Abstract
Substance use is common in first-episode psychosis (FEP) and has been linked to poorer outcomes with more severe psychopathology and higher relapse rates. Early substance discontinuation appears to improve symptoms and function. However, studies vary widely in their methodology, and few have examined patients longitudinally, making it difficult to draw conclusions for practice and treatment. We aimed to investigate the relationship between substance use and early abstinence and the long-term course of illness in a representative sample of FEP patients. Out of 301 included patients, 266 could be divided into 4 groups based on substance use patterns during the first 2 years of treatment: persistent users, episodic users, stop-users and nonusers. Differences in clinical and functional measures during the follow-up period were assessed using linear mixed effects models for the analysis of repeated measures data. Patients who stopped using substances within the first 2 years after diagnosis had outcomes similar to those who had never used with fewer symptoms than episodic or persistent users. Both episodic and persistent users had lower rates of symptom remission than nonusers, and persistent users also had more negative symptoms than those who stopped using. Our findings emerge from one of very few long-term longitudinal studies examining substance use cessation in FEP with 10-year follow-up. The results convey hope that the detrimental effects of substance abuse on mental health may be significantly reversed if one stops the abuse in time. This can help patients who struggle with addiction with their motivation to embrace abstinence.
Keywords: substance abuse, schizophrenia, psychosis, negative symptoms
Introduction
Substance use is common among patients with psychosis. Literature suggests prevalence rates that are approximately twice that of the general population,1–3 with an effect on prognosis that can be deleterious.4–6 Psychosis and substance use have been associated with more hospital days,7 shorter, but more frequent admissions,6 greater violence,7 more severe psychopathology,4,8–10 higher relapse rates,2,5,11 and lower life expectancy.12 Several studies indicate that patients who continue abusing throughout their illness have poorer outcomes than those who stop early on in their course.10,13 Abuse discontinuation, on the other hand, has been associated with significant improvements in positive symptoms, depression, global functioning,14 and negative symptoms.15 Given the high rates of substance abuse in first-episode psychosis (FEP), outcomes in current and past users should be mapped out and differentiated from outcomes in nonusers. However, these studies are often hampered by selective sampling, or ambiguous sampling such as grouping patients with acute FEP and chronic psychosis.4,7,16 Also, most studies are short-term or cross-sectional,17,18 leaving longitudinal course unclear.14,19 To date, there are only 2 FEP longitudinal studies focusing on current and former substance users with psychosis; and only 2 following patients long term.15,20,21 In a well-designed study of patients hospitalized for a FEP, González-Pinto et al focused on cannabis use following patients for 8 years,15 assessing patients with clinical interviews at years 1, 3, and 5. Out of an original number of 112 inpatients, 82 completed follow-up and researchers concluded that those who discontinued use early on had significantly better outcomes. This was also the conclusion in the 5-year follow-up in the OPUS trial where patients who stopped using cannabis had lower levels of psychotic symptoms and better functioning.21 Even if these results are promising, it is unclear to what extent they can be generalized to other samples and other types of substances.
The aim of this study is to examine the long-term (10 y) influence of substance use and the effect of early substance use discontinuation in a representative sample of FEP patients. We hypothesize that:
patients who never used substances have superior long-term symptom and function outcomes compared to those who abuse or have abused,
patients who stop using have superior long-term symptom and function outcomes compared to those who continue using, and
persistent use predicts the worst long-term symptom and function.
Methods
Study Design
The study was a naturalistic, longitudinal follow-up of a large, clinical epidemiological sample collected consecutively from 4 Scandinavian healthcare sectors, including 2 sectors in Rogaland County, Norway, the Ullevaal sector in Oslo County, Norway and a sector from Roskilde County, Denmark. The combined estimated population was 665000 inhabitants. In all sectors, healthcare services were catchment area based and publicly funded. The 2 Rogaland sectors engineered systematic, early detection of psychosis and constituted the experimental sample.22 The Oslo and Roskilde sectors did not use an early detection paradigm and formed the comparison sample. For the present study, the samples from all areas are merged.
The areas were similar sociodemographically (urbanicity, mean educational level, income level, and opportunities for employment).23 Patients from all areas were treated according to a 2-year standard treatment protocol that included antipsychotic medication, supportive psychotherapy, and multifamily psycho education. Patients from the early detection area had lower symptom levels, shorter duration of untreated psychosis (DUP), lower age, and more alcohol and/or substance abuse at baseline presentation.23
The Regional Committee for Research Ethics approved this study.
Participants
The inclusion criteria, extensively described elsewhere,23 included first-episode schizophrenia, schizophreniform disorder or schizoaffective disorder, delusional disorder, mood disorder with mood-incongruent psychotic features, brief psychotic disorder or psychosis not otherwise specified,24 living in one of the participating sites, being 15–65 years of age (18–65 in control sectors), and functionally within the normal range of intellectual capacity (WAIS-R-based IQ estimate > 70). All study participants gave informed consent. Of eligible participants, 23% declined participation. Those who declined participation had longer DUP (32 vs 10 wk). There were no other significant differences between those who did and those who did not give consent to enter the study.25
Three hundred and one patients were included between 1997 and 2001 and followed up at 3 months and 1, 2, 5, and 10 years. At 10 years, 85 patients did not complete follow-up (49 refused, 23 did not show up, and 13 were untraceable), and 30 additional patients had died.26 An analysis of drop-out was conducted through a 2-way ANOVA with group and drop-out status at 10 years as factors and symptom levels at 2 years (positive and negative) as dependent variables. There was no association measured by interaction effects between group and drop-out status on positive (F = 0.6; df = 3; P = .62) or negative (F = 1.5; df = 3; P = .21) symptoms.
