the University Committee on Use and Care of Animals at the University of Michigan.
Virus infection in vivo
Influenza A/Puerto Rico/8/34 virus was used for all of experiments. For intranasal infection, mice were anesthetized by intraperitoneal injection of ketamine and xylazine and then infected by intranasal administration of 2×50% lethal dose (LD50: 40pfu) of virus in 30µl of saline.
Bronchoalveolar lavage and lung sampling
Mice were euthanized by CO2 inhalation. The trachea was exposed and cannulated with 22 G intravenous catheter. BAL was performed with 1.5ml PBS (three aliquot 500µl of PBS), and then pulmonary circulation was rinsed by 1ml PBS. Right lungs were harvested to determine the virus titer and stored at −80°C. Left lungs were harvested for RNA extraction, immediately snap-frozen in liquid nitrogen. After a collection of leukocytes in BAL fluids, cytospin (1000 rpm × 5 min) preparations were made from each sample and stained with modified Wright stain. Differential cell counts of neutrophils and monocytes and macrophages were obtained for at least 400 cells counts in each sample at a magnification of ×1000.
Histopathological examination
Lungs and trachea were removed from euthanized animals and inflated at 20cm H2O with 4% paraformaldehyde through trachea, and fixed for paraffin embedding. All lungs were sectioned and stained with haematoxylin and eosin (H&E). Quantitative analysis of tissue injury was measured using the lung injury scoring system as described.24 Lung injury scoring system parameters include neutrophils in the alveolar space (A), neutrophils in the interstitial space (B), hyaline membranes (C), proteinaceous debris filling the airspaces (D) and alveolar septal thickening (E). At least 20 random regions were scored 0–2 independently at a magnification of ×400 in a blinded fashion. The final lung injury score per each lungs was calculated as below; score = [(20 × A) + (14 × B) + (7 × C) + (7 × D) + (2 × E)] / (number of fields × 100).
Virus titer
Madin-Darby canine kidney (MDCK) cells were plated at 1 × 106 cells in a flat bottomed 6-well plate 24 h before infection. Supernatant from right lung homogenates serially diluted were used to infect the MDCK cells at 37°C for 1h. The cells were subsequently overlaid with DMEM mixed 0.4% agarose (Sigma-Aldrich, St. Louis, MO, USA) in the presence of 0.5µg/ml Trypsin (Sigma-Aldrich) and incubated for 96 h. The plaques were visualized by staining the cells with crystal violet.
Total lung leukocyte
Lung leukocytes were prepared as described in our previous study. 46 Briefly, lungs were homogenated in 15 ml of digestion buffer (RPMI1640 medium supplemented with 5%FCS and containing 1mg/ml collagenase [Roche Diagnostics, Mannheim, Germany] and 30µg/ml DNase I [Sigma-Aldrich]) per lung and enzymatically digested for 60 min at 37°C. Tissue fragments were removed by passing the mesh. Total lung cell pellet was re-suspended in 4ml of 40% (v/v) Percoll (Pharmacia, Uppsala, Sweden) and layered onto 4ml of 80% (v/v) Percoll. After centrifugation at 2,000rpm for 20 min at room temperature, the cells were collected.
Murine pulmonary macrophage and alveolar epithelial cell isolation and culture
Murine pulmonary macrophages (PMs) and type II alveolar epithelial cells (AECs) were isolated using the method described previously.47 Briefly, PMs were isolated from dispersed lung homogenates by adherence purification and plated at a density 5 × 105 cells/ml. For the isolation of murine AECs, the pulmonary vasculature was perfused. The lungs were filled via the trachea with 1.5 ml dispase (Worthington, Lakewood, NJ. USA), then 1.5 ml of low-melting point agarose and finally placed in ice cold PBS. The lungs were submerged in dispase for 45 min at 24°C before the lung tissue was teased from the airways and minced in DMEM with 0.01% DNase. After swirling for 15 min, followed by passage through a series of nylon filters, the cell suspension was collected by centrifugation and incubated with biotinylated Abs (anti-CD32 and anti-CD45; BD Pharmingen, San Diego, CA, USA). After incubation with streptavidin-coated magnetic particles, myeloid cells were removed using a magnetic tube separator. Mesenchymal cells were removed by overnight adherence in a Petri dish and the resulting non-adherent cells were plated on plastic dishes coated with fibronectin. Previous work has shown that the day 3 time point has >90% pure AECs.47 These cells were treated with influenza virus at a multiplicity of infection (MOI) of 10 – 0.1, LPS (1µg/ml) (Sigma-Aldrich), TLR-3 ligand: poly(I:C) (25µg/ml), TLR-7 ligand: R843 (25µg/ml) (Invivogen, San Diego, CA, USA ) and recombinant IL-36α (rIL-36α; R&D Systems Minneapolis, MN, USA) (100ng/ml). For blockade of caspase-1 and caspase-3/7, inhibitor of Caspase-1 and Caspase-3/7 (Cayman Chemical Co., Ann Arbor, MI, USA) which were soluble in DMSO (add vehicle control) added to cultures 1 h before stimulation with medium and influenza virus. Final concentrations were 20 µM (caspase-1 inhibitor) and 100 µM (caspase-3/7 inhibitor).
