Summary
Background
Oxidative stress represents tissue damage caused by reactive forms of oxygen and nitrogen due to the inability of antioxidant mechanisms to reduce reactive forms into more stable ones. The aim of the study was to evaluate the influence of surgical trauma on nitric oxide (NO) and nitrotyrosine (NT) values in patients undergoing conventional and laparoscopic cholecystectomy.
Methods
A prospective study included sixty patients from the Department of Emergency Surgery, Clinical Centre of Serbia who were operated for gallstone related chronic cholecystitis. All the patients enrolled in the study underwent cholecystectomy; the first group was operated conventionally (30 patients – control group), while the second group was operated laparoscopically (30 patients – treatment group).
Results
There were no statistically significant differences in the values of NO and its postoperative changes in both groups, the conventionally operated group (p=0.943) and the laparoscopically operated group (p=0.393). We found an increase in NT values 24 hours postoperatively (p=0.000) in the conventionally operated patients, while in the group operated laparoscopically we didn’t find statistically significant changes in the values of NT (conventionally operated group (p=0.943) and laparoscopically operated group (p=0.393)).
Conclusions
In our study, we found a significant increase in NT values 24 hours postoperatively in conventionally operated patients i.e. the control group, vs. the treatment group. Further randomized studies are needed for a better understanding of the impact of surgical trauma on oxidative stress response.
Keywords: cholecystectomy, nitrotyrosine, nitric oxide, aparoscopy, stress
Kratak sadržaj
Uvod
Oksidativni stres predstavlja oštećenje tkiva izazvano reaktivnim oblicima kiseonika i azota usled nesposobnosti antioksidantnih mehanizama da redukuju reaktivne oblike u stabilnije forme. Cilj ove studije bio je da se proceni uticaj hirurške traume na vrednosti azot-monoksida (NO) i nitrotirozina (NT) kod pacijenata podvrgnutih konvencionalnoj i laparoskopskoj holecistektomiji.
Metode
Ova prospektivna studija obuhvatila je 60 pacijenata sa Klinike za urgentnu hirurgiju Kliničkog centra Srbije koji su operisani zbog hroničnog holecistitisa vezanog za kamen u žučnoj kesi. Svi pacijenti uključeni u studiju podvrgnuti su holecistektomiji, prva grupa konvencionalnoj (30 pacijenata – kontrolnagrupa), dok jedruga grupa operisana laparoskopski (30 pacijenata – terapijska grupa).
Rezultati
Nije bilo statistički značajnih razlika između vrednosti NO ili postoperativnih promena ovih vrednosti u obe grupe, konvencionalno operisanoj grupi (p=0,943) i laparoskopski operisanoj grupi (p=0,393). Otkrili smo porast vrednosti NT 24 časa posle operacije (p=0,000) kod konvencionalno operisanih pacijenata, dok u grupi operisanoj laparoskopski nismo pronašli statistički značajne promene vrednosti NT(konvencionalno operisana grupa: p=0,943 i laparoskopski operisana grupa: p=0,393).
Zaključok
U ovoj studiji, značajan porast vrednosti NT 24 časa posle operacije utvrđen je u kontrolnoj grupi konvencionalno operisanih pacijenata u odnosu na terapijsku grupu. Potrebne su dalje nasumične kontrolisane studije kako bi se bolje razumeo uticaj hirurške traume na odgovor na oksidativni stres.
Introduction
Cholecystectomy is only a curative solution in patients suffering from gallstones. Laparoscopic cholecystectomy todayrepresents a gold standard in place of open cholecystectomy due to lesser surgical trauma, shorter hospital stay and cosmetic effects. It was shown in several studies that beside the previously named advantages it causes weaker inflammatory and oxidative stress responses in contrast to open cholecystectomy (1–3).
It is known that nitric oxide (NO) is significant both as a cellular signalization mediator but also as a strong oxidative reagent (4, 5), especially in reactions with lipids (6), and its free radical derivative NO2 is one of the most important lipid peroxidation inductors (7). Nitric oxide associated oxidative stress creates several byproducts although many of them have short presence in serum so currently it is challenging to determine their serum values. One of its products which has a longer half-life in serum is nitrotyrosine or 3 nitrotyrosine. Values of NT are increased in many diseases and due to its stability and presence in body fluids such as plasma, bronchus aspirate or its metabolite in urine NHPA (3-nitro-4-hydroxyphenylacetic acid) it can be useful in the determination of nitric oxide associated oxidative stress damage.
