Abstract
Embolic events from infective endocarditis can cause acute coronary syndrome. Mortality rate is high and optimal management might be different from those chosen in setting of classic atherosclerotic coronary artery disease. We present a case of 56-year-old male who had received 5 weeks of antibiotics for aortic valve endocarditis and developed acute ST segment elevation myocardial infarction in hospital settings. Interestingly, patient had recent left heart catheterization that was normal. This was recognized as embolic event from sterile vegetation. Patient was managed with balloon angioplasty and placement of intracoronary stent. Following re-vascularization, patient chest pain and electrocardiogram normalized and he improved in short term. However due to multiple comorbidities he had to be intubated and placed on dialysis.
Key words: Endocarditis, myocardial infacrtion, stent
Competing interest statement
Conflict of interest: the authors declare no potential conflict of interest.
Introduction
Systemic embolization is common complication that usually occurs in patient with left sided endocarditis. These emboli can involve virtually any organ system in body with the most common being cerebral circulation. Coronary artery embolization is well known complication of infective endocarditis that can rarely present with transmural myocarditis infarction. This can happen as initial clinical presentation or even many weeks after treatment with antimicrobial therapy. Therefore, endocarditis should be kept as potential cause of ST segment myocardial infarction in these settings.
Case Report
A 56-year-old African American male with history of prostate cancer had undergone open prostatectomy at an outlying hospital, which was followed by a complicated recovery due to wound dehiscence that ultimately led to Enterococcal bacteremia and endocarditis. He was started on intravenous gentamicin and ampicillin for 4 weeks while inpatient and then discharged to community nursing home to finish his course of antibiotics. One week later he presented to our tertiary care center with generalized weakness and recurrent falls. Vital signs on admission were blood pressure of 149/78 mmHg, respiratory rate 17/min, pulse 99 bpm, SaO2 95% on room air. Physical exam showed expiratory wheezing but otherwise unremarkable. Labs were significant for BUN 41 mg/dL, Cr 5.22 mg/dL, Na 136 meq/L, K 4.3 meq/L, troponin 0.03 ng/mL, WBC count was 14,000/mm3, Hb 8.4 g/dL, PLT 505/mm3. His baseline creatinine was normal. He was found to be in non-oliguric acute kidney injury likely secondary to gentamicin, so ampicillin and gentamicin were discontinued and patient was started on daptomycin. Electrocardiogram (ECG) showed normal sinus rhythm without any ST-T wave changes. A transthoracic echo was obtained on which echogenic mass was visualized on aortic valve leaflets measuring 1.99x1.67 cm with moderate aortic regurgitation (Figure 1). Cardiothoracic surgery was consulted, they recommended aortic valve repair once renal function normalized. Three days later patient started to complain of left sided chest pain radiating down the left arm and left jaw. Stat ECG was obtained that showed ST segment elevation in I, aVL and V3-V6 leads consistent with anterolateral STEMI (Figure 2). Emergent coronary angiogram showed 99% left anterior descending artery occlusion (Figure 3). Due to the presence of persistent symptoms and ECG changes, a bare metal stent was placed. This acute coronary event was thought to be an embolic —phenomenon given the fact that he had just had a normal coronary angiogram 3 months prior. Unfortunately, patient's condition gradually deteriorated with worsening respiratory and renal function requiring mechanical ventilation and hemodialysis. Patient was on ventilator support for a few days. He continued dialysis through temporary dialysis catheter. His respiratory status improved gradually and he was extubated. Patient renal functions improved slowly as well and got discharged to rehabilitation facility He is being followed in cardiology office and continues to be stable.
Figure 1.
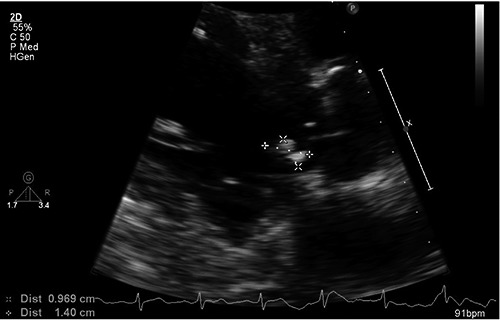
Parasternal long axis showing vegetation on ventricular side of aortic valve.
Figure 2.

Electrocardiogram showing ST segment elevation in lead V3-V6 and I, aVL.
Figure 3.