Isolation of microparticles and exosomes in vivo and in vitro
We used a standard three step differential centrifugation method to isolate MPs and EXs in vivo and in vitro samples, as previously described.22 BAL fluid and CM was centrifuged to remove cells and large debris at 3,000rpm for 10min and stored these samples at −80°C overnight. Each sample supernatant was centrifuged at 17,000rpm for 45min to obtain the MPs. After collecting the supernatant, the pellet containing the MPs fraction was suspended in 100µl of lysis buffer or PBS. For the final step, each supernatant was centrifuged at 28,000rpm for 90 min to isolate EXs. The pellet was suspended in 100µl of lysis buffer or PBS. In some experiments, MPs were washed twice by DMEM and suspended 100µl of DMEM and cultured with MDCK cells. MPs, EXs and the post-spin fluid in which MPs and EXs were removed by ultracentrifugation were stored in −80°C.
Flow cytometry analysis
Cells, isolated from whole lung or MPs and EXs as described above, were stained with the following FITC- or PE- or PerCP-Cy5.5 labeling antibodies to CD3, CD4, CD8, NK1.1, γδTCR, CD69 and Annexin V (BD Pharmigen) and analyzed by Attune® Acoustic Focusing Cytometer (Thermo Scientific-Applied Biosystems, Foster City, CA, USA). Isotype control was used for all the samples. MPs and EXs were defined as Annexin V positive cells. To measure the size of MPs and EXs, we used calibration beads from 0.1 to 3 µm in diameter, as previously described. 48, 49
Determination of cytokine production by ELISA
IL-36α, secreted in fluid or contained in MPs and EXs, was measured by sandwich ELISA protocol. Other cytokines/chemokines (TNF-α, IL-6, IFN-γ, IL-17, KC and IP-10; R&D systems,) and albumin (Albumin Quantification Kit: Bethyl Laboratories, Montgomery, TX, USA) were quantified using a modified double-ligand method as described.
RNA isolation and real-time PCR
RNA was isolated and real time quantitative RT-PCR was performed by AB Step One plus Real-Time PCR System (Thermo Scientific-Applied Biosystems). Predesigned primer and probes of targeted molecules and β-actin as a control were purchased from Integrated DNA Technologies (Coralville, IA, USA). Quantification of β-actin and target genes in each sample set was performed by the standard curve method.
Western blotting
Cells were digested by RIPA buffer (Sigma-Aldrich) plus protease inhibitors and gels were subjected to electrophoresis as previously described.47 Membranes were incubated with primary anti-IL-36α antibody (R&D systems; diluted 1:250), anti-Influenza virus M2 antigen antibody (Santa Cruz; diluted 1: 1,000) or β-actin (Sigma-Aldrich; diluted 1:5,000), blots were incubated with a secondary antibody linked to HRP and the signals were developed with an ECL (SuperSignal West Pico Substrate, Pierce Biotechnology, and Rockford, IL, USA).
Statistical analysis
Descriptive statics, such as means and standard deviations, were collected. The difference in survival rates was evaluated by the log rank test (Mantel-Cox). Two sets of values were evaluated by the Student’s t-test, and more than three sets of value were evaluated by ANOVA, followed by the Turkey’s multiple comparison test. Data analysis was conducted using GraphPad prism 6 (GraphPad Software, La Jolla, CA, USA). A P value of <0.05 was considered satirically significance.
