Abstract
Aim
Diagnostic evaluation practices for suspected coronary artery disease (CAD) may vary between countries. Our objective was to compare a CT-derived fractional flow reserve (FFRCT) diagnostic strategy with usual care in patients with planned invasive coronary angiography (ICA) enrolled in the PLATFORM (Prospective Longitudinal Trial of FFRCT: Outcome and Resource Impacts) study at German sites.
Methods
Patients were divided into two consecutive observational cohorts, receiving either usual care or CT angiography (CTA)/FFRCT. The primary endpoint was the percentage of patients planned for ICA, with no obstructive CAD on ICA within 90 days. Secondary endpoints included death, myocardial infarction, unstable angina, hospitalisation leading to unplanned revascularisation, cumulative radiation exposure, estimated medical costs and quality of life (QOL) at 1 year.
Results
116 patients were included. The primary endpoint occurred in 4 of the 52 patients (7.7%) in the CTA/FFRCT group and in 55 of the 64 patients (85.9%) in the usual care group (risk difference 78.2%, 95% CI 67.1% to 89.4%, p<0.001). ICA was cancelled in 40 of the 52 patients (77%) who underwent CTA/FFRCT. Clinical event rates were low overall. The mean radiation exposure was lower in the FFRCT versus the usual care group (7.28 vs 9.80 mSv, p<0.001). Mean estimated medical costs were €4217 (CTA/FFRCT) versus €6894 (usual care), p<0.001. Improvement in QOL (EQ-5D score) was greater in the FFRCT (+0.09 units) versus the usual care cohort (+0.03 units), p=0.04.
Conclusions
In patients with suspected CAD planned for ICA at German sites, initial CTA/FFRCT compared with usual care was associated with a markedly reduced rate of ICA showing no obstructive CAD, lower cumulative radiation exposure and estimated costs and greater improvement in QOL.
Keywords: CT angiography, CT-derived fractional flow reserve (FFRCT), non-invasive chest pain evaluation, stable chest pain
Key questions.
What is already known about this subject?
Although CT angiography (CTA) reduces the rate of invasive coronary angiography (ICA) showing no obstructive coronary artery disease (CAD) compared with functional testing, the rate remains significant with this approach. The observational PLATFORM (Prospective Longitudinal Trial of FFRCT: Outcome and Resource Impacts) study showed that in patients with suspected CAD, substitution of an initial invasive strategy with CTA, in addition to CT-derived fractional flow reserve (FFRCT) if abnormal, was associated with a high rate of cancellation of ICA, thereby reducing the proportion of ICA showing no obstructive CAD, with no increase in adverse clinical outcomes.
What does this study add?
This study showed that in the subgroup of patients enrolled in the PLATFORM study in Germany, where the rate of ICA is higher compared with other European countries or the USA, a greater proportion of patients in the CTA/FFRCT group had their ICA cancelled, resulting in a lower proportion of ICA showing no obstructive CAD compared with the main study.
How might this impact on clinical practice?
This report suggests that in healthcare systems with higher rates of ICA, the absolute benefit of an initial CTA/FFRCT strategy over an initial invasive strategy for investigation of suspected stable CAD may be more pronounced.
Introduction
Stable chest pain is a common clinical presentation, often warranting further evaluation by non-invasive or invasive means.1 A considerable proportion of patients require invasive coronary angiography (ICA) for definitive assessment, which has inherent risks and economic costs. Coronary CT angiography (CTA) may improve the efficiency of triage to ICA and potentially reduce radiation exposure.2 However, this may come at a price of increased rates of coronary angiography and revascularisation compared with a strategy of non-invasive testing.3
CTA is limited by the provision of an exclusively anatomical assessment of the coronary vasculature. CT-derived fractional flow reserve (FFRCT) may address this shortcoming by providing functional information obtained by non-invasive means in addition to the anatomical information provided by coronary CTA.4 Indeed, a number of trials have validated its use against invasive FFR.5–7 The PLATFORM (Prospective Longitudinal Trial of FFRCT: Outcome and Resource Impacts) study, which enrolled patients at 11 centres across 6 European countries, showed that coronary CTA/FFRCT, when used as an alternative initial diagnostic strategy in patients planned for invasive catheterisation, was associated with a significantly lower rate of angiography showing no obstructive coronary artery disease (CAD) within 90 days,2 with no difference in clinical outcomes or quality of life (QOL) at 1 year.8 Furthermore, a resource use and cost analysis performed at 90 days and 1 year showed that an FFRCT strategy was associated with reduced resource use and lower cost than an initial invasive strategy.8 9
In patients with suspected CAD, diagnostic evaluation practices may differ from country to country. Specifically, in the German healthcare system, a higher rate of coronary angiography is observed in comparison with other European countries or the USA.10–12 Moreover, it has been suggested that the associated healthcare costs and reimbursement models may favour a more invasive approach to the evaluation of chest pain.10 Against this background, the aim of this study is to compare an initial CTA/FFRCT versus an ICA strategy in patients enrolled in the PLATFORM study at German sites, who were planned for ICA for investigation of chest pain, in terms of clinical efficacy and safety, resource use, cost and QOL.
