Abstract
Neighborhood characteristics such as racial composition and social capital have been widely linked to health outcomes, but the direction of the relationship between these characteristics and health of minority populations is controversial. Given this uncertainty, we examined the relationship between neighborhood racial composition, social capital, and black all-cause mortality between 1997 and 2000 in 68 Philadelphia neighborhoods. Data from the U.S. Census, the Philadelphia Health Management Corporation’s 2004 Southeast Pennsylvania Community Health Survey, and city vital statistics were linked by census tract and then aggregated into neighborhoods, which served as the unit of analysis. Neighborhood social capital was measured by a summative score of respondent assessments of: the livability of their community, the likelihood of neighbors helping one another, their sense of belonging, and the trustworthiness of their neighbors. After adjustment for the sociodemographic characteristics of neighborhood residents, black age-adjusted all-cause mortality was significantly higher in neighborhoods that had lower proportion of black residents. Neighborhood social capital was also associated with lower black mortality, with the strongest relationship seen for neighborhoods in the top half of social capital scores. There was a significant interaction between racial composition and social capital, so that the effect of social capital on mortality was greatest in neighborhoods with a higher proportion of black residents and the effect of racial composition was greatest in neighborhoods with high social capital. These results demonstrate that age-adjusted all-cause black mortality is lowest in mostly black neighborhoods with high levels of social capital in Philadelphia.
Keywords: USA, Health inequalities, Social capital, Neighborhood racial composition, Race
Introduction
Multiple studies have demonstrated relationships between neighborhood characteristics and residents’ health, even after adjusting for individual resident characteristics. While many of these studies have focused on demonstrating the adverse impact of physical and economic neighborhood deprivation (Cohen et al., 2003; Diez Roux et al., 2001; Malmstrom, Sundquist, & Johansson, 1999; Stafford, Cummins, Macintyre, Ellaway, & Marmot, 2005), a growing body of work examines the neighborhood social characteristics, such as residential demographic composition and neighborhood social capital (Fang, Madhavan, Bosworth, & Alderman, 1998; Lochner, Kawachi, Brennan, & Buka, 2003; Roberts, 1997; Veenstra, 2000, 2002). The accumulation of evidence linking these social characteristics with residential health, particularly for vulnerable populations points to more complex pathways than initially hypothesized (Jaffee & Perloff, 2003; Kushner & Sterk, 2005; Mellor & Milyo, 2004). This manuscript focuses on the relationships between two of these neighborhood characteristics –racial composition and social capital – in their effects on mortality among blacks.
Studies about the effect of neighborhood racial composition on minority health have mixed results. Several studies demonstrate that higher proportions of blacks in a geographic area are associated with higher mortality (Bird, 1995; Cooper et al., 2001; Deaton & Lubotsky, 2003; McLaughlin & Stokes, 2002) and worse self-reported health status (White & Borrell, 2006), often for both blacks and whites. However, many of these studies do not adjust for other individual or area-level sociodemographic characteristics, limiting the insight into independent effects of racial composition. In contrast, Fang et al. (1998) and Roberts (1997) found lower black mortality in neighborhoods with higher proportions of black residents, after adjusting for neighborhood sociodemographic characteristics. This seemingly paradoxical relationship is supported by a recent analysis demonstrating higher mortality for low socioeconomic status (SES) individuals residing in high SES neighborhoods than for low SES individuals living in low SES neighborhoods (Winkleby, Cubbin, & Ahn, 2006). Although underlying mechanisms are uncertain, minorities residing in neighborhoods with proportionally small minority populations may have higher levels of isolation and lower social support. This hypothesis raises the possibility that the effects of neighborhood racial composition may depend, in part, upon other neighborhood characteristics related to the level of social isolation and social support.
Social capital is a term that is used to describe a related group of community characteristics including social trust, norms of reciprocity and cooperation, and civic engagement (Carpiano, 2006; Kawachi, 1999; Putnam, 2000). Social capital is hypothesized to benefits individuals by: (1) building cooperation among neighbors that can facilitate collective action (Cattell, 2001); (2) promoting healthy behaviors through norms and social control (Cattell, 2001); (3) affecting psychosocial processes that increase positive feelings of subjective well-being, self-esteem, hopefulness, and control over one’s health (Cattell, 2001); (4) improving individual access to resources through social networks; and (5) increasing identification with community members, including solidarity with others of the same ethnic background (Kawachi & Berkman, 2000, Chap. 8; Portes, 1998). Numerous studies link area-level measures of social capital to positive health outcomes, including good self-rated health, lower all-cause, infant, and disease specific mortality (Kawachi & Berkman, 2000, Chap. 8; Kawachi, Kennedy, & Glass, 1999; Kawachi, Kennedy, Lochner, & Prothrow-Stith, 1997; Lochner et al., 2003; Veenstra, 2000, 2002); desirable health behaviors (exercise, tobacco cessation and positive parenting) (Lindstrom, Hanson, & Ostergren, 2001; Lindstrom, Hanson, Ostergren, & Berglund, 2000; Zolotor & Runyan, 2006), and reduced violent behavior (Kennedy, Kawachi, Prothrow-Stith, Lochner, & Gupta, 1998; Sampson, Raudenbush, & Earls, 1997). However, the purported effects of social capital have engendered controversy, because of the definition, the theoretical specification of the construct (Stephens, 2008), and the complexity of its effects (Kushner & Sterk, 2005). Social connectedness and in-group identification (identifying with other members of your race) may benefit members of the majority group but lead to isolation and disenfranchisement for minorities (Cook, 2005; Portes, 1998). The implications of neighborhood social capital may differ by race in the US (Lochner et al., 2003), or between a black living in a mostly black neighborhood versus a mostly white neighborhood; the effect of social capital may transcend neighborhood homogeneity. There is relatively little empirical evidence examining the impact of neighborhood social capital on the health of minorities considered separately from the general population and specifically whether this impact varies by neighborhood racial composition.