Assessments
The Structured Clinical Interview for the DSM-IV (SCID)27 was used for diagnostic purposes. This takes into account the persons own description of events and symptoms as well as medical records and co-lateral information. All included patients were assessed using Global Assessment of Functioning (GAF) where scores were split into symptom and function scores.28 Demographic data were collected for all study eligible patients. DUP was measured as time (weeks) from the emergence of positive psychotic symptoms to the start of adequate treatment of psychosis. Adequate treatment was defined as the start of structured treatment with antipsychotic medication or admission to highly staffed psychiatric wards organized to manage psychotic symptoms. A few nonadmitted patients started outpatient psychotherapy structured and directed towards psychosis, but did not want medication initially. For these patients, start of psychotherapy was regarded as start of adequate treatment. Symptom levels were measured by the Positive and Negative Syndrome Scale (PANSS),27 scored on 5 symptom domains: positive, negative, cognitive, depressive, and excitative symptoms.29 Onset of first-episode positive psychotic symptoms was defined as a PANSS score of 4 or higher on positive scale items P1-delusions, P3-hallucinatory behavior, P5-grandiosity, P6-suspiciousness, or General scale item G9-unusual thought content; not previously receiving adequate treatment for psychosis was defined as antipsychotic medication of 3.5 haloperidol equivalents for 12 weeks or until remission of psychotic symptoms.
Premorbid functioning was measured by the Premorbid Adjustment Scale (PAS),30 covering 2 areas of functioning—school adaptation and socialization—described through initial childhood level and subsequent change.31 Scores ranged from 1 to 6 with higher scores indicating more impairment. A PAS change score was calculated as the difference between childhood scores and the last score available, to indicate decline or improvement over time.31
Length of treatment was split into length of psychotherapy and length of antipsychotic treatment and measured in the sum of weeks of periods of uninterrupted antipsychotic medication or psychotherapy with a frequency of once every fortnight or more (between 5 and 10 y: once a month).
Outcome Measures
Symptom outcome was defined as the proportion of patients in remission in accordance with international standardized criteria,32 ie, no score of 4 or higher for the past 6 months on any of the following PANSS-items: P1-delusions, P2-disorganized thought, P3-hallucinatory behavior, N1-affective flattening, N4-passive social withdrawal, N6-lack of spontaneity, G5-bizarre posture, or G9-unusual thought content.
Functional outcome was assessed using the Strauss-Carpenter level of functioning scale,33 specifying degree of competitive employment or academic activity, housing, social contact, and the extent to which patients had been hospitalized for mental health problems over the last 12 months.
Recovery was defined as a combination of symptom remission and adequate social functioning according to the Strauss-Carpenter score. This includes at least 12 months of work or study full time, living independently, seeing friends at least once a week, and not having been hospitalized.
All ratings were conducted by our assessment team of trained raters who were blind to substance use group affiliation of participants. Reliability of GAF, DUP, and diagnosis has previously been reported on34,35 and was found satisfactory throughout the study.
Measurement and Classification of Substance Use
Substance and alcohol use were measured by the Alcohol and Drug Use Scale36 which employs a scale from 1 to 5 (1 = no-use; 2 = use without impairment; 3 = abuse; 4 = dependence; 5 = dependence with institutionalization). All commonly used illegal psychoactive substances were included. Alcohol was classified as a separate variable and used as a covariate.
We did not include tobacco or caffeine in our definition as treatment and sequelae for these differ substantially from other substances. We defined “use” as any score >1. Patients were assessed with regards to pattern of substance use at all follow-up points except at 3 months. At 5-year follow-up, we assessed substance use at 3 and 4 years based on patient information and medical charts.
Patients’ substance use changed the most during the first 2 years after inclusion, thus this interval was chosen for grouping. This interval is consistent with prior studies.37–40
We grouped patients into (a) nonusers (NUs), ie, patients who had never used; (b) stop-users (SUs); (c) episodic users (EUs), and (d) persistent users (PUs). This 4-group solution was chosen on the basis of newer studies that have shown that around half of substance-using patients stop using early on in their illness3 and that these patients appear to have less severe symptoms than those who continue using.14 As a result of including SU in the user groups, earlier studies may have underestimated symptom load in patients who uphold substance use habits. Furthermore, merging previous substance users with NUs does not aid in understanding how stopping substance use can benefit patient trajectories/prognoses.
