Abstract
Background:
Blood stasis has received increasing attention in research related to traditional Chinese medicine (TCM) and integrative Chinese and Western medicine. More than 90% of research studies use hemorheology indexes to evaluate the establishment of animal blood stasis models rather than pathological methods, as hemorheology index evaluations of blood stasis were short of the consolidated standard. The aim of this study was to evaluate the accuracy of hemorheology indexes in rat models of acute blood stasis (ABS) based on studies in which the ABS model had been confirmed by pathological methods.
Materials and Methods:
We searched the Chinese National Knowledge Infrastructure database (CNKI), Chinese Medical Journal Database (CMJD), Chinese Biology Medicine disc (CBM), Wanfang database, and PubMed for studies of rat blood stasis models; the search identified 18 studies of rat ABS models induced by subcutaneous injection of epinephrine combined with an ice bath. Each included study received a modified Collaborative Approach to Meta-Analysis and Review of Animal Data from Experimental Studies (CAMARADES) score list and methodological quality assessment, then data related to whole blood viscosity, plasma viscosity, platelet aggregation rate, erythrocyte aggregation index, and fibrinogen concentration were extracted. Extracted data were analyzed using Revman 5.3; heterogeneity was tested using Egger’s test.
Results:
A total of 343 studies of rat blood stasis were reviewed. Eighteen studies were included in this meta-analysis; the mean CAMARADES score was 3.5. The rat ABS model revealed a significant increase in whole blood viscosity (medium shear rate), whole blood viscosity (high shear rate), plasma viscosity, platelet aggregation rate, erythrocyte aggregation index, and fibrinogen concentration compared to controls, with weighted mean differences (WMD) of 2.42 mPa/s (95% confidence interval (CI) = 1.73 - 3.10); 1.76 mPa/s (95% CI = 1.28 - 2.24); 0.39 mPa/s (95% CI = 0.24 - 0.55); 13.66% (95% CI = 9.78 - 17.55); 0.84 (95% CI = 0.53 - 1.16); and 1.22 g/L (95% CI = 0.76 - 1.67), respectively. Subgroup analysis showed that whole blood viscosity, plasma viscosity, and the platelet aggregation rate test methods were more sensitive when measured at 0-24 h than at 24-72 h after induction of blood stasis.
Conclusions:
Rat blood stasis studies have incomplete experimental design and quality controls, and thus need an integrated improvement. Meta-analysis of included studies indicated that the unified hemorheology index of whole blood viscosity (medium and high shear rate), platelet aggregation rate, erythrocyte aggregation rate, and fibrinogen concentration might be used for assessment of rat ABS models independent of pathology methods.
Keywords: Blood stasis, hemorheology, traditional Chinese medicine, meta-analysis, rats
Introduction
Blood stasis is a common pathological mechanism of traditional Chinese medicine (TCM), and a common pathological basis of cardiovascular disease. The concept of blood stasis includes two types: poor blood stasis, and blood flow outside meridians. This paper focuses on poor blood stasis. The TCM classic reference Neijing (The Internal Canon of Medicine) did not propose the concept of “blood stasis,” but repeatedly mentioned “blood coagulation and weep” to highlight the pathological mechanisms of blood stasis. Around 220 AD, the Treatise on Fevers (shang han lun) officially proposed “blood stasis” as an important pathological condition. In the 14th century, Prescriptions for Universal Relief (pu ji fang) stressed that blood stasis plays a major role in the development of chronic diseases. TCM physicians Ye Tianshi in the 17th century and Wang Qing Ren in the 18th century highlighted the significance of blood stasis in the development and progression of diseases.
Blood stasis has attracted much attention in TCM and integrative Chinese and Western medicine research. Animal models of acute blood stasis (ABS) have been widely used to investigate the pathological changes of blood stasis. Blood flow retardation in the microvasculature, pathological performance of blood stasis, and increasing thrombus formation in vitro constitute the pathological features of blood stasis. More than 90% of studies use hemorheology indexes such as whole blood viscosity, plasma viscosity, erythrocyte aggregation indexes, and platelet aggregation rate, to evaluate the establishment of an animal blood stasis model rather than a pathological method (Gao et al., 2003). Hemorheology index evaluations of blood stasis lack consolidated standards and pathological support, but they are characterized by a variety of hemorheology indexes and easy application, and have been used as common evaluation criteria for studies focusing on therapeutic evaluations and pharmacology of blood stasis (He et al., 2005). Our study aimed to investigate the relationship between hemorheology indexes and rat models of ABS, based on the studies in which the ABS model had been confirmed by pathological methods.
