Abstract
Background
Exercise and statins reduce cardiovascular disease (CVD). Exercise capacity may be assessed using cardiopulmonary exercise testing (CPET). Whether statin medication is associated with CPET parameters is unclear. We investigated if statins are related with exercise capacity during CPET in the general population.
Methods
Cross-sectional data of two independent cohorts of the Study of Health in Pomerania (SHIP) were merged (n = 3,500; 50% males). Oxygen consumption (VO2) at peak exercise (VO2peak) and anaerobic threshold (VO2@AT) was assessed during symptom-limited CPET. Two linear regression models related VO2peak with statin usage were calculated. Model 1 adjusted for age, sex, previous myocardial infarction, and physical inactivity and model 2 additionally for body mass index, smoking, hypertension, diabetes and estimated glomerular filtration rate. Propensity score matching was used for validation.
Results
Statin usage was associated with lower VO2peak (no statin: 2336; 95%-confidence interval [CI]: 2287–2,385 vs. statin 2090; 95%-CI: 2,031–2149 ml/min; P < .0001) and VO2@AT (no statin: 1,172; 95%-CI: 1,142–1,202 vs. statin: 1,111; 95%-CI: 1,075–1,147 ml/min; P = .0061) in males but not females (VO2peak: no statin: 1,467; 95%-CI: 1,417–1,517 vs. statin: 1,503; 95%-CI: 1,426–1,579 ml/min; P = 1.00 and VO2@AT: no statin: 854; 95%-CI: 824–885 vs. statin 864; 95%-CI: 817–911 ml/min; P = 1.00). Model 2 revealed similar results. Propensity scores analysis confirmed the results.
Conclusion
In the general population present statin medication was related with impaired exercise capacity in males but not females. Sex specific effects of statins on cardiopulmonary exercise capacity deserve further research.
Introduction
Cardiovascular diseases (CVD) are the most common cause of morbidity and mortality in Western societies [1]. Primary and secondary prevention strategies target predisposing risk factors (e.g. increased low-density lipoprotein [LDL] plasma concentrations or physical inactivity) using pharmacological and lifestyle-modification strategies. A prime example for pharmacological strategies is statin medication which is predominantly used to reduce LDL levels [2]. Possible non-pharmacological prevention modalities include increasing physical activity and dietary counselling. In the past a plethora of research has investigated the effectiveness and specificity of these prevention options [3,4]. However, possible interactions between drugs and lifestyle interventions are only beginning to be recognized [5].
Exercise is well known to increase endothelial nitric oxide bioavailability and improve endothelial function as well as decrease the overall inflammatory burden and vascular resistance [6–8]. The non-lipid pleiotropic effects of statins exert similar effects on these parameters [2,9]. Additionally, a previous randomized clinical trial reported that statin medication impaired training induced increases in exercise capacity [10]. Therefore, exercise and statins may interact with one another. Standardized cardiopulmonary exercise testing (CPET) is a standard method to determine exercise capacity. Currently there is a knowledge gap in the literature whether statins are related with CPET results. We explored the association of statin medication with CPET parameters in the general population. The aim of this study was to investigate if statins are associated with cardiorespiratory exercise capacity using cross-sectional data from two independent population-based cohorts (Study of Health in Pomerania [SHIP]). Based on the previous findings we hypothesized an inverse association between exercise capacity and statin medication.
Methods
Study design and participants
For this analysis data derived from two independent cohorts of SHIP in West Pomerania in the Northeast of Germany [11] were merged. Recruitment strategy and study design have been reported elsewhere [12]. Briefly, between October 1997 and May 2001 6,265 subjects (age 20 to 79) were invited to participate in the study (SHIP-0). At baseline a total of 4,308 men and women agreed to an in depth health screening (response 68.8%), which has previously been described [12]. This investigation included data from the first follow-up examination between March 2003 and July 2006 (SHIP-1). Ten years after SHIP-0 a second, independent cross-sectional population-based study was initiated in the same geographical region: SHIP-Trend-0. A stratified random sample of 8,016 adults between the ages of 20–79 years was drawn. Both studies were approved by the ethics committee of the University of Greifswald and comply with the Declaration of Helsinki. All participants gave written consent. SHIP data are publically available for scientific and quality control purposes. Data usage can be applied for via www.community-medicine.de.
Initially all subjects who choose to participate in CPET testing were included. After exclusion of subjects with missing data (n = 18), severe renal disease (estimated glomerular filtration rate [eGFR] < 30 ml/min) (n = 4), chronic lung disease (n = 68), bronchial asthma (n = 48), and chronic bronchitis (n = 122) a total of 3,500 subjects remained in the sample. Of these 1,752 were male (253 on statin medication) and 1,748 female (171 on statin medication).
Interview, medical and laboratory examination
All assessments were done according to standardized protocols. Study nurses were certified semi-annually. Trained and certified staff used standardized computer-assisted interviews to ask the subjects about their age, sex, smoking habits, and physical inactivity. Smoking habits were classified either as current smoker or non-smoker. Physical inactivity was defined as being physically active for less than one hour per week.
Medical history of the subjects (including previous myocardial infarction) was assessed using a computer-assisted interview questionnaire. Diabetes was defined based on the self-reported use of antidiabetic medication (anatomic, therapeutic, and chemical [ATC] code: A10) in the last 7 days or a glycosylated hemoglobin level > 6.5%. Blood pressure was assessed after a 5 min resting period in sitting position. Systolic and diastolic blood pressure measurements were taken three times, with three minutes rest in between, on the right arm using a digital blood pressure monitor (HEM-705CP, Omron Corporation, Tokyo, Japan). The second and third reading were averaged and used as blood pressure for the specific subject. Hypertensive patients were identified by either self-reported antihypertensive medication (antihypertensive medication [ATC C02], diuretics [ATC C03], vasodilators [ATC C04], beta blockers [ATC C07], calcium channel blockers [ATC C08], angiotensin-converting enzyme blockers [ATC C09A]) or blood pressure measurement (systolic blood pressure > 140 mmHg or diastolic blood pressure > 90 mmHg). Body mass index (BMI) was calculated as body weight (kg) / height (m)2. Statin (ATC C10AA) medication was assessed via questionnaire and scanning of a unique drug identifier (pharmaceutical central number, Pharmazentralnummer, PZN). Non-fasting blood samples were taken and serum levels of cholesterol (chol), and LDL cholesterol were assessed photometrically (Hitachi 704, Roche, Mannheim, Germany). The estimated glomerular filtration rate (eGFR) was calculated according to Stevens et al. [13]: eGFR = 186 x (plasma creatinine concentration x 0.0113118)-1.154 x age-0.203; multiplied by 0.742 for female subjects [mL/min/1.73 m2].