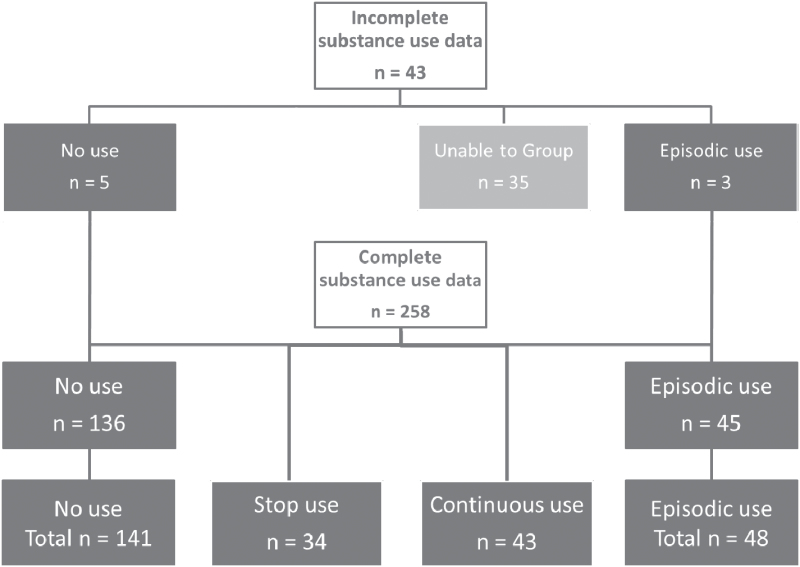
Figure 1 provides an overview of patient characteristics. Two hundred and fifty-eight patients had ratings at baseline, 1 year, and 2 years. Among these, 136 had 3 consecutive measurements of “no-use,” and were assigned to the NU group. Thirty-four patients used substances at baseline but had no-use the 2 following years. They constituted the SU group. PU contained 43 patients who had “use” at all 3 follow-up points. Forty-five patients with various other patterns were termed EU. Among the 43 patients with incomplete data sets, we were able to assign 8 to user groups. Five of these were assigned to the NU group. Four had missing data at 2 years but no-use at baseline, 1 year, and 3 years, and 1 had missing data at 1 year but no-use at baseline, 2 years, and 3 years. Three patients were assigned to the EU group. One had no-use at baseline and 2 years but was using at 3 years and 2 patients were assigned to the EU group due to no-use at baseline but use at 1 year. Consequently, they would have been assigned to of the EU group irrespective of status at 2-year follow-up. A total of 266 patients were assigned (NU = 141, SU = 34, EU = 48, and PU = 43). The 35 non-assigned patients were not significantly different from the assigned ones at baseline except for lower scores on GAF symptoms (27.0 vs 29.6) and GAF function (28.3 vs 32.0). Only 2 (6%) of the non-assigned patients completed 10-year follow-up compared to 184 (69%) of the assigned ones.
Fig. 1.
Overview of patient grouping in a long-term follow-up study of early detection in psychosis.
Statistical Analyses
Statistical analyses were carried out using SPSS version 22.041 and R.42
Differences between substance use groups were described using frequencies and percentages for categorical variables and means and SDs or medians and ranges for continuous variables. Comparisons between groups were made using chi-square tests for categorical data and ANOVA or Kruskal-Wallis for continuous data with Scheffe post hoc tests for group-by-group comparisons. All tests were 2-tailed. Two-way repeated measures ANOVA was used to investigate differences over the first 2 years between groups.
To investigate the effect of substance abuse on symptom and function outcome, we used linear mixed effects (LME) models. Separate models were estimated, each with one of the 5 PANSS component scores, GAF symptom or GAF function as the dependent variable and substance use group as predictor. For PANSS positive and negative symptoms, the models included random intercept only, while for the other symptom components and GAF symptom and GAF function, random intercept and random slope models were employed. Linear models yielded the best fit, except for the depressive component where a cubic model proved superior. Because the effect of interest was that of substance abuse during the first 2 years of treatment, outcome variables were based on data from 2-, 5-, and 10-year follow-up assessments. Other predictors and possible confounders were chosen on the basis of literature and on group differences at baseline: age, DUP, length of medication treatment, length of psychotherapy, alcohol use, and gender. Persistent use provided a reference category. The average PANSS negative component values over time indicated different change rates for the negative component scores, and we fitted a model allowing for this by including the interaction effect between group and time. Use of such complex models can be justified by the size of the data set, and it produced an adequate fit to the data with close to minimal Akaike Information Criterion (AIC) value.
Results
At 10 years, 49.5% of the sample was remitted, while 25% also fulfilled criteria for recovery. Table 1 outlines background and clinical characteristics at study inclusion and at 2-year follow-up of the 4 substance use groups. In substance user groups, the proportion of males was higher than in the NU group. NUs were significantly older than PU or EUs. PUs had a lower baseline GAF symptom score than NUs; no other differences. Drake substance use scores at baseline showed significant differences between user groups (SU: 2.65; EU: 1, 83; CU: 3.07; SD = 0.1 in all 3 groups; df between = 2; df within = 122; F = 25, 2; P = .001). Hence, EUs had the lowest and the PUs the highest baseline substance use scores, with the SUs at an intermediate mean score. There were no differences in premorbid adjustment, except that PUs had a larger premorbid decline in academic functioning. There was a significant difference among groups with regards to decrease in positive symptoms during the first 2 years of follow-up (F = 8.5; df = 3, 243; P = .009) with a significantly larger decline in the NU compared to the PU group (Scheffe post hoc test mean difference = −2.0; P = .020). GAF symptoms showed that both the NU and the SU group had significantly more improvement compared to the PU group (substance use group by GAF symptom interaction F = 6.6; df = 3; P = .004; mean differences 5.4 and 5.5, respectively, and P = .026 for both). There was no difference in DUP among groups.
Table 1.