Many methods are used to establish rat ABS models. The model of Qi stagnation and Cold condensation (QSCC), a common cause of acute blood stasis in TCM, used subcutaneous injection of epinephrine combined with an ice bath. This method accounted for a larger number of studies than others. This rat ABS model was established by two subcutaneous injections of epinephrine (8 μg/kg per injection, at an interval of 4 hours). Two hours after the first injection, the rats were subjected to a 5-min soak in ice water. The rat ABS model was established after the second injection.
Our study focused on rat ABS models induced by subcutaneous injection of epinephrine combined with an ice bath. Meta-analysis of whole blood viscosity, plasma viscosity, platelet aggregation rate, erythrocyte aggregation index, and fibrinogen concentration in the rat ABS model were conducted, and we estimated the accuracy and standardization of those indexes.
Materials and methods
Studies were included if they met the following criteria: (i) controlled studies that used an animal ABS model induced by subcutaneous injection of epinephrine combined with an ice bath; (ii) utilized rats as experimental subjects; (iii) assessed at least one of the following outcomes: whole blood viscosity, plasma viscosity, platelet aggregation rate, erythrocyte aggregation rate, or fibrinogen concentration; and (iv) applied pathological methods to a confirmed ABS model. Studies were excluded if (i) the ABS model was induced using other methods in combination with subcutaneous epinephrine injection combined with an ice bath, or (ii) data were presented in a way not suitable for meta-analysis.
Search strategy
Studies were identified through electronic databases, including the Chinese National Knowledge Infrastructure (CNKI), Chinese Medical Journal Database (CMJD), Chinese Biology Medicine disc (CBM), Wanfang database, and PubMed. The time period searched included all articles published before May 2016. The search terms used were as follows: “blood stasis,” “stasis of blood,” “xueyu,” “yuxue,” and “rat.” Limitations included “other animals.”
Study selection
The identification of eligible publications was conducted by one investigator (JXZ) based on inclusion and exclusion criteria; a second author (YL) was consulted if articles were questionable. The citations of included studies were read in detail to examine their agreement with inclusion criteria.
Methodological quality
Methodological quality assessment of eligible publications was conducted independently by two authors (YF, SDL). The Collaborative Approach to Meta-Analysis and Review of Animal Data from Experimental Studies (CAMARADES) was applied for methodological quality assessment criteria (Zeng et al., 2012), and adjusted criteria included 10 dimensions: sample size estimation, randomization application, ABS model in the theory of Qi stagnation and Cold condensation, model verification, negative side-effects of anesthetics on the cardiovascular system, experimental temperature control, application of blinding methods in results, experimental animal protection principles, publication through peer review, and conflicts of interest. CAMARADES was frequently used to determine the methodological quality of experimental animal studies (Macleod et al., 2004; Crossley et al., 2008).
Data extraction
A data extraction sheet was made, and two reviewers (JXZ, YL) conducted the extraction independently. Any disagreements were resolved by consultation. The following information was entered in the extraction sheet: study year, study design, animal strains, animal weight, animal cleanliness class, breeding facilities, randomization and group, anesthetic class, model replicating methods, and ethical principles. Data for whole blood viscosity, plasma viscosity, platelet aggregation rate, erythrocyte aggregation index, and fibrinogen concentration from each study were recorded. The data were recorded or calculated using mean and standard deviation.
Statistical analysis
Data of included studies were entered into Review Manager 5.3 (Cochrane Collaboration, Oxford, UK). A P-value < 0.05 was considered significant. Cochrane’s Q-statistic and I2 statistics were calculated and reported to assess the degree of heterogeneity (Higgins et al., 2002). If P > 0.05 and I2 < 50%, the study was considered homogeneous and a fixed effects model was applied. If P < 0.05 and I2 > 50%, the study was considered heterogeneous and a random effects model was applied. The random effects model was selected because it can be used to assume heterogeneity, it incorporates intra- and inter-study variability, including the potential impact on effect magnitude from publication variations, and it is suitable for the analysis of heterogeneous studies (Swardfager et al., 2013). The weighted mean difference (WMD) was used to analyze continuous data from the same determination method, and the standardized mean difference (SMD) was used for a pooled analysis of continuous data from different determination methods (Harris et al., 2008). 95% CIs were calculated. STATA 12 (StataCorp, LLC, College Station, TX, USA) was used to assess publication bias. The publication bias of included studies was assessed using Begg’s funnel plot and Egger’s publication bias plot based on Begg’s rank correlation test and Egger’s linear regression test respectively (Begg et al., 1994; Egger et al., 1997). Two subgroups were divided by sampling time: 0-24 h and 24-72 h.