Exercise testing
Exercise capacity was assessed with a cycle ergometer (Ergoselect 100, Ergoline, Bitz, Germany) using a modified Jones protocol [14]. Briefly, 3 min of rest were followed by 1 min of unloaded cycling (20 Watts) at ~60 rpm. Thereafter, the workload was increased by 16 W every minute. Even though, subjects were encouraged to reach maximal exhaustion before, no encouragement was provided during the test. Exercise testing was stopped by the subject due to exhaustion or by the attending physician due to chest pain and/or ECG abnormalities. Twelve lead ECG was recorded during rest and every minute thereafter. Peak heart rate was determined based on the highest 10 s average during late exercise or early recovery.
Gas exchange variables
During exercise testing tidal volume (VE), oxygen consumption (VO2), and carbon dioxide consumption (VCO2) were assessed on a breath-by-breath basis using an Oxycon Pro with a Rudolf’s mask (JÄGER/VIASYS Healthcare System, Hoechberg, Germany) and averaged over 10 s intervals. Pulse oximetry was monitored continuously. Maximal oxygen consumption (VO2peak) was defined as the highest 10 s average of VO2 during late exercise or early recovery. Oxygen consumption at the aerobic threshold (VO2@AT) was determined by the V-slope method as described previously [15]. Peak oxygen pulse (O2HRmax) was calculated as VO2peak divided by peak heart rate.
Statistics
For sample baseline characteristics continuous data are expressed as median and 25th/75th quantile. Nominal data are expressed as frequency and percentage. A directed acyclic graph was used to determine potential confounding and appropriately adjust for age, sex, previous myocardial infarction, physical inactivity and a potential statin*sex interaction (S1 Fig) [16,17]. In addition, a clinical model which adjusted for age, sex, previous MI, physical inactivity, eGFR, BMI, smoking, hypertension and diabetes was calculated. All associations with O2HRmax were further adjusted for beta blocker usage. The statin sex interaction term in the linear regression model was significant (p < .0001). Therefore, further analyses were stratified by sex. The Wilcoxon-Mann-Whitney-Test was used for descriptive continuous variables and Chi-square for nominal variables. Sex specific linear regression model were used to assess the association between statin usage and VO2peak, VO2@AT and O2HRmax. Normality of residuals and homoscedasticity was visually checked using histograms, Q-Q plots, and residuals-vs-fitted plots. In addition, a quantile regression analysis in 5 percentile steps from the 5th to the 95th quantile was calculated. Further, as a sensitivity analysis a propensity score analysis was performed. Propensity scores based on sex, age, BMI, diabetes, hypertension, and previous myocardial infarction were calculated using a logistic regression [18]. A stringent caliper of 0.1 was used for a 1:1 matching of subjects taking statins and those who do not take statins. Thereafter, a two-sided paired t-test was used to compare VO2peak between statin-taking and non-taking subjects. All calculations were done in SAS 9.4 (SAS Institute, Cary, NC, USA) or STATA13.1 (Stata Corporation, College Station, TX, USA). All results are given as least-square means and 95%-confidence interval (CI) unless otherwise indicated. Bonferroni adjustment for multiple testing was used when appropriate for group comparisons. Significance was determined by P < .05.
Results
General characteristics
Descriptive statics of SHIP-1 and SHIP-T are provided in S1 Table and S2 Table. Of the 3,500 analyzed subjects in the merged data set a total of 1,752 were male (253 [14.4%] on statin medication) and 1,748 female (171 [9.8%] on statin medication) (Table 1). Study participants taking statins were significantly older, smoked less, and had higher BMI, more often hypertension as well as diabetes mellitus. Further, median plasma LDL and cholesterol concentrations were lower, while median TG concentration was higher in statin compared to non-statin taking subjects. Values for VO2peak, VO2@AT and eGFR were lower in statins users. Also, subjects on statins were more likely to receive beta blockers, calcium-channel blockers and angiotensin-converting enzyme blockers. Interestingly, in males but not in females median diastolic blood pressure was lower in statin users compared to non-users. However, females on statins had significantly higher median systolic blood pressure compared to females without statins. No such difference was found in males. Median O2HRmax was significantly lower in males with statins compared to male subjects without this drug, while no difference was seen for females.
Table 1. Descriptive statistics.