Baseline Characteristics at Study Inclusion and at 2 y for First-Episode Psychosis Patients Across Patterns of Substance Abuse
| N = 266 | No (NU) | Stop (SU) | Episodic (EU) | Persistent (PU) | Analysis | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 141 | n = 34 | n = 48 | n = 43 | |||||||
| N | % | N | % | N | % | N | % | χ2 | df | |
| Malea | 66 | 47 | 26 | 76 | 30 | 63 | 34 | 79 | 20.3 | 3 |
| Diagnosis at inclusion | ||||||||||
| Schizophrenia spectrum | 82 | 58 | 23 | 6 | 34 | 71 | 28 | 65 | 3.1 | 3 |
| Affective | 24 | 17 | 3 | 9 | 5 | 10 | 4 | 9 | 1.9 | 3 |
| Other | 35 | 25 | 8 | 24 | 9 | 19 | 11 | 26 | 6.4 | 3 |
| Median | Range | Median | Range | Median | Range | Median | Range | F | df | |
| DUPb (wk) | 6 | 0–1196 | 10 | 0–416 | 14 | 0–468 | 12 | 1–555 | 0.7 | 262 |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | F | df d | |
| Agec | 30.8 | 10.2 | 26.5 | 8.3 | 22.6 | 5.0 | 22.4 | 4.4 | 18.0 | 262 |
| Premorbid adjustment, change from childhood to adolescence | ||||||||||
| Social | 0.8 | 1.5 | 0.9 | 1.5 | 0.9 | 1.6 | 0.9 | 1.4 | 0.1 | 256 |
| Academic | 0.5 | 1.3 | 0.5 | 1.3 | 0.9 | 1.3 | 1.1 | 1.2 | 3.7 | 256 |
| PANSS and GAF | ||||||||||
| Positive | 15.2 | 4.3 | 15.8 | 4.7 | 14.7 | 3.9 | 15.6 | 4.4 | .52 | 261 |
| Negative | 20.6 | 9.7 | 20.8 | 8.0 | 21.0 | 8.7 | 20.5 | 7.9 | .99 | 260 |
| GAF symptome | 29.3 | 7.0 | 28.0 | 7.0 | 29.3 | 7.7 | 32.2 | 5.7 | 2.7 | 260 |
| GAF function | 31.6 | 10.6 | 29.7 | 9.6 | 32.0 | 11.3 | 35.1 | 8.8 | 1.9 | 260 |
| PANSS and GAF at 2 y | ||||||||||
| Positive | 8.2 | 3.8 | 8.3 | 3.8 | 11.1 | 5.6 | 11.1 | 5.7 | 7.4 | 243 |
| Negative | 16.6 | 7.7 | 17.8 | 8.9 | 19.0 | 8.9 | 16.2 | 7.0 | 1.2 | 243 |
| GAF symptomf | 55.3 | 16.8 | 53.7 | 17.0 | 45.2 | 14.2 | 46.7 | 14.7 | 5.9 | 245 |
| GAF function | 56.2 | 16.0 | 53.9 | 17.5 | 44.9 | 15.5 | 47.7 | 15.7 | 6.8 | 246 |
Note: Other diagnoses: delusional disorder (n = 7), brief psychotic disorder (n = 3), organic psychosis (n = 1), and psychosis NOS (n = 10). DUP, duration of untreated psychosis; EU, episodic user; GAF, Global Assessment of Functioning; NOS, not otherwise specified; NU, nonuser; PANSS, Positive and Negative Syndrome Scale; PU, persistent user; SU, stop-user.
a P < .001, pairwise comparisons NU vs SU and NU vs PU.
bReported values are median values, while ANOVA was done with log-transformed DUP values.
cAll between-group df =3; df reported in table concerns within-group df.
dPost hoc comparisons Scheffe test pairwise comparisons NU and EU, NU and PU, P < .001.
ePost hoc comparisons Scheffe test pairwise comparison NU and PU, P < .012.
fPost hoc comparisons Scheffe test pairwise comparison SU and PU, P < .045.
At 10-year follow-up, mean duration of psychotherapy was 62% of the time (SD = 30.6), and for use of antipsychotic medication 68% of the time (SD = 34.0) with no differences among substance use groups. The mean percentage of time hospitalized was 11% (SD = 19%). EUs spent the highest proportion of time hospitalized, significantly longer than the NU group (19.6% vs 8.3%, respectively; F = 4.2; df between = 3; df within = 192; P = .007).
Table 2 outlines the main results at the 10-year follow-up. Significantly more NUs and SUs were in symptomatic remission at 10 years compared both to patients with persistent and with episodic use. With regards to social functioning, a significantly higher percentage of SUs were able to work compared to all other groups.
Table 2.
Clinical and Functional Status of First-Episode Psychosis Patients at 10-y Follow-up Across Patterns of Substance Abuse
| Pattern of Substance Abuse | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pattern of Use | NU | SU | EU | PU | Analysis | |||||
| N = 184 | n = 98 | n = 22 | n = 32 | n = 32 | ||||||
| N | % | N | % | N | % | N | % | df | χ2 | |
| Remissiona | 54 | 55.1 | 14 | 63.6 | 10 | 31.3 | 12 | 37.5 | 3 | 9.1 |
| Recovery | 26 | 26.5 | 8 | 36.4 | 3 | 9.4 | 7 | 21.9 | 3 | 6.0 |
| Any employmentb | 47 | 48.0 | 16 | 72.7 | 8 | 25.0 | 13 | 40.6 | 3 | 12.5 |
| Livingc independently | 75 | 76.5 | 17 | 77.3 | 13 | 40.6 | 20 | 62.5 | 3 | 15.6 |
| Weekly contact with friends | 46 | 47.4 | 12 | 54.5 | 14 | 43.8 | 14 | 43.8 | 3 | 0.6 |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | df | F | |
| % of time admittedd | 8.3 | 15.3 | 11.2 | 23.7 | 19.6 | 22.4 | 18.6 | 24.2 | 192 | 4.2 |
Note: Abbreviations are explained in the first footnote to table 1.
a P = .007.
b P = .006.
c P = .001.
d P = .007.