Methods
Study population and study protocol
PLATFORM is an observational, prospective, consecutive cohort, comparative effectiveness study (ClinicalTrials.gov number NCT01943903). Full details of the study population, methods, endpoints and primary analysis have been previously reported.2 In the main study, symptomatic outpatients ≥18 yearS of age without known CAD but with an intermediate likelihood of obstructive CAD, whose physician had planned either non-invasive tests or ICA to investigate suspected CAD were enrolled between September 2013 and November 2014. In this study, we report only the results in the group planned for ICA in the German subgroup (see online supplementary figure 1). Exclusion criteria included (1) acute coronary syndrome or clinical instability, (2) previously documented CAD, (3) contraindications for CTA or FFRCT, (4) need for urgent or emergent procedure or (5) ICA within 90 days before enrolment.
openhrt-2016-000526supp001.pdf (296.1KB, pdf)
In patients with planned ICA, there were two prospective cohorts with consecutive enrolment, meaning that enrolment in the second cohort commenced only after completion of enrolment in the first. Patients in the first cohort received the usual invasive care testing already planned by the treating physician. In the second, patients received an initial CTA in lieu of the planned invasive testing, followed by FFRCT analysis when requested by the treating site (advised if the CTA revealed ≥30% coronary stenosis). Non-invasive and invasive diagnostic testing (including CTA) was performed and interpreted on-site. All CTAs used a ≥64-slice multidetector, single-source or dual-source CT scanner and followed scanning protocols satisfying quality standards of the Society of Cardiac Computed Tomography.13 Quantitative coronary angiography (QCA) and FFRCT measurements were performed by independent core laboratories. QCA measurements were performed using QAngio software (Medis, The Netherlands) according to standard procedures.14 15 FFRCT analysis was performed centrally by HeartFlow (Redwood City, California, USA), as previously described.5–7 16 In brief, three-dimensional blood flow simulations in the coronary arteries were performed using proprietary software with quantitative image quality analysis, image segmentation and physiological modelling using computational fluid dynamics. Coronary blood flow was simulated under conditions that modelled intravenous adenosine to mirror pressure and flow data and the FFR numeric values obtained during ICA.2 The lowest FFRCT numeric value in each coronary artery and colour-scale representations of the coronary vasculature showing FFRCT values in vessels >1.8 mm in diameter were provided to clinical sites. Local clinicians made all subsequent decisions regarding clinical management, following standard practice, including whether to alter management based on FFRCT results. Optimal medical therapy was encouraged in both groups. This report includes rates of occurrence of the primary endpoint at 90 days, in addition to all final 1-year clinical, safety, QOL and economic results (using German cost weights) for the German subgroup. Ethical approval was obtained from local institutional review boards at each enrolling centre, and all patients provided written consent. The study was conducted in accordance with the Declaration of Helsinki.
Endpoints and definitions
The primary endpoint was the rate of ICA at ≤ 90days showing no obstructive CAD in patients with invasive testing planned before enrolment in the usual invasive care cohort versus the initial CTA/FFRCT cohort. Obstructive CAD was defined as stenosis of ≥50% in any coronary artery in a vessel ≥2.0 mm in diameter by core laboratory QCA or invasive FFR <0.80 in the absence of this degree of stenosis. Secondary endpoints included clinical, economic and QOL outcomes at 1 year. The clinical secondary endpoints included the following: (1) a composite of major cardiovascular events (MACE) at 1 year, including all-cause mortality, myocardial infarction (MI) and unplanned hospitalisation for chest pain leading to urgent revascularisation and (2) MACE plus vascular events within 14 days of procedures. MACE were adjudicated by an event adjudication committee blinded to the treatment groups based on standard, prospectively determined definitions.17 Cumulative radiation exposure from all cardiovascular tests and procedures was determined over 1 year after enrolment, as previously described.2
The use of key medical resources, including non-invasive stress tests, CTA, invasive tests, coronary revascularisation procedures and clinical events, was demonstrated from study enrolment through 1 year. Cumulative medical costs (in euro) over 1 year were calculated on a per-patient basis by multiplying a standardised cost weight for each resource by the number of times that resource was used. Cost data were obtained using reimbursement rates for privately insured patients from the 2016 German doctor’s fee schedule (GOÄ) for outpatient examinations and the 2016 German Diagnosis-Related Groups (G-DRG) system for inpatient investigations. The G-DRG system operates on a flat-fee principle based on the final documented diagnosis on discharge, taking into account factors such as comorbidities and length of stay. GOÄ reimbursement, on the other hand, operates on a fee-for-service basis for privately insured patients. When calculating the difference in subsequent costs between patients with the FFRCT strategy versus the conventional strategy, the FFRCT cost weight was set at zero, as there is no G-DRG or GOÄ cost weight at this time. QOL was assessed at baseline and one year using the Seattle Angina Questionnaire (SAQ), the EuroQOL scale (EQ-5D) and the EuroQOL visual analogue scale, and the magnitude of change was compared between patients in the usual invasive care cohort versus the initial CTA/FFRCT cohort.