| Males (n = 1,752) | Females (n = 1,748) | |||||
|---|---|---|---|---|---|---|
| Statin users (n = 253) |
Non-users (n = 1,499) |
P | Statin users (n = 171) |
Non-users (n = 1,577) |
P | |
| Age (years) | 66 (57; 72) | 50 (40; 61) | < .0001 | 65 (59; 71) | 50 (40; 60) | < .0001 |
| BMI (kg/m2) | 29.38 (26.97; 31.78) | 27.80 (25.30; 30.60) | < .0001 | 28.93 (26.29; 32.67) | 25.96 (23.08; 29.76) | < .0001 |
| Hypertension (%) | 87.7 | 49.4 | < .0001 | 74.3 | 33.3 | < .0001 |
| Myocardial infarction (%) | 21.3 | 1.4 | < .0001 | 4.1 | 0.4 | < .0001 |
| Diabetes mellitus (%) | 29.6 | 7.1 | < .0001 | 22.8 | 4.9 | < .0001 |
| Diastolic BP (mmHg) | 77 (71; 84) | 81 (75; 88) | < .0001 | 76 (70; 81) | 76 (70; 82) | 0.6744 |
| Systolic BP (mmHg) | 134 (124; 144) | 133 (123; 144) | 0.6503 | 127 (117; 139) | 120 (110; 132) | < .0001 |
| LDL (mmol/l) | 2.64 (2.18; 3.19) | 3.58 (2.98; 4.18) | < .0001 | 2.97 (2.55; 3.53) | 3.40 (2.79; 4.12) | < .0001 |
| TG (mmol/l) | 1.72 (1.21; 2.54) | 1.50 (1.01; 2.30) | 0.002 | 1.47 (1.11; 1.96) | 1.18 (0.84; 1.68) | < .0001 |
| Chol (mmol/l) | 4.50 (3.90; 5.20) | 5.60 (4.80; 6.30) | < .0001 | 5.20 (4.60; 5.80) | 5.60 (4.90; 6.31) | < .0001 |
| Smoking (%) | 14.2 | 25.2 | 9.9 | 22.7 | ||
| VO2max (ml/min) | 1922 (1573; 2237) | 2450 (2062; 2868) | < .0001 | 1400 (1159; 1600) | 1600 (1366; 1870) | < .0001 |
| VO2@AT (ml/min) | 1050 (850; 1200) | 1200 (1000; 1400) | < .0001 | 800 (700; 950) | 900 (800; 1000) | < .0001 |
| O2HRmax (ml/beat) | 14.6 (12.8; 16.7) | 15.7 (13.8; 17.9) | < .0001 | 10.7 (9.5; 12.2) | 10.5 (9.3; 12.0) | 0.2635 |
| Beta Blocker (%) | 60.1 | 16.3 | < .0001 | 53.8 | 18.7 | < .0001 |
| Calcium Channel Blockers (%) | 17 | 3.3 | < .0001 | 7.6 | 2.4 | < .0001 |
| Angiotensin-converting enzyme blockers (%) | 47 | 10.5 | < .0001 | 25.7 | 7.2 | < .0001 |
| Physical inactivity (%) | 41.9 | 38.4 | 0.2952 | 32.7 | 35.38 | 0.4932 |
| eGFR | 79.5 (67.4; 90.7) | 89.46 (78.5; 101.8) | < .0001 | 75.1 (64.1; 85.6) | 85.2 (74.1; 99.6) | < .0001 |
The association between statin medication and VO2peak
Since a significant sex–statin interaction was observed in the initial linear regression model all further group comparisons were stratified by sex (p < .001) (S3 Table). Results for the individual studies (SHIP-1 and SHIP-T) are provided in S4 and S5 Tables. In model 1 statin medication was inversely associated with VO2peak in males (no statin: 2,337; 95%-confidence interval [CI]: 2,287–2,386 vs. statin: 2,091; 95%-CI: 2,032–2,150 ml/min; P < .0001) but not females (no statin: 1,467; 95%-CI: 1,417–1,517 vs. statin: 1,503: 95%-CI: 1,426–1,579 ml/min; P = 1.00). Model 2 showed similar results (male no statin: 2,268; 95%-CI: 2,214–2,321 vs. male statin: 2,035; 95%-CI: 1,975–2,096 ml/min; P < .0001; female no statin: 1,388; 95%-CI: 1,334–1,443 vs. female statin: 1,434; 95%-CI: 1,356–1,511 ml/min; P = 1.00).
Quantile regression analysis revealed a consistent effect throughout the range of observed values for both sexes. Specifically, statin usage was associated with a significantly reduced VO2peak for all observed values between the 5th and the 95th percentile in males. Quantile regression analysis also confirmed that statin usage was not associated with reduced VO2peak in females for the range of observed values (Fig 1).
Fig 1.
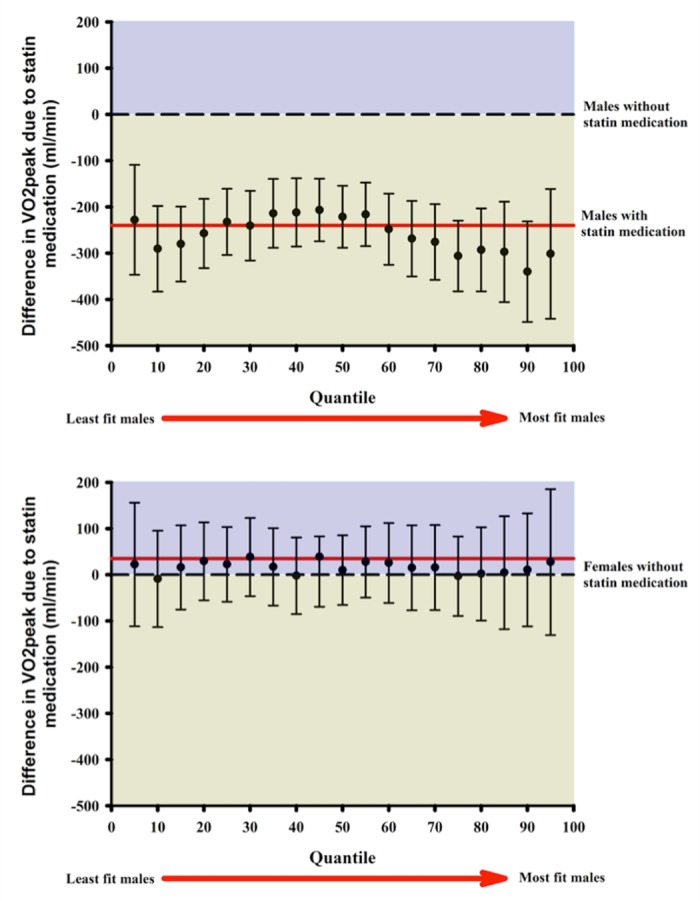
Association between statin medication with VO2peak for males (A) and females (B). The dashed line indicates a β-coefficient of “0”, which means that there are no significant differences in VO2peak between statin users and non-users. The red line is representative of the overall β (i.e. the observed difference in VO2peak between statin users and non-users). The quantiles on the x-axis are representative of exercise capacity. Subjects with the lowest VO2peak are on the left and while the one with highest exercise capacity are on the right. Statin medication was associated with a significantly reduced VO2peak in male between the 5th and 95th quantiles. For females no significant differences were observed.