Given this background, we investigated the relationship among neighborhood racial composition, neighborhood social capital, and age-adjusted black mortality in Philadelphia, Pennsylvania. We focused on Philadelphia because it includes 68 previously defined neighborhoods that vary widely in neighborhood racial composition and the Philadelphia Health Management Corporation collects information on neighborhood social capital in their biannual survey of the health of Philadelphia residents. Based upon the prior literature, we hypothesized that, after adjusting for other neighborhood sociodemographic characteristics, black mortality would be highest in predominantly white neighborhoods and among neighborhoods with the lowest levels of social capital. Furthermore, we hypothesized that these effects would be interrelated, such that the greatest effect of neighborhood racial composition on black mortality would occur in neighborhoods with low social capital whereas the greatest effect of social capital on black mortality would occur in neighborhoods with the greatest proportion of black residents.
Methods
This study linked data from the 2000 U.S. Census, the Philadelphia Health Management Corporation 2004 Southeast Pennsylvania Community Health Database survey (CHDB), and the city vital statistics files. To conduct the analyses, data from the 381 Philadelphia census tracts were aggregated into 68 neighborhoods that were defined based upon the Neighborhood Information System at the Cartographic Modeling Laboratory at the University of Pennsylvania (http://cml.upenn.edu/nbase). The 68 neighborhoods are relatively small and spatially coherent geographic units whose “boundaries were developed by the Temple University Social Science Data Library based on information gathered from the Philadelphia Police Department, the Philadelphia Inquirer and historical research.” (http://cml.upenn.edu/nbase, help section). While there is no consensus definition of Philadelphia neighborhoods, these boundaries were created based upon maximizing consensus among the existing neighborhood definitions (Bruch, 1999, McMullin, 1975). These neighborhoods are generally larger than individual census tracts, thereby resulting in a greater stability of neighborhood estimates from the limited sample size of the CHDB survey. Because the neighborhood boundaries were defined based upon 1990 census tract boundaries, they required slight modifications to match 2000 census tract boundaries.
Sources of data
Race, sex, age, educational attainment, employment status, poverty level, and renter occupancy composition for the 381 Philadelphia census tracts were obtained from the 2000 U.S. Census. For the purposes of these analyses, respondents were grouped into categories of non-Hispanic black, non-Hispanic white, Hispanic and other. Eight age categories were used: under age 18, 18–25, 26–35, 36–45, 46–55, 56–65, 66–75 and over 75.
Census data on median household income were obtained at the neighborhood level from the University of Pennsylvania’s Cartographic Modeling Laboratory (CML). Although a few CML neighborhoods were slightly different from the neighborhood boundaries used in this study because of census tract changes from 1990 to 2000, only four neighborhoods had more than a 5% difference in total population. Analyses that included the median household income were run with and without these neighborhoods without affecting the results (data not shown).
Data on neighborhood social capital were obtained from a random digit dialing survey of households in Philadelphia conducted by the Philadelphia Health Management Corporation (PHMC) (Health in context: an examination of social capital in Southeastern Pennsylvania, 2004). The survey population was selected using stratified sampling of telephone exchanges within 54 service areas in the greater Philadelphia area. Multiple attempts were made to contact each household, with the respondent selected using the birthday method, i.e., the adult resident who had the last birthday. The response rate was 33% (AAPOR 4). The final sample included 4415 individuals of whom 41% were black, 40% white and 9% Hispanic; 33% were male; 31% were between 18 and 35 years of age; 35% were between 36 and 55, and 34% were over 55; 11% were below the federal poverty level and 14% had not completed high school. Survey items asked respondents to rate the livability of their community, the likelihood of neighbors helping one another, their sense of belonging, and the trustworthiness of their neighbors. The internal consistency of responses to these four items was high (Cronbach’s α = 0.89). We constructed neighborhood level estimates of social capital items and a summative score of the four items using the sampling weights provided by the PHMC to accurately represent 2000 U.S. census populations. These estimates included individuals from all racial groups as the sample size of respondents per neighborhood was too small to permit race-specific estimates for many of the neighborhoods. Three out of the sixty-eight neighborhoods had fewer than twenty respondents from which to calculate a social capital score, and these neighborhoods were excluded from the analysis.
We obtained black age-adjusted all-cause mortality rates for the years 1997–2000 calculated as average rates per 100,000 people per year. These data are compiled from the vital statistics files of the Philadelphia Department of Public Health and are standardized to the 1940 US population. The available mortality data were based upon the boundaries defined by the 1990 census tracts whereas the data obtained from the census were based on 2000 census tracts. The only changes that were made between 1990 and 2000 by the U.S. Census Bureau in the city of Philadelphia were the subdivision of some tracts into two or more tracts (“1990–2000 Census Tract Correspondence”, Philadelphia Health Management Corporation, 2008). The subdivided tracts were able to be reaggregated into comparable geographic zones. Five neighborhoods had one 2000 census tract for which no mortality data were provided, but each of these neighborhoods contained at least six other tracts with complete data.