The aim of this study was to evaluate the influence of surgical trauma on the values of nitric oxide (NO) and nitrotyrosine (NT) in patients undergoing conventional and laparoscopic cholecystectomy.
Material and Methods
This study included sixty patients from the Department of Emergency Surgery, Clinical Centre of Serbia who were operated for gallstone related chronic cholecystitis (30 patients – control group), while a second group was operated laparoscopically (30 patients – treatment group).
This study was designed as prospective. All the patients enrolled in the study underwent cholecystectomy, the first group conventional while the second group was operated laparoscopically. Patient age was between 36 and 78 years. Patients with chronic systemic illnesses, under the age of 18 and those with icterus were excluded from the study. Patients who participated in our study were not previously surgically treated. All patients had ultrasonographically confirmed gallstones without ultrasonographic signs of perforation, distention or stratification of gallbladder wall. Laboratory inflammation markers were within their reference values and preoperative risk was ASA I according to the Classification of the American Society of Anesthesiology. Conventional cholecystectomy was performed through a right subcostal incision, while a four-port technique was used for laparoscopic cholecystectomy. Serum samples were taken preoperatively, 24 and 72 hours postoperatively and were stored at –80°C degrees and analyzed using Nitrotyrosine ELISA Kit (ab113848) and Nitric Oxide Assay Kit (ab65328) (both kits were produced by Abcam.plc). The first kit used for measuring NT values is based on colorimetric examination of samples. Microplates which were provided in the kit were coated with NT containing antigen and if no NT antigens were present in a sample, all of the NT antibodies bonded on present antigens in microplates. After preparation, samples were added with HRP detector antibodies after which samples were incubated at room temperature for 2 hours and then analyzed using colorimetric examination at 600 nm for 15 minutes. Components of the kit used for NT were stored at +4 °C degrees and included 10x blocking buffer, 1x HRP development solution, 20x wash buffer, 3-nitrotyrosine BSA standard, extraction buffer, HRP conjugated 3nt detector antibody (1000x), nitrotyrosine coated 96-well solid plate and plate seals. Values of NT range from 10–2000 ng/mL. As for the NO kit, samples used for analysis were first deproteinized by centrifuge at 13 000 for 2 min at 4 °C after which supertant centrifuged again at the same rate for 15 minutes at 4 °C after which samples were ready for examination. Ranges of NO values in these sets were 0.1 nmol/mL – 10 nmol/mL and were examined colorimetrically at 540 nm according to the principle of examining nitrite and nitrate values in serum since most of NO in serum is oxidized in nitrite and nitrate. Components of the NO kit were stored at –20 °C and included assay buffer, enhancer (lyophilized), enzyme cofactor (lyophilized), Griess reagent R1 and R2, microtiter plate and plate cover, nitrate reductase (lyophilized), nitrate standard (lyophilized), nitrite standard (lyophilized).
Results
Demographic data about patients are shown in Table I. We divided patients who participated in our study in two groups. The first group was operated laparoscopically and the second was operated conventionally (open). Mean age in the first group was 60, 43±11.68, and in the second 55.43±12.47 years. Mean lasting time of conventional cholecystectomy was 112.53±12.99 and of laparoscopic 84.20 + 28.72. We didn’t find a statistically significant difference in age of the patients (p=0.114) but we found a statistically significant difference in the length of operation (p=0.000*) (Table I). None of the participants in this study was previously operated.
Table I.
Demographic data of patients (aχ2–test; bt–test; cMann Whitney test)
| Evaluated parameters | Operative technique | Significance | ||
|---|---|---|---|---|
| n (%)/(x±SD; (Med; min-max)) | Conventional | Laparoscopic | ||
| Number of patients | 30 | 30 | ||
| Sex | Female | 15 (50%) | 21 (70%) | ap = 0.114 |
| Male | 15 (50%) | 9 (30%) | ||
| Age | 60.43 + 11.68 | 55.43 + 12.47 | bp=0.114 | |
| (62.5; 29–75) | (56.5; 36–78) | |||
| Length of operation | 112.53 + 12.99 | 84.20+28.72 | cp=0.000* | |
| (113.5; 95–138) | (93; 25–125) | |||
After an analysis of the NO values in serum, we concluded that there were no statistically significant differences in its values and postoperative changes in both groups, in the conventionally operated group (p = 0.943) and laparoscopically operated group (p=0.393) (Table II, Figure 1).