Supplementary Material
Acknowledgments
This work was supported by Tohoku University Leading Young Researcher Overseas Visit Program (TA), Japanese Society for the Promotion of Science Grant-in-Aid for Scientific Research 25860825 (TA) and National Institutes of Health/National Heart Lung, and Blood Institute Grants NIH/NHLBI R01 HL123515 and R01 HL097564 (TJS)
Footnotes
Conflict of interest
The authors declare no conflict of interests.
Reference
- 1.Dawood FS, et al. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. The Lancet Infectious diseases. 2012;12:687–695. doi: 10.1016/S1473-3099(12)70121-4. [DOI] [PubMed] [Google Scholar]
- 2.de Jong MD, et al. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat Med. 2006;12:1203–1207. doi: 10.1038/nm1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chi Y, et al. Cytokine and chemokine levels in patients infected with the novel avian influenza A (H7N9) virus in China. J Infect Dis. 2013;208:1962–1967. doi: 10.1093/infdis/jit440. [DOI] [PubMed] [Google Scholar]
- 4.To KK, et al. Delayed clearance of viral load and marked cytokine activation in severe cases of pandemic H1N1 2009 influenza virus infection. Clin Infect Dis. 2010;50:850–859. doi: 10.1086/650581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gabay C, Towne JE. Regulation and function of interleukin-36 cytokines in homeostasis and pathological conditions. Journal of leukocyte biology. 2015;97:645–652. doi: 10.1189/jlb.3RI1014-495R. [DOI] [PubMed] [Google Scholar]
- 6.Carrier Y, et al. Inter-regulation of Th17 cytokines and the IL-36 cytokines in vitro and in vivo: implications in psoriasis pathogenesis. The Journal of investigative dermatology. 2011;131:2428–2437. doi: 10.1038/jid.2011.234. [DOI] [PubMed] [Google Scholar]
- 7.Vigne S, et al. IL-36 signaling amplifies Th1 responses by enhancing proliferation and Th1 polarization of naive CD4+ T cells. Blood. 2012;120:3478–3487. doi: 10.1182/blood-2012-06-439026. [DOI] [PubMed] [Google Scholar]
- 8.Johnston A, et al. IL-1F5, -F6, -F8, and -F9: a novel IL-1 family signaling system that is active in psoriasis and promotes keratinocyte antimicrobial peptide expression. Journal of immunology. 2011;186:2613–2622. doi: 10.4049/jimmunol.1003162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marrakchi S, et al. Interleukin-36-receptor antagonist deficiency and generalized pustular psoriasis. The New England journal of medicine. 2011;365:620–628. doi: 10.1056/NEJMoa1013068. [DOI] [PubMed] [Google Scholar]
- 10.Blumberg H, et al. Opposing activities of two novel members of the IL-1 ligand family regulate skin inflammation. The Journal of experimental medicine. 2007;204:2603–2614. doi: 10.1084/jem.20070157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tortola L, et al. Psoriasiform dermatitis is driven by IL-36-mediated DC-keratinocyte crosstalk. The Journal of clinical investigation. 2012;122:3965–3976. doi: 10.1172/JCI63451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chustz RT, et al. Regulation and function of the IL-1 family cytokine IL-1F9 in human bronchial epithelial cells. American journal of respiratory cell and molecular biology. 2011;45:145–153. doi: 10.1165/rcmb.2010-0075OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vos JB, et al. Transcriptional response of bronchial epithelial cells to Pseudomonas aeruginosa: identification of early mediators of host defense. Physiological genomics. 2005;21:324–336. doi: 10.1152/physiolgenomics.00289.2004. [DOI] [PubMed] [Google Scholar]
- 14.Ramadas RA, Ewart SL, Iwakura Y, Medoff BD, LeVine AM. IL-36alpha exerts pro-inflammatory effects in the lungs of mice. PloS one. 2012;7:e45784. doi: 10.1371/journal.pone.0045784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramadas RA, Ewart SL, Medoff BD, LeVine AM. Interleukin-1 family member 9 stimulates chemokine production and neutrophil influx in mouse lungs. American journal of respiratory cell and molecular biology. 2011;44:134–145. doi: 10.1165/rcmb.2009-0315OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin U, et al. Externalization of the leaderless cytokine IL-1F6 occurs in response to lipopolysaccharide/ATP activation of transduced bone marrow macrophages. Journal of immunology. 2009;183:4021–4030. doi: 10.4049/jimmunol.0803301. [DOI] [PubMed] [Google Scholar]