Statistical analysis
Analyses were conducted using STATA 8.0 or R 2.4. All p-values are two sided with p < 0.05 used as the criteria for statistical significance. Descriptive statistics and graphical approaches were used to explore the relationship between black all-cause mortality and the racial composition of the neighborhoods, and the correlation among other neighborhood characteristics, including demographic composition and socioeconomic status. We used age-adjusted mortality rates rather than crude mortality rates because diagnostic statistics from our linear regression models suggested that this age-adjusted rates yielded models with better fit well without violation of key assumptions.
Linear regression models were used to determine the association between neighborhood racial composition (percent of residents who were black), the neighborhood social capital score, and black all-cause mortality. The results of early models and scatter plots suggested non-linear associations between age-adjusted mortality and the variables of interest. For this reason, we used natural splines for certain variables to fit curves to data and to identify threshold effects while preserving power to detect associations of interest. For the final multivariate model we attempted to strike a balance between adjusting for possible confounders of percent black and social capital score, and overfitting the model. We used the adjusted r2 and p-values for the individual variables to guide model selection with the result that the final model included several variables that were marginally significant (0.05 < p < 0.10). The final model included percent renter occupancy (p < 0.0001), percent with a university degree (p = 0.020), percent unemployed (p = 0.094) and percent male (p = 0.092). Median household income was very highly correlated with the other neighborhood socioeconomic characteristics and was non-significant when added to the model (p = 0.48); thus it was not included in the final model. The final model demonstrated reasonable explanatory power with an adjusted r2 of 0.513. Residual analysis suggested the data were well fit by the final models.
In the final step of the analysis, we constructed a social capital stratum variable corresponding to social capital scores below or above the median social capital score. We added this variable to the final model that we had previously built, along with an interaction between social capital and percent black. Results for this model are presented in terms of predicted means and 95% confidence intervals for several combinations of social capital score and percent black. For this model the adjusted r2 was 0.564 and the original terms in the model continued to have similar effects as in the original model.
Results
Table 1 shows the characteristics of the 68 neighborhoods. Compared to neighborhoods with 50% or higher black residents, neighborhoods that are less than 50% black have a higher percentage of men, an older population, higher rates of educational attainment, lower rates of unemployment, fewer residents living in poverty, a higher median household income, and a higher level of owner occupancy. Neighborhoods that are less than 50% black also have higher levels of social capital with residents more likely to rate their neighborhood as a good place to live and their neighbors as more willing to help one another, to feel a sense of neighborhood belonging and to have a high level of trust in their neighbors. In addition, neighborhood social capital was highly negatively correlated with measures of socioeconomic disadvantage, including poverty, low educational attainment, low household income and high unemployment rate (data not shown).
