Abstract
Background
The volume of joint replacement surgery has risen steadily in recent years, because the population is aging and increasingly wishes to preserve a high functional status onward into old age. Infection is among the more common complications of joint replacement surgery, arising in 0.2% to 2% of patients, or as many as 9% in special situations such as the implantation of megaprostheses. The associated morbidity and mortality are high. It is thus very important to minimize risk factors for infection and to optimize the relevant diagnostic and therapeutic strategies.
Methods
This review is based on pertinent publications retrieved by a selective search in PubMed, including current guidelines and expert recommendations.
Results
The crucial diagnostic step is joint biopsy for the identification of the pathogenic organism, which succeeds with over 90% sensitivity and specificity. If the prosthesis is firmly anchored in bone, the pathogen is of a type that responds well to treatment, and symptomatic infection has been present only for a short time, then rapidly initiated treatment can save the prosthesis in 35–90% of cases. The pillars of treatment are thorough surgical care (radical débridement) and targeted antibiotic therapy. On the other hand, if the prosthesis is loose or the pathogen is of a poorly treatable type, the infection can generally only be cured by a change of the prosthesis. This can be performed in either one or two procedures, always in conjunction with systemic antibiotic therapy tailored to the specific sensitivity and resistance pattern of the pathogen.
Conclusion
The risk of infection of an artificial joint is low, but the overall prevalence of such infections is significant, as the number of implanted joints is steadily rising. Artificial joint infections should be treated by a standardized algorithm oriented toward the recommendations of current guidelines. Many of these recommendations, however, are based only on expert opinion, as informative studies providing high-grade evidence are lacking. Thus, for any particular clinical situation, there may now be multiple therapeutic approaches with apparently comparable efficacy. Randomized trials are urgently needed.
Total endoprosthetic replacement of joints such as the hip joint is one of the most successful surgical procedures in orthopedic traumatology today (e1). Endoprosthetic joint replacement can give arthritis patients significant pain reduction, improved quality of life, and increased mobility, in both the medium and the long term (1). However, complications following artificial joint replacement pose a major challenge to patients and the physicians treating them. Complication rates following primary hip replacement, for example, are between 2 and 10%. Periprosthetic joint infections are the third-most common complication, accounting for 15.3% of cases, after aseptic loosening (36.5%) and prosthesis dislocation (17.7%) (2). They are associated with one-year mortality rates of between 8% and 25.9% (3, 4).
Periprosthetic joint infection refers to infection of tissues surrounding an artificial joint implanted in the body. Any artificial joint (e.g. hip, knee, elbow, ankle) can potentially be affected (e2). The number of joint replacement surgeries performed has been increasing steadily for years as a result of the ageing population and increasing patient demand to remain functional even in old age (5). The absolute number of revision surgeries and resulting complications is therefore also likely to increase (6– 8). This is essentially true for all artificial joints. According to recent research, the mean incidence of periprosthetic infections for primary total hip arthroplasty (THA) is between 0.2% and 2% (7, 9– 11). For revision surgeries it can be as high as 5% (12– 15). Figures on the incidence of infection vary according to location and type of artificial joint (hip <1%, knee <2%, elbow <9%, shoulder <1%, mega-endoprostheses/tumor endoprostheses 15%) and patient-dependent factors (16).
Periprosthetic joint infection is one of the most common reasons for revision surgery on an artificial joint (hip 15%, knee 25%) (17). Risk factors can be divided into the following groups:
Patient-dependent factors (e.g. excess weight, diabetes mellitus, nicotine/alcohol/drug abuse, malnutrition)
Surgery-dependent factors (e.g. prolonged surgery times)
Implant-dependent factors (e.g. mega-prostheses)
All of these increase the risk of periprosthetic joint infection (table 1) (18– 20).