Table II.
NO and p values obtained using aMann Whitney test; bFriedman test and cintergroup comparison.
| Observed parameter | Operative technique | Significance | ||
|---|---|---|---|---|
| (x±SD; (Med; min-max)) | Conventional | Laparoscopic | ||
| NO (nmol/mL) | 0h | 4.66 + 2.37 (4.06; 41.96–11.74) | 3.58+1.06 (3.33; 2.24–6.45) | ap = 0.128 |
| 24h | 4.56 + 1.80 (4.03; 2.14–9.01) | 3.95+1.27 (3.79; 1.94–6.83) | ap=0.209 | |
| 72h | 4.19 + 1.98 (4.6; 0–9.77) | 3.67 + 2.41 (4.33; 0–9.77) | ap=0.407 | |
| Significancec | bp=0.943 | bp=0.393 | ||
Figure 1.
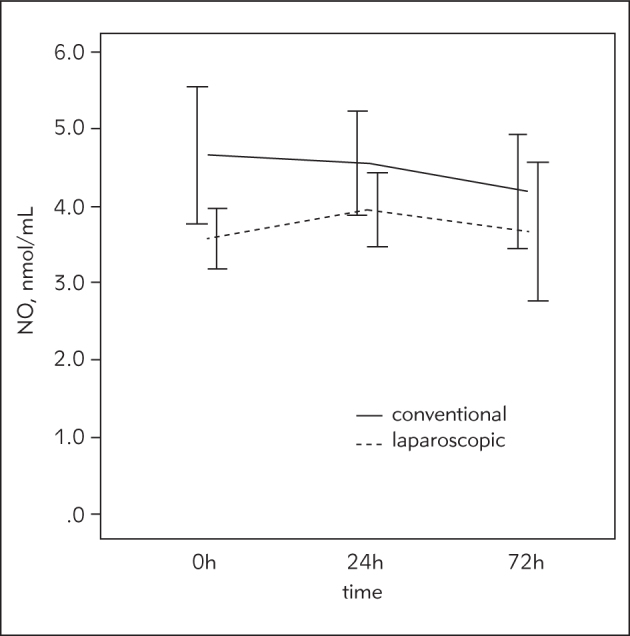
Time trend of NO values.
There was significant increase in NT values 24 hours postoperatively in the conventionally operated patients (p = 0.000*) while in the group operated laparoscopically we didn’t find statistically significant changes in the values of NT (p=0.291) (Table III, Figure 2).
Table III.
NT and p values obtained using Mann Whitney testa; Friedman testb and intergroup comparisonc
| Observed parameter | Operative technique | Significance | ||
|---|---|---|---|---|
| (x±SD; (Med; min-max)) | Conventional | Laparoscopic | ||
| NT (ng/mL) | 0h | 4.31+2.86 (3.68; 0.65–13.0) | 3.38+2.21 (3.46; 0.38–9.98) | ap=0.188 |
| 24h | 15.31+11.57 (11.98; 2.54–62.23) | 3.28 + 11.62 (3.09; 0.95–6.92) | ap=0.000* | |
| 72h | 6.05 + 5.10 (5.175; 0–25.2) | 3.04+2.38 (2.615; 0–7.89) | ap=0.007* | |
| Significancec | bp=0.000* | bp=0.291 | ||
Figure 2.
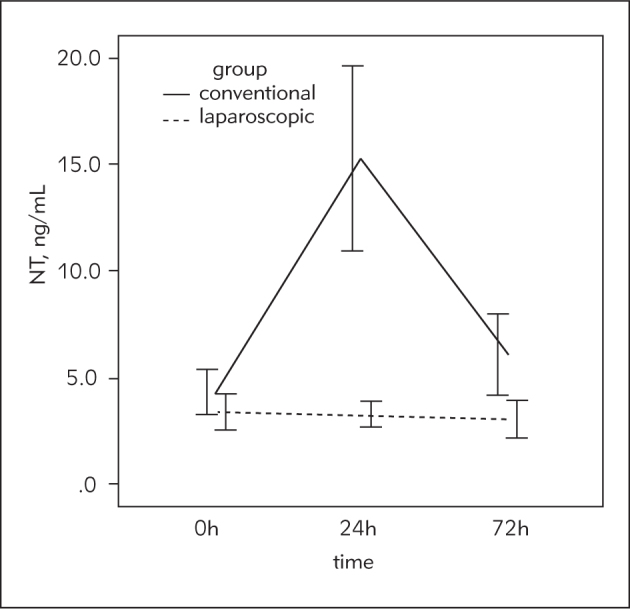
Time trend of NT values.