Results
Identification of eligible studies
Database searches identified 343 references. Thirty-two references were excluded due to duplication and irrelevance, 312 descriptive studies remained. One hundred eighty-seven studies were excluded due to model replicating methods, another 64 studies were excluded because they lacked pathological assessment, and another 36 studies were excluded because they were not relevant to the study aims. An additional 7 studies were excluded due to inappropriate results forms or study design. Finally, 18 studies were included in this meta-analysis.
Figure 1.
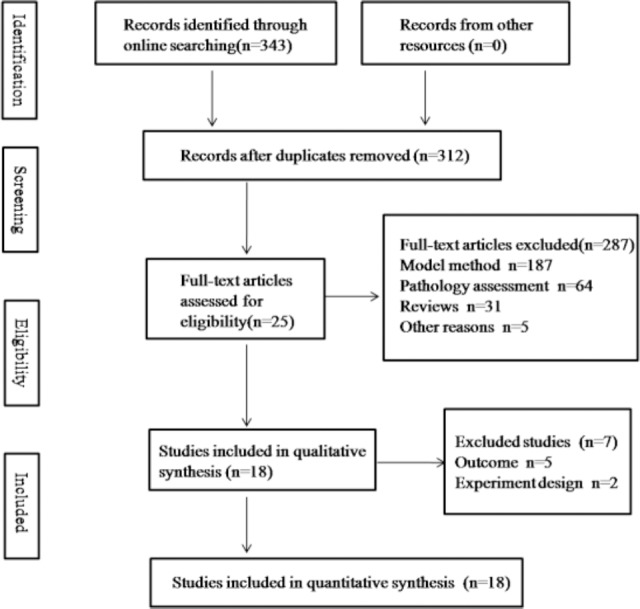
Flow diagram showing the number of records identified, screened, extracted, and included in the final analysis.
Study characteristics and methodological quality
Eighteen studies published from 1999 to 2016 were eligible for meta-analysis. A total of 348 rats were included; Wistar rats accounted for 27.59% of the total number of rats used; Sprague-Dawley rats accounted for 72.41%. Female rats made up 33.92% of the number of rats used; male rats accounted for 61.49%, and sex was not disclosed for the remaining 4.6%. Four studies used rats massing 200 g and below, 1 study used rats massing 300 g and above, and 13 studies used rats massing 200 to 300 g. Studies applied the same method for modeling: two subcutaneous injection of epinephrine combined with a 5-min ice bath midway between the two injections; the interval between the injections was 4 hours. One study used hematoxylin and eosin (HE) staining to assess rat ABS models, 1 study used blood perfusion quantity, 3 studies used the visual outcome of microcirculation, and 13 studies used an in vitro thrombus.
None of the included studies described the sample size calculation methods or randomization methods used. The anesthetic used included urethane in 3 studies, pentobarbital in 3 studies, chloral hydrate in 8 studies, and 4 studies that did not mention an anesthetic agent. None of the included studies described blinding methods used, animal ethics guidelines adhered to, or conflicts of interest. For methodological quality assessment, 3 studies scored 5 points, 3 studies scored 4 points, and 12 studies scored 3 points.
Table 1.