- 17.Lian LH, Milora KA, Manupipatpong KK, Jensen LE. The double-stranded RNA analogue polyinosinic-polycytidylic acid induces keratinocyte pyroptosis and release of IL-36gamma. The Journal of investigative dermatology. 2012;132:1346–1353. doi: 10.1038/jid.2011.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gombault A, Baron L, Couillin I. ATP release and purinergic signaling in NLRP3 inflammasome activation. Frontiers in immunology. 2012;3:414. doi: 10.3389/fimmu.2012.00414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eltom S, et al. Respiratory infections cause the release of extracellular vesicles: implications in exacerbation of asthma/COPD. PloS one. 2014;9:e101087. doi: 10.1371/journal.pone.0101087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sakaki H, et al. P2×4 receptor regulates P2×7 receptor-dependent IL-1beta and IL-18 release in mouse bone marrow-derived dendritic cells. Biochemical and biophysical research communications. 2013;432:406–411. doi: 10.1016/j.bbrc.2013.01.135. [DOI] [PubMed] [Google Scholar]
- 21.Reid VL, Webster NR. Role of microparticles in sepsis. British journal of anaesthesia. 2012;109:503–513. doi: 10.1093/bja/aes321. [DOI] [PubMed] [Google Scholar]
- 22.Kovach MA, et al. IL-36gamma is secreted in microparticles and exosomes by lung macrophages in response to bacteria and bacterial components. Journal of leukocyte biology. 2016 doi: 10.1189/jlb.4A0315-087R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Takeuchi O, Akira S. Pattern recognition receptors and inflammation. Cell. 2010;140:805–820. doi: 10.1016/j.cell.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 24.Matute-Bello G, et al. An official American Thoracic Society workshop report: features and measurements of experimental acute lung injury in animals. American journal of respiratory cell and molecular biology. 2011;44:725–738. doi: 10.1165/rcmb.2009-0210ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang X, et al. IL-36gamma Transforms the Tumor Microenvironment and Promotes Type 1 Lymphocyte-Mediated Antitumor Immune Responses. Cancer cell. 2015;28:296–306. doi: 10.1016/j.ccell.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Short KR, Kroeze EJ, Fouchier RA, Kuiken T. Pathogenesis of influenza-induced acute respiratory distress syndrome. The Lancet Infectious diseases. 2014;14:57–69. doi: 10.1016/S1473-3099(13)70286-X. [DOI] [PubMed] [Google Scholar]
- 27.Iwasaki A, Pillai PS. Innate immunity to influenza virus infection. Nature reviews Immunology. 2014;14:315–328. doi: 10.1038/nri3665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Herold S, et al. Lung epithelial apoptosis in influenza virus pneumonia: the role of macrophage-expressed TNF-related apoptosis-inducing ligand. The Journal of experimental medicine. 2008;205:3065–3077. doi: 10.1084/jem.20080201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hogner K, et al. Macrophage-expressed IFN-beta contributes to apoptotic alveolar epithelial cell injury in severe influenza virus pneumonia. PLoS pathogens. 2013;9:e1003188. doi: 10.1371/journal.ppat.1003188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grommes J, Soehnlein O. Contribution of neutrophils to acute lung injury. Molecular medicine. 2011;17:293–307. doi: 10.2119/molmed.2010.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Narasaraju T, et al. Excessive neutrophils and neutrophil extracellular traps contribute to acute lung injury of influenza pneumonitis. The American journal of pathology. 2011;179:199–210. doi: 10.1016/j.ajpath.2011.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Snelgrove RJ, Edwards L, Rae AJ, Hussell T. An absence of reactive oxygen species improves the resolution of lung influenza infection. European journal of immunology. 2006;36:1364–1373. doi: 10.1002/eji.200635977. [DOI] [PubMed] [Google Scholar]