Table 1. Relative risk of periprosthetic infection by underlying disease and circumstances (e6, e7).
| Risk factor | Relative risk [95% CI] |
| Excess weight (BMI ≥ 40 vs. <40) | 3.68 [2.25; 6.01] |
| Diabetes mellitus | 1.74 [1.45; 2.09] |
| Nicotine abuse | 1.83 [1.24; 2.70] |
| Alcohol abuse | 2.84 [0.81; 10.02] |
| *Prolonged surgery time (>120 minutes) | 1.58 [1.23; 2.03] |
*Prolonged surgery time is stated in e7 only.
BMI: Body-mass index; CI: Confidence interval
The most common pathogens causing periprosthetic joint infections are coagulase-negative staphylococci, Staphylococcus aureus, streptococci, enterococci, and Gram-negative bacteria (19, 21).
Pathogens may enter the joint either during surgery or later due to bacteremia; alternatively, they may spread to the joint continuously from an adjacent locus of infection (table 2). Classification, diagnostic procedure, and treatment recommendations are based on guideline or consensus recommendations (18, 22, 23– 27).
Table 2. Classification of periprosthetic infections (modified according to [19]).
| Time since surgery | |||
| 0 to 2 months | 3 to 24 months | Any time | |
| Type of infection | Early infection | Delayed (low-grade) infection | Late infection |
| Route of infection | Perioperative | Perioperative | Hematogenous (focus usually on lungs, skin, urinary tract, dental) or continuous spreading from elsewhere |
| Clinical symptoms | Local reddening, overheating, fever, pain, wound dehiscence, secretion | Persistent or new-onset pain, loosening, fistula formation | Acute or subacute |
|
Most common pathogens |
Staphylococcus aureus, streptococci, enterococci | Coagulase-negative staphylococci, Propionibacterium acnes | Staphylococcus aureus, Escherichia coli, streptococci |
Method
This article is based on a search of the literature in PubMed using the search terms „periprosthetic AND joint AND infection AND guidelines,“ „periprosthetic AND joint AND infection AND consensus,“ „prosthetic AND joint AND infection AND guidelines,“ and „prosthetic AND joint AND infection AND consensus.“ In addition to the international guideline and consensus recommendations of specialist societies representing both surgery and conservative medicine, primary literature was also evaluated. This article aims to summarize the current standards for diagnosis and treatment of joint prosthesis infections and to formulate them as a recommendation for clinical practice.
Classification systems
Periprosthetic joint infections are classified as either early or late, depending on the length of time from endoprosthesis implantation to onset of infection (table 2) (19). Early infections are usually defined as those with an interval of 2 weeks to 3 months between prosthesis implantation and onset of symptoms.
A more therapeutically relevant classification system is the distinction between acute and chronic infections (24). This is based on the time from the first symptoms of infection to the beginning of treatment rather than time from prosthesis implantation to onset of infection. In cases of acute infection—those detected and treated within a few weeks of the beginning of the infection—the formation of a biofilm on the implant is not yet complete. In other words, although the microorganisms are surrounded by a protective film of mucus made from extracellular polymeric substances that is unaffected by most antibiotics or the host‘s immune defenses, the film is still treatable (28, 29). In such cases, the aim of treatment is to rupture the biofilm while preserving the prosthesis. Different literature sources state that this type of infection has a latency period of between 2 and 4 weeks after the beginning of the infection (23– 25, 27). For infections that are treated later, expert opinion is that biofilm formation is complete. The bacteria have then transitioned to an untreatable latent state (28), so cure of the infection usually requires removal or replacement of the prosthesis.
Symptoms and clinical presentation
Acute periprosthetic joint infections usually result in the typical signs of inflammation: pain, swelling, reddening, and overheating of the affected joint, accompanied by fever. Postoperatively, impaired wound healing or secretion from the surgical wound, for example, may persist (30).
These typical signs of inflammation may be entirely absent in delayed or chronic infections, which are often caused by less virulent bacteria (low-grade infection). In these cases, the main symptoms include chronically persistent pain in the artificial joint, sometimes with implant loosening, and secondary implant failure (30).
Formation of a joint fistula in contact with the prosthesis is evidence of a joint infection (22– 24, 31). This is usually a sign of a chronic periprosthetic infection and occurs in a mean of 7% of cases (32); frequencies of up to 20% are described for Propionibacterium spp. (33). Pus in contact with the prosthesis is also evidence of a joint infection (23, 24).