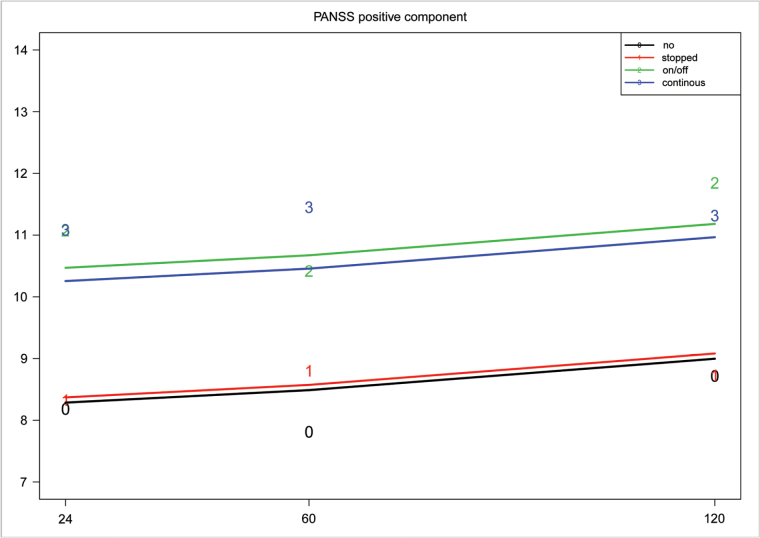
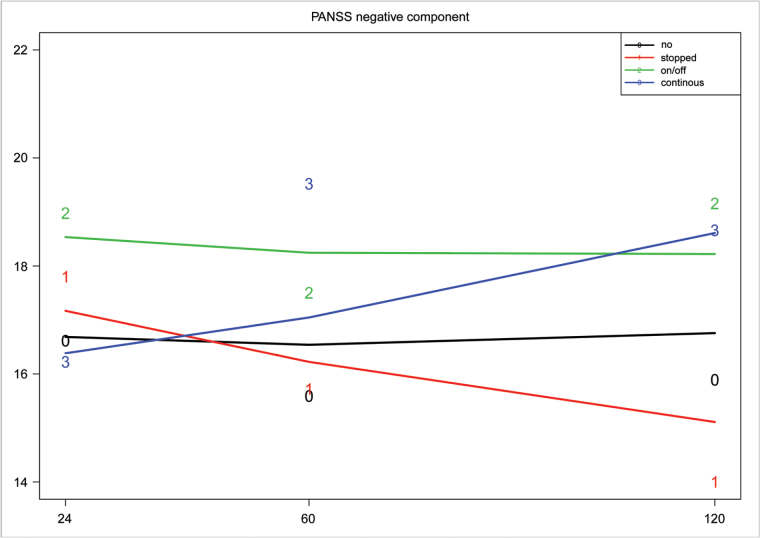
Figures 2 and 3 illustrate development of positive and negative symptoms over time in the various groups. No-use and stop-use both statistically predicted overall lower positive symptom scores compared to the persistent-use group across the whole follow-up period (rate 1.97/y: df = 252; t = −2.8; P = .006 and rate 1.89/y: df = 252; t = −2.2; P = .031, respectively). Lower positive symptom levels were also associated with shorter medication use, female gender, less alcohol abuse, and shorter DUP. PU patients had increasing levels of negative symptoms, though not statistically significant (rate 0.026 points/year: df = 345; t = 2.1; P = .07), whereas those who had stopped showed decreasing rates (rate −0.019/y: df = 345; t = −2.1; P = .04) (figure 3). Male gender and longer medication use were also associated with more negative symptoms.
Fig. 2.
PANSS positive scores measured by the 5-factor model with LME model superimposed in first-episode psychosis patients. LME, linear mixed effects; PANSS, Positive and Negative Syndrome Scale.
Fig. 3.
PANSS negative scores measured by the 5-factor model with LME model superimposed in first-episode psychosis patients. LME, linear mixed effects; PANSS, Positive and Negative Syndrome Scale.
Between 2 and 10 years, there was a significant increase across all groups in positive and depressive symptoms (regression coefficient = 0.10; df = 348; t = 2.1; P = .040 for the positive component and regression coefficient = 0.6; df = 346, t = −3.4; P < .001 for depressive symptoms). However, NU statistically predicted lower excitatory, depressive, and cognitive symptom scores compared to the other groups (df = 252; t = −2.9; P = .004 for the excitatory; df = 252; t = −2.3; P = .022 for the depressive; df 345; t = −2.7; P = .007 for the cognitive component). Alcohol abuse statistically predicted higher depressive component scores (df = 346; t = 2.0; P = .043).
The NU and SU groups had significantly lower GAF symptom levels compared to PU patients (df = 254; t = 3.1; P = .003 for NU and df = 254; t = 2.9; P = .037 for SU). GAF function was significantly better in both NUs and SUs (df = 254; t = 3.9; P = .0001 for NU and df = 254; t = 2.4; P = .019 for SU) compared to PUs. NU patients, however, showed deteriorating GAF function scores over time (df = 346; t = 2.8; P = .005). Longer DUP, longer treatment with medication, more psychotherapy, and male gender were significant covariates that were also associated with lower GAF function scores.