The association between statin medication and VO2@AT
Statin medication was associated with reduced VO2@AT in males (no statin: 1,172; 95%-CI: 1,142–1,202 vs. statin: 1,111; 95%-CI: 1,075–1,147 ml/min; P = .0061) but not females (no statin: 854; 95%-CI: 824–885 vs. statin 864; 95%-CI: 817–911 ml/min; P = 1.00). In Model 2 a significantly lower VO2@AT was seen in statin taking males (no statin: 1,153; 95%-CI: 1,120–1,186 vs. statin: 1,089; 95%-CI: 1,051–1,126 ml/min; P = .0032) but not females (no statin: 835; 95%-CI: 801–868 vs. statin: 840; 95%-CI: 792–888 ml/min; P = 1.00).
Interaction between physical inactivity with statin medication
In order to investigate whether differences in physical activity may be responsible for our results we explored the three-way interaction between physical inactivity, statins, and sex. This interaction revealed to be significant in model 1 (P < .0001) and model 2 (P < .0001). Thus, a post-hoc analysis between groups adjusted for multiple testing was conducted. In model 1 physically active non-statin taking males (inactive: 2,236 95%-CI: 2,180–2,291 vs. active: 2,440 95%-CI: 2,389–2,493 ml/min; P < .0001) and females (inactive: 1,407 95%-CI: 1,351–1,464 vs. active: 1,549 95%-CI: 1,497–1,601 ml/min; P < .0001) had significantly higher VO2peak compared to their inactive counterparts. In statin taking males (inactive: 2,061 95%-CI: 1,977–2,146 ml/min vs. active: 2,171 95%-CI: 2,098–2,245 ml/min; P = 0.9776) and females (inactive: 1,528 95%-CI: 1,412–1,644 ml/min vs. active: 1,563 95%-CI: 1452–1627 ml/min; P = 1.0) no significant difference was observed due to physical activity. The results for model 2 were similar. Specifically, physically active males (inactive– 2,171 95%-CI: 2,112–2,230 ml/min vs. active– 2,367 95%-CI: 2,311–2,424 ml/min; P < .0001) and females (inactive– 1,345 95%-CI: 1,285–1,405 ml/min vs. active– 1,468 95%-CI: 1,410–1,525 ml/min; < .0001) had significantly higher VO2peak compared to inactive individuals. For statin taking males (inactive– 2,015 95%-CI: 1,930–2,100 ml/min vs. active– 2,102 95%CI: 2,028–2,176 ml/min; P = 1.00) and females (inactive– 1,465 95%CI: 1,350–1,580 ml/min vs. active– 1,489 95%-CI: 1,399–1,579 ml/min; P = 1.00) physically activity had no effect on VO2peak.
The association between statin medication and O2HRmax
In model 1 statin medication was associated with a significantly reduced O2HRmax in males (no statin: 15.5; 95%-CI: 15.2–15.8 vs. statin: 14.6; 95%-CI: 14.2–15.0 ml/beat; P < .0001) but not females (no statin: 10.3; 95%-CI: 9.9–10.6 vs. statin: 10.5; 95%-CI: 10.0–11.0 ml/beat; P = 1.00). Model 2 also showed that for males (no statin: 15.5; 95%-CI: 15.2–15.9 vs. statin: 14.5; 95%-CI: 14.1–14.9 ml/beat; P < .0001) but not females (no statin: 10.3; 95%-CI: 9.9–10.6 vs. statin: 10.5; 95%-CI: 10.0–11.0 ml/beat; P = 1.00) statin usage was inversely associated with O2HRmax.
The association between cardiopulmonary exercise capacity and lipids
Circulating LDL and cholesterol concentration was inversely associated with VO2peak in men (LDL: -33.51 95%-CI: -59.26 –-7.75 ml/mmol/l; P = 0.0108 and cholesterol: -27.29 95%-CI: -48.64–-5.93 ml/mmol/l; P = 0.0123) but not women (LDL: -14.65 95%-CI: -31.65–2.35; P = 0.0911 and cholesterol: 14.76 95%-CI: -29-8–0.25; P = 0.054).
Sensitivity analysis using propensity scores
In our sample a total of 253 male subjects took statins. A total of 229 individuals were matched according to their likelihood to receive a statin. The discrepancy between the 253 males in the cohort and 232 matched is likely due to the stringent matching caliper of 0.1. According to this approach, male subjects on statin medication had significantly lower VO2peak compared to subjects without this medication by 110.5 ml/min (95%-CI: 31.0–111.0 ml/min; P < .001). All 171 female subjects taking statins could be matched to controls. No significant difference between groups was found (mean difference 28.4; 95%-CI: -87.6–30.8 ml/min; P = .34). Therefore, the propensity score analysis confirmed our findings.
Discussion
Statins and exercise are life-saving therapeutics with systemic pleiotropic effects. This investigation explored a potential association between statins and cardiopulmonary exercise testing capacity in two independent cross-sectional population-based cohorts from Northeast Germany. We report that statin usage was inversely related with VO2peak and VO2@AT in males but not females. Male statin users had significantly lower VO2peak between the 5th and 95th percentile. In females no association of statins with VO2peak and VO2@AT was observed throughout the range of observed values. In line with these findings, statin medication was also associated with reduced oxygen pulse in males but not females. In addition, the results of the investigated three-way interaction between sex, physical inactivity, and statin medication indicate that the relation between statins and reduced VO2peak was dependent on sex but independent of physical activity. This is in contrast to previous findings which reported that physical activity decreased in elderly men after initiation of statin treatment [19].