Follow-up and analysis
Patients were followed up by clinic visit at 90 days, 6 months and 1 year from enrolment. Data were analysed at 90 days and 1 year. The country of enrolment was a prespecified subgroup in the PLATFORM study.
Statistical analysis
Baseline characteristics were summarised and compared across usual care and CTA/FFRCT-guided care cohorts. Continuous data are presented as mean ± SD and were compared using Student’s t-test or the Wilcoxon rank-sum test. Categorical variables are presented as counts (percentages) and were compared using the Pearson χ2 test or Fisher’s exact test, where the expected cell value was <5. The level of statistical significance was set to 0.0025 using the Bonferroni correction to adjust for multiple comparisons.
Endpoints were compared between the FFRCT-guided and usual care management strategies. All analyses were performed on an intention-to-treat basis. The risk difference and 95% CI were determined, and a one-sided Wald test (α error=0.025) for a risk difference <0 evaluated whether CTA/FFRCT was superior compared with usual testing. Analysis of the secondary endpoints at 1 year was determined in both cohorts. Cumulative radiation exposure was compared between groups using Student’s t-test and the Wilcoxon rank-sum test and is presented as mean±SD and median (IQR). For economic analyses, unadjusted costs were compared between strategies using the non-parametric Wilcoxon rank-sum test on all patients and in the propensity-matched cohorts. A 95% CI for the difference in mean per-patient cost between usual care and FFRCT-guided care cohorts was determined using empirical bootstrap resampling with 100 000 replicates. The Wilcoxon signed-rank test was used to analyse changes in QOL scores from baseline to 1 year of follow-up for the entire cohort, and the Wilcoxon rank-sum test was used to compare QOL changes between groups. Changes in medication use from baseline to 1 year of follow-up were compared between groups using logistic regression fit using generalised estimating equations. There were no specific methods employed to account for missing data or loss to follow-up. All statistical assessments were performed by statisticians at HeartFlow, and analyses were performed using SAS version 9.3 (Cary, North Carolina, USA). A p value <0.05 was considered statistically significant, unless otherwise specified.
Results
Patients
Between September 2013 and November 2014, 116 patients who were planned for ICA were enroled at the three participating German sites ; 64 patients were allocated to usual care, and 52 patients were allocated to CTA/FFRCT. Pre-enrolment non-invasive testing had been done in 16 of the 52 patients in the CTA/FFRCT and 41 of the 64 patients in the usual care group (p<0.001). Complete follow-up data at 1 year was available for all but 5 patients in each group. A patient study flow chart is shown in online supplementary figure 1.
Baseline demographics and clinical characteristics are shown in table 1. Compared with the FFRCT cohort, patients in the usual care cohort were older, had a higher incidence of diabetes and had a higher pretest probability of obstructive CAD than the CTA/FFRCT cohort.
Table 1.
Baseline characteristics of study participants
| Variable |
Planned invasive test
(n=116) |
||
|
Usual care strategy
(n=64) |
FFRCT-guided strategy
(n=52) |
p Value | |
| Demographics | |||
| Age, years | 63.6±11.6 | 55.3±10.2 | <0.001 |
| Female sex | 25 (39.1) | 24 (46.2) | 0.41 |
| Racial/ethnic minority (self-reported) | 1 (1.6) | 1 (1.9) | |
| Cardiac risk factors | |||
| Hypertension | 45 (70.3) | 28 (53.8) | 0.07 |
| Diabetes | 12 (18.8) | 3 (5.8) | 0.04 |
| Dyslipidaemia | 15 (23.4) | 10 (19.2) | 0.58 |
| Current or past tobacco use | 33 (51.6) | 26 (50.0) | 0.51 |
| Pretest probability of obstructive CAD* | 54.5±17.1 | 44.6±16.1 | 0.002 |
| Anginal type | 0.22 | ||
| Typical angina | 19 (29.7) | 17 (32.7) | |
| Atypical angina | 42 (65.6) | 35 (67.3) | |
| Non-cardiac chest pain | 3 (4.7) | 0 (0.0) | |
Data shown as mean±SD or number (percentage). *Pretest probability of obstructive CAD±SD calculated by the updated Diamond and Forrester score.18
CAD, coronary artery disease; FFRCT, fractional flow reserve estimated using CT.
By study design, all patients in the CTA/FFRCT group underwent CTA. FFRCT analysis of CTA images was indicated in 30 cases (57.7%), 25 of which were suitable for same. ICA was performed in 100% of patients in the usual care cohort and in 12 patients (23.1%) in the CTA/FFRCT cohort, with the remainder of invasive tests being cancelled by the treating physician based on the CTA/FFRCT result (see online supplementary figure 1).
