Abstract
Celiac crisis is a rare life-threatening presentation of celiac disease that manifests as profuse diarrhea, hypoproteinemia, and severe metabolic disturbances. It may be precipitated by a general immune stimulus such as surgery, infection, or pregnancy. We report the case of a 26-year-old woman who presented with a celiac crisis, potentially triggered by a preceding urinary tract infection. Metabolic derangement is caused by malabsorption and profuse diarrhea, which can be unremitting unless the celiac crisis is recognized, and treatment with gluten restriction is initiated.
Keywords: Urinary tract infection, Celiac crisis, Celiac disease, Diarrhea
Introduction
Celiac disease (CD) is a chronic, small intestinal, immune-mediated enteropathy that is precipitated by dietary gluten in genetically predisposed individuals. In most adult cases, even untreated CD has an indolent course with gastrointestinal symptoms and nutritional abnormalities. Like childhood CD, many adults with CD present with diarrhea, steatorrhea, bloating, flatulence, and weight loss. However, CD can rarely present as an acute, life-threatening syndrome referred to as a celiac crisis, manifested by profuse diarrhea, hypoproteinemia, and severe metabolic disturbances significant enough to require hospitalization [1, 2]. The term “celiac crisis” was first used in 1953 by Andersen and Di Sant'Agnese when reporting a case series of 35 children with acute diarrheal illness attributed to a celiac crisis [3, 4]. In this series, a case fatality rate of 9% was reported. A celiac crisis is associated with a high morbidity [5] which makes an immediate identification and treatment imperative. As celiac crisis is not well documented, it remains a frequently underrecognized entity and is rarely considered in adults presenting with acute severe diarrheal illness, even after the exclusion of infectious etiologies. A celiac crisis is often precipitated by a general immune stimulus such as surgery, trauma, infection, or pregnancy [6, 7, 8]. It is unclear whether a celiac crisis in adults heralds the onset of CD or is an acute manifestation of previously undiagnosed CD. The initiation of a gluten-free diet (GFD) and parenteral fluid, along with nutritional support, and in most cases corticosteroids, remains the mainstays in the treatment of a celiac crisis. We report the case of a 26-year-old woman who presented with severe, acute, and unremitting diarrheal illness. After excluding common etiologies, she was diagnosed with CD presenting as celiac crisis.
Case Presentation
A 26-year-old Caucasian woman presented to the emergency department with a 3-week history of nausea, vomiting, anorexia, and diarrhea. She reported 6–12 daily episodes of watery brown stools, associated nausea, and multiple episodes of non-bloody and non-bilious emesis. She had not been travelling recently, has had no sick contacts, or hospitalization. She had been treated for uncomplicated urinary tract infection (UTI) with 3 days of levofloxacin, 3 days prior to the onset of her current symptoms. Her vital signs revealed a blood pressure of 98/68 mm Hg, a heart rate of 102 beats/min, a respiratory rate of 18/min, and a temperature of 36.4°C. On examination, she appeared dehydrated with a dry oral mucosa and decreased skin turgor. Notable lab abnormalities included a potassium level of 2.0 mEq/L, a bicarbonate level of 10 mmol/L, a WBC of 12.6 ×109/L, a hemoglobin level of 15.8 g/dL, and an albumin level of 1.6 g/dL. Her liver function tests were significant for ALT (113 U/L) and AST (126 U/L). Serum lactate, stool Clostridium difficile PCR and ova, parasites, and cultures were all negative. A CT of the abdomen showed diffusely edematous colonic mucosa.