Characteristics of included studies
| Study author(s) | Rat strain and sex | Rat weight (g) | Number of control rats | Number of model rats | Anesthetic | Detection time after modeling(h) | Pathology assessment |
|---|---|---|---|---|---|---|---|
| Li et al., 2011) | Wistar male | 150-200 | 8 | 8 | Chloral hydrate | 1 | microcirculation + thrombus |
| Wang et al., 2011 | SD male | 350-450 | 10 | 10 | Chloral hydrate | 24 | thrombus |
| Zhang et al., 2016 | SD male | 250-350 | 10 | 10 | Chloral hydrate | 24 | thrombus |
| Shi et al., 2006 | Wistar Half male half female | 250-300 | 10 | 10 | Chloral hydrate | 24 | thrombus |
| Bao et al., 2008 | Wistar Half male half female | 250-300 | 10 | 10 | NA | 72 | thrombus |
| Deng et al., 2007 | SD female | 220-240 | 10 | 10 | Chloral hydrate | 20 | HE staining |
| Wang et al., 2007 | SD male | 200-220 | 10 | 10 | urethane | NA | thrombus |
| Guo et al., 2009 | SD Half male half female | 180-200 | 10 | 10 | Chloral hydrate | 12 | Blood perfusion |
| Gao et al., 2013 | Wistar Half male half female | 230-270 | 10 | 10 | urethane | 12 | thrombus |
| Si et al., 2007 | SD NA | 280-300 | 8 | 8 | pentobarbital | 12 | thrombus |
| Yin et al., 2008 | SD Half male half female | 280-320 | 8 | 8 | pentobarbital | 12 | thrombus |
| Li et al., 2010 | Wistar Half male half female | 250-300 | 10 | 10 | Chloral hydrate | 12 | thrombus |
| Peng et al., 2012 | SD Half male half female | 220-280 | 8 | 8 | NA | 12 | microcirculation |
| Guo et al., 2012 | SD Half male half female | 180-200 | 10 | 10 | Chloral hydrate | 12 | thrombus |
| Xie et al., 1999 | SD male | 230-260 | 10 | 10 | NA | NA | thrombus |
| Chen et al., 2012 | SD Half male half female | 248-288 | 10 | 10 | urethane | 24 | thrombus |
| Zhang et al., 2014 | SD Half male half female | 200-220 | 12 | 12 | pentobarbital | 24 | thrombus |
| Li et al., 2001 | SD male | 120-160 | 10 | 10 | NA | 24 | microcirculation |
Note: NA = not available
Table 2.
Methodological quality assessment of included studies
| Study | ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ⑨ | ⑩ | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Li et al., 2011 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Wang et al., 2011 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Zhang et al., 2016 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Shi et al., 2006 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Bao et al., 2008 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Deng et al., 2007 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Wang et al., 2007 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 |
| Guo et al., 2009 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Gao et al., 2013 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 |
| Si et al., 2007 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 4 |
| Yin et al., 2008 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 4 |
| Li et al., 2010 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Peng et al., 2012 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Guo et al., 2012 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Xie et al., 1999 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
| Chen et al., 2012 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 4 |
| Zhang et al., 2014 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 5 |
| Li et al., 2001 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 |
①: sample size estimation; ②: randomization application; ③: acute blood stasis (ABS) model in the theory of Qi stagnation and Cold condensation; ④: model verification; ⑤: anesthetic side-effects on the cardiovascular system; ⑥: experimental temperature control; ⑦: application of blinding method in results; ⑧: experimental animal protection principles; ⑨: publication through peer review; ⑩: conflicts of interest. (1 = positive; 0 = negative).
Whole blood viscosity changes
Whole blood viscosity meta-analysis included 15 studies, eight in the 0-24 h subgroup and seven in the 24-72 h subgroup. Studies were heterogeneous (χ2 = 261.77; P < 0.05; I2 = 95%). The random effects model and weighted mean difference (WMD) were used to assess differences in whole blood viscosity between the ABS experimental and control groups.
Low shear rate of whole blood viscosity changes
The low shear rate of whole blood viscosity increased in the ABS experimental group compared to the control group: showed an absolute difference between experimental and control rats: WMD = -7.74 mPa/s, (95% CI = -9.99 - 5.59; Z = 7.06; P < 0.05). The 0-24 h and 24-72 h subgroups of the model both increased compared to the control group: WMD = -11.45 mPa/s, (95% CI = -15.71 - 7.19; Z = 5.27; P < 0.05) and WMD = -3.05 mPa/s, (95% CI = -4.78 - 1.32; Z = 3.45; P < 0.05), respectively. A higher increase in whole blood viscosity was observed in the 0-24 h subgroup of the model.
Medium shear rate of whole blood viscosity changes
The ABS model experimental group showed an increase in medium shear rate of whole blood viscosity compared to the control group: WMD = -2.42 mPa/s, (95% CI = -3.1 - 1.73; Z = 6.94; P < 0.05). The ABS model showed significant increase in the 0-24 h and 24-72 h subgroups compared to the control group: WMD = -3.07 mPa/s, (95% CI, -3.98 - 2.15; Z=6.57, P < 0.05) and WMD = -1.7 mPa/s, (95% CI, -2.24 - 1.17; Z = 6.28; P < 0.05) respectively. The 0-24 h subgroup of the ABS model in showed the greatest degree of change in medium shear rate of whole blood viscosity.