Table 1.
Sociodemographic and social capital measures for Philadelphia neighborhoods.
| All Philadelphia neighborhoods, mean (range) (n = 68) | Neighborhoods that are <50% black, mean (range) (n = 40) | Neighborhoods that are ≥50% black, mean (range) (n = 28) | |
|---|---|---|---|
| Demographics | |||
| Total population | 22,316 (202–51,569) | 21,961 (10,624–40,358) | 22,565 (202–51,569) |
| Racial composition | |||
| % Black | 42.7 (0.21–96.9) | 15.4 (0.21–49.3) | 81.6 (54.6–96.9) |
| % White | 42.9 (0.6–96.8) | 65.1 (4.0–96.8) | 11.1 (0.6–38.3) |
| % Hispanic | 8.3 (1.0–70.4) | 12.1 (1.4–70.4) | 3.0 (1.0–25.6) |
| % Other | 6.1 (1.2–25.9) | 5.8 (1.63–14.5) | 6.2 (1.2–25.9) |
| Male (%) | 46.6 (41.9–56.7) | 47.8 (41.9–56.7) | 44.5 (43.2–49.1) |
| Age (%) | |||
| < 18 | 24.6 (5.0–42.5) | 22.4 (5.0–42.5) | 27.8 (16.5–34.4) |
| 18–25 | 13.0 (4.5–65.9) | 13.8 (4.5–65.9) | 11.8 (8.1–21.6) |
| 26–35 | 15.1 (10.6–30.3) | 16.4 (11.3–30.3) | 13.2 (10.6–19.7) |
| 36–45 | 14.4 (5.9–21.3) | 14.4 (5.9–21.3) | 14.5 (11.5–16.4) |
| 46–55 | 11.7 (3.5–20.0) | 11.6 (3.5–20.0) | 11.8 (9.5–18.0) |
| 56–65 | 8.2 (2.1–13.0) | 8.1 (2.1–11.6) | 8.3 (6.1–13.0) |
| 66–75 | 6.9 (1.5–12.3) | 6.9 (1.5–12.3) | 6.9 (4.1–10.6) |
| >75 | 6.1 (1.8–15.7) | 6.5 (1.8–15.7) | 5.7 (2.6–10.7) |
| Socioeconomic status | |||
| Median household income | 30,400 (13,711–76,698) | 39,529 (23,399–76,698) | 26,860 (13,711–57,672) |
| % <Federal poverty level | 22.4 (3.4–56.0) | 18.9 (3.5–56.0) | 27.4 (9.3–44.4) |
| % High school degree | 32.1 (9.1–46.4) | 31.2 (9.1–46.4) | 33.5 (24.3–41.8) |
| % Bachelor’s degree | 11.0 (1.4–42.9) | 13.4 (1.4–42.9) | 7.6 (2.1–16.5) |
| % Unemployed | 11.7 (0–27.6) | 6.5 (0–16.7) | 13.7 (2.8–27.6) |
| % Renter occupied | 42.0 (13.5–91.3) | 40.2 (13.5–91.3) | 44.6 (18.0–72.7) |
| Social capital scores | |||
| Combined score | 9.1 (6.6–11.5) | 9.4 (6.6–11.5) | 8.6 (7.4–10.6) |
| Trust | 2.4 (1.6–3.1) | 2.5 (1.6–3.1) | 2.2 (1.9–2.8) |
| Community | 2.2 (1.4–3.1) | 2.4 (1.4–3.1) | 1.9 (1.5–2.5) |
| Helpful neighbors | 2.7 (1.9–3.3) | 2.7 (1.9–3.3) | 2.6 (2.2–3.3) |
| Belong | 1.9 (1.5–2.3) | 1.9 (1.5–2.3) | 1.8 (1.7–2.2) |
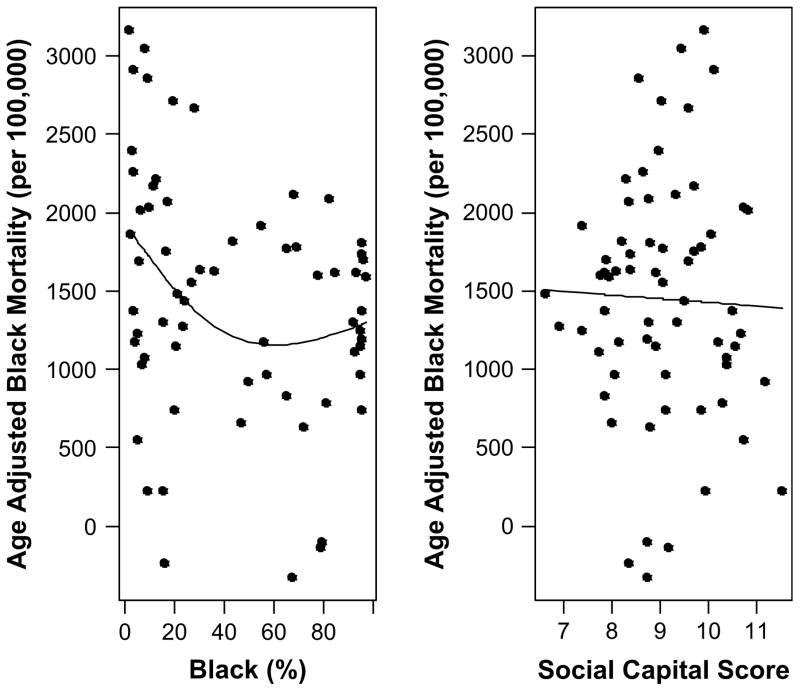
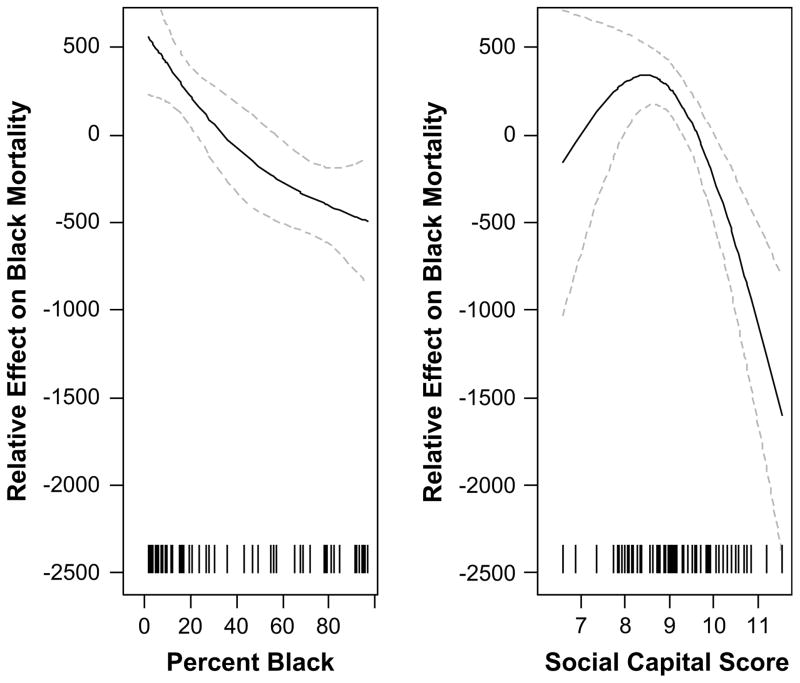
In univariate analyses, the percent of neighborhood residents who were black was inversely associated with age-adjusted black mortality (p = 0.029), with the strongest relationship with mortality seen below 50% black (Fig. 1). After adjusting for other neighborhood characteristics including educational attainment, unemployment, renter occupancy and gender breakdown, neighborhoods with a greater percentage of black residents continued to demonstrate lower age-adjusted black mortality (p = 0.002), albeit in a non-linear fashion (Fig. 2). In this model, age-adjusted black mortality was higher by approximately 1000 excess deaths per 100,000 black residents in neighborhoods with less than 10% of residents who were black compared to neighborhoods with over 90% of residents who were black.
Fig. 1.
Age-adjusted all-cause mortality among blacks (per 100,000) as a function of percent black or social capital score (SCS). Fitted curves are predicted values from univariate linear regression models.
Fig. 2.
Non-linear effects of percent black and social capital score on mean levels of black age-adjusted mortality. Solid lines are predicted values from the linear regression model and dashed lines are 95% confidence intervals. Regions where the 95% CI include zero are those with no statistical evidence of an effect. Hatches along the X-axis indicate the neighborhood data points. The precision of the estimates is higher in regions of the curve with more data points.