Maximal oxygen consumption is a very well established predictor for mortality in healthy populations [20] and in patients with coronary heart disease [21]. The positive outcomes of participating in structured exercise programs for patients who experienced acute cardiovascular events are well established [22,23]. Also, patients with heart failure [24] and coronary heart disease [25], who receive statins, cannot just safely participate in endurance and interval training protocols, but also increase their cardiopulmonary exercise capacity. However, some previous studies suggest that statins may also worsen cardiac function. In a very small trial, 14 patients without previous myocardial function and heart failure were given 20 mg of atorvastatin per day [26]. A total of 10 patients showed a worsening of diastolic ventricular function (e.g. 10% decrease in the E/A ratio, a 10% increase in E-wave DT, or a 10% increase in IVRT). The authors of the trial reported that affected patients had very low coenzyme Q10 which can be further reduced by statins [27]. In line with this, a very recent clinical trial with 420 heart failure patients reported that coenzyme Q10 supplementation significantly reduced major adverse cardiovascular events [28].
Statins are also recommended for subjects without cardiovascular disease but who have an increased risk for CVD [29,30]. The separate efficacy of either exercise or statins in primary CVD prevention has been well established [31,32]. To demonstrate the suitability of statins for subjects without cardiovascular disease, previous studies have reported that statins did not decrease VO2peak [33]. However, these results have to be taken with caution since they are based on a small sample size of 28. Also, large epidemiological studies reported an additive effect of statins and physical activity on mortality reduction in dyslipidaemic and hypertensive individuals [34,35]. Interestingly, Kokkinos et al. reported that the fittest study participants had the lowest risk of mortality independent of statin usage [34]. However, while in secondary disease prevention, subjects were able to increase their VO2peak with exercise training; this may not be the case in primary prevention. Mikus et al. recently showed that statins impaired the beneficial effects of a twelve week supervised aerobic endurance exercise training protocol in obese subjects [10]. Their investigation was the first to compare two exercise groups to assess the additional effect of statins on top of exercise on trainability. Statins inhibited an increase in VO2peak. We report that in males from a general population cohort current statin usage was associated with significantly lower VO2peak independent of age, previous myocardial infarction, physical activity behavior, BMI, diabetes, hypertension, beta blocker usage, calcium channel blockers, and angiotensin converting enzyme blockers. Further research is warranted to understand which subjects benefit most from statins and/or exercise.
In addition to lower VO2peak, statin usage was related with lower VO2@AT in males, but not females. In contrast to our data, a human trial which investigated cardiopulmonary exercise capacity in patients with statin induced myotoxicity reported that the aerobic threshold was not impacted by statin medication in their control group [36]. The authors speculated that an increased resting respiratory exchange ratio due to statins may impair the lipid metabolism during exercise. Our findings point to a more nuanced interpretation, since our results suggest sex specific relation of statins with cardiopulmonary exercise capacity. Nonetheless, we acknowledge that our results are based on observational data and not based on a randomized controlled trial (RCT). Hence, our results are subject to bias and confounding. Overall, these effects deserve further research.
Several studies have explored the impact of statins on physical fitness and activity [10,19,34,37–44]. However, these investigations are very heterogeneous in terms of participants and experimental design. For example, Sinzinger and O’Grady examined the impact of statins on muscle pain in elite athletes with familial hypercholesterolemia. They reported that merely 20% tolerated statin treatment without reporting any adverse effects [37]. Contrarily, in healthy individuals with increased LDL concentration, simvastatin treatment for 12 weeks was not associated with decreases in cardiopulmonary exercise capacity and muscle function [38]. In a large observational study with 1,201 patients undergoing cardiac rehabilitation significant improvements in VO2peak were reported for statin users and non-users alike [40]. In a large very recent epidemiological study Williams and Thompson investigated the role of statins in more than 60,000 runners and walkers [44]. Statins did not influence exercise activity or duration in individuals who developed hypercholesterolemia. Lastly, in the The Henry Ford Exercise Testing (FIT) Project statin usage was not associated with decreased VO2peak in males or females [42]. These data suggest that statins may not adversely influence physical activity and capacity.
The sex specific results of our analysis are of particular interest. Even though, we acknowledge that our population-based approach is observational, it is well established that statin therapy increases the risk for skeletal muscle myopathy. This side effect primarily impacts glycolytic type II muscle and not oxidative type I fibers [45,46]. Since women have more type I fibers compared to men [47], males may be at a higher risk to experience statin induced muscle damage. Interestingly, previous experimental evidence demonstrated higher rates of statin induced muscle problems in women [48]. A second possible explanation is that lipophilic statins (i.e. lovastatin, simvastatin, fluvastatin, atorvastatin, and pivastatin) are metabolized in first-pass in the liver through the hepatic cytochrome enzyme system [49]. The enzyme responsible for this reaction is cytochrome P450 3A4 (CYP3A4). Women have been found to have higher concentrations of CYP3A4 [50,51]. Hence, females may be able to metabolize statins more quickly and thus reduce their efficacy. The third possible reason as to why a sex-specific association was observed in our investigation may be due to the difference in O2HRmax. While statin taking males had lower O2HRmax compared to non-users, female statin takers and non-takers had similar O2HRmax. Since O2HRmax is strongly related with left ventricular ejection fraction (LVEF), the inverse association between statin usage and VO2peak in males may be a result of lower LVEF which was not evident in female statin users. A reduced LVEF in male statin users may be partly responsible for their lower cardiopulmonary exercise capacity. Overall, at least three explanations (e.g. effect of statins on type I skeletal muscle fibers, sex-specific CYP3A4 concentration and/or differences in O2HRmax) for the observed sex-specific associations between statins and CPET parameters are likely. Nonetheless, we are currently unable to unequivocally determine the underlying reason for our observations.
Our findings are in contrast to previous observations that reported an increased incidence of statin adverse effects in women compared to men [48]. Further, in a randomized controlled trial (RCT) women receiving statins experienced more fatigue compared to men [52]. These observed side effects of statins were related to alterations in mitochondrial function [48]. Since mitochondrial function is associated with cardiopulmonary exercise capacity [53], one would propose that statins show an inverse association with VO2peak. One may speculate the different results are due to the fact that we analyzed data from a general populated based cohort while the above mentioned RCT recruited subjects from a primary prevention population without overt cardiovascular disease or diabetes.