A 90-day coronary revascularisation was performed in 22 patients (19.0%) in total: 14 patients (21.9%) in the usual care cohort and 8 patients (15.4%) in the FFRCT cohort. Between 90 days and 1 year, no patient in either cohort had a new unplanned revascularisation, while 1 patient (1.6%) in the usual care cohort had a repeat revascularisation procedure. Medications at 1 year of follow-up did not differ significantly between the CTA/FFRCT and usual care groups: aspirin (25/47 (53%) vs 36/59 (61%), p=0.42), clopidogrel (7/47 (15%) vs 6/59 (10%), p=0.46) and any statin (21/47 (45%) vs 35/59 (59%), p=0.13).
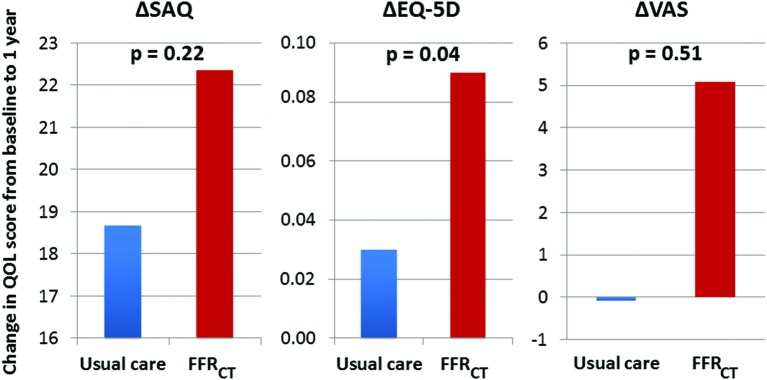
Primary endpoint
The primary endpoint of ICA showing no obstructive CAD at 90 days occurred in 55 of the 64 (85.9%) patients in the usual care group compared with only 4 of the 52 (7.7%) patients in the CTA/FFRCT group (risk difference 78.2%, 95% CI 67.1 to 89.4, p<0.001, as shown in figure 1).
Figure 1.
Rates of occurrence of the primary endpoint by evaluation strategy. The primary endpoint occurred in 85.9% and 7.7% of patients in the usual care and FFRCT cohorts, respectively (risk difference 78.2%, 95% CI 67.1-89.4, p<0.001). 76.9% of patients in the FFRCT cohort had their ICA cancelled on the basis of their CTA/FFRCT result. CAD=coronary artery disease; FFRCT=fractional flow reserve estimated using computed tomography; ICA=invasive coronary angiography; Obst CAD=obstructive coronary artery disease.
Clinical efficacy and safety outcomes at 1 year
There were no cases of MACE at 1 year in either group. No patients in the CTA/FFRCT group versus two patients (3.1%) in the usual care group had vascular complications, both related to ICA (risk difference 3.1%, 95% CI −12.29 to 18.44).
There were no adverse clinical events at 1-year follow-up in any of the 40 patients who had their ICA cancelled on the basis of their CTA/FFRCT result; 2 (5.0%) of these patients required an initial ICA during 1-year follow-up, both of which were performed because of a subsequent clinical presentation with chest pain and both showing no obstructive CAD.
Cumulative radiation exposure at 1 year was significantly lower in the FFRCT cohort compared with the usual care cohort, with mean values of 7.28±9.33 versus 9.80±6.73 mSv and median values of 3.68 (IQR 1.69–8.73) versus 7.00 (IQR 7.00–7.00) mSv, respectively (p<0.001). One-year clinical outcomes are shown in table 2.
Table 2.
One-year clinical outcomes according to study group
|
Planned invasive test
n= 116 |
|||
|
Usual care strategy
n=64 |
FFRCT-guided strategy
n=52 |
p Value | |
| Invasive catheterisation without obstructive CAD by core lab QCA (at 90 days) | |||
| Number of patients (%) | 55 (85.9) | 4 (7.7) | <0.001 |
| Risk difference, % (CI) | 78.2 (67.1 to 89.4) | ||
| MACE | |||
| No of patients (%) | 0 (0) | 0 (0) | |
| MACE or vascular complications | 2 (3.1) CI 0.38 to 10.84 |
0 (0) CI 0.00 to 6.85 |
NS |
| Risk difference, % (CI) | 3.1 (–12.29 to 18.44) | ||
| Cumulative radiation exposure | <0.001 | ||
| Mean±SD, mSv | 9.80 (6.73) | 7.28 (9.33) | |
| Median (IQR), mSv | 7.00 (7.00, 7.00) |
3.68 (1.69, 8.73) |
|
CAD, coronary artery disease; FFRCT, fractional flow reserve estimated using CT; MACE, major adverse cardiovascular events; MI, myocardial infarction; NS, non-significant; QCA, quantitative coronary angiography.