- 33.Sugamata R, et al. Contribution of neutrophil-derived myeloperoxidase in the early phase of fulminant acute respiratory distress syndrome induced by influenza virus infection. Microbiology and immunology. 2012;56:171–182. doi: 10.1111/j.1348-0421.2011.00424.x. [DOI] [PubMed] [Google Scholar]
- 34.Hagau N, et al. Clinical aspects and cytokine response in severe H1N1 influenza A virus infection. Critical care. 2010;14:R203. doi: 10.1186/cc9324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ichikawa A, et al. CXCL10-CXCR3 enhances the development of neutrophil-mediated fulminant lung injury of viral and nonviral origin. American journal of respiratory and critical care medicine. 2013;187:65–77. doi: 10.1164/rccm.201203-0508OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hartupee J, Liu C, Novotny M, Li X, Hamilton T. IL-17 enhances chemokine gene expression through mRNA stabilization. Journal of immunology. 2007;179:4135–4141. doi: 10.4049/jimmunol.179.6.4135. [DOI] [PubMed] [Google Scholar]
- 37.Khader SA, et al. IL-23 and IL-17 in the establishment of protective pulmonary CD4+ T cell responses after vaccination and during Mycobacterium tuberculosis challenge. Nature immunology. 2007;8:369–377. doi: 10.1038/ni1449. [DOI] [PubMed] [Google Scholar]
- 38.Crowe CR, et al. Critical role of IL-17RA in immunopathology of influenza infection. Journal of immunology. 2009;183:5301–5310. doi: 10.4049/jimmunol.0900995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li C, et al. IL-17 response mediates acute lung injury induced by the 2009 pandemic influenza A (H1N1) virus. Cell research. 2012;22:528–538. doi: 10.1038/cr.2011.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang W, et al. Monoclonal antibody against CXCL-10/IP-10 ameliorates influenza A (H1N1) virus induced acute lung injury. Cell research. 2013;23:577–580. doi: 10.1038/cr.2013.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hamada H, et al. Tc17, a unique subset of CD8 T cells that can protect against lethal influenza challenge. Journal of immunology. 2009;182:3469–3481. doi: 10.4049/jimmunol.0801814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bozoyan L, Dumas A, Patenaude A, Vallieres L. Interleukin-36gamma is expressed by neutrophils and can activate microglia, but has no role in experimental autoimmune encephalomyelitis. Journal of neuroinflammation. 2015;12:173. doi: 10.1186/s12974-015-0392-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cook DN, et al. Requirement of MIP-1 alpha for an inflammatory response to viral infection. Science. 1995;269:1583–1585. doi: 10.1126/science.7667639. [DOI] [PubMed] [Google Scholar]
- 44.Dawson TC, Beck MA, Kuziel WA, Henderson F, Maeda N. Contrasting effects of CCR5 and CCR2 deficiency in the pulmonary inflammatory response to influenza A virus. The American journal of pathology. 2000;156:1951–1959. doi: 10.1016/S0002-9440(10)65068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carey MA, et al. Contrasting effects of cyclooxygenase-1 (COX-1) and COX-2 deficiency on the host response to influenza A viral infection. Journal of immunology. 2005;175:6878–6884. doi: 10.4049/jimmunol.175.10.6878. [DOI] [PubMed] [Google Scholar]
- 46.Aoyagi T, et al. Activation of pulmonary invariant NKT cells leads to exacerbation of acute lung injury caused by LPS through local production of IFN-gamma and TNF-alpha by Gr-1+ monocytes. International immunology. 2011;23:97–108. doi: 10.1093/intimm/dxq460. [DOI] [PubMed] [Google Scholar]
- 47.Seki M, et al. Critical role of IL-1 receptor-associated kinase-M in regulating chemokine-dependent deleterious inflammation in murine influenza pneumonia. Journal of immunology. 2010;184:1410–1418. doi: 10.4049/jimmunol.0901709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Densmore JC, et al. Endothelium-derived microparticles induce endothelial dysfunction and acute lung injury. Shock. 2006;26:464–471. doi: 10.1097/01.shk.0000228791.10550.36. [DOI] [PubMed] [Google Scholar]
- 49.Dinkla S, Brock R, Joosten I, Bosman GJ. Gateway to understanding microparticles: standardized isolation and identification of plasma membrane-derived vesicles. Nanomedicine. 2013;8:1657–1668. doi: 10.2217/nnm.13.149. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.