One of the reasons for the statin treatment in our population was most likely increased circulating LDL and cholesterol. Altered lipid metabolism is an early hallmark of subclinical cardiovascular disease and may therefore influence cardiopulmonary exercise capacity. We assessed the association between circulating LDL and cholesterol with VO2peak in subjects not taking statin medication. We report an inverse association between VO2peak to LDL and cholesterol in males but not females. Interestingly, the parameter estimate for LDL points to an inverse association for both sexes. This agrees with the common thought that increased LDL is associated with subclinical CVD and therefore reduced cardiopulmonary exercise capacity. However, the parameter estimate for the association between VO2peak and cholesterol is inverse for males but positive for females. Future analyses need to verify this finding as it may just be a result of chance.
We acknowledge that based on the cross-sectional analysis of observational data we cannot conclusively determine the direction of the investigated associations. Further, the cross sectional design only allows for the comparison of current statin users and non-users. Since CPET was voluntary in our cohort, a potential bias may have been introduced due to more fit individuals selecting to participate in this test. Nonetheless, the strength of our study is the population-based design. This may allow drawing inferences for the general population from our results. However, we are aware that only a small number of participants took statins, which in turn may be a realistic assumption about the general population. In addition, we employed a highly standardized quality control during the course of the study. Lastly, we recognize our analysis would benefit from information regarding the duration and dose of statin treatment as well as possible muscle symptoms. Unfortunately this data is not available for our cohorts. Our findings may be influenced by residual confounding since we included variables which are strongly predictive of cardiopulmonary exercise capacity and have a large degree of variability. Most importantly we were unable to adjust to lipid levels prior to statin treatment.
One may argue that the observed associations between VO2peak and VO2@AT with present statin medication are the result of an observational bias due to comparing healthy with sick sub-populations. To investigate whether this was the case, we used propensity scores in a sensitivity analysis as a method to overcome this potential shortcoming. The propensity scores were calculated using a logistic regression adjusted for age, sex, BMI, diabetes, hypertension, previous myocardial infarction and usage of beta-blockers, calcium channel blockers, and angiotensin-converting enzyme blockers. Thereafter, we matched subjects with and without statins according to a very stringent caliper of 0.1. This means that the difference in propensity scores has to be less than 0.1. This method is more rigorous than using nearest neighbor matching which is exemplified by the fact that we were unable to match all statin taking subjects. A paired t-test between matched male subject pairs demonstrated that statin users had significantly lower VO2peak and VO2@AT compared to non-users. No significant difference was observed for females. Therefore, the propensity score analysis confirmed the results of the regression analysis.
Conclusion
We report that present statin medication was related with impaired cardiopulmonary exercise capacity in male but not female subjects in a cross-sectional population based study from northeast Germany. Based on previous research, statins may inhibit increases in VO2peak due to exercise training in primary, but not secondary disease prevention. Therefore, whether subjects in primary cardiovascular prevention aiming to increase their cardiopulmonary exercise capacity should take this medication deserves further research. Future research should use a randomized design to test whether our observational results can be confirmed to assess whether exercise and not drug usage is more suitable as a first frontier in primary disease prevention.
Supporting information
Variables in red are included into the model while variables in blue are considered mediators.
(JPG)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
The authors acknowledge and greatly appreciate the work of all study nurses and technicians who helped collect data for the SHIP study. Further, the authors thank all SHIP participants for their contribution to science by participating in the study.
Data Availability
The informed consent given by SHIP study participants does not cover data posting in public databases. However, data are available upon request from SHIP (http://community-medicine.de) by means of a project agreement. Data can be applied for online and are subject to approval by the Steering Committee of the Research Network for Community Medicine. Interested researchers may contact Prof. Matthias Nauck (matthias.nauck@uni-greifswald.de) and Prof. Thomas Kohlmann (icm-mcm@uni-greifswald.de) with queries related to data access.
Funding Statement
SHIP is part of the Community Medicine of the University of Greifswald, which is funded by grants from the German Federal Ministry of Education and Research for SHIP (BMBF, grant 01ZZ96030, 01ZZ0701) and German Asthma and COPD Network (COSYCONET; BMBF grant 01GI0883); the Ministry for Education, Research, and Cultural Affairs; and the Ministry for Social Affairs of the Federal State of Mecklenburg–West Pomerania. There are no relationships with industry.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. (2014) Executive summary: heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 129: 399–410. doi: 10.1161/01.cir.0000442015.53336.12 [DOI] [PubMed] [Google Scholar]
- 2.Davignon J (2004) Beneficial Cardiovascular Pleiotropic Effects of Statins. Circulation 109: III-39–III-43. [DOI] [PubMed] [Google Scholar]
- 3.Pedersen TR, Olsson AG, Faergeman O, Kjekshus J, Wedel H, Berg K, et al. (2004) Lipoprotein changes and reduction in the incidence of major coronary heart disease events in the Scandinavian Simvastatin Survival Study (4S). 1998. Atheroscler Suppl 5: 99–106. doi: 10.1016/j.atherosclerosissup.2004.08.030 [DOI] [PubMed] [Google Scholar]