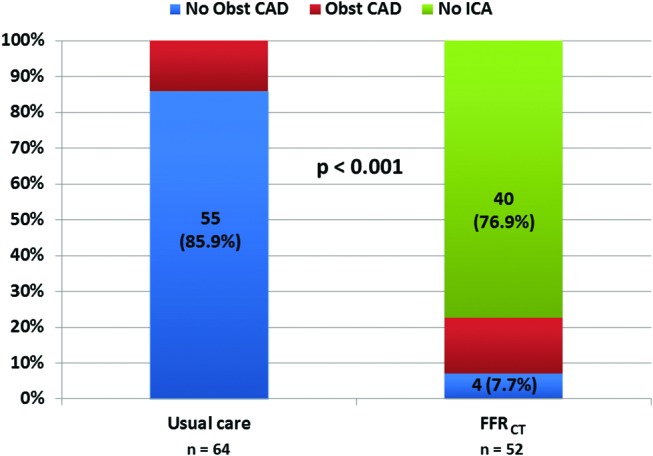
Resource use and economic outcomes at 1 year
Resource use over 1 year is shown in table 3, and cost weights are shown in online supplementary table 1. As there is currently no cost weight available for FFRCT, we set the cost weight at the cost of CTA plus zero for the initial estimate. The mean 1-year patient cost of cumulative medical care was significantly lower in the FFRCT group, at €4217±€9740 compared with €6894±€7379 in the usual care group (p<0.001). In addition, more patients in the FFRCT group had low costs than in the usual care group, with median costs of €465 (IQR €2930) versus €5243 (IQR €4326), respectively (p<0.001). Cumulative medical costs are shown in figure 2. In a sensitivity analysis, we recalculated the 1-year costs using a series of cost weights that were multiples of the cost weight for CTA and compared these costs with the costs of a usual care strategy. A cost benefit for CTA/FFRCT over usual care was maintained up to the value of 14 times the cost of CTA, at €6894 versus €6506, respectively, p=0.02.
Table 3.
Resource use over 12 months
|
Planned invasive test
n=116 |
||
|
Usual care strategy
n=64 |
FFRCT-guided strategy
n=52 |
|
| Non-invasive tests | ||
| Stress ECG | 6 | 12 |
| Stress echo | 3 | 2 |
| Stress nuclear | 1 | 0 |
| MRI | 2 | 0 |
| CTA | 1 | 52 |
| FFRCT | 0 | 25 |
| Invasive procedures | ||
| Diagnostic ICA | 61 | 9 |
| ICA with PCI | 11 | 10 |
| FFRINV | 2 | 1 |
| Intravascular ultrasound | 0 | 0 |
| Optical coherence tomography | 1 | 0 |
| Coronary revascularisation | ||
| Percutaneous intervention | 12 | 10 |
| Stents per patient (mean) | 2.1 | 1.6 |
| Bypass surgery | 4 | 1 |
| Hospital days | 122 | 65 |
| Clinic visits | 20 | 19 |
Data shown as number of times used.
CTA, CT angiography; FFRCT, fractional flow reserve estimated using CT; FFRINV, fractional flow reserve determined by ICA; ICA, invasive coronary angiography; PCI, percutaneous coronary intervention.
Figure 2.
One-year costs by evaluation strategy. Box plot showing median and interquartile range of cumulative 1-year medical costs calculated on a per patient basis according to treatment strategy when CTA/FFRCT is given the same cost weight as CTA alone. The vertical axis indicates cumulative medical costs at one year. The top line of each box indicates the 75th percentile, the dashed line within each box indicates the 50th percentile (median) and the line at the bottom of each box represents the 25th percentile. The triangles represent mean costs. Both median and mean costs were significantly lower in the CTA/FFRCT cohort compared with the usual care cohort. CTA=computed tomography angiography; ICA=invasive coronary angiography; FFRCT=fractional flow reserve estimated using computed tomography.
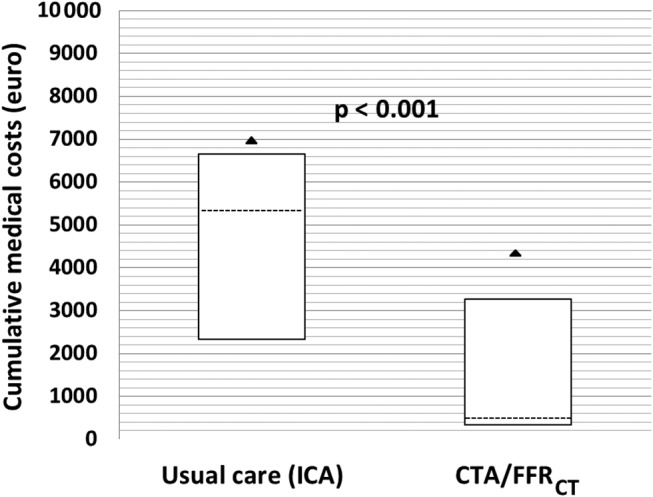
QOL outcomes at 1 year
Functional status and QOL scores improved from baseline to 1-year follow-up to a greater degree in the FFRCT cohort compared with the usual care cohort, regardless of the score used. This difference was statistically significant when the EQ-5D score was used. Respective mean improvements using all three scores were as follows: +18.68 and +22.36 units on the SAQ (p=0.22); +0.03 versus +0.09 units on the EQ-5D (p=0.04) and -0.07 versus +5.09 units on the Visual Analogue Scale (p=0.51). Changes in QOL scores are demonstrated in figure 3.