High shear rate of whole blood viscosity changes
The ABS model experimental group showed an increase in high shear rate of whole blood viscosity compared to the control group: WMD = -1.76 mPa/s, (95% CI = -2.24 - 1.28; Z = 7.24; P < 0.05). The 0-24 h and 24-72 h subgroups of the ABS model both increased compared to the control group: WMD = -1.86 mPa/s, (95% CI = -2.34 - 1.37; Z = 7.52; P < 0.05) and WMD = -1.74 mPa/s, (95% CI = -2.57 - 0.9; Z = 4.07; P < 0.05) respectively.
Plasma viscosity changes
The plasma viscosity meta-analysis included 14 studies: 8 in the 0-24 h subgroup and 6 in the 24-72 h subgroup. Studies were heterogeneous (χ2 = 144.7; P < 0.05; I2 = 91%). The random effects model and WMD were used to assess differences in plasma viscosity between the ABS model and the control group.
The ABS model experimental group showed a clear increase in plasma viscosity compared to the control group: WMD = -0.39 mPa/s, (95% CI = -0.55 - 0.24; Z = 5.15; P < 0.05). Both the 0-24 h and 24-72 h subgroups of the experimental model showed increased plasma viscosity compared to the control group: WMD = -0.47 mPa/s, (95% CI = -0.71 - 0.23; Z = 3.87, P < 0.05) and WMD = -0.26 mPa/s, (95% CI = -0.4 - 0.11; Z = 3.47; P < 0.05) respectively.
Platelet aggregation rate changes
The platelet aggregation rate meta-analysis included 10 studies, 4 in the 0-24 h subgroup and 6 in the 24-72 h subgroup. Studies were heterogeneous (χ2 = 62.95; P < 0.05; I2 = 86%). The random effects model and WMD were used to assess differences in the platelet aggregation rate between the ABS model and the control group.
The ABS experimental group showed an increase in the platelet aggregation rate compared to the control group: WMD = -13.66%, (95% CI = -17.55 - 9.78; Z = 6.89; P < 0.05). The 0-24 h and 24-72 h subgroups of the ABS model both increased compared to the control group: WMD = -14.45%, (95% CI = -22.34 - 6.57; Z = 3.59; P < 0.05) and WMD = -12.8%, (95% CI = 14.61 - 10.98; Z = 3.47; P < 0.05), respectively.
Erythrocyte aggregation index changes
Erythrocyte aggregation index changes meta-analysis included 7 studies. Studies were heterogeneous (χ2 = 39.54; P < 0.05; I2 = 85%). The random effects model and WMD were used to assess differences in erythrocyte aggregation rate between the ABS model and the control group. The ABS experimental group showed a clear increase in erythrocyte aggregation index compared to the control group: WMD = -0.84, (95% CI = -1.16 - 0.53; Z = 5.26; P < 0.05).
Fibrinogen concentration changes
The meta-analysis of fibrinogen concentration changes included 7 studies. Studies were heterogeneous (χ2 = 30.68; P < 0.05; I2 = 77%). The random effects model and WMD were used to assess differences in fibrinogen concentration between the ABS model and the control group. The ABS experimental group showed a clear increase in fibrinogen concentration compared to the control group: WMD = -1.22 g/L, (95% CI = -1.67 - 0.76; Z = 5.28; P < 0.05).
Figure 2.
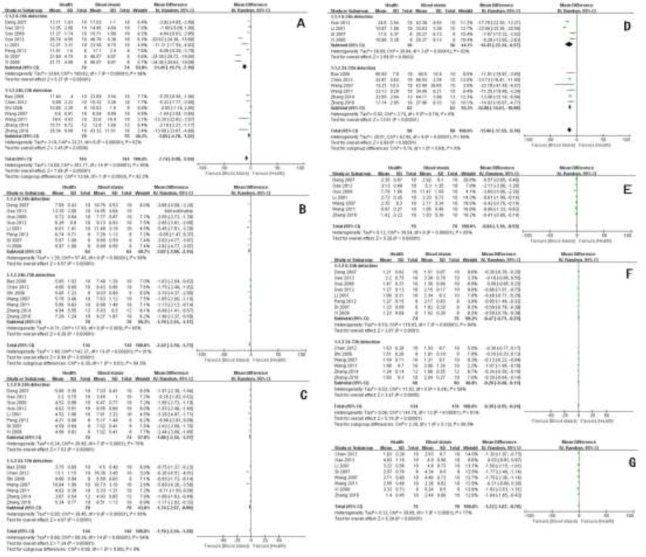
Forrest plot of hemorheology indexes. Mean, standard deviation, sample size, weighted mean difference (WMD), and 95% confidence interval (CI) were calculated from included studies. A: whole blood viscosity (low shear rate); B: whole blood viscosity (medium shear rate); C: whole blood viscosity (high shear rate); D: platelet aggregation rate; E: RBC aggregation index; F: plasma viscosity; G: fibrinogen concentration.