- 4.Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, Lichtenstein AH, et al. (2010) Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation 122: 406–441. doi: 10.1161/CIR.0b013e3181e8edf1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bamman MM, Cooper DM, Booth FW, Chin ER, Neufer PD, Trappe S, et al. (2014) Exercise biology and medicine: innovative research to improve global health. Mayo Clin Proc 89: 148–153. doi: 10.1016/j.mayocp.2013.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whyte JJ, Laughlin MH (2010) The effects of acute and chronic exercise on the vasculature. Acta Physiol (Oxf) 199: 441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA (2011) The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol 11: 607–615. doi: 10.1038/nri3041 [DOI] [PubMed] [Google Scholar]
- 8.Sanchis-Gomar F, Fiuza-Luces C, Lucia A (2014) Exercise as the master polypill of the 21st century for the prevention of cardiovascular disease. International journal of cardiology. [DOI] [PubMed] [Google Scholar]
- 9.Ii M, Losordo DW (2007) Statins and the endothelium. Vascul Pharmacol 46: 1–9. doi: 10.1016/j.vph.2006.06.012 [DOI] [PubMed] [Google Scholar]
- 10.Mikus CR, Boyle LJ, Borengasser SJ, Oberlin DJ, Naples SP, Fletcher J, et al. (2013) Simvastatin impairs exercise training adaptations. J Am Coll Cardiol 62: 709–714. doi: 10.1016/j.jacc.2013.02.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.John U, Greiner B, Hensel E, Ludemann J, Piek M, Sauer S, et al. (2001) Study of Health In Pomerania (SHIP): a health examination survey in an east German region: objectives and design. Soz Praventivmed 46: 186–194. [DOI] [PubMed] [Google Scholar]
- 12.Volzke H, Alte D, Schmidt CO, Radke D, Lorbeer R, Friedrich N, et al. (2011) Cohort profile: the study of health in Pomerania. Int J Epidemiol 40: 294–307. doi: 10.1093/ije/dyp394 [DOI] [PubMed] [Google Scholar]
- 13.Stevens LA, Coresh J, Greene T, Levey AS (2006) Assessing kidney function—measured and estimated glomerular filtration rate. N Engl J Med 354: 2473–2483. doi: 10.1056/NEJMra054415 [DOI] [PubMed] [Google Scholar]
- 14.Jones NL, Makrides L, Hitchcock C, Chypchar T, McCartney N (1985) Normal standards for an incremental progressive cycle ergometer test. Am Rev Respir Dis 131: 700–708. doi: 10.1164/arrd.1985.131.5.700 [DOI] [PubMed] [Google Scholar]
- 15.Wasserman K (2005) Principles of Exercise Testing and Interpretation: Including Pathophysiology and Clinical Applications: Lippincott Williams & Wilkins. [Google Scholar]
- 16.Textor J, Hardt J, Knuppel S (2011) DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology 22: 745. [DOI] [PubMed] [Google Scholar]
- 17.Greenland S, Pearl J, Robins JM (1999) Causal diagrams for epidemiologic research. Epidemiology 10: 37–48. [PubMed] [Google Scholar]
- 18.Lanehart RE, de Gil PR, Kim ES, Bellara AP, Kromrey JD, Lee RS. Propensity score analysis and assessment of propensity score approaches using SAS procedures; 2012.
- 19.Lee DS, Markwardt S, Goeres L, Lee CG, Eckstrom E, Williams C, et al. (2014) Statins and physical activity in older men: the osteoporotic fractures in men study. JAMA Intern Med 174: 1263–1270. doi: 10.1001/jamainternmed.2014.2266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kodama S, Saito K, Tanaka S, et al. (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 301: 2024–2035. doi: 10.1001/jama.2009.681 [DOI] [PubMed] [Google Scholar]
- 21.Keteyian SJ, Brawner CA, Savage PD, Ehrman JK, Schairer J, Divine G, et al. (2008) Peak aerobic capacity predicts prognosis in patients with coronary heart disease. Am Heart J 156: 292–300. doi: 10.1016/j.ahj.2008.03.017 [DOI] [PubMed] [Google Scholar]
- 22.Flynn KE, Pina IL, Whellan DJ, Lin L, Blumenthal JA, Ellis SJ, et al. (2009) Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301: 1451–1459. doi: 10.1001/jama.2009.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.West RR, Jones DA, Henderson AH (2012) Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart 98: 637–644. doi: 10.1136/heartjnl-2011-300302 [DOI] [PubMed] [Google Scholar]
- 24.Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, et al. (2007) Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 115: 3086–3094. doi: 10.1161/CIRCULATIONAHA.106.675041 [DOI] [PubMed] [Google Scholar]
- 25.Conraads VM, Pattyn N, De Maeyer C, Beckers PJ, Coeckelberghs E, Cornelissen VA, et al. (2015) Aerobic interval training and continuous training equally improve aerobic exercise capacity in patients with coronary artery disease: the SAINTEX-CAD study. Int J Cardiol 179: 203–210. doi: 10.1016/j.ijcard.2014.10.155 [DOI] [PubMed] [Google Scholar]
- 26.Silver MA, Langsjoen PH, Szabo S, Patil H, Zelinger A (2004) Effect of atorvastatin on left ventricular diastolic function and ability of coenzyme Q10 to reverse that dysfunction. Am J Cardiol 94: 1306–1310. doi: 10.1016/j.amjcard.2004.07.121 [DOI] [PubMed] [Google Scholar]
- 27.Mortensen SA, Leth A, Agner E, Rohde M (1997) Dose-related decrease of serum coenzyme Q10 during treatment with HMG-CoA reductase inhibitors. Mol Aspects Med 18 Suppl: S137–144. [DOI] [PubMed] [Google Scholar]
- 28.Mortensen SA, Rosenfeldt F, Kumar A, Dolliner P, Filipiak KJ, Pella D, et al. (2014) The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC Heart Fail 2: 641–649. doi: 10.1016/j.jchf.2014.06.008 [DOI] [PubMed] [Google Scholar]
- 29.Eckel RH, Jakicic JM, Ard JD, Miller NH, Hubbard VS, Nonas CA, et al. (2013) 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular RiskA Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. [DOI] [PubMed] [Google Scholar]
- 30.Fifth Joint Task Force of the European Society of C, European Association of E, European Association of Percutaneous Cardiovascular I, European Heart Rhythm A, Heart Failure A, European Association for Cardiovascular P, et al. (2012) European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): the Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur J Prev Cardiol 19: 585–667. doi: 10.1177/2047487312450228 [DOI] [PubMed] [Google Scholar]