Figure 3.
Change in quality-of-life scores from baseline to 1 year by evaluation strategy. The vertical axes indicate changes in quality of life scores from baseline to 1 year, with a greater improvement seen in the FFRCT cohort compared with the usual care cohort, regardless of the score used. This difference was statistically significant when the EQ-5D score was used. FFRCT=fractional flow reserve estimated using computed tomography, SAQ=Seattle Angina Questionnaire, EQ-5D=EuroQOL, VAS=visual analogue scale for health state.
Discussion
The main finding of our analysis was that in patients with a planned invasive strategy for investigation of suspected CAD enrolled in a consecutive cohort study at German sites, a CTA/FFRCT strategy was associated with a significantly lower rate of ICA showing no obstructive CAD compared with those who received usual care. Moreover, an initial CTA±FFRCT strategy was associated with a high rate of cancellation of ICA. Furthermore, CTA/FFRCT was associated with significantly lower cumulative radiation exposure, significantly lower medical resource use and cost and greater improvement in QOL at 1-year follow-up.
One of the limitations of the use of CTA in routine practice is that it has low specificity for obstructive CAD and may increase the rate of referral for ICA. The PLATFORM study data suggest that by using CTA, with FFRCT as required, due to the known higher specificity for obstructive CAD, this issue might be addressed in a clinically relevant way.7 19
It is well recognised that in patients presenting with chest pain with intermediate risk of obstructive CAD, considerable variation exists in relation to diagnostic practices. In particular, in Germany, the rate of ICA is higher than in other European countries or in the USA.10 However, the ratio of revascularisation (both percutaneous and surgical) to ICA is lower in Germany,10 which would imply that a higher proportion of ICA performed shows no obstructive CAD. Against this background, the analysis of outcomes of patients enroled in the PLATFORM study at German sites might be expected to be of particular interest.
In terms of the primary endpoint, the findings of this report are generally consistent with those of the main PLATFORM study, although the benefits of an initial CTA/FFRCT strategy in patients planned for ICA may be even more pronounced in the setting of the German healthcare system. In this respect, the risk difference in the occurrence of the primary endpoint between the CTA/FFRCT group and the usual care group was greater than in the main PLATFORM study (78.2% vs 61.0%, respectively). This is a result of both a higher rate of occurrence of the primary endpoint in the usual care cohort in the German subgroup compared with the main study (86% vs 73%, respectively), which is to be expected given the higher rate of ICA in Germany, and a lower rate of occurrence of the primary endpoint in the FFRCT cohort in the German subgroup compared with the main study (8% vs 12%, respectively), which can be partly explained by a higher rate of cancellation of ICA based on the CTA/FFRCT result in this cohort in the German subgroup (77%) compared with the main study (61%). The rate of the primary endpoint in the usual care group as determined by core laboratory QCA was higher than the site-reported rate (86% vs 69%, respectively). However, this did not change the overall results and is consistent with known differences between the two assessment techniques.
It is also noteworthy that a lower proportion of patients who underwent CTA were referred for FFRCT analysis in the German subgroup than in the main study (57.7% vs 69.4%, respectively). This is likely because more patients with normal coronary arteries were filtered out by CTA alone, without the need for FFRCT analysis. This is supported by the fact that a higher proportion of ICA was cancelled in patients in the CTA cohort in the German subgroup compared with the main study, despite the lower rate of FFRCT analysis. In addition, there was no significant difference in rates of measurable CTA in those referred for FFRCT analysis between the German subgroup and the main study (83.3% vs 87.3%, respectively). Despite the use of a dedicated evaluation protocol, it is possible that a proportion of patients with obstructive CAD remain undetected. In this respect, in the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps), the addition of FFRCT to CTA alone, increased the specificity from 34% to 79% (compared with 83% with ICA). In addition, the sensitivity of this approach was 86% (compared with 64% for ICA).7
In terms of secondary endpoints, the absence of MACE among patients in the CTA/FFRCT group who had their ICA cancelled is important (and consistent with findings in the overall PLATFORM population), with only two of these patients undergoing ICA during 1-year follow-up, both showing no obstructive CAD. The finding of lower cumulative medical costs over 1 year in the CTA/FFRCT cohort compared with the usual care cohort is also consistent with findings from the main PLATFORM study. Furthermore, when German cost weights were used to calculate cumulative medical costs at 1 year for all patients enrolled in the main PLATFORM study, this effect persisted (mean costs of €5961 vs €8865 and median costs of €5271 vs €556, respectively, p<0.001).