Discussion
The main finding of this study is that those who became completely abstinent early achieved outcomes similar to patients who had never used. Both of these groups had outcomes superior to patients who continued using. Even though our statistical models cannot establish causality, our results are nevertheless in agreement with other studies that have shown that young people with substance use and severe mental illness who stop using have more benign illness courses.38,43 Our user groups were based on the absence or presence of substance use, in absolute terms, whereas, many programs working with FEP or schizophrenia focus on harm-reduction methods. Some studies, for instance a large London-based study, have shown that reduction of use is beneficial for course and outcome, along with abstinence.44 Our data suggest abstinence as an effective way to positively influence outcome, in line with previous literature.15 Also, abstinence is a culturally relevant concept in Norway, where substance use is largely restricted to subgroups, with any use being considered harmful.
The patients in our stop-use group stopped early in the course of treatment. A recent meta-analysis14 also underscores the point that early substance use discontinuation can improve prognosis. The fact that harm can be substantially minimized with early discontinuation gives a hopeful message for patients who struggle with addiction and psychosis.
Considering that the stop-use group by far outperforms the other groups on being in employment, as well as having the highest remission rate, one might wonder whether substance use has elicited psychotic symptoms in the context of lower vulnerabilities. The fact that PUs were the only group to show a significant decline in premorbid functioning points in this direction.
Several negative symptom-like aspects have been observed in different types and stages of substance use,45,46 but the relation between substance abuse and negative symptoms in psychosis remains unclear. Our results, showing improvement in negative symptoms with cessation of substance use, are of interest as these are symptoms difficult to treat with antipsychotics. In addition, these symptoms are closely linked to daily and social functioning and quality of life. Focusing explicitly on cessation of substance use may present as an opportunity to improve patient outcomes in this distinctively destructive domain.
There are more males in all substance use groups with lower ages of onset in both EU and PU patients compared to NU patients, confirming what has been found by others.7,10,16,47 Male gender statistically predicted more positive symptoms and poorer GAF scores, and greater increases in negative symptoms over time. Male gender and lower age could be confounding variables, partly explaining the association between substance use and poorer prognosis. However, all of our analyses indicated independent contributions of all these factors in the prediction models. This strongly support the notion that early discontinuation of substance use is an independent factor for better outcomes.
Another prognostic factor concerns DUP, with longer DUP predicting higher positive symptom scores as well as worse functioning. Substance-related symptoms could imaginably masquerade the earliest signs of psychosis, thus delaying help-seeking behavior, leading to lower functioning, higher symptom loads at presentation, and worse prognosis.48
LME analysis showed an association between the PANSS positive component score and the use of more medication, as one would expect. Despite this, analyses did not reveal any differences in length of treatment (medication or psychotherapy) among the groups. This could be due to noncompliance within groups. This is in line with other studies, where no association with treatment type or medication adherence and lifetime substance use was found.49
Strengths and Limitations
The study has several strengths. The sample is representative, grouped by applying rigorous monitoring during the first 2 years after inclusion, with follow-up up to 10 years.
The main limitations concern a lack of valid information of substances used and the lack of means for controlling patients’ claims of substance use cessation. Measures such as urine toxicology screenings could have strengthened our findings. On the other hand, urine samples are viewed as intrusive by many and might have reduced the representability of our sample. Additionally, they are only valid for shorts amounts of time and only for a limited number of substances. We were aware of the possibility of underreporting with regards to substance use. However, assessors were conscious of adopting a nonjudgmental approach, and our experience was that the information patients provided was generally consistent with other sources of information. Patients were part of the project voluntarily and we used all available information, such as co-lateral information and patient files in addition to clinical interviews. This allowed for triangulation of information, as done in other studies.10,20
Conclusion
Addressing substance use as early as possible is critical, as early substance use termination predicts better long-term outcome.
Funding
This work was supported by Health West, Norway #911369; the Norwegian National Research Council #133897/320 and #154642/320, the Norwegian Department of Health and Social Affairs, and the National Council for Mental Health, Health and Rehabilitation #1997/41 and #2002/306, Rogaland County and Oslo County. This work was also funded by the Theodore and Vada Stanley Foundation and the Regional Health Research Foundation for Eastern Region, Denmark; Roskilde County, Helsefonden, Lundbeck Pharma, Eli Lily, and Janssen Cilag Pharmaceuticals Denmark; the National Alliance for Research on Schizophrenia and Depression NARSAD distinguished investigator award and NIM grant MH-01654 and a NARSAD young investigator award; and Health South East #2008001 and Health West #200202797-65 and #911313.
Acknowledgments
The project has been approved by the Regional Committee for Research Ethics Health Region 2 (#S95189) and the Regional Committee for Research Ethics Health Region East (#1.2007.2177). Data inspectorate license: #96/3017-2, #2003/2052. The Regional Committee for science ethics region Sjælland: #1-01-83-0002-07. S.O. has given advice to Otsuka and Lundbeck and lectured in meetings organized by those companies. All other authors state that they have nothing to disclose. S.F., T.M., J.O.J., T.K.L., I.J., P.V., S.O., I.M., B.R.R., E.S., and U.H. took part in designing the study. T.K.L., I.M., S.F., E.S., U.H., W.T.V.H., and J.E. collected the data. M.A.W., S.F., and B.A. undertook the analysis. M.A.W. wrote the first draft of the manuscript. All authors critically reviewed the paper and approved the final version.