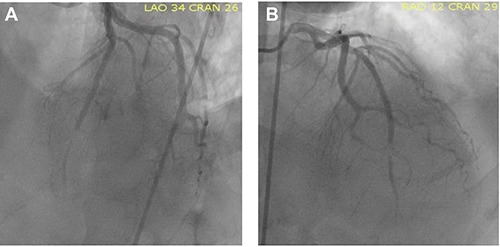
A and B) Coronary angiogram showing mid left anterior descending artery cut off lesion.
Discussion
Acute ST-segment elevation myocardial infarction (STEMI) is an uncommon complication of infective endocarditis with high mortality rate. In review of 154 patients over 6-year period from 1968-1973, coronary embolization was reported in 7% of patients with native valve endocarditis.1 In a Spanish series of 586 cases of infective endocarditis, acute coronary syndrome (ACS) was found in 14 cases (2.9%). Half of these patients with ACS had prosthetic valve endocarditis, 1.5% of cases of ACS occurred with native valves, and embolism was the cause in only 3 (0.51%) of 586 patients.2 In a Russian series 11 out of 104 (10.6%) had infarction as result of septic embolism.3 Mostly coronary embolization occurs in left anterior descending artery because the take off and downward course is more favorable for emboli to lodge compared to right coronary and left circumflex artery which have perpendicular take offs.4
The proposed mechanisms of myocardial infarction in patients with endocarditis include coronary embolization, complete occlusion of coronary ostia by vegetation on aortic cusp or extrinsic compression of coronaries from periannular abscesses and aneursyms. Occasionally in patients with underlying atherosclerotic coronary artery disease, insufficient coronary flow would lead to myocardial ischemia from decreased perfusion pressure even in the absence of full blown obstruction. Perriannular aortic complications and resultant coronary compression is the most common mechanism responsible for ACS that was found to be the cause in 8 out of 14 cases in series of 586 patients with infective endocarditis.2
The presence of aortic valve vegetation is an ongoing risk for future development of ACS. It depends upon the size of vegetation, its location and virulence of underlying organism involved. Depending upon those risk factors, ACS might be the initial manifestation of infection. Usually it occurs early during treatment of infective endocarditis but may occur even after finishing antibiotic treatment. Clinical presentation of patients with ACS in setting of infective endocarditis is like those seen in individuals with atherosclerotic coronary artery disease. Majority of cases present with anterior and anterolateral STEMI. Fulminant heart failure and cardiogenic shock might be seen in some cases because of severe left ventricular dysfunction.
Treatment of ACS in infective endocarditis is the unique therapeutic challenge. Many of these patients have emboli at other sites such brain, spleen and kidneys. Therefore, they are high risk for hemorrhagic complications and fatal outcomes with use of traditional antiplatlets, anticoagulants and fibrinolytics.5 Coronary angiography is relatively safer approach but there is always risk of fragmentation of vegetation by the catheter encountering vegetation on valve surface and resultant dislodgement in distal coronary circulation. Therefore, in patients who are hemodynamically stable and do not have active ongoing ischemia, surgical approach is the safest option. Perivalvular complications such as abscess, pseudoaneurysm and persistent vegetations >10 mm in setting of embolic episodes should be considered for urgent surgical evaluation.6
Percutaneous coronary intervention should not be considered the definitive therapeutic strategy. There is little evidence to support its use and benefits are questionable. Mycotic aneurysm can develop at the site of angioplasty and stenting with risk of ultimate coronary rupture and sudden death.7 The only indication might be persistent ongoing ischemia, large size infarct and hemodynamic instability in setting of STEMI. In patients in whom there is likelihood of complications of infective endocarditis particularly aortic valve endocarditis or prosthetic endocarditis, transesophageal echo should be done to evaluate for periannular complications. If these complications are found these patients should have surgical evaluation to allow drainage of abscess, debridement of necrotic tissue and possible valve replacement.8
In presently described case, patient developed anterior wall Myocardial infarction 5 weeks after starting antibiotics. Patient had left heart catheterization done 6 weeks before diagnosis of infective endocarditis that did not show any coronary artery disease. His 2-D echocardiogram clearly demonstrated aortic valve vegetation so we did not pursue transesophageal echocardiogram and he was being managed conservatively with outpatient antibiotics. Given his recent normal LHC, embolic occlusion of LAD from aortic valve vegetation was considered the mechanism responsible for MI.