Diagnosis, differential diagnosis
The main diagnostic challenge is to distinguish between periprosthetic joint infection and an aseptic implant complication. The diagnostic procedure for this is extensive and complex. Reliable detection of a low-grade, often subclinical infection caused by less virulent bacteria (e.g. coagulase-negative staphylococci) (34) is particularly difficult. Combining several methods of investigation (laboratory, microbiological, histopathological, and imaging) increases the probability of detecting an infection.
The gold standard for the diagnosis of periprosthetic joint infections is microbiological evidence of pathogens on the prosthesis, obtained via arthrocentesis or intraoperatively (35). Sensitivity and specificity of more than 90% are stated for this procedure (35). False positive or false negative findings can occur as a result of contamination when samples are taken or in patients who have already undergone antibiotic treatment (26, 27). Sufficient sample incubation time (ranging from 5 to more than 14 days) is crucial to pathogen detection (18, 31).
If possible, multiple samples should be taken from the joint, in order to distinguish between sample contamination and a pathogen that is causing infection. Two or more cultures that test positive for the same organism, particularly one that typically causes infection, is evidence of a periprosthetic infection even if the pathogen is of low virulence (23, 31). For highly virulent pathogens such as Staphylococcus aureus, evidence from one sample is sufficient to be considered relevant.
In clinically stable patients, antibiotic treatment should not be started until after samples have been taken via arthrocentesis or intraoperatively. If treatment has already been started, antibiotic administration should be halted for at least 2 weeks before samples are taken in order to increase the probability of detecting the pathogen causing the infection (18, 19, 23).
Laboratory diagnostics
Acute periprosthetic infections often result in changes on laboratory tests that are typical of infection. Guidelines recommend that white blood cell (WBC) count, C-reactive protein (CRP) level, and erythrocyte sedimentation rate (ESR) be determined (18, 23, 24). Although a lack of CRP or ESR elevation makes periprosthetic joint infection unlikely (18), it does not rule it out completely, as low-grade infections, for example, cannot always be detected using a laboratory test.
Overall, however, no laboratory test is sensitive or specific enough to confirm or rule out a periprosthetic joint infection definitively (36). Blood culture tests should be performed if there are signs of bacteremia (e.g. fever) (23, 24).
Arthrocentesis
Synovial fluid must be taken from the affected joint under strictly aseptic conditions. No local anesthetic should be used in the joint, as local anesthetics have a bactericidal effect and thus falsify the test result. Due to the depth of the site, hip arthrocentesis should be performed with radiological monitoring and recording (arthrography) (24).
If possible, some of the fluid should undergo microbiological (aerobic and anaerobic cultures) and pathological (consider crystallopathy) examination (23), and some WBC count, including differential (18, 23, 24). It is essential that samples be transported swiftly and undergo further processing rapidly, as transportation conditions are not ideal for pathogen survival (19).
If there is a discrepancy between the findings of laboratory tests and arthrocentesis, arthrocentesis should be repeated (18). If this cannot clarify the diagnosis, further diagnostic procedures such as intraoperative sample removal and possibly an additional imaging procedure such as scintigraphy or positron emission tomography (PET) should be performed if infection is likely (according to clinical or laboratory evidence). If infection is unlikely and no revision surgery of the joint is scheduled, it is recommended that the joint be re-evaluated 3 months later (18).
Removal of tissue from joint
Tissue samples should be taken from the affected joint for microbiological and pathological examination during scheduled surgery, including revision surgery, or beforehand if, for example, the safety of arthrocentesis is unclear or its findings are inconclusive and periprosthetic joint infection is suspected (18, 23, 24). This can be done either arthroscopically or in open surgery. Prophylactic perioperative antibiotic administration should not be performed (18, 19).