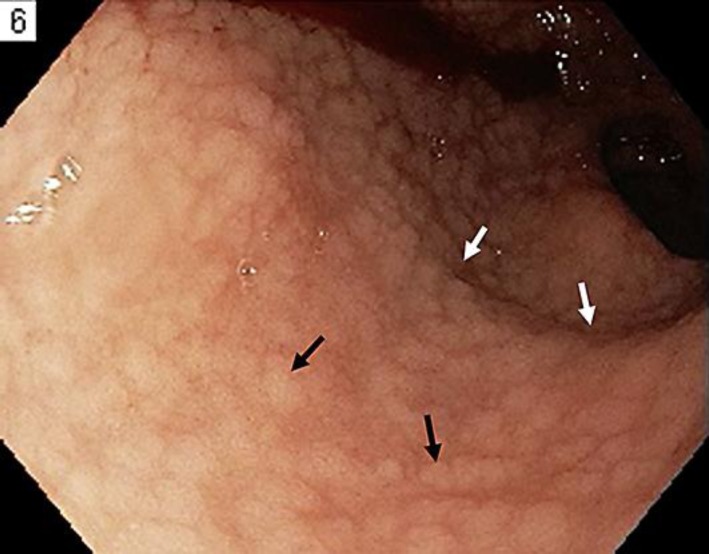
She was volume resuscitated with intravenous (IV) normal saline along with electrolyte replacement. She was also started on empiric antibiotics with IV ciprofloxacin and metronidazole. However, her diarrhea did not resolve in the next few days. After having completed the initial work-up, the tissue transglutaminase (tTG) antibody level was obtained which returned to be strongly positive (>100 U, normal 4–10 U). Esophagogastroduodenoscopy was then preformed, which revealed nodular duodenal mucosa with scalloping of the duodenal folds (Fig. 1). A duodenal mucosal histology revealed total villous atrophy, crypt hyperplasia, and marked epithelial lymphocytosis confirming the diagnosis of CD.
Fig. 1.
Duodenum showing nodular mucosa (black arrows) with scalloping of the folds (white arrows).
Her current diarrheal illness was attributed to a celiac crisis, and she was started on a GFD and oral budesonide. Total parenteral nutrition was also initiated to supplement nutrition. Within a few days, her diarrhea resolved, and she was discharged home on a GFD and a tapering dose of steroid.
Discussion
Although the term “celiac crisis” has been used since the 1950s to describe the acute, fulminant form of CD, only a handful of cases exist in the literature. It is a life-threatening syndrome seen mostly in children and rarely in adults with untreated CD. Clinically, it is characterized by profuse diarrhea that leads to severe dehydration, metabolic disturbances, renal dysfunction, and, in some instances, hemodynamic instability. Metabolic derangement includes hypokalemia, hyponatremia, hypocalcemia, hypomagnesemia, and hypoproteinemia.
There are no widely accepted, standardized, diagnostic criteria for a celiac crisis; however, Jamma et al. [9] proposed the following criteria to diagnose a celiac crisis in adults:
An acute onset or rapid progression of gastrointestinal symptoms attributable to CD requiring hospitalization and/or parenteral nutrition along with at least 2 of the following:
Signs of severe dehydration – hemodynamic instability or orthostatic hypotension;
Neurologic dysfunction;
Renal dysfunction;
Metabolic acidosis defined as a pH value <7.35;
Albumin <30 g/L;
Abnormal electrolyte levels including: hyper-/hyponatremia, hypocalcemia, hypokalemia, or hypomagnesemia; and
Weight loss >4.5 kg.
Our patient was hemodynamically instable, had metabolic acidosis, hypoalbuminemia, and abnormal electrolyte levels. Although these criteria are helpful for the diagnosis of a celiac crisis in patients with CD, the real challenge lies in diagnosing a celiac crisis in patients without a prior diagnosis of CD.