In univariate analyses, the neighborhood level of social capital showed no evidence of an association with black adjusted mortality (p = 0.805) (Fig. 1). However, after adjustment for other neighborhood characteristics as described above, neighborhoods with a higher social capital score had lower age-adjusted black mortality (p = 0.0004), although this relationship was largely confined to neighborhoods in the top half of social capital scores (Fig. 2).
In the final model including the interaction between neighborhood racial composition (percent black residents) and neighborhood level of social capital (above versus below median score), the effect of neighborhood racial composition on age-adjusted black mortality was modified by the neighborhood’s level of social capital (p = 0.01 for interaction term). Table 2 demonstrates this relationship, with the lowest rates of black mortality seen in high social capital neighborhoods with a high percentage of black residents. We also looked further at the individual items comprising the social capital score (trust, livability, helpful neighbors and belonging), and like social capital, created a stratum variable corresponding to below/above median social capital score. All of the interactions between the individual social capital items and percent black were similar to the interaction between social capital score and percent black. The interaction between percent black and trust (p = 0.008) was particularly strong while interactions with belonging (p = 0.09), helpful neighbors (p = 0.032), livability (p = 0.029) were weaker.
Table 2.
Mean (95% CI) predicted black age-adjusted mortality as a function of neighborhood percent black and social capital score (p-value for interaction .01).
| Percent black | Social capital score | Age-adjusted black mortality (deaths per 100,000) |
|---|---|---|
| 10 | 8 | 1626 (1126, 2127) |
| 10 | 10 | 1759 (1391, 2128) |
| 90 | 8 | 1213 (786, 1640) |
| 90 | 10 | 379 (−156,a 913) |
Based upon the predicted confidence interval from the linear regression model.
Discussion
Our results show that blacks living in predominantly white neighborhoods in Philadelphia have significantly higher mortality than blacks living in neighborhoods with a greater percentage of black residents, even after adjusting for other neighborhood characteristics. However, this benefit is largely confined to neighborhoods with high social capital. Similarly, black mortality is lower in neighborhoods with high social capital and this association is strongest in neighborhoods that have a greater percentage of black residents.
This study significantly extends the existing literature on neighborhood racial composition and health. Despite an extensive literature examining the association between racial residential segregation and health outcomes, studies of neighborhood racial composition are relatively sparse and those that exist rarely examine mediating factors. Interestingly, while ecological studies of large areas (e.g., states, counties) have generally demonstrated a positive correlation between the percentage of blacks in the area and mortality rates (Bird, 1995; Cooper et al., 2001; Deaton & Lubotsky, 2003; McLaughlin & Stokes, 2002), studies of smaller areas, and multi-level studies using individual-level outcomes, have had mixed results. Studies of New York City have demonstrated lower mortality for elderly blacks, Hispanics, and whites living in neighborhoods with higher proportions of their respective racial group (Fang et al., 1998; Inagami et al., 2006), but worse self-reported health status for blacks who live in neighborhoods with a greater proportion of black residents (White & Borrell, 2006). Roberts’ (1997) Chicago neighborhoods study found an inverse correlation between rates of low birth weight babies among blacks and the proportion of blacks in the neighborhood. Other studies of national cohorts have demonstrated higher mortality for certain black subgroups (e.g., women 65 years and older) in census tracts with a greater proportion of blacks (Jackson, Anderson, Johnson, & Sorlie, 2000) or among black participants who reported higher contact with other blacks in school, childhood neighborhood, present neighborhood, and church (LaVeist, 2003). Although it is tempting to attribute the variation in study results to differences in the ability to adjust for other variables, including individual socioeconomic status, the effect of neighborhood racial composition persists after extensive adjustment for socioeconomic variables in some studies (Fang et al., 1998) but not in others (Henderson et al., 2005; Mellor & Milyo, 2004).
This study adds a potential explanation for the variation in prior findings: our results suggest that neighborhood racial composition effects vary according to other neighborhood characteristics, like social capital. These results are important because they emphasize the complex nature of the relationship between neighborhood racial composition and minority health while also suggesting that the pathway is through social connections and social support (Winkleby et al., 2006).
There are several possible explanations for the interrelated effects of neighborhood racial composition and social capital on black mortality found here. Several studies suggest that minorities living in mostly white areas have less access to health care. Haas et al. (2004) linked 1996 Medical Expenditure Panel Survey data to county-level characteristics and found that blacks reported less difficulty obtaining care and fewer financial barriers when they lived in counties with a high prevalence of blacks. Similarly, blacks and Hispanics have higher rates of certain preventive care services if they live in counties with a high prevalence of blacks (Benjamins, Kirby, & Bond Huie, 2004). Other studies have shown higher numbers of minority practitioners in areas that have a higher percentage of minority residents (Komaromy et al., 1996). Perhaps black residents in Philadelphia neighborhoods that are mostly black have better access to health care, particularly if their neighborhood social capital is high. Neighborhood social capital predicts higher trust in physicians, which, in turn, is associated with greater utilization of preventive care among minorities (Ahern & Hendryx, 2003). Alternatively, blacks who have more long-term contact with other blacks have also been found to have greater racial self-identification and subjective well-being (Postmes & Branscombe, 2002). These individual psychological responses have been correlated with better health outcomes and may be reinforced by high neighborhood social capital. A prior analysis has suggested that racial homogeneity may be an important predictor of lower mortality in societies with low levels of tolerance (Reidpath, 2003). Finally, as mentioned previously, blacks living in neighborhoods with greater proportions of blacks may have different social networks than blacks in mostly white neighborhoods; these networks may provide different levels of social support or access to resources and opportunities. Furthermore, it is possible that these networks are also affected by social capital levels such that beneficial effects are only seen when social capital is relatively high.