For optimum sample evaluation, 3 to 6 tissue samples should be taken from locations with major intraoperative macroscopic signs of infection for microbiological and pathological examination (18, 23, 31). Pathological examination of the samples involves performing a neutrophil count in 10 fields of view in order to detect inflammatory changes. The finding is positive if there are more than 10 granulocytes per high-power field (18, 19). The SLIM (synovial-like interface membrane) around the prosthesis should undergo pathological classification according to the Morawietz/Krenn consensus classification (37, 38). Two of the 4 types of SLIM in this classification indicate infectious pathogenesis:
Septic loosening (periprosthetic bacterial infection)
Combination of periprosthetic bacterial infection and wear
Intraoperative Gram staining does not appear to be beneficial (18).
Ultrasound treatment of prosthesis components removed intraoperatively (ultrasound bath treatment to remove the biofilm from the prosthesis, followed by microbiological examination of fluid) is not part of standard diagnostics and is controversial. However, it may be helpful in specific situations such as high risk of infection despite negative arthrocentesis findings or antibiotic administration in the days before surgery (18, 31).
Imaging diagnostics
The recommended radiological diagnostic procedure is 2-level conventional X-raying of the artificial joint (18, 23, 24, 31). Typical radiological signs of an infected artificial joint are periprosthetic osteolysis or loosening lines. Detectable periarticular calcification on X-ray may also indicate infection.
Other cross-sectional imaging diagnostic procedures (CT, MRI) are associated with artefacts caused by metal implants. They should therefore only be used when indicated in specific circumstances, possibly with administration of a contrast medium (18, 23).
Other radiological diagnostic procedures such as 99mTc bone scintigraphy and PET are not part of standard diagnostics. They should be used only in isolated cases, where specifically indicated (18, 23, 24, 31).
Studies available to date
To date there are no available randomized controlled trials on surgery (preservation of prosthesis, one-stage or two-stage revision) or antibiotic therapy (duration of treatment, time of switch to oral administration).
However, 3 randomized trials are currently ongoing. These compare 6-week versus 12-week antibiotic treatment (e3), oral versus intravenous antibiotic treatment (e4), and one-stage versus two-stage prosthesis revision (e5). Their findings are not yet available.
Treatment
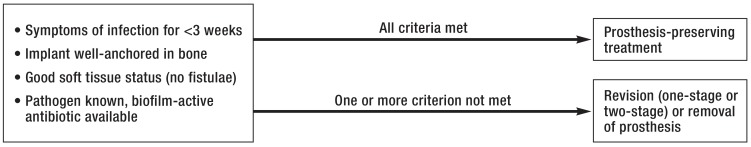
In order to decide whether a prosthesis-preserving strategy can be pursued, the prosthesis infection must be correctly classified as either acute or chronic on the basis of symptom duration. Another decisive factor is whether the prosthesis is well-anchored in the bone or has loosened (figure 1).
Figure 1.
Treatment algorithm (modified according to [19])
An attempt at prosthesis-preserving treatment is usually justified if the infection is acute, the implant is well-anchored, soft tissues are intact, and the pathogen is easily treatable (figure 1) (18, 23, 24, 31, 39). Such treatment consists of aggressive surgical debridement and, if possible, replacement of the prosthesis parts not anchored in the bone (e.g. femoral head, inlay), in order to reduce the pathogen population as much as possible. This can be repeated until the infection is under control. This surgical treatment must be combined with targeted, antibiogram-guided antibiotic treatment that penetrates the bone; if there is evidence of staphylococci, this should include a biofilm-active antibiotic such as rifampicin or fosfomycin. Antibiotics are initially administered intravenously; a switch to oral administration is possible after 2 to 6 weeks if clinical response is good (23). Antibiotic therapy should usually last at least 6 weeks to 3 months for prosthesis-preserving treatment (23, 24). Some authors propose a treatment duration of up to 6 months, particularly for infections following total knee replacement (23). Appropriate treatment makes it possible to preserve the prosthesis in 35 to 90% of cases (40). Because the necessary antibiotic therapy is of long duration, it is important to monitor for adverse drug effects such as gastrointestinal effects, blood count changes, kidney and liver dysfunction, and drug interactions.