Discussion
Laparoscopic cholecystectomy experienced significant development in the last years of the 20th century andhas become a guide for elective treatment of cholelithasis. Elective laparoscopic cholecystectomy has become a »gold standard« for symptomatic cholelithiasis (8). Accordingly, laparoscopic cholecystectomy is the most common minimally invasive surgical procedure, while elective cholecystectomy is used in several special cases (9).
Some authors have also examined the clinical and financial advantages of laparoscopic cholecystectomy in contrast to open cholecystectomy. A study done by Schiertoma et al. (10)examined the number of hospital days, pain, postoperative monitoring and returning to normal activities. It was proved in this study that patients who were operated laparoscopically had shorter duration of hospital stay, lesser pain and faster time of returning to normal activities.
Beside these advantages, Zolfikaroglu et al. (11) proved in their study that laparoscopic cholecystectomy causes a lesser oxidative stress response.
Patients who participated in our study were not previously surgically treated. We examined two markers of nitrogen associated oxidative stress, nitric oxide (NO) and nitrotyrosine (NT) in patients who were operated laparoscopically and by open cholecystectomy with an aim to examine the influence of choice of operative technique and change of values of these parameters. Nitric oxide (NO) is a free radical gas which is produced in the vascular endothelium by nitric oxide synthase (NOS) by using the amino acid l-arginine as substrate. Currently, two isoforms of this enzyme are known, inducible NOS (iNOS) which is induced in macrophages and hepatocytes by cytokines and endotoxins; it is a calcium independent enzyme, unlike constitutive NOS (cNOS) which is calcium and calmodulin dependant (1). Reactive nature of NO causes it to undergo numerous chemical reactions, of which nitrosative and oxidative lead to the formation of reactive oxygen forms (12). It is known that the parameters which are correlated with metabolic reaction during operative treatment or in trauma return to normal values in short time. In one study which examined oxidative stress markers value changes in patients operated laparoscopically and by open cholecystectomy, it was concluded that the values of nitric oxide (NO) increased in both groups but returned to normal values on the first postoperative day (1).
In our study, we did not find statistically significant differences in values of NO in both groups pre- and post-operatively which may suggest that the duration of operation might correlate with changes in the values of oxidative stress parameters. Similar results were published by Zolfikaroglu et al. (11) who did not find statistically significant difference in value changes in patients who were operated laparoscopically and by open cholecystectomy.
Bukan et al. (1) examined the effects of open and laparoscopic cholecystectomy on oxidative stress. They concluded that the oxidative stress markers (nitrate+nitrite) increased in both groups, but the increase was significantly lesser in the group operated laparoscopically. Some of the hypotheses concerning increase or decrease in oxidative stress response suggest that these may be the effects of operative treatment as a stressor and impact of intraabdominal pressure in patients undergoing laparoscopic operation. Polat et al. (13) examined the effects of intraabdominal pressure increase on lipid peroxidation and protein oxidation in patients undergoing laparoscopic cholecystectomy who were divided in a group which was operated on 10 mmHg pressure and another on 15 mmHg. Despite an increase in oxidative stress markers in the 15 mmHg group there was no statistically significant difference between the two groups (12). Similar results in correlation with more intensive oxidative stress in patients undergoing open cholecystectomy were shown by Stipancic et al. (14). One of the factors which also might be correlated with higher oxidative stress is the length of operation. Ray et al. (15) examined the impact of length of operation in patients undergoing laparoscopic and open cholecystectomy on oxidative stress response, and they found higher increase of TBARS (thiobarbituric acid reacting substances) and decreasing levels of TAS (total antioxidant