Income inequality and relative differences in income are known to have deleterious effects on health (Kaplan, Pamuk, Lynch, Cohen, & Balfour, 1996; Lynch et al., 1998). Given racial income inequality in the US, blacks residing in mostly white neighborhoods may have incomes lower than the average white resident. Indeed, one hypothesized mechanism linking income inequality and health is through disruption of the social fabric of the neighborhood, ultimately leading to decreased social capital (Kawachi & Kennedy, 1997). This correlation between income inequality and social capital may explain the reasons why black mortality is lower in mostly white neighborhoods with higher levels of social capital. Perhaps the neighborhoods that we identified as having higher social capital also have lower income inequality, resulting in lower mortality. Alternatively, it is possible that social capital attenuates the damaging effects of income inequality on health. Unfortunately, without access to the individual income of the residents who died, we cannot provide concrete evidence for this mechanism.
In addition to informing discussions of the effect of neighborhood racial composition on health, our results demonstrate a protective effect of neighborhood social capital on black mortality, particularly in predominantly black neighborhoods. These results are consistent with a growing body of literature that suggests that neighborhood social capital has positive effects on health including decreased overall age-adjusted mortality rates, lower teen birth rates, less firearm crime, and decreased proportions of people reporting only fair or poor health (Gold, Kennedy, Connell, & Kawachi, 2002; Kawachi, 1999; Kawachi et al., 1997; Kennedy et al., 1998; Lochner et al., 2003). Further, these results suggest a “group density effect,” that the benefit of social capital for racial/ethnic minority groups may be related to ethnic density of a neighborhood (Halpern, 1993). Living in a concentrated area with other black residents may confer psychological benefits for blacks through racial self-identification and strong social support ties (Aneshensel et al., 2007; Halpern, 1993; Postmes & Branscombe, 2002). Some researchers have also suggested that ethnic enclaves confer protection against racial discrimination, raising the possibility that the very character of social capital may be different in neighborhoods with a greater proportion of minority residents (Postmes & Branscombe, 2002). This group density effect has also been used to explain findings in other ethnic groups, including Mexican-Americans, where high neighborhood ethnic density buffers deleterious area-level effects on health (Ostir, Eschbach, Markides, & Goodwin, 2003), and Chinese Canadians, whose hospitalization rates decreased when they lived in areas with a Chinatown (Murphy, 1965).
This study has several limitations. Our analysis was cross-sectional and ecological and should not imply causality. We cannot conclude that living in mostly white neighborhoods with low social capital caused increases in black all-cause mortality. Because we studied Philadelphia exclusively, the generalizability of our findings to other cities is uncertain. There are many ways to define a neighborhood. We aggregated census tracts into 68 accepted neighborhoods – neighborhoods that seemed more consistent with what individuals identify than with ones defined by the government, such as census tracts, block groups or zip codes. However, the result of this aggregation did result in a wide range of neighborhood sizes, with the majority being over 10,000 in total population. Despite agreed upon definitions of neighborhoods, there is evidence to suggest that they are too large: up to 25% of people consider their neighborhood to extend only one block in each direction; 32% believe that neighborhoods have only a half mile radius (Lochner et al., 2003). A different unit of analysis or neighborhood definition may have yielded different results. In our case, making larger areas the unit of analysis is more likely to bias us in the direction of the null hypothesis since smaller areas allow for easier identification of contextual characteristics affecting health. In addition, our study is also limited by the relatively low response rate of the PHMC survey, which was used to calculate the social capital scores. The social capital score for each neighborhood was based on responses from an average of 35 residents. This relatively low number of respondents decreases precision around the neighborhood social capital score at the neighborhood level. However, given that the sampling is random across the neighborhoods, the lack of precision should make finding associations between social capital and mortality harder, thereby biasing our analyses towards the null.
This study shows that blacks living in mostly white neighborhoods with low social capital have increased all-cause mortality. Further studies are needed to determine if this correlation is seen in other cities, to elucidate the mechanisms that may underlie increased mortality for minorities living in mostly white neighborhoods and to understand the ways in which social capital modifies the effect of racial composition on health.
References
- Ahern MM, Hendryx MS. Social capital and trust in providers. Social Science & Medicine. 2003;57(7):1195–1203. doi: 10.1016/s0277-9536(02)00494-x. [DOI] [PubMed] [Google Scholar]
- Aneshensel CS, Wight RG, Miller-Martinez D, Botticello AL, Karlamangla AS, Seeman TE. Urban neighborhoods and depressive symptoms among older adults. Journal of Gerontology Series B Psychological Sciences and Social Sciences. 2007;62(1):S52–S59. doi: 10.1093/geronb/62.1.s52. [DOI] [PubMed] [Google Scholar]
- Benjamins MR, Kirby JB, Bond Huie SA. County characteristics and racial and ethnic disparities in the use of preventive services. Preventive Medicine. 2004;39(4):704–712. doi: 10.1016/j.ypmed.2004.02.039. [DOI] [PubMed] [Google Scholar]
- Bird ST. Separate black and white infant mortality models: differences in the importance of structural variables. Social Science & Medicine. 1995;41(11):1507–1512. doi: 10.1016/0277-9536(95)00029-7. [DOI] [PubMed] [Google Scholar]
- Bruch LJ. Focus on neighborhoods. Philadelphia Inquirer. 1999 Apr 11;4 [Google Scholar]
- Carpiano RM. Toward a neighborhood resource-based theory of social capital for health: can Bourdieu and sociology help? Social Science & Medicine. 2006;62(1):165–175. doi: 10.1016/j.socscimed.2005.05.020. [DOI] [PubMed] [Google Scholar]
- Cartographic Modeling Laboratory. Retrieved November 5, 2008, from < http://cml.upenn.edu/nbase/nbAbout.asp> and help section.