Prosthesis-preserving treatment is likely to fail if infection is caused by difficult-to-treat pathogens such as small-colony variant staphylococci, enterococci, quinolone-resistant Pseudomonas aeruginosa, any multiresistant pathogens/rifampicin resistance, pathogens with no orally bioavailable antibiotic, or fungi (24) (Figure 2).
Figure 2.
Treatment algorithm for confirmed periprosthetic infection, based on guideline recommendations
*1Standard procedure is to switch to oral administration after 2 weeks if clinical response is good (wound dry/normal, pain decreasing) and C-reactive protein (CRP) is normal; 4 weeks‘ IV antibiotic treatment if wound is not healing correctly/CRP remains high.
*2DTT: Difficult-to-treat pathogen: small-colony variant staphylococci, enterococci, quinolone-resistant Pseudomonas aeruginosa, all multiresistant pathogens/rifampicin resistance, pathogens with no orally bioavailable antibiotic
IV: Intravenous; SR: Sample removal; p.o.: Per os
For chronic infections, in which biofilm formation must be assumed to be complete (latency time between onset of infection and beginning of treatment more than 3 to 4 weeks), and when the prosthesis is not firmly anchored in the bone, removal or revision of the prosthesis is usually required to cure the infection. Depending on the pathogen spectrum and the patient‘s situation, this may be either as a one-stage or, as usually preferred in clinical practice, as a two-stage procedure. If the pathogen is known and soft tissues are intact, removal of the infected prosthesis and implantation of a new prosthesis can be performed in a single surgery. For two-stage surgery, the infected prosthesis is first removed, aggressive debridement is performed, and a temporary, antibiotic-releasing spacer is inserted; a new prosthesis is then implanted in a subsequent surgery (23, 24, e8). For two-stage revision, the new prostheses may be implanted either early (short interval, 2 to 3 weeks after prosthesis removal, new prosthesis implanted during antibiotic treatment) or after a delay (long interval, usually 6 to 8 weeks after prosthesis removal), depending on the spectrum of the pathogen and soft tissue and bone status (24). Options for mobilization during the prosthesis-free interval in cases of two-stage revision range from complete immobilization to full weight bearing. This must be decided on a case-by-case basis.
In addition to surgical treatment, systemic antibiotic therapy is also essential in these cases. Antibiotics must be administered first intravenously, then orally after 2 to 6 weeks if clinical response is good. Oral administration is only ever possible if an antibiotic that penetrates the bone well and has high bioavailability is available. Unlike prosthesis-preserving treatment, with two-stage prosthesis revision there is no need to administer a biofilm-active antibiotic initially until a new prosthesis is implanted at the site, which may still be infected. Durations of antibiotic treatment ranging from 6 weeks to 3 months after prosthesis removal are recommended.
In justified exceptional cases, such as very poor bone status, seriously ill patients, or if the patient so wishes, no new joint prosthesis is implanted (girdlestone) (23). Leaving the infected prosthesis in situ and creating a chronic fistula and/or administering antibiotic suppression therapy until the affected extremity is amputated may also be a treatment option in individual cases (23, 27).
Summary
Infection of a total endoprosthesis is a traumatic event for patients and is associated with high treatment costs (39, e8). Infection prophylaxis is therefore critical. In addition to preoperative risk assessment and risk minimization, infection prophylaxis includes both swift, appropriate surgery that minimizes surgical risk and a surgical team with sufficient experience. Treatment optimization can cut long-term costs and reduce the risk for patients. Diagnosis and treatment should follow a standardized algorithm and comply with available guideline recommendations (Figure 2). The findings of currently ongoing randomized trials on periprosthetic infections are not yet available.
Key Messages.
The risk of infection following primary prosthesis implantation is approximately 0.2 to 9%, depending on the joint replaced. It is substantially higher for revision operations.
Determining what pathogen is causing the infection is crucial to diagnosis. This can be done via arthrocentesis or by taking a sample from the joint during surgery.
Evidence of pathogens in the joint cavity, a fistula in contact with the joint, or pus in the joint cavity is evidence of an infection in the joint.