Risk of bias in included studies
Egger’s linear regression test was applied to analysis of the publication bias in the meta-analysis of whole blood viscosity, plasma viscosity, platelet aggregation rate, erythrocyte aggregation rate, and fibrinogen concentration. Egger’s publication bias plot of whole blood viscosity (low shear rate) revealed a significant publication bias (P = 0.002). Egger’s publication bias plots of whole blood viscosity (medium shear rate), whole blood viscosity (high shear rate), plasma viscosity, platelet aggregation rate, erythrocyte aggregation index, and fibrinogen concentration showed negative publication bias (P = 0.819, 0.391, 0.402, 0.221, 0.131, and 0.471, respectively).
Figure 3.
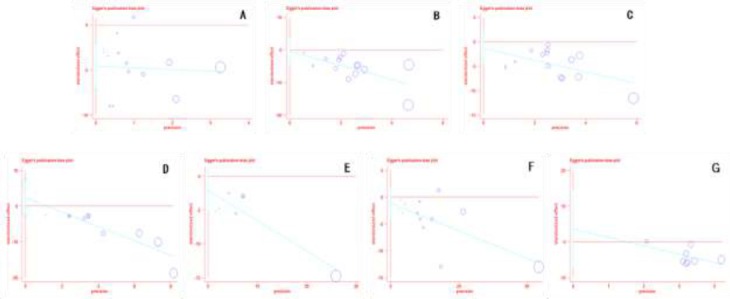
Funnel plot of publication bias (Egger’s test). A: whole blood viscosity (low shear rate); B: whole blood viscosity (medium shear rate); C: whole blood viscosity (high shear rate); D: platelet aggregation rate; E: RBC aggregation index; F: plasma viscosity; G: fibrinogen concentration.
Discussion
Blood stasis was characterized by microcirculation disorder and hemorheology changes. The hemorheology index has been regarded as a criterion to assess blood stasis in recent studies (Chen et al., 1990). The hemorheology index, including whole blood viscosity, plasma viscosity, platelet aggregation rate, erythrocyte aggregation rate, and fibrinogen concentration, increased during blood stasis (Jiang, 1990). We systematically reviewed the publication of rat ABS models and meta-analyzed the changes of the hemorheology indexes.
Literature retrieval results found that 34 different methods have been used to establish rat blood stasis models. Physical methods included alpine cold, anoxia, fatigue, positive acceleration, and radiation injury. Biochemical methods used drugs including endotoxins, epinephrine, and dextran. The majority of studies used a combination of two or three methods to establish a rat blood stasis model, such as subcutaneous injection of epinephrine combined with an ice bath, or a high-fat diet combined with swimming. The TCM features of cold coagulation, Qi stagnation, heat toxin, blood deficiency, and Qi deficiency in the rat blood stasis model corresponding to different modeling methods explained TCM blood stasis theory. Subcutaneous injection of epinephrine combined with an ice bath was the most frequently used modeling method based on TCM theory of Qi stagnation and Cold condensation, accounting for one third of rat blood stasis studies, but only about 17% of those studies assessed rat ABS model using pathology-based methods; the rest compared the hemorheology index between the control group and the experimental group. There was a lack of unified hemorheology index evaluation criteria. The methodological quality of included studies indicated a low-quality study. Inadequate experimental design and incomplete experimental quality control were the highest contributors to the low study quality.
Integrated conclusions of the meta-analysis of included studies was reached as follows: studies of the low shear rate of whole blood viscosity included a significant publication bias, and the results were not reliable. The medium shear rate of whole blood viscosity, high shear rate of whole blood viscosity, plasma viscosity, platelet aggregation rate, erythrocyte aggregation index, and fibrinogen concentration all increased compared to the control group. The hemorheology results above were extracted and analyzed from studies in which the ABS model had been tested using pathology methods. We conclude that the observed increases compared to the control group could serve as criteria for successful establishment of a rat ABS model, independent of pathological methods. Among those hemorheology indexes, the medium shear rate of whole blood viscosity and platelet aggregation rate were more sensitive. Both methods were also more sensitive at 0-24 hours sampling than at 24-72 hours, which suggests a better sampling timepoint in therapeutic studies. In general, the unified hemorheology index could be useful for assessing the rat acute blood stasis model; its advantages over pathology methods include convenient detection, variety, quantitative analysis, and accurate evaluation.