status) in patients who had longer operative time. Decreasing levels of TAS might correlate with progressive antioxidant system depletion caused by surgical trauma but further studies are needed (15). There are however also studies in which length of operating time did not correlate with increased oxidative stress markers. Aktimur et al. (16) examined the difference in the values of total oxidant status (TOS), total antioxidant status (TAS) and oxidative stress index (OSI) in patients who were operated for acute appendicitis by open and laparoscopic techniques. Length of operation was higher in patients undergoing open appendectomy. Previously mentioned markers values were determined preoperatively and 24 hours postoperatively. Their results showed that patients undergoing laparoscopic appendectomy had significantly higher values of TOS and OSI, but TAS values remained unchanged. Preoperative values were not significantly different in both groups (16). Increased values of previously mentioned markers (TOS and TAS) were also seen in patients who were operated for acute appendicitis in contrast with control group which was composed of healthy individuals (16). Beside in appendectomies and cholecystectomies, values of oxidative stress markers were determined in some other major surgical procedures such as colorectal operations. In one double-blind randomized study, values of 8-isoprostanes (8-epiPGF2a), protein carbonyls (PC), 8-hydroxyguanosine (8- OHG), and 3-nitrotyrosine (3-NT) were determined in patients undergoing laparoscopic and open operations. Values of these markers were significantly lower in patients undergoing laparoscopic operation which might also correlate with smaller trauma to the abdominal wall caused by the laparoscopic technique (18). A systematic review of 197 papers examined the values of oxidative stress markers in different operations, whether open, laparoscopic or the impact of pneumoperitoneum of stress oxidative markers. A majority of the studies reviewed showed higher oxidative stress immediately following open surgery. In the majority of studies, there were no discernable differences between open and laparoscopic surgery after 24 h. There were no attempts to determine the clinical significance of alteration in the oxidative stress markers. Despite the numerous studies that have been published, consensus has still not been achieved as to the respective effects of different surgical approaches (19).
In our study we found a significant increase in NT values 24 hours postoperatively in the conventionally operated control group, vs. the treatment group. This increase of nitrotyrosine values (NT) in patients who were operated by open cholecystectomy is correlated with duration of operation, and it also might be related with type of surgical technique. The analysis of NO values showed no significant differences in both groups. Additional randomized and multicentric studies are needed for further evaluation of the influence of surgical treatment and changes which happen in oxidative stress metabolism. Increased training and shorter length of operation might be beneficial in reducing systematic response to surgical treatment.
Study limitation
Number of patients. This is a type of »small study« but our results likely represent a large number of cases. To generalize the results, it is necessary to conduct the same research over a few centers to obtain stronger conclusions.
Footnotes
Conflict of interest statement: The authors stated that they have no conflicts of interest regarding the publication of this article.
References
- 1.Bukan MH, Bukan N, Kaymakcioglu N, Tufan T.. Effects of open vs. laparoscopic cholecystectomy on oxidative stress. The Tohoku Journal of Experimental Medicine. 2004;202(1):51–6. doi: 10.1620/tjem.202.51. [DOI] [PubMed] [Google Scholar]
- 2.Schietroma M, Carlei F, Mownah A, Franchi L, Mazzotta C, Sozio A, Amicucci G.. Changes in the blood coagulation, fibrinolysis, and cytokine profile during laparoscopic and open cholecystectomy. Surgical Endoscopy And Other Interventional Techniques. 2004;18(7):1090–6. doi: 10.1007/s00464-003-8819-0. [DOI] [PubMed] [Google Scholar]
- 3.Helmy SAK, Wahby MAM, El Nawaway M.. The effect of anaesthesia and surgery on plasma cytokine production. Anaesthesia. 1999;54(8):733–8. doi: 10.1046/j.1365-2044.1999.00947.x. [DOI] [PubMed] [Google Scholar]