Prosthesis infections should be treated in line with a standardized algorithm based on recommendations set out in guidelines.
It may be possible to preserve the prosthesis, if treatment is begun swiftly, using debridement and replacement of artificial parts followed by antibiotic treatment; this depends on the nature of the case (symptom duration, pathogen type, bone stock, prosthesis anchoring). Revision surgery is usually unavoidable in cases of loosening or infections caused by difficult-to-treat pathogens.
Acknowledgments
Translated from the original German by Caroline Shimakawa-Devitt, M.A.
Footnotes
Conflict of interest statement Dr. Otto-Lambertz has received lecture fees from RG Gesellschaft für Information & Organisation mbH.
PD Dr. Jung has received reimbursement of conferences fees and travel expenses from Novartis and Gilead. She has received lecture fees from Labor Stein, Novartis, Astellas Pharma, Alere GmbH, and Basilea Pharmaceutica AG. She has received trial funding (third-party funds) from Infectofos.
The other authors declare that no conflict of interest exists.
References
- 1.Meftah S, Belhaj K, Zahi S, Mahir L, Lmidmani F, El Fatimi. A comparison of functional outcomes and quality of life after THA according to indication about 210 THA. Ann Phys Rehabil Med. 2016;59S (Epub ahead of print). [Google Scholar]
- 2.Wetters NG, Murray TG, Moric M, Sporer SM, Paprosky WG, Della Valle CJ. Risk factors for dislocation after revision total hip arthroplasty. Clin Orthop Relat Res. 2013;471:410–416. doi: 10.1007/s11999-012-2561-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gundtoft PH, Pedersen AB, Varnum C, Overgaard S. Increased mortality after prosthetic joint infection in primary THA. Clin Orthop Relat Res. 2017 doi: 10.1007/s11999-017-5289-6. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zmistowski B, Karam JA, Durinka JB, Casper DS, Parvizi J. Periprosthetic joint infection increases the risk of one-year mortality. J Bone Joint Surg Am. 2013;95:2177–2184. doi: 10.2106/JBJS.L.00789. [DOI] [PubMed] [Google Scholar]
- 5.Wengler A, Nimptsch U, Mansky T. Hip and knee replacement in Germany and the USA—analysis of individual inpatient data from German und US hospitals for the years 2005 to 2011. Dtsch Arztbl Int. 2014;11:407–416. doi: 10.3238/arztebl.2014.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iorio R, Robb WJ, Healy WL, et al. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: preparing for an epidemic. J Bone Joint Surg. 2008;90:1598–1605. doi: 10.2106/JBJS.H.00067. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 8.BVMed. Bundesverband Medizintechnologie - Weißbuch Gelenkersatz. www.bvmed.de/weissbuch-gelenkersatz (last accessed on 3 March 2017) [Google Scholar]
- 9.Gundtoft PH, Overgaard S, Schønheyder HC, Møller JK, Kjærsgaard-Andersen P, Pedersen AB. The „true„ incidence of surgically treated deep prosthetic joint infection after 32,896 primary total hip arthroplasties. Acta Orthop. 2015;86:326–334. doi: 10.3109/17453674.2015.1011983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ong KL, Kurtz SM, Lau E, et al. Prosthetic joint infection risk after total hip arthroplasty in the Medicare population. J Arthroplasty. 2009;24(6):105–109. doi: 10.1016/j.arth.2009.04.027. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz SM, Ong KL, Lau E, et al. Prosthetic joint infection risk after TKA in the medicare population. Clin Orthop Relat Res. 2010;468:52–56. doi: 10.1007/s11999-009-1013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahomed NN, Barrett J, Katz JN, et al. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87:1222–1228. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 13.Phillips CB, Barrett JA, Losina E, et al. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am. 2003;85-A:20–26. doi: 10.2106/00004623-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Urquhart DM, Hanna FS, Brennan SL, et al. Incidence and risk factors for deep surgical site infection after primary total hip arthroplasty: a systematic review. J Arthroplasty. 2010;25:1216–1212. doi: 10.1016/j.arth.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 15.Mahomed NN, Barrett J, Katz JN, et al. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87:1222–1228. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 16.Trampuz A, Zimmerli W. Diagnosis and treatment of implant-associated septic arthritis and osteomyelitis. Curr Infect Dis Rep. 2008;10:394–403. doi: 10.1007/s11908-008-0064-1. [DOI] [PubMed] [Google Scholar]
- 17.Bozic KJ, Kurtz SM, Lau E, et al. The Epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parvizi J, Della Valle CJ. AAOS: Clinical Practice Guideline: diagnosis and treatment of periprosthetic joint infections of the hip and knee. J Am Acad Orthop Surg. 2010;18:771–772. doi: 10.5435/00124635-201012000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351:1645–1654. doi: 10.1056/NEJMra040181. [DOI] [PubMed] [Google Scholar]
- 20.Gollwitzer H, Dombrowski Y, Prodinger PM, et al. Antimicrobial peptides and proinflammatory cytokines in periprosthetic joint infection. J Bone Joint Surg Am. 2013;95:644–651. doi: 10.2106/JBJS.L.00205. [DOI] [PubMed] [Google Scholar]
- 21.Lamagni T. Epidemiology and burden of prosthetic joint infections. J Antimicrob Chemother. 2014;69(1):i5–i10. doi: 10.1093/jac/dku247. [DOI] [PubMed] [Google Scholar]
- 22.Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J Arthroplasty. 2001;26:1136–1138. doi: 10.1016/j.arth.2011.09.026. [DOI] [PubMed] [Google Scholar]
- 23.Osmon DR, Berbari EF, Berendt AR, et al. Diagnosis and management of prosthetic joint infection: Clinical Practice Guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56:e1–e25. doi: 10.1093/cid/cis803. [DOI] [PubMed] [Google Scholar]
- 24.Société de Pathologie Infectieuse de Langue Française (SPILF) Recommendations for bone and joint prosthetic device infections in clinical practice (prosthesis, implants, osteosynthesis). Société de Pathologie Infectieuse de Langue Française. Med Mal Infect. 2010;40:185–211. doi: 10.1016/j.medmal.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Minassian AM, Osmon DR, Berendt AR. Clinical guidelines in the management of prosthetic joint infection. J Antimicrob Chemother. 2014;69(1):i29–i35. doi: 10.1093/jac/dku253. [DOI] [PubMed] [Google Scholar]
- 26.Frommelt L. [Guidelines on antimicrobial therapy in situations of periprosthetic THR infection] Orthopaede. 2004;33:822–828. doi: 10.1007/s00132-004-0677-5. [DOI] [PubMed] [Google Scholar]
- 27.Esposito S, Leone S, Bassetti M, et al. Italian guidelines for the diagnosis and infectious disease management of osteomyelitis and prosthetic joint infections in adults. Infection. 2009;37:478–496. doi: 10.1007/s15010-009-8269-2. [DOI] [PubMed] [Google Scholar]
- 28.Walter G, Kemmerer M, Kappler C, Hoffmann R. Treatment algorithms for chronic osteomyelitis. Dtsch Arztebl Int. 2012;109:257–264. doi: 10.3238/arztebl.2012.0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gbejuade HO, Lovering AM, Webb JC. The role of microbial biofilms in prosthetic joint infections. A review. Acta Orthop. 2015;86:147–158. doi: 10.3109/17453674.2014.966290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schmidt HG, Tiemann AH, Braunschweig R, et al. [Definition of the diagnosis Osteomyelitis-Osteomyelitis Diagnosis Score (ODS)]Z. Orthop Unfall. 2011;149:449–460. doi: 10.1055/s-0030-1270970. [DOI] [PubMed] [Google Scholar]
- 31.Parvizi J, Gehrke T, Chen AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J. 2013;95-B:1450–1452. doi: 10.1302/0301-620X.95B11.33135. [DOI] [PubMed] [Google Scholar]
