Abstract
Background
Recently, basic and clinical studies have provided evidence supporting the relationship between circulating levels of fibroblast growth factor (FGF) 23 and the development of atherosclerosis. Given that diabetes is an established risk factor for lower extremity atherosclerotic disease (LEAD), the goal of the present study was to explore the relationship between serum FGF23 levels and LEAD, as well as the related factors, in Chinese patients with type 2 diabetes mellitus (T2DM).
Methods
A total of 401 hospitalized T2DM patients (201 subjects with LEAD and 200 subjects without LEAD) were enrolled in this study. Serum FGF23 levels were determined by a sandwich enzyme-linked immunosorbent assay. Femoral intima-media thickness (F-IMT) and lower limb atherosclerotic plaque were assessed through color Doppler ultrasound.
Results
The median (interquartile range) serum FGF23 levels in the entire study population was 42.08 (35.59–49.17) pg/mL. Subjects with LEAD had significantly higher serum FGF23 levels compared with those without LEAD (44.00 [37.54–51.30] pg/mL versus 40.42 [32.61–48.23] pg/mL, P < 0.