- 4.Beckman J, Beckman TW, Chen J, Marshall PA., Freeman BA.. Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide and superoxide. Proceedings of the National Academy of Sciences of the United States of America. 1999;87(4):1620–4. doi: 10.1073/pnas.87.4.1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crow JP, Beckman JS.. The importance of superoxide in nitric oxide-dependent toxicity: evidence for peroxynitritemediated injury. Advances in Experimental Medicine and Biology. 1996;387:147–61. doi: 10.1007/978-1-4757-9480-9_21. [DOI] [PubMed] [Google Scholar]
- 6.Liu X, Miller MS, Joshi MS, Thomas DD, Lancaster JR.. Accelerated reaction of nitric oxide with O2 within the hydrophobic interior of biological membranes. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:2175–9. doi: 10.1073/pnas.95.5.2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kappus H.. A survey of chemicals inducing lipid peroxidation in biological systems. Chemistry and Physics of Lipids. 1987;45(2–4):105–15. doi: 10.1016/0009-3084(87)90062-4. [DOI] [PubMed] [Google Scholar]
- 8.Ogawa T, Shimizu S, Mizumoto K, Uchiyama A, Yokohata K, Chijiiwa K, Tanaka M.. Comparison of laparoscopic versus open cholecystectomy in patients with cardiac valve replacement. Journal of hepato-biliarypancreatic surgery. 2001;8(2):158–60. doi: 10.1007/s005340170040. [DOI] [PubMed] [Google Scholar]
- 9.Kraas E, Farke S.. Laparoscopic cholecystectomy – surgical standard in cholelithiasis. Kongressband/Deutsche Gesell schaft fur Chirurgie. Deutsche Gesellschaft fur Chirurgie. Kongress. 2001;119:322–7. [PubMed] [Google Scholar]
- 10.Schietroma M, Carlei F, Liakos C, Rossi M, Carloni A, Enang GN, Pistoia M.. Laparoscopic versus open cholecystectomy. An analysis of clinical and financial aspects. Panminerva Medica. 2001;43(4):239–42. [PubMed] [Google Scholar]
- 11.Zulfikaroglu B, Koc M, Soran A, Isman FK, Cinel I.. Evaluation of oxidative stress in laparoscopic cholecystectomy. Surgery Today. 2002;32(10):869–74. doi: 10.1007/s005950200169. [DOI] [PubMed] [Google Scholar]
- 12.Polat C, Yilmaz S, Serteser M, Koken T, Kahraman A, Dilek ON.. The effect of different intraabdominal pressures on lipid peroxidation and protein oxidation status during laparoscopic cholecystectomy. Surgical Endoscopy And Other Interventional Techniques. 2003;17(11):1719–22. doi: 10.1007/s00464-002-9258-z. [DOI] [PubMed] [Google Scholar]
- 13.Besedina A.. NO-synthase activity in patients with coronary heart disease associated with hypertension of different age groups. J Med Biochem. 2016;35:43–49. doi: 10.1515/jomb-2015-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stipancic I, Zarkovic N, Servis D, Sabolovic S, Tatzber F, Busic Z.. Oxidative stress markers after laparoscopic and open cholecystectomy. Journal of Laparoendoscopic & Advanced Surgical Techniques. 2005;15(4):347–52. doi: 10.1089/lap.2005.15.347. [DOI] [PubMed] [Google Scholar]
- 15.Ray D, Gayen S, Mondal R, Sen S, Dasgupta S.. Oxidative stress in cholecystectomy and possible correlation with operative time – a study conducted at BS Medical college, Bankura, WB, India. Journal of Evolution of Medical and Dental Sciences. 2013;1(2):6849–56. [Google Scholar]
- 16.Aktimur R, Gokakin AK, Deveci K, Atabey M, Topcu O.. Oxidative stress markers in laparoscopic vs. open appendectomy for acute appendicitis: A double-blind randomized study. J Minim Access Surg. 2016;12(2):143–7. doi: 10.4103/0972-9941.156203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dumlu EG, Tokaç M, Bozkurt B, Yildirim MB, Ergin M, Yalçin A. et al. Correlation between the serum and tissue levels of oxidative stress markers and the extent of inflammation in acute appendicitis. Clinics (Sao Paulo) 2014;69:677–82. doi: 10.6061/clinics/2014(10)05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pappas-Gogos G, Tellis C, Lasithiotakis K, Tselepis AD, Tsimogiannis K, Tsimoyiannis E. et al. Oxidative stress markers in laparoscopic versus open colectomy for cancer: A double-blind randomized study. SurgEndosc. 2013;27:2357–65. doi: 10.1007/s00464-013-2788-8. [DOI] [PubMed] [Google Scholar]
- 19.Arsalani-Zadeh R, Ullah S, Khan S, MacFie J.. Oxidative stress in laparoscopic versus open abdominal surgery: A systematic review. J Surg Res. 2011;169:59–68. doi: 10.1016/j.jss.2011.01.038. [DOI] [PubMed] [Google Scholar]