- 32.Achermann Y, Stasch P, Preiss S, Lucke K, Vogt M. Characteristics and treatment outcomes of 69 cases with early prosthetic joint infections of the hip and knee. Infection. 2014;42:511–519. doi: 10.1007/s15010-014-0584-6. [DOI] [PubMed] [Google Scholar]
- 33.Rienmüller A, Borens O. Propionibacterium prosthetic joint infection: experience from a retrospective database analysis. Eur J Orthop Surg Traumatol. 2016;26:429–434. doi: 10.1007/s00590-016-1766-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knudtzen FC, Nielsen SL, Gradel KO, et al. Characteristics of patients with community-acquired bacteremia who have low levels of C-reactive protein (= 20 mg/L) J Infect. 2014;68:149–155. doi: 10.1016/j.jinf.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 35.Bauer TW, Parvizi J, Kobayashi N, et al. Diagnosis of periprosthetic infection. J Bone Joint Surg Am. 2006;88:869–882. doi: 10.2106/JBJS.E.01149. [DOI] [PubMed] [Google Scholar]
- 36.Moran E, Byren I, Atkins BL. The diagnosis and management of prostetic joint infections. J Antimicrob Chemother. 2010;65:45–54. doi: 10.1093/jac/dkq305. [DOI] [PubMed] [Google Scholar]
- 37.Krenn V, Otto M, Morawietz L, et al. [Histopathologic diagnostics in endoprosthetics: periprosthetic neosynovialitis, hypersensitivity reaction, and arthrofibrosis] Orthopade. 2009;38:520–530. doi: 10.1007/s00132-008-1400-8. [DOI] [PubMed] [Google Scholar]
- 38.Morawietz L, Classen RA, Schröder JH, et al. Proposal for a histopathological consensus classification of the periprosthetic interface membrane. J Clin Pathol. 2006;59:591–597. doi: 10.1136/jcp.2005.027458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kapadia BH, Berg RA, Daley JA, et al. Periprosthetic joint infection. Lancet. 2016;387:386–394. doi: 10.1016/S0140-6736(14)61798-0. [DOI] [PubMed] [Google Scholar]
- 40.Triantafyllopoulos GK, Soranoglou V, Memtsoudis SG, Poultsides LA. Implant retention after acute and hematogenous periprosthetic hip and knee infections: Whom, when and how? World J Orthop. 2016;7:546–552. doi: 10.5312/wjo.v7.i9.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- E2.Barg A, Wimmer MD, Wiewiorski M, Wirtz DC, Pagenstert GI, Valderrabano V. Total ankle replacement—indications, implant designs, and results. Dtsch Arztebl Int. 2015;111:177–184. doi: 10.3238/arztebl.2015.0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E3.ClinicalTrials.gov. Treatment of the infections on osteo-articular prostheses by 6 versus 12 weeks of antibiotherapy (DATIPO) https://clinicaltrials.gov/ct2/show/NCT01816009?term=datipo&rank=1 (last accessed on 26 February 2017) [Google Scholar]
- E4.Li HK, Scarborough M, Zambellas R, et al. Oral versus intravenous antibiotic treatment for bone and joint infections (OVIVA): study protocol for a randomised controlled trial. Trials. 2015;16 doi: 10.1186/s13063-015-1098-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E5.Strange S, Whitehouse MR, Beswick AD, et al. One-stage or two-stage revision surgery for prosthetic hip joint infection—the INFORM trial: a study protocol for a randomised controlled trial. Trials. 2016;17 doi: 10.1186/s13063-016-1213-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E6.Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD. Patient-related risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. PLoS One. 2016;11 doi: 10.1371/journal.pone.0150866. p. e0150866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E7.Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R. Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:844–850. doi: 10.1302/0301-620X.87B6.15121. [DOI] [PubMed] [Google Scholar]
- E8.Alp E, Cevahir F, Ersoy S, Guney A. Incidence and economic burden of prosthetic joint infections in a university hospital: a report from a middle-income country. J Infect Public Health. 2016;9:494–498. doi: 10.1016/j.jiph.2015.12.014. [DOI] [PubMed] [Google Scholar]