Conclusions
Rat blood stasis model studies have contributed a great deal to the understanding of blood stasis, a TCM pathology condition. Different rat blood stasis models have illustrated a modern medicine pathological mechanism from a variety of aspects, which have helped the global spread and development of the TCM blood stasis theory. However, systematic reviews of rat blood stasis studies revealed deficiencies in experimental design and quality control, which require integrated improvements. Meta-analysis of the included studies indicated that the unified hemorheology index of whole blood viscosity (medium and high shear rate), platelet aggregation rate, erythrocyte aggregation rate, and fibrinogen concentration could serve as criteria for the successful establishment of a rat ABS model independent of pathological methods.
Limitations
We included studies of rat ABS models induced by subcutaneous injection of epinephrine combined with an ice bath; the conclusion of meta-analysis determined that this model might not suitable for all the types of rat ABS models, but provides suggestions for the assessment of rat ABS models. The sample sizes of included studies were similar; there is a lack of large sample analyses of rat ABS models. Our review only focused on the assessment of rat ABS models. Many studies examining drug therapy for rat ABS models, which should be investigated in future studies.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Bao xuepeng, Zhao yu, Qu jibing. Effect of Huonaoxin oral solution on hemorheology indexes in rats acute blood stasis model [J] Journal of Apoplexy and Nervous Diseases. 2008;2008;02:224–225. [Google Scholar]
- 2.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias [J] Biometrics. 1994;50:1088–101. [PubMed] [Google Scholar]
- 3.Chen keji, Liang zijun. Researches of blood stasis and activating blood to remove stasis[M] Shanghai: Shanghai Scientific & Technical Publishers; 1990. pp. 499–600. [Google Scholar]
- 4.Chen yahui, Zhu mei, Li baoli, Zhu jianwen, Zhang zhengxiang. Effect of Suanbaizhiyou capsule on the hemorheology in rats acute blood stasis model [J] Chinese journal of Gerontics. 2012;13:2773–2775. [Google Scholar]
- 5.Crossley NA, Sena E, Goehler J. Empirical evidence of bias in the design of experimental stroke studies:a metaepidemiologic approach [J] Stroke. 2008;39(3):929–34. doi: 10.1161/STROKEAHA.107.498725. [DOI] [PubMed] [Google Scholar]
- 6.Deng gaopei, Luo huanhuan, Zhao ying. Effect of activating blood and dissolving stasis on morphology changes of uerine and ovarian in rats blood stasis model[J] Liaoning Traditional Chinese Medicine Journal. 2007;06:851–853. [Google Scholar]
- 7.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test [J] British Medical Journal. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gao han, Shang yingzhao, Hou anhui. Influence of Naomaining pill on the hemorheology and thrombus in vitro in rats acute blood stasis model[J] Neimenggu Journal of Traditional Chinese Medicine. 2013;2013;01:100–101. [Google Scholar]
- 9.Gao jian, Gu zhenlun, Wang tianyou. A review of studies related with blood stasis, hemorheology and traditional Chinese medicine [J] Chinese Journal of Blood Rheology. 2003;13(2):183–185. [Google Scholar]
- 10.Guo qin, Yang guangyi. Influence of Naodesheng pill on the blood hemorheology and microcirculation of blood stasis rats[J] Herald of Medicine. 2009;01:40–42. [Google Scholar]
- 11.Guo yudong, Wang zhibin, Zuo zeping, Hu yuchi, Wang bisong, Gao yang. Effect of Shuxuening injection on hemorheology and thrombosis of acute blood stasis model in rat[J] Clinical pharmacology Journal of Traditional Chinese Medicine. 2012;02:157–159. [Google Scholar]
- 12.Harris RJ, Bradburn MJ, Deeks JJ, Hardord RM. Metan: Fixed- and random-effects meta-analysis [J] Stata. 2008;2008;8(1):3–28. [Google Scholar]
- 13.He lan, Mao tengmin. Comparative study on effects of blood-breaking drugs san leng and e zhu on hemorheology indexes in rats with blood stasis syndrome[J] Journal of Anhui Traditional Chinese Medicine Colloge. 2005;06:35–37. [Google Scholar]