- 31.Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, et al. (2013) Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 1: CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Green DJ, O'Driscoll G, Joyner MJ, Cable NT (2008) Exercise and cardiovascular risk reduction: time to update the rationale for exercise? J Appl Physiol 105: 766–768. doi: 10.1152/japplphysiol.01028.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chung J, Brass EP, Ulrich RG, Hiatt WR (2008) Effect of atorvastatin on energy expenditure and skeletal muscle oxidative metabolism at rest and during exercise. Clin Pharmacol Ther 83: 243–250. doi: 10.1038/sj.clpt.6100264 [DOI] [PubMed] [Google Scholar]
- 34.Kokkinos PF, Faselis C, Myers J, Panagiotakos D, Doumas M (2013) Interactive effects of fitness and statin treatment on mortality risk in veterans with dyslipidaemia: a cohort study. Lancet 381: 394–399. doi: 10.1016/S0140-6736(12)61426-3 [DOI] [PubMed] [Google Scholar]
- 35.Kokkinos P, Faselis C, Myers J, Kokkinos JP, Doumas M, Pittaras A, et al. (2014) Statin therapy, fitness, and mortality risk in middle-aged hypertensive male veterans. Am J Hypertens 27: 422–430. doi: 10.1093/ajh/hpt241 [DOI] [PubMed] [Google Scholar]
- 36.Phillips PS, Phillips CT, Sullivan MJ, Naviaux RK, Haas RH (2004) Statin myotoxicity is associated with changes in the cardiopulmonary function. Atherosclerosis 177: 183–188. doi: 10.1016/j.atherosclerosis.2004.06.014 [DOI] [PubMed] [Google Scholar]
- 37.Sinzinger H, O'Grady J (2004) Professional athletes suffering from familial hypercholesterolaemia rarely tolerate statin treatment because of muscular problems. Br J Clin Pharmacol 57: 525–528. doi: 10.1111/j.1365-2125.2004.02044.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Traustadottir T, Stock AA, Harman SM (2008) High-dose statin use does not impair aerobic capacity or skeletal muscle function in older adults. Age (Dordr) 30: 283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parker BA, Capizzi JA, Grimaldi AS, Clarkson PM, Cole SM, Keadle J, et al. (2013) Effect of statins on skeletal muscle function. Circulation 127: 96–103. doi: 10.1161/CIRCULATIONAHA.112.136101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rengo JL, Savage PD, Toth MJ, Ades PA (2014) Statin therapy does not attenuate exercise training response in cardiac rehabilitation. J Am Coll Cardiol 63: 2050–2051. doi: 10.1016/j.jacc.2014.02.554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Terpak K, Guthrie S, Erickson S (2015) Statin use and self-reported swimming performance in US masters swimmers. J Sports Sci 33: 286–292. doi: 10.1080/02640414.2014.942688 [DOI] [PubMed] [Google Scholar]
- 42.Qureshi WT, Keteyian SJ, Brawner CA, Dardari Z, Blaha MJ, Al-Mallah MH (2015) Impact of statin use on cardiorespiratory fitness in multi-racial men and women: The Henry Ford Exercise Testing (FIT) Project. Int J Cardiol 197: 76–77. doi: 10.1016/j.ijcard.2015.06.047 [DOI] [PubMed] [Google Scholar]
- 43.Panza GA, Taylor BA, Dada MR, Thompson PD (2015) Changes in muscle strength in individuals with statin-induced myopathy: A summary of 3 investigations. J Clin Lipidol 9: 351–356. doi: 10.1016/j.jacl.2015.01.004 [DOI] [PubMed] [Google Scholar]
- 44.Williams PT, Thompson PD (2015) Effects of Statin Therapy on Exercise Levels in Participants in the National Runners' and Walkers' Health Study. Mayo Clin Proc 90: 1338–1347. doi: 10.1016/j.mayocp.2015.06.019 [DOI] [PubMed] [Google Scholar]
- 45.Keller-Pinter A, Murlasits Z, Szucs G, Menesi D, Puskas L, Ferdinandy P, et al. (2011) P5.68 Upregulation of squalene synthase in type IIB fibers is an early response for statin treatment. Neuromuscular Disorders 21: 744–745. [Google Scholar]
- 46.Westwood FR, Bigley A, Randall K, Marsden AM, Scott RC (2005) Statin-induced muscle necrosis in the rat: distribution, development, and fibre selectivity. Toxicol Pathol 33: 246–257. doi: 10.1080/01926230590908213 [DOI] [PubMed] [Google Scholar]
- 47.Lundsgaard AM, Kiens B (2014) Gender differences in skeletal muscle substrate metabolism—molecular mechanisms and insulin sensitivity. Front Endocrinol (Lausanne) 5: 195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Golomb BA, Evans MA (2008) Statin adverse effects: a review of the literature and evidence for a mitochondrial mechanism. Am J Cardiovasc Drugs 8: 373–418. doi: 10.2165/0129784-200808060-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bhardwaj S, Selvarajah S, Schneider EB (2013) Muscular effects of statins in the elderly female: a review. Clin Interv Aging 8: 47–59. doi: 10.2147/CIA.S29686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sica DA, Gehr TW (2002) Rhabdomyolysis and statin therapy: relevance to the elderly. Am J Geriatr Cardiol 11: 48–55. [DOI] [PubMed] [Google Scholar]
- 51.Wolbold R, Klein K, Burk O, Nüssler AK, Neuhaus P, Eichelbaum M, et al. (2003) Sex is a major determinant of CYP3A4 expression in human liver. Hepatology 38: 978–988. doi: 10.1053/jhep.2003.50393 [DOI] [PubMed] [Google Scholar]
- 52.Golomb BA, Evans MA, Dimsdale JE, White HL (2012) Effects of statins on energy and fatigue with exertion: results from a randomized controlled trial. Arch Intern Med 172: 1180–1182. doi: 10.1001/archinternmed.2012.2171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Terjung RL, Zarzeczny R, Yang HT (2002) Muscle blood flow and mitochondrial function: influence of aging. Int J Sport Nutr Exerc Metab 12: 368–378. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Variables in red are included into the model while variables in blue are considered mediators.
(JPG)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
The informed consent given by SHIP study participants does not cover data posting in public databases. However, data are available upon request from SHIP (http://community-medicine.de) by means of a project agreement. Data can be applied for online and are subject to approval by the Steering Committee of the Research Network for Community Medicine. Interested researchers may contact Prof. Matthias Nauck (matthias.nauck@uni-greifswald.de) and Prof. Thomas Kohlmann (icm-mcm@uni-greifswald.de) with queries related to data access.