- Cattell V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Social Science & Medicine. 2001;52(10):1501–1516. doi: 10.1016/s0277-9536(00)00259-8. [DOI] [PubMed] [Google Scholar]
- 1990 –2000 Census Tract Correspondence. Philadelphia. PA: Philadelphia Health Management Corporation; 2008. [Google Scholar]
- Cohen DA, Mason K, Bedimo A, Scribner R, Basolo V, Farley TA. Neighborhood physical conditions and health. American Journal of Public Health. 2003;93(3):467–471. doi: 10.2105/ajph.93.3.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook K. Networks, norms and trust: the social psychology of social capital* 2004 Cooley Mead Awards address. Social Psychology Quarterly. 2005;68(1):1–14. [Google Scholar]
- Cooper RS, Kennelly JF, Durazo-Arvizu R, Oh HJ, Kaplan G, Lynch J. Relationship between premature mortality and socioeconomic factors in black and white populations of US metropolitan areas. Public Health Reports. 2001;116(5):464–473. doi: 10.1093/phr/116.5.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deaton A, Lubotsky D. Mortality, inequality and race in American cities and states. Social Science & Medicine. 2003;56(6):1139–1153. doi: 10.1016/s0277-9536(02)00115-6. [DOI] [PubMed] [Google Scholar]
- Diez Roux A, Kiefe C, Jacobs D, Haan M, Jackson S, Nieto F, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Annals of Epidemiology. 2001;11:395–405. doi: 10.1016/s1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- Fang J, Madhavan S, Bosworth W, Alderman MH. Residential segregation and mortality in New York City. Social Science & Medicine. 1998;47(4):469–476. doi: 10.1016/s0277-9536(98)00128-2. [DOI] [PubMed] [Google Scholar]
- Gold R, Kennedy B, Connell F, Kawachi I. Teen births, income inequality, and social capital: developing an understanding of the causal pathway. Health Place. 2002;8(2):77–83. doi: 10.1016/s1353-8292(01)00027-2. [DOI] [PubMed] [Google Scholar]
- Halpern D. Minorities and mental health. Social Science & Medicine. 1993;36(5):597–607. doi: 10.1016/0277-9536(93)90056-a. [DOI] [PubMed] [Google Scholar]
- Haas J, Phillips KA, Sonneborn D, McCulloch C, Kaplan C, Liang S. Variation in access to health care for different racial/ethnic groups by the racial/ethnic composition of an individual’s county of residence. Medical Care. 2004;42(7):707–714. doi: 10.1097/01.mlr.0000129906.95881.83. [DOI] [PubMed] [Google Scholar]
- Health in context: An examination of social capital in Southeastern Pennsylvania. Philadelphia. PA: Philadelphia Health Management Corporation; 2004. [Google Scholar]
- Henderson C, Diez Roux AV, Jacobs DR, Jr, Kiefe CI, West D, Williams DR. Neighbourhood characteristics, individual level socioeconomic factors, and depressive symptoms in young adults: the CARDIA study. Journal of Epidemiology and Community Health. 2005;59(4):322–328. doi: 10.1136/jech.2003.018846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inagami S, Borrell LN, Wong MD, Fang J, Shapiro MF, Asch SM. Residential segregation and Latino, black and white mortality in New York City. Journal of Urban Health. 2006;83(3):406–420. doi: 10.1007/s11524-006-9035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SA, Anderson RT, Johnson NJ, Sorlie PD. The relation of residential segregation to all-cause mortality: a study in black and white. American Journal of Public Health. 2000;90(4):615–617. doi: 10.2105/ajph.90.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee KD, Perloff JD. An ecological analysis of racial differences in low birthweight: implications for maternal and child health social work. Health & Social Work. 2003;28(1):9–22. doi: 10.1093/hsw/28.1.9. [DOI] [PubMed] [Google Scholar]
- Kaplan GA, Pamuk ER, Lynch JW, Cohen RD, Balfour JL. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. British Medical Journal. 1996;312:999–1003. doi: 10.1136/bmj.312.7037.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I. Social capital and community effects on population and individual health. Annals of the New York Academy of Sciences. 1999;896:120–130. doi: 10.1111/j.1749-6632.1999.tb08110.x. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Berkman L. Social cohesion, social capital, and health. In: Kawachi I, Berkman L, editors. Social epidemiology. New York: Oxford University Press; 2000. [Google Scholar]
- Kawachi I, Kennedy BP. The relationship of income inequality to mortality–Does the choice of indicator matter? Soc Sci Med. 1997;45:1121–1127. doi: 10.1016/s0277-9536(97)00044-0. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Kennedy B, Glass R. Social capital and self-related health: a contextual analysis. American Journal of Public Health. 1999;89(8):1187–1193. doi: 10.2105/ajph.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Kennedy B, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. American Journal of Public Health. 1997;87(9):1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy B, Kawachi I, Prothrow-Stith D, Lochner K, Gupta V. Social capital, income inequality, and firearm violent crime. Social Science & Medicine. 1998;47(1):7–17. doi: 10.1016/s0277-9536(98)00097-5. [DOI] [PubMed] [Google Scholar]
- Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, et al. The role of black and Hispanic physicians in providing health care for underserved populations. New England Journal of Medicine. 1996;334(20):1305–1310. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- Kushner HI, Sterk CE. The limits of social capital: Durkheim, suicide, and social cohesion. American Journal of Public Health. 2005;95(7):1139–1143. doi: 10.2105/AJPH.2004.053314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA. Racial segregation and longevity among African Americans: an individual-level analysis. Health Services Research. 2003;38(6 Pt 2):1719–1733. doi: 10.1111/j.1475-6773.2003.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom M, Hanson BS, Ostergren PO. Socioeconomic differences in leisure-time physical activity: the role of social participation and social capital in shaping health related behaviour. Social Science & Medicine. 2001;52(3):441–451. doi: 10.1016/s0277-9536(00)00153-2. [DOI] [PubMed] [Google Scholar]
- Lindstrom M, Hanson BS, Ostergren PO, Berglund G. Socioeconomic differences in smoking cessation: the role of social participation. Scandinavian Journal of Public Health. 2000;28(3):200–208. [PubMed] [Google Scholar]
- Lochner KA, Kawachi I, Brennan RT, Buka SL. Social capital and neighborhood mortality rates in Chicago. Social Science & Medicine. 2003;56(8):1797–1805. doi: 10.1016/s0277-9536(02)00177-6. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Kaplan GA, Pamuk ER, Cohen RD, Balfou JL, Yen IH. Income inequality and mortality in metropolitan areas of the United States. American Journal of Public Health. 1998;88:1074–1080. doi: 10.2105/ajph.88.7.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malmstrom M, Sundquist J, Johansson SE. Neighborhood environment and self-reported health status: a multilevel analysis. American Journal of Public Health. 1999;89(8):1181–1186. doi: 10.2105/ajph.89.8.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin DK, Stokes CS. Income inequality and mortality in US counties: does minority racial concentration matter? American Journal of Public Health. 2002;92(1):99–104. doi: 10.2105/ajph.92.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMullin RJ. The neighborhoods of Philadelphia. Philadelphia: Office of the Deputy Managing Director for Housing; 1975. [Google Scholar]
- Mellor JM, Milyo JD. Individual health status and racial minority concentration in US states and counties. American Journal of Public Health. 2004;94(6):1043–1048. doi: 10.2105/ajph.94.6.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy H. Migration and the major mental diseases. In: Kantor M, editor. Mobility and mental health. Springfield; Charles Thomas: 1965. p. 5. [Google Scholar]
- Ostir GV, Eschbach K, Markides KS, Goodwin JS. Neighbourhood composition and depressive symptoms among older Mexican Americans. Journal of Epidemiology and Community Health. 2003;57(12):987–992. doi: 10.1136/jech.57.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portes A. Social capital: its origins and applications in modern sociology. Annual Review of Sociology. 1998;24:1–24. [Google Scholar]
- Postmes T, Branscombe NR. Influence of long-term racial environmental composition on subjective well-being in African Americans. Journal of Personality and Social Psychology. 2002;83(3):735–751. doi: 10.1037//0022-3514.83.3.735. [DOI] [PubMed] [Google Scholar]
- Putnam R. Bowling alone. The collapse and revival of the American community. New York: Simon and Schuster; 2000. [Google Scholar]
- Reidpath DD. “Love thy neighbour” — it’s good for your health: a study of racial homogeneity, mortality and social cohesion in the United States. Social Science & Medicine. 2003;57(2):253–261. doi: 10.1016/s0277-9536(02)00344-1. [DOI] [PubMed] [Google Scholar]
- Roberts EM. Neighborhood social environments and the distribution of low birthweight in Chicago. American Journal of Public Health. 1997;87(4):597–603. doi: 10.2105/ajph.87.4.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Stafford M, Cummins S, Macintyre S, Ellaway A, Marmot M. Gender differences in the associations between health and neighbourhood environment. Social Science & Medicine. 2005;60(8):1681–1692. doi: 10.1016/j.socscimed.2004.08.028. [DOI] [PubMed] [Google Scholar]
- Stephens C. Social capital in its place: using social theory to understand social capital and inequalities in health. Social Science & Medicine. 2008;66(5):1174–1184. doi: 10.1016/j.socscimed.2007.11.026. [DOI] [PubMed] [Google Scholar]
- Veenstra G. Social capital, SES and health: an individual-level analysis. Social Science & Medicine. 2000;50(5):619–629. doi: 10.1016/s0277-9536(99)00307-x. [DOI] [PubMed] [Google Scholar]
- Veenstra G. Social capital and health (plus wealth, income inequality and regional health governance) Social Science & Medicine. 2002;54(6):849–868. doi: 10.1016/s0277-9536(01)00049-1. [DOI] [PubMed] [Google Scholar]
- White K, Borrell LN. Racial/ethnic neighborhood concentration and self-reported health in New York City. Ethnicity & Disease. 2006;16(4):900–908. [PubMed] [Google Scholar]
- Winkleby M, Cubbin C, Ahn D. Low individual socioeconomic status, neighborhood socioeconomic status, and adult mortality. American Journal of Public Health. 2006 doi: 10.2105/AJPH.2004.060970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zolotor AJ, Runyan DK. Social capital, family violence, and neglect. Pediatrics. 2006;117(6):e1124–e1131. doi: 10.1542/peds.2005-1913. [DOI] [PubMed] [Google Scholar]