- 14.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta analysis [J] Statistics in Medicine. 2002;2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 15.Jiang chunhua. New edition of activating blood and dissolving stasis researches [M] Shanghai: Shanghai Medical Universiity Publishers; 1990. pp. 3–6. 41-50. [Google Scholar]
- 16.Li lun, Liu lin, Li chuanyu, Zhao ying. A comparative study on the effect of 3 kinds of activating blood and dissolving stasis in rats blood stasis model[J] Acta Chinese Medicine and Pharmacology. 2011;06:37–39. [Google Scholar]
- 17.Li luping, Yue haitao, Li tianshu, Lv wenwei, Lu mengmeng. Effect of hippophae rhamnoides extraction on the hemorheology and thrombus in vitro in rats acute blood stasis model [J] Chinese Traditional and Herbal Drugs. 2010;02:272–274. [Google Scholar]
- 18.Li xianliang, Xia daiyu, Li gang, Luo jianping, Shen yingjun, Kong jie. Effect of Yaotukang on hemorheology in rat blood stasis model and mesentery microcirculation in mouse together with anti-inflammatory and analgesic effect[J] Journal of Traditional Chinese Bone-setting. 2001;06:8–10+1. [Google Scholar]
- 19.Macleod MR, O’Collins T, Howells DW. Pooling of animal experimental data reveals influence of study design and publication bias [J] Stroke. 2004;35(5):1203–8. doi: 10.1161/01.STR.0000125719.25853.20. [DOI] [PubMed] [Google Scholar]
- 20.Peng yunsong, Chen suhong, Lv guiyuan, Lou zhaohuang, Wan xiaoqing. Effect of different processing products of Panax Notoginseng against rats model with blood-stagnation[J] Chinese Archives of Traditional Chinese Medicine. 2012;04:901–902. [Google Scholar]
- 21.Shi yanyu, Xu huibo, Ji fenglan, Zhang wei, Wen fuchun, Ding tao, Zhang dianwen, Sun xiaobo. Effect of FuFangJiangYaPain on hemorheology indexes in rats blood stasis model[J] Chinese Jounal of Experimental Traditional Medical Fomulae. 2006;05:54–55. [Google Scholar]
- 22.Si li, Huang shifu, Li tao, Guan shihe. Effect of Achyranthes Bidentata Saponin on hemorheology indexes in rats acute blood stasis model[J] Clinical Journal of Traditional Chinese Medicine. 2007;04:356–358. [Google Scholar]
- 23.Swardfager W, Herrmann N, Mazereeuw G. Zinc in depression:a meta-analysis [J] Biological Psychiatry. 2013;2013;74(12):872–878. doi: 10.1016/j.biopsych.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 24.Wang linlin, Ding anwei. Research on effects of total paeony glycoside on rat blood stasis model[J] Jounal of Nanjing Traditional Chinese Medicine University. 2011;06:552–554. [Google Scholar]
- 25.Wang youhua, Zhou duan, Yang jianmei, Cao min, Yuan suyun, Xiao meifang, Jin ruomin. Effect of Huoxueqiannyang prescription on hemorheology, platelet aggregation and thrombus in vitro in rats acute blood stasis model[J] Chinese Journal of Integrative Medicine on Cardio vascular and Cerebrovascular disease. 2007;08:699–700. [Google Scholar]
- 26.Xie yanhua, Li yurong, Wang siwang, Wang jianbo. Influence of hirudo extraction on platelet aggregation and thrombus in vitro in rats blood stasis model[J] Chinese Jounal of Traditional Medical Science and Technology. 1999;03:159–160. [Google Scholar]
- 27.Yin zheng, Hu guanyu, Xia xingxing, Chen qin. Effect of Qingbai capsule on hemorheological changes and formation of extracorporeal thrombus in rats with acute blood stasis[J] Chinese Journal of New Drugs. 2008;03:207–209+218. [Google Scholar]
- 28.Zeng xiantao, Zhuang liping, Yang zongguo, Dong shengjie. Meta-analysis series senven:Methodological quality assessment of non-randomized experimental study, Diagnostic test research and animal experiment research [J] Chinese Journal of Evidence Based Cardiovascular Medicine. 2012;06:496–499. [Google Scholar]
- 29.Zhang hong, Cao liang, Li na, Tang chaohui, Ding gang, Wang zhenzhong, Xiao wei. Effects of Tianshu Dropping pill on hemorheology and thrombosis thrombus in vitro in rats acute blood stasis model [J] Drugs & Clinic. 2014;05:471–475. [Google Scholar]
- 30.Zhang xiaoyan, Wang deqin, Li chuyuan, Zhang yifan, Tan renan. Effect of compound Danshen tablet on the rat model with blood stasis[J] Journal of Guandong Pharmaceutical University. 2016;03:344–347+361. [Google Scholar]


