After the approval of safe and highly effective oral direct acting agents (DAA) for the treatment of hepatitis C virus (HCV) in 2014, commentaries and discussions about the elimination of hepatitis C on a population level have rapidly proliferated in scientific literature and popular press. Indeed, the World Health Organization (WHO) has announced proposed global targets of an 80% reduction in new cases of HCV infection from the 2010 level and several countries, including Australia, Egypt, Georgia and Iceland have embarked on ambitious plans to control HCV infection in their populations [1].
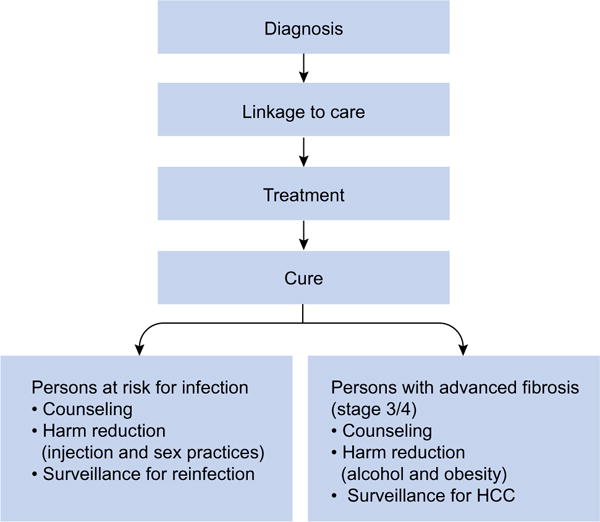
The launch of such programs has led to increased focus on the hepatitis C care continuum with particular emphasis on the identification of HCV-infected persons and linkage of such persons to HCV care and treatment to achieve HCV cure. Modeling data from multiple groups provide the basis for optimism and suggest that the crucial step in reducing the prevalence of HCV infection over a period of time is an increase in HCV treatment uptake in key populations [2,3]. In particular, persons living with HIV infection represent a population for whom HCV control has been prioritized due to the high prevalence of HCV infection and high burden of HCV-related morbidity and mortality. Further, ongoing global efforts to improve the HIV care continuum, linking HIV-infected persons to long-term antiretroviral therapy provide an ideal foundation on which to launch concerted efforts to eliminate HCV coinfection. As these programs take shape, it is important to recognize that the HIV and HCV care continuum are not identical. In the absence of HIV cure, patients must continue antiretroviral therapy indefinitely, whereas HCV treatment is finite and curative. However, in the absence of an effective HCV vaccine, persons cured of chronic HCV are at-risk for reinfection if exposed. Thus, the HCV care continuum does not end with cure; and the prevention of reinfection must be addressed in persons at-risk (Fig. 1). To date, relatively high rates of reinfection with hepatitis C following cure have been observed in two patient groups: People who inject drugs (PWID) and HIV-infected men who have sex with men (MSM) [4–7].
Fig. 1. Extended Hepatitis C care continuum.
Preserving the benefits of HCV cure.
The global incidence of HCV among HIV-infected MSM is estimated to be 0.53/100 person-years (PYs) [8]. Estimates of the incidence of reinfection are much higher at 9.6–15.2/100 PYs suggesting that there is a finite pool of HIV-infected MSM who require focused concerted effort for HCV control [4–6]. In this issue of the Journal of Hepatology, Ingiliz et al. present additional data highlighting the high rates of HCV reinfection among HIV-infected MSM from eight centers in Europe [9]. These men had either previously cleared HCV spontaneously or after successful treatment. They found a reinfection prevalence of 7.3 (95% CI 6.2–8.6)/100 PYs with a trend for a lower incidence of reinfection among men who had spontaneously cleared their incident infection than among individuals who were treated (Hazard ratio 0.62, 95% CI 0.38–1.02, p = 0.06). The strengths of this study include the large number of individuals studied (606 MSM) and the analysis of HCV reinfection among these individuals from eight centers in multiple countries (Austria, France, Germany and the UK). The authors were thus able to describe regional differences in HCV reinfection risk. However, what was most striking was the increase in reinfection incidence rates with each subsequent reinfection (HCV reinfection incidence 7.3/100 PY for the first reinfection and 18.8/100PY for the second reinfection). As described by the authors, this is suggestive of ongoing high risk behaviors in certain groups.