References
- 1. Barnett JH, Werners U, Secher SM, et al. Substance use in a population-based clinic sample of people with first-episode psychosis. Br J Psychiatry. 2007;190:515–520. [DOI] [PubMed] [Google Scholar]
- 2. Wade D, Harrigan S, Edwards J, Burgess PM, Whelan G, McGorry PD. Substance misuse in first-episode psychosis: 15-month prospective follow-up study. Br J Psychiatry. 2006;189:229–234. [DOI] [PubMed] [Google Scholar]
- 3. Wisdom JP, Manuel JI, Drake RE. Substance use disorder among people with first-episode psychosis: a systematic review of course and treatment. Psychiatr Serv. 2011;62:1007–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Harrison I, Joyce EM, Mutsatsa SH, et al. Naturalistic follow-up of co-morbid substance use in schizophrenia: the West London first-episode study. Psychol Med. 2008;38:79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Malla A, Norman R, Bechard-Evans L, Schmitz N, Manchanda R, Cassidy C. Factors influencing relapse during a 2-year follow-up of first-episode psychosis in a specialized early intervention service. Psychol Med. 2008;38:1585–1593. [DOI] [PubMed] [Google Scholar]
- 6. Schmidt LM, Hesse M, Lykke J. The impact of substance use disorders on the course of schizophrenia–a 15-year follow-up study: dual diagnosis over 15 years. Schizophr Res. 2011;130:228–233. [DOI] [PubMed] [Google Scholar]
- 7. Crebbin K, Mitford E, Paxton R, Turkington D. Drug and alcohol misuse in first episode psychosis: an observational study. Neuropsychiatr Dis Treat. 2008;4:417–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Farrelly S, Harris MG, Henry LP, et al. Prevalence and correlates of comorbidity 8 years after a first psychotic episode. Acta Psychiatr Scand. 2007;116:62–70. [DOI] [PubMed] [Google Scholar]
- 9. Margolese HC, Carlos Negrete J, Tempier R, Gill K. A 12-month prospective follow-up study of patients with schizophrenia-spectrum disorders and substance abuse: changes in psychiatric symptoms and substance use. Schizophr Res. 2006;83:65–75. [DOI] [PubMed] [Google Scholar]
- 10. Addington J, Addington D. Patterns, predictors and impact of substance use in early psychosis: a longitudinal study. Acta Psychiatr Scand. 2007;115:304–309. [DOI] [PubMed] [Google Scholar]
- 11. Linszen DH, Dingemans PM, Lenior ME. Cannabis abuse and the course of recent-onset schizophrenic disorders. Arch Gen Psychiatry. 1994;51:273–279. [DOI] [PubMed] [Google Scholar]
- 12. Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–1131. [DOI] [PubMed] [Google Scholar]
- 13. Drake RE, McHugo GJ, Xie H, Fox M, Packard J, Helmstetter B. Ten-year recovery outcomes for clients with co-occurring schizophrenia and substance use disorders. Schizophr Bull. 2006;32:464–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mullin K, Gupta P, Compton MT, Nielssen O, Harris A, Large M. Does giving up substance use work for patients with psychosis? A systematic meta-analysis. Aust N Z J Psychiatry. 2012;46:826–839. [DOI] [PubMed] [Google Scholar]
- 15. González-Pinto A, Alberich S, Barbeito S, et al. Cannabis and first-episode psychosis: different long-term outcomes depending on continued or discontinued use. Schizophr Bull. 2011;37:631–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sorbara F, Liraud F, Assens F, Abalan F, Verdoux H. Substance use and the course of early psychosis: a 2-year follow-up of first-admitted subjects. Eur Psychiatry. 2003;18:133–136. [DOI] [PubMed] [Google Scholar]
- 17. Wade D, Harrigan S, Edwards J, Burgess PM, Whelan G, McGorry PD. Course of substance misuse and daily tobacco use in first-episode psychosis. Schizophr Res. 2006;81:145–150. [DOI] [PubMed] [Google Scholar]
- 18. Hides L, Dawe S, Kavanagh DJ, Young RM. Psychotic symptom and cannabis relapse in recent-onset psychosis. Prospective study. Br J Psychiatry. 2006;189:137–143. [DOI] [PubMed] [Google Scholar]
- 19. Van Mastrigt S, Addington J, Addington D. Substance misuse at presentation to an early psychosis program. Soc Psychiatry Psychiatr Epidemiol. 2004;39:69–72. [DOI] [PubMed] [Google Scholar]
- 20. Turkington A, Mulholland CC, Rushe TM, et al. Impact of persistent substance misuse on 1-year outcome in first-episode psychosis. Br J Psychiatry. 2009;195:242–248. [DOI] [PubMed] [Google Scholar]
- 21. Clausen L, Hjorthøj CR, Thorup A, et al. Change in cannabis use, clinical symptoms and social functioning among patients with first-episode psychosis: a 5-year follow-up study of patients in the OPUS trial. Psychol Med. 2014;44:117–126. [DOI] [PubMed] [Google Scholar]
- 22. Johannessen JO, Larsen TK, Joa I, et al. Pathways to care for first-episode psychosis in an early detection healthcare sector: part of the Scandinavian TIPS study. Br J Psychiatry Suppl. 2005;48:s24–s28. [DOI] [PubMed] [Google Scholar]
- 23. Melle I, Larsen TK, Haahr U, et al. Reducing the duration of untreated first-episode psychosis: effects on clinical presentation. Arch Gen Psychiatry. 2004;61:143–150. [DOI] [PubMed] [Google Scholar]
