Forgive my quoting the great Albert Einstein in my title (Isaacson, 2007, epigraph), but his words seemed perfect for this Perspectives article. Life and ageing in good health are synonymous with physical activity, which contributes to maintain a physiological balance (equilibrium) until a rupture point caused by uncompensated cumulative damage. Sedentariness is unnatural and the human body is designed for great physical activity, if we take the example of master athletes. In support of this statement, sedentariness brings prematurely its burden of morbidities and associated loss of quality of life with age; in Canada alone, the total economic costs of physical inactivity represented 2.6% of the total health care costs in 2004, more than obesity alone (Katzmarzyk & Janssen, 2004).
In the current issue of The Journal of Physiology, Hotta and colleagues showed that even when exercise training is started late in life in sedentary 24‐month‐old Fisher 344 rats with typical signs of age‐related cardiac and coronary dysfunction, the metabolic demand required by physical exercise can be met, while cardiac and coronary functions significantly improve after only 10 weeks of training (Hotta et al. 2017). First, this demonstrates that in these old animals with the sole fault of being sedentary, the heart is still able to respond to exercise and to improve both myocardium and coronary microvascular functions. Second, the fact that chronic exercise restores myocardial perfusion to the level measured in 4‐month‐old rats could be suggestive of angiogenesis, even in old animals. Conclusion? Unless ventricular dysfunction is overt with clinical signs of heart failure and irreversible damage, the heart and the coronary microcirculation are fit to run anytime; training will only take you further. The authors propose that this restoration of myocardial function is partly due to normalized coronary endothelial dilatory properties and improved antioxidant defences. During the transition from a sedentary to an active lifestyle, is it the coronary microcirculation that drives cardiomyocyte improvement, or is it the augmented cardiomyocyte activity that drives endothelial coronary improvement? In agreement with the authors’ hypothesis, it is known that the endothelium benefits from repeated acute rises in shear rate caused by exercise, leading to an optimized blood delivery (Seals et al. 2009). On the other hand, it is the increase in sympathetic activity that is at the origin of the increase in heart rate during exercise; it stimulates cardiac work that creates a need for a rise in coronary flow, a transitory and repeated increase in shear rate beneficial to the endothelium. Thus, the increase in myocardial activity may drive endothelial improvement in the coronary microcirculation. The sympathetic nervous system is instrumental in the initial cardiac response to exercise, as demonstrated in transplanted patients with denervated hearts who have a delayed adaptive response to exercise in terms of heart rate and blood delivery (Awad et al. 2016). Hence, when we decide to run, this activates our skeletal muscles and the nervous system initiates the cardiac response; this leads to an increase in blood flow in the coronaries and the skeletal muscle (Fig. 1).
Figure 1. Schematic illustration of integrative pathways of the body exposed to physical activity.
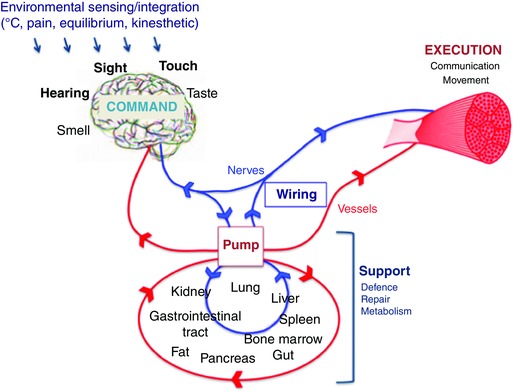
Skeletal muscles are responsible for movements and to communicate to the external world under the command of the brain. Each variation in physical activity requires metabolic matching and fast adaptation of heart rate to optimize blood delivery for metabolism, hormonal signalling, etc. The balance between all organ functions is therefore essential.
The central nervous system is instrumental to the maintenance of the equilibrium triggered by regular exercise. Recurrent episodes of high intensity physical exercise increase heart rate (acute increases in sympathetic nervous system activity), while in between these episodes, resting heart rate is maintained low because exercise has up‐regulated the counter‐regulatory parasympathetic system that is also a potent anti‐inflammatory system (Olshansky, 2016). With sedentariness, resting heart rate increases because the parasympathetic drive diminishes. The imbalance created by sedentariness between the sympathetic and parasympathetic nervous systems could be sufficient to create the disequilibrium and explain the increased risk of chronic inflammatory diseases with age (hypertension, insulin resistance, obesity, dyslipidaemia). Consequently, a better cardiopulmonary fitness is associated with a lower blood pressure and heart rate, and most importantly, a better blood pressure trajectory with ageing (Liu et al. 2014). But the resilience of the body is amazing: it is able to respond to exercise and to regain equilibrium after life‐long sedentariness. This is clearly what the present study of Dr Muller‐Delp's group shows and should encourage physicians to ‘prescribe’ physical exercise to the elderly, and more generally to all sedentary individuals able to exercise. Our health system is not as resilient as our body and in times of shortage of resources, it should be reinforced that our only hope to reduce the societal and cost burden in the future is to favour a healthy life style. The promise of a better quality of life should be a strong incentive. Life is [indeed] like riding a bicycle. To keep your balance you must keep moving!
Additional information
Competing interests
None declared.
Linked articles This Perspective highlights an article by Hotta et al. To read this article, visit https://doi.org/10.1113/JP274172.
References
- Awad M, Czer LS, Hou M, Golshani SS, Goltche M, De Robertis M, Kittleson M, Patel J, Azarbal B, Kransdorf E, Esmailian F, Trento A & Kobashigawa JA (2016). Early denervation and later reinnervation of the heart following cardiac transplantation: A review. J Am Heart Assoc 5, e004070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotta K, Chen B, Behnke BJ, Ghosh P, Stabley JN, Bramy JA, Sepulveda JL, Delp MD & Muller‐Delp JM (2017). Exercise training reverses age‐induced diastolic dysfunction and restores coronary microvascular function. J Physiol 595, 3703–3719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzmarzyk PT & Janssen I (2004). The economic costs associated with physical inactivity and obesity in Canada: an update. Can J Appl Physiol 29, 90–115. [DOI] [PubMed] [Google Scholar]
- Isaacson W (2007). Einstein: His Life and Universe, Epigraph. Simon & Schuster, New York. [Google Scholar]
- Liu J, Sui X, Lavie CJ, Zhou H, Park YM, Cai B, Liu J & Blair SN (2014). Effects of cardiorespiratory fitness on blood pressure trajectory with aging in a cohort of healthy men. J Am Coll Cardiol 64, 1245–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olshansky B (2016). Vagus nerve modulation of inflammation: Cardiovascular implications. Trends Cardiovasc Med 26, 1–11. [DOI] [PubMed] [Google Scholar]
- Seals DR, Walker AE, Pierce GL & Lesniewski LA (2009). Habitual exercise and vascular ageing. J Physiol 587, 5541–5549. [DOI] [PMC free article] [PubMed] [Google Scholar]