In some respects, our findings are consistent with those from the randomised CONSERVE (Coronary computed tomographic angiography for selective cardiac catheterization: relation to cardiovascular outcomes, cost effectiveness and quality of life) trial, which also studied patients with an intermediate pretest probability of obstructive CAD, planned for ICA and compared outcomes between those who proceeded to ICA as planned (direct ICA) versus those who underwent initial CTA (without FFRCT) with ICA, if necessary (selective ICA). In that study, selective ICA did reduce the rate of ICA and revascularisation, as well as overall cost, although there was no difference in clinical adverse outcomes at 1 year. However, in contrast to PLATFORM, the investigational approach did not reduce the rate of ICA showing no obstructive CAD compared with direct ICA.20
Interestingly, cumulative radiation exposure at 1 year was significantly lower in the FFRCT cohort in the German subgroup, an effect not observed in the main PLATFORM study. While cumulative radiation dose in the usual care cohort was similar in the German substudy and the main study, it was much lower in the FFRCT cohort (mean radiation dose 7.28 vs 10.72 mSv and median 3.68 vs 7.94 mSv, respectively). Finally, the greater improvement in QOL in the FFRCT cohort in the German subgroup is consistent with the main study, although this was only statistically significant for the German subgroup. The reason for this greater degree of improvement in the FFRCT group is unclear and must be interpreted with caution due to the non-randomised, unblinded nature of the study and the risk of a type I error. However, it is possible that the avoidance of an invasive procedure, even if no further intervention was required, and the overall lower number of hospital days may have contributed to the observed differences.
Although there are randomised clinical trial data to support the role of CTA in the investigation of stable chest pain, some clinical trials have shown that CTA alone for the investigation of stable chest pain is associated with a higher rate of ICA showing no obstructive CAD and, potentially a higher rate of revascularisation in the absence of knowledge of lesion functional severity.19 21 While our study suggests some benefit from a CTA/FFRCT strategy in reducing rates of ICA showing no obstructive disease compared with routine CTA, it should be acknowledged that the design of this study does not permit direct assessment of the incremental benefit of CTA/FFRCT over CTA alone. Randomised data are needed to clarify this issue.
Limitations
This study has a number of important limitations that must be taken into account. First, group allocation was not randomised: patients in the FFRCT arm were significantly younger than those in the usual care arm, with a lower incidence of diabetes and lower pretest probability of obstructive CAD. This may have led to increased rates of cancellation of ICA and lower rates of FFRCT utilisation in the CTA/FFRCT group. Although this likely increased the difference in occurrence of the primary endpoint between treatment groups, it is unlikely to have changed the overall result. Second, the sample size was relatively small, and the study was not equipped to show a difference in clinical events, such as MACE. In addition, the number of clinical events occurring during follow-up was relatively low. Therefore, failure to detect a difference between groups does not reliably rule out a difference. Third, patients at intermediate risk of obstructive CAD were referred for ICA based on the judgement of the referring physician, as ICA was deemed to be appropriate, even though non-invasive testing was not performed in all patients. Although this approach may be considered according to current guidelines,1 the specific reasons as to why non-invasive testing was not undertaken were not analysed as part of the study protocol, and this limits the external validity of the findings. Finally, the cost weights used for outpatient tests in this study apply to reimbursement for investigations and procedures performed in privately insured patients. Therefore, the cost analysis is not generalisable to all patients within the German healthcare system.
Conclusion
In patients with stable chest pain planned for invasive coronary angiography at German sites, an initial CTA/FFRCT strategy compared with usual care was associated with a significantly lower rate of ICA showing no obstructive CAD. This strategy was also associated with lower cumulative radiation exposure, lower cost and improved quality of life, with no increase in adverse clinical events at 1-year follow-up.
Footnotes
Funding: RC reports support from the Irish Board for Training in Cardiovascular Medicine sponsored by MSD; PSD has received research grants from HeartFlow during the conduct of the study and other support from GE Medical systems outside the submitted work; MG reports speaker fees of Siemens, Philips, Bayer and Bracco; ; AW is an employee of HeartFlow; GP reports speakers fees from GE Healtchare, Bracco and Medtronic; MAH consults for the Blue Cross Blue Shield Association and received a research grant from HeartFlow during the conduct of the study; FW served as a consultant for HeartFlow during the conduct of the study and received financial compensation for these services; CR is an employee of HeartFlow and reports a salary and equity from HeartFlow; RAB reports receiving institutional research grants from Boston Scientific and HeartFlow and lecture fees from B. Braun Melsungen AG, Biotronik and Boston Scientific.