- 24. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 25. Friis S, Melle I, Larsen TK, et al. Does duration of untreated psychosis bias study samples of first-episode psychosis? Acta Psychiatr Scand. 2004;110:286–291. [DOI] [PubMed] [Google Scholar]
- 26. Friis S, Melle I, Johannessen JO, et al. Early predictors of ten-year course in first-episode psychosis. Psychiatr Serv. 2016;67:438–443. [DOI] [PubMed] [Google Scholar]
- 27. Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 28. Pedersen G, Hagtvet KA, Karterud S. Generalizability studies of the Global Assessment of Functioning-Split version. Compr Psychiatry. 2007;48:88–94. [DOI] [PubMed] [Google Scholar]
- 29. Bentsen H, Munkvold OG, Notland TH, et al. The interrater reliability of the Positive and Negative Syndrome Scale (PANSS). Int J Methods Psychiatr Res. 1996;6:227–235. [Google Scholar]
- 30. Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. 1982;8:470–484. [DOI] [PubMed] [Google Scholar]
- 31. Larsen TK, Friis S, Haahr U, et al. Premorbid adjustment in first-episode non-affective psychosis: distinct patterns of pre-onset course. Br J Psychiatry. 2004;185:108–115. [DOI] [PubMed] [Google Scholar]
- 32. Andreasen NC, Carpenter WT, Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162:441–449. [DOI] [PubMed] [Google Scholar]
- 33. Strauss JS, Carpenter WT., Jr The prediction of outcome in schizophrenia. II. Relationships between predictor and outcome variables: a report from the WHO international pilot study of schizophrenia. Arch Gen Psychiatry. 1974;31:37–42. [DOI] [PubMed] [Google Scholar]
- 34. Hegelstad WT, Larsen TK, Auestad B, et al. Long-term follow-up of the TIPS early detection in psychosis study: effects on 10-year outcome. Am J Psychiatry. 2012;169:374–380. [DOI] [PubMed] [Google Scholar]
- 35. Friis S, Larsen TK, Melle I, et al. Methodological pitfalls in early detection studies—the NAPE Lecture 2002. Nordic Association for Psychiatric Epidemiology. Acta Psychiatr Scand. 2003;107:3–9. [DOI] [PubMed] [Google Scholar]
- 36. Mueser KT, Noordsy DL, Drake RE, Fox L. Integrated Treatment for Dual Disorders. New York: The Guilford Press; 2003. [Google Scholar]
- 37. Baeza I, Graell M, Moreno D, et al. Cannabis use in children and adolescents with first episode psychosis: influence on psychopathology and short-term outcome (CAFEPS study). Schizophr Res. 2009;113:129–137. [DOI] [PubMed] [Google Scholar]
- 38. Lambert M, Conus P, Lubman DI, et al. The impact of substance use disorders on clinical outcome in 643 patients with first-episode psychosis. Acta Psychiatr Scand. 2005;112:141–148. [DOI] [PubMed] [Google Scholar]
- 39. Grech A, Van Os J, Jones PB, Lewis SW, Murray RM. Cannabis use and outcome of recent onset psychosis. Eur Psychiatry. 2005;20:349–353. [DOI] [PubMed] [Google Scholar]
- 40. Archie S, Rush BR, Akhtar-Danesh N, et al. Substance use and abuse in first-episode psychosis: prevalence before and after early intervention. Schizophr Bull. 2007;33:1354–1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.IBM Corp. Released 2010. IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp. [Google Scholar]
- 42.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 43. Strakowski SM, DelBello MP, Fleck DE, et al. Effects of co-occurring cannabis use disorders on the course of bipolar disorder after a first hospitalization for mania. Arch Gen Psychiatry. 2007;64:57–64. [DOI] [PubMed] [Google Scholar]
- 44. Stone JM, Fisher HL, Major B, et al. ; MiData Consortium Cannabis use and first-episode psychosis: relationship with manic and psychotic symptoms, and with age at presentation. Psychol Med. 2014;44:499–506. [DOI] [PubMed] [Google Scholar]
- 45. Kirschner M, Aleman A, Kaiser S. Secondary negative symptoms—a review of mechanisms, assessment and treatment [published online ahead of print May 23, 2016]. Schizophr Res. doi:10.1016/j.schres.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 46. Leventhal AM, Kahler CW, Ray LA, et al. Anhedonia and amotivation in psychiatric outpatients with fully remitted stimulant use disorder. Am J Addict. 2008;17:218–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Caton CL, Hasin DS, Shrout PE, et al. Predictors of psychosis remission in psychotic disorders that co-occur with substance use. Schizophr Bull. 2006;32:618–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Larsen TK, McGlashan TH, Johannessen JO, et al. Shortened duration of untreated first episode of psychosis: changes in patient characteristics at treatment. Am J Psychiatry. 2001;158:1917–1919. [DOI] [PubMed] [Google Scholar]
- 49. Kovasznay B, Fleischer J, Tanenberg-Karant M, Jandorf L, Miller AD, Bromet E. Substance use disorder and the early course of illness in schizophrenia and affective psychosis. Schizophr Bull. 1997;23:195–201. [DOI] [PubMed] [Google Scholar]