In our case, patient has already been treated with iv antibiotics for 4 weeks and his repeat blood cultures were negative. Acute hemodynamic instability in setting of MI obviated the need for urgent coronary angiography. Balloon angioplasty alone was not successful to sustain patency at site of occlusion so we proceeded with placement of intracoronary stent. There have been five previously reported cases of embolic MI from infective endocarditis managed successfully with intracoronary stenting in acute settings. In four of these case, patient survived following PCI and outcomes were favorable.9-12 while in one case patient succumbed to death.11 Still there are no controlled studies proving superiority or safety of stenting over other intervention strategies. The decision to choose stenting should consider the risks of infection of stent material in bacteremia, formation of mycotic aneurysm, coronary rupture and sudden death.
Recently aspiration thrombectomy has been tried as an option both alone and in combination with stent implantation to provide complete resolution of stenosis.13 Risk of formation of mycotic aneurysm might reduced by aspiration of septic embolus prior to placement of stent. There is still possibility of subsequent appearance of aneurysm and these patients might need angiographic follow up.
Conclusions
The optimal management of myocardial infarction as a complication of infective endocarditis remains to be elucidated. Percutaneous coronary intervention might be considered in patient with large size infarct, electrical or hemodynamic instability and active ongoing ischemia who are too high risk for surgery in acute settings but it is not the definitive therapeutic strategy because of multiple risks involved. In patients who can be stabilized with conservative medical management, early valvular surgery may be the safest option. Optimal management must be decided on an individual patient basis, taking into consideration the risks of severe hemorrhage, embolic phenomena and the complications associated with percutaneous intervention. Large clinical trials comparing different interventional strategies for those who are likely to encounter this condition would be needed in future.
References
- 1.Garvey GJ, Neu HC. Infective endocarditis-an evolving disease: a review of endocarditis at The Columbia-Presbyterian Medical Center, 1968-1973. Medicine 1978;57:105-28. [PubMed] [Google Scholar]
- 2.Manzano MC, Vilacosta I, San Román JA, et al. Acute coronary syndrome in infective endocarditis. Rev Española Cardiol (English Edition) 2007;60:24-31. [PubMed] [Google Scholar]
- 3.Tiurin VP, Korneev NV. The mechanisms of the development and diagnosis of myocardial infarct in septic endocarditis. Terapevticheskii arkhiv 1991:64:55-8. [PubMed] [Google Scholar]
- 4.Prizel KR, Hutchins GM, Bulkley BH. Coronary artery embolism and myocardial infarction: a clinicopathologic study of 55 patients. Ann Intern Med 1978;88:155-61. [DOI] [PubMed] [Google Scholar]
- 5.Hunter AJ, Girard DE. Thrombolytics in infectious endocarditis associated myocardial infarction. J Emerg Med 2001;21:401-6. [DOI] [PubMed] [Google Scholar]
- 6.Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis. The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Giorn Ital Cardiol 2006;17:277. [DOI] [PubMed] [Google Scholar]
- 7.Serruys PW, De Jaegere P, Kiemeneij F, et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. N Engl J Med 1994;331: 489-95. [DOI] [PubMed] [Google Scholar]
- 8.Bayer AS, Bolger AF, Taubert KA, et al. Diagnosis and management of infective endocarditis and its complications. Circulation 1998;98:2936-48. [DOI] [PubMed] [Google Scholar]
- 9.Beldner S, Bajwa A, Kaplan B, et al. Septic coronary embolism. J Intervent Cardiol 2002;15:301-4. [DOI] [PubMed] [Google Scholar]
- 10.Glazier JJ, Mcginnity JG, Spears JR. Coronary embolism complicating aortic valve endocarditis: treatment with placement of an intracoronary stent. Clin Cardiol 1997;20:885-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ural E, Bildirici U, Kahraman G, Komsuoğlu B. Coronary embolism complicating aortic valve endocarditis: treatment with successful coronary angioplasty. Int J Cardiol 2007;119: 377-9. [DOI] [PubMed] [Google Scholar]
- 12.Hohmann D, Bertram H, Schieffer B, Wessel A. Acute myocardial infarction in a 16-year-old girl caused by infective endocarditis of a bicuspid aortic valve. Pediatr Cardiol 2011;32:534-5. [DOI] [PubMed] [Google Scholar]
- 13.Khan F, Khakoo R, Failinger C. Managing embolic myocardial infarction in infective endocarditis: current options. J Infect 2005;51:el01-5. [DOI] [PubMed] [Google Scholar]