Competing interests: None declared
Provenance and peer review: Not commissioned; externally peer reviewed
Data sharing statement: No additional data are available
References
- 1.Windecker S, Kolh P, Alfonso F, et al. ; SCOT-HEART Investigators. ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;2014:2541–619. 10.1093/eurheartj/ehu278 [DOI] [PubMed] [Google Scholar]
- 2.Douglas PS, Pontone G, Hlatky MA, et al. ; PLATFORM Investigators. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J 2015;36:3359–67. 10.1093/eurheartj/ehv444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossi A, Dharampal A, de Feyter PJ. Coronary CT angiography for patients with suspected coronary artery disease. Heart 2014;100:976–84. 10.1136/heartjnl-2012-301949 [DOI] [PubMed] [Google Scholar]
- 4.Nørgaard BL, Jensen JM, Leipsic J. Fractional flow reserve derived from coronary CT angiography in stable coronary disease: a new standard in non-invasive testing? Eur Radiol 2015;25:2282–90. 10.1007/s00330-015-3619-1 [DOI] [PubMed] [Google Scholar]
- 5.Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 2011;58:1989–97. 10.1016/j.jacc.2011.06.066 [DOI] [PubMed] [Google Scholar]
- 6.Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 2012;308:1237–45. 10.1001/2012.jama.11274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nørgaard BL, Leipsic J, Gaur S, et al. ; NXT Trial Study Group. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 2014;63:1145–55. 10.1016/j.jacc.2013.11.043 [DOI] [PubMed] [Google Scholar]
- 8.Douglas PS, De Bruyne B, Pontone G, et al. ; PLATFORM Investigators. 1-Year outcomes of FFRCT-Guided care in patients with suspected coronary disease: The PLATFORM study. J Am Coll Cardiol 2016;68:435–45. 10.1016/j.jacc.2016.05.057 [DOI] [PubMed] [Google Scholar]
- 9.Hlatky MA, De Bruyne B, Pontone G, et al. ; PLATFORM Investigators. Quality-of-life and economic outcomes of assessing fractional flow reserve with computed tomography angiography: PLATFORM. J Am Coll Cardiol 2015;66:2315–23. 10.1016/j.jacc.2015.09.051 [DOI] [PubMed] [Google Scholar]
- 10.Flachskampf FA, von Erffa J, Seligmann C. Reimbursement and the practice of cardiology. J Am Coll Cardiol 2012;59:1561–5. 10.1016/j.jacc.2011.11.058 [DOI] [PubMed] [Google Scholar]
- 11.Meinertz T, Diegeler A, Stiller B, et al. German heart report 2013. Thorac Cardiovasc Surg 2015;63:112–23. 10.1007/s00392-014-0799-7 [DOI] [PubMed] [Google Scholar]
- 12.OECD Health Statistics 2015: Organisation for Economic Co-operation and Development. 2015. http://www.oecd.org/els/health-systems/health-data.htm
- 13.Leipsic J, Abbara S, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the society of cardiovascular computed tomography guidelines committee. J Cardiovasc Comput Tomogr 2014;8:342–58. 10.1016/j.jcct.2014.07.003 [DOI] [PubMed] [Google Scholar]
- 14.Tuinenburg JC, Janssen JP, Kooistra R, et al. Clinical validation of the new T- and Y-shape models for the quantitative analysis of coronary bifurcations: an interobserver variability study. Catheter Cardiovasc Interv 2013;81:E225–36. 10.1002/ccd.24510 [DOI] [PubMed] [Google Scholar]
- 15.Reiber JH, Kooijman CJ, Slager CJ, et al. Coronary artery dimensions from cineangiograms methodology and validation of a computer-assisted analysis procedure. IEEE Trans Med Imaging 1984;3:131–41. 10.1109/TMI.1984.4307669 [DOI] [PubMed] [Google Scholar]
- 16.Taylor CA, Fonte TA, Min JK. Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: scientific basis. J Am Coll Cardiol 2013;61:2233–41. 10.1016/j.jacc.2012.11.083 [DOI] [PubMed] [Google Scholar]
- 17.Hicks KA, Tcheng JE, Bozkurt B, et al. ACC/AHA Key Data Elements and Definitions for Cardiovascular Endpoint Events in Clinical Trials: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). J Am Coll Cardiol 2014;2015:403–69. 10.1161/CIR.0000000000000156 [DOI] [PubMed] [Google Scholar]
- 18.Genders TS, Steyerberg EW, Alkadhi H, et al. ; CAD Consortium. A clinical prediction rule for the diagnosis of coronary artery disease: validation, updating, and extension. Eur Heart J 2011;32:1316–30. 10.1093/eurheartj/ehr014 [DOI] [PubMed] [Google Scholar]
- 19.Douglas PS, Hoffmann U, Patel MR, et al. ; PROMISE Investigators. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 2015;372:1291–300. 10.1056/NEJMoa1415516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan H-j. Coronary computed tomographic angiography for selective cardiac catheterization: relation to cardioVascular outcomes, cost effectiveness and quality of life (NCT01810198). Rome, Italy: European Society of Cardiology Congress, 2016. [DOI] [PubMed] [Google Scholar]
- 21.SCOT-HEART Investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet 2015;385:2383–91. 10.1016/S0140-6736(15)60291-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2016-000526supp001.pdf (296.1KB, pdf)