Although it is still unclear what triggers this crisis in few individuals with CD, it is likely due to the combination of severe mucosal inflammation and immune activation. A celiac crisis is usually precipitated by a general immune stimulus such as surgery, trauma, infection, or pregnancy [6, 7, 8]. Although it is difficult to demonstrate any causality, we postulate that our patient's preceding UTI likely precipitated her celiac crisis, in the setting of a previously undiagnosed CD. Also, the possibility of a viral entero-colitis triggering a celiac crisis cannot be excluded, given the evidence of diffusely edematous colonic mucosa on the CT scan. As exemplified in our case, the celiac crisis may be the very first manifestation of CD [9]. Jamma et al. [9] in a case series of 12 adults with celiac crisis reported that all 11 patients, in whom initial labs were available, had either high titer IgA tTG or IgA deficiency, suggesting that standard diagnostic testing is adequate for an initial evaluation of a celiac crisis in acutely ill individuals. Esophagogastroduodenoscopy with small intestine biopsy revealed marked villous atrophy in all cases [9]. Therefore, all patients suspected to have a celiac crisis should be tested for celiac antibodies, and should then receive esophagogastroduodenoscopy to obtain a tissue diagnosis.
The treatment of a celiac crisis involves the admission of IV hydration, electrolyte repletion, and the institution of a GFD. Jamma et al. [9] in their case series reported that about 50% of the patients improved with these interventions alone, while others required a short course of prednisone or budesonide. Therefore, depending upon the severity, a short course of glucocorticoids may be tried until the GFD takes effect.
In conclusion, even a simple UTI can acutely trigger an immune reaction causing a celiac crisis in predisposed individuals. A celiac crisis can be an acute manifestation of even previously undiagnosed CD. After having ruled out common etiologies, all patients with acute unremitting diarrhea should be evaluated for celiac antibodies. Any patient with elevated IgA tTG in this setting should be placed on a GFD and small intestinal biopsy performed as soon as possible.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
All authors have no financial disclosures. No conflict of interest exists.
References
- 1.Mones RL, Atienza KV, Youssef NN, Verga B, Mercer GO, Rosh JR. Celiac crisis in the modern era. J Pediatr Gastroenterol Nutr. 2007;45:480–483. doi: 10.1097/MPG.0b013e318032c8e7. [DOI] [PubMed] [Google Scholar]
- 2.Fasano A, Catassi C. Current approaches to diagnosis and treatment of celiac disease: an evolving spectrum. Gastroenterology. 2001;120:636–651. doi: 10.1053/gast.2001.22123. [DOI] [PubMed] [Google Scholar]
- 3.Ozaslan E, Koseoglu T, Kayhan B. Coeliac crisis in adults: report of two cases. Eur J Emerg Med. 2004;11:363–365. doi: 10.1097/00063110-200412000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Bai J, Moran C, Martinez C, Niveloni S, Crosetti E, Sambuelli A, Boerr L. Celiac sprue after surgery of the upper gastrointestinal tract. Report of 10 patients with special attention to diagnosis, clinical behavior, and follow-up. J Clin Gastroenterol. 1991;13:521–524. doi: 10.1097/00004836-199110000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Malnick SD, Atali M, Lurie Y, Fraser G, Geltner D. Celiac sprue presenting during the puerperium: a report of three cases and a review of the literature. J Clin Gastroenterol. 1998;26:164–166. doi: 10.1097/00004836-199804000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Smecuol E, Maurino E, Vazquez H, Pedreira S, Niveloni S, Mazure R, Boerr L, Bai JC. Gynaecological and obstetric disorders in coeliac disease: frequent clinical onset during pregnancy or the puerperium. Eur J Gastroenterol Hepatol. 1996;8:63–89. doi: 10.1097/00042737-199601000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Andersen DH, Di Sant'Agnese PA. Idiopathic celiac disease. I. Mode of onset and diagnosis. Pediatrics. 1953;11:207–223. [PubMed] [Google Scholar]
- 8.Di Sant'Agnese PA. Idiopathic celiac disease. II. Course and prognosis. Pediatrics. 1953;11:224–237. [PubMed] [Google Scholar]
- 9.Jamma S, Rubio-Tapia A, Kelly CP, Murray J, Najarian R, Sheth S, Schuppan D, Dennis M, Leffler DA. Celiac crisis is a rare but serious complication of celiac disease in adults. Clin Gastroenterol Hepatol. 2010;8:587–590. doi: 10.1016/j.cgh.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]