These high-risk behaviors such as unprotected, traumatic sex with concomitant illicit drug use and the more recent proliferation of chemsex (the use of drugs to increase sexual disinhibition and arousal) likely drive incident HCV infection and reinfection. Without behavior change, gains in population level HCV control from HCV treatment may be significantly compromised [10]. HCV treatment interventions will need to be combined with harm reduction and behavioral interventions to reduce rates of HCV reinfection to preserve reductions achieved in prevalent HCV infections at the population level. While every patient treated for HCV should receive counseling regarding the risk of and strategies to prevent HCV reinfection, it will be critical to identify factors associated with particularly high risk of reinfection in specific groups. This knowledge should guide design of effective combined behavioral and biomedical harm reduction and treatment interventions that specifically target these groups. For at-risk HIV-infected MSM, these interventions should focus on addressing the risks of disease transmission surrounding chemsex, unprotected anal intercourse and reinforce the need for condom use and avoidance of sex while using drugs. Similarly, at-risk PWID will require counseling on safer injection practices including the risk of HCV transmission with sharing of any drug use paraphernalia including cookers, cotton or water, access to clean needles and syringes, needle/syringe exchange programs and treatment for addiction including opioid agonist therapy.
Are there subgroups of HIV-infected MSM that are at highest risk of HCV infection and reinfection? The work carried out by Ingiliz et al. and others would suggest so [9,11,12]. A better understanding of predictors of HCV reinfection in high risk populations is urgently needed and will require improved surveillance for HCV reinfection in clinical practice and funding of research studies aimed at understanding the modes and mechanisms of HCV transmissions among these populations. In clinical practice, individuals with ongoing risk after HCV cure should receive at least annual HCV RNA testing with more frequent testing in some cases to assess for reinfection. Acute HCV infection also needs to be quickly diagnosed and treated as individuals at the highest risk of infection and reinfection are also those most likely to transmit HCV to others. Acute hepatitis C infection is most often asymptomatic; thus, clinicians need to be vigilant. For persons without prior HCV infection, hepatitis C antibody testing at regular intervals may be sufficient for HCV screening in an individual with ongoing risk factors for HCV infection. However, HCV re-screening may also be indicated in the context of self-reported high risk exposures and/or newly elevated alanine aminotransferase (ALT) levels. The sooner acute HCV infection is diagnosed, the sooner it can be addressed to reduce the risk of onward transmission to others.
As we continue to scale-up HCV treatment, careful thought and research must focus on the development of innovative treatment models for populations at-risk for repeated infections. One such model is that utilizing the concept of treating individuals such as PWID and their injecting networks or HIV-infected MSM and their sexual networks at the same time, popularly referred to as the “treat your friends” strategy [13]. This is analogous to the contact tracing methods that have been used for many decades by public health officials to control sexually transmitted diseases such as syphilis. Among PWID populations, modeling data supports the efficiency of this approach to reduce the prevalence of HCV among PWID in 15 short years [2]. Achieving this reduction in HCV prevalence through HCV treatment will however require combined effective harm reduction interventions and prompt treatment of any new infections introduced into the network to prevent onward transmission. HIV-infected MSM who are in routine HIV care with regular contact with the health care system would appear to be a population for which this treatment model might be effective.
The availability of all oral DAAs has opened an inspiring door of opportunity for HCV control at the population level. While oral DAAs are necessary to achieve these goals, treatment alone is not going to be sufficient. Every step in the HCV care continuum must be optimized to ensure that HCV-infected individuals are aware of their infection and linked to HCV treatment. Additionally, HCV treatment needs to be combined with harm reduction strategies for PWID, at-risk MSM and other high risk groups to reduce the risk of reinfection. After HCV cure, particular attention needs to be paid to surveillance for reinfections. These reinfections need to be prevented and when they occur, quickly treated to prevent onward transmission. And although it has eluded us thus far, work toward the development of an effective vaccine to prevent HCV infection must be intensified if the ambitious WHO HCV elimination targets are to be achieved by 2030 [14].
Acknowledgments
Financial support
Dr. Sulkowski received support through a NIH mid-career mentor award, K24 DA034621 and R01DA16065. Dr. Falade-Nwulia was supported by a NIH Mentored Patient-Oriented Research Career Development Award K23 DA041294.
Footnotes
Conflict of interest
Dr. Falade-Nwulia has nothing to disclose. Dr. Sulkowski reports research grants and personal fees from AbbVie, personal fees from Cocrystal, research grants and personal fees from Gilead, research grants and personal fees from Janssen, research grants and personal fees from Merck, and personal fees from Trek.
Authors’ contributions
Dr. Falade-Nwulia wrote the first draft of the manuscript; Dr. Sulkowski provided critical revisions to the work and created the figure. Both authors approved the final submission.
References
- 1.World Health Organization. Draft global health sector strategy on viral hepatitis 2016–2021. The first of it’s kind. 2015 [Google Scholar]
- 2.Martin NK, Vickerman P, Grebely J, Hellard M, Hutchinson SJ, Lima VD, et al. Hepatitis C virus treatment for prevention among people who inject drugs: Modeling treatment scale-up in the age of direct-acting antivirals. Hepatology. 2013;58:1598–1609. doi: 10.1002/hep.26431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin NK, Thornton A, Hickman M, Sabin C, Nelson M, Cooke GS, et al. Can hepatitis C virus (HCV) direct-acting antiviral treatment as prevention reverse the HCV epidemic among men who have sex with men in the United Kingdom? Epidemiological and modeling insights Clin Infect Dis. 2016;62:1072–1080. doi: 10.1093/cid/ciw075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lambers FA, Prins M, Thomas X, Molenkamp R, Kwa D, Brinkman K, et al. Alarming incidence of hepatitis C virus re-infection after treatment of sexually acquired acute hepatitis C virus infection in HIV-infected MSM. Aids. 2011;25:F21–F27. doi: 10.1097/QAD.0b013e32834bac44. [DOI] [PubMed] [Google Scholar]
- 5.Martin TC, Martin NK, Hickman M, Vickerman P, Page EE, Everett R, et al. Hepatitis C virus reinfection incidence and treatment outcome among HIV-positive MSM. Aids. 2013;27:2551–2557. doi: 10.1097/QAD.0b013e32836381cc. [DOI] [PubMed] [Google Scholar]
- 6.Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of late relapse or reinfection with hepatitis C virus after achieving a sustained virological response: a systematic review and meta-analysis. Clin Infect Dis. 2016;62:683–694. doi: 10.1093/cid/civ948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Midgard H, Bjoro B, Maeland A, Konopski Z, Kileng H, Damas JK, et al. Hepatitis C reinfection after sustained virological response. J Hepatol. 2016;64:1020–1026. doi: 10.1016/j.jhep.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Hagan H, Jordan AE, Neurer J, Cleland CM. Incidence of sexually transmitted hepatitis C virus infection in HIV-positive men who have sex with men. Aids. 2015;29:2335–2345. doi: 10.1097/QAD.0000000000000834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ingiliz P, Martin TC, Rodger A, Stellbrink HJ, Mauss S, Boesecke C, et al. HCV reinfection incidence and spontaneous clearance rates in HIV-positive men who have sex with men in Western Europe. J Hepatol. 2017;66:282–287. doi: 10.1016/j.jhep.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Salazar-Vizcaya L, Kouyos RD, Zahnd C, Wandeler G, Battegay M, Darling KE, et al. Hepatitis C virus transmission among HIV-infected men who have sex with men: Modeling the effect of behavioral and treatment interventions. Hepatology. 2016 doi: 10.1002/hep.28769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matser A, Vanhommerig J, Schim van der Loeff MF, Geskus RB, de Vries HJ, Prins JM, et al. HIV-infected men who have sex with men who identify themselves as belonging to subcultures are at increased risk for hepatitis C infection. PLoS One. 2013;8:e57740. doi: 10.1371/journal.pone.0057740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erica L, Pufall MK, Maryam Shahmanesh, Anthony Nardone, Richard Gilson, Valerie Delpech, Helen Ward, Postive Voices Study Group Chemsex and high-risk sexual behaviours in hiv-positive men who have sex with men; Conference on Retroviruses and Opportunistic Infections; Boston. 2016. [Google Scholar]
- 13.Hellard M, Rolls DA, Sacks-Davis R, Robins G, Pattison P, Higgs P, et al. The impact of injecting networks on hepatitis C transmission and treatment in people who inject drugs. Hepatology. 2014;60:1861–1870. doi: 10.1002/hep.27403. [DOI] [PubMed] [Google Scholar]
- 14.Cox AL. MEDICINE. Global control of hepatitis C virus. Science. 2015;349:790–791. doi: 10.1126/science.aad1302. [DOI] [PubMed] [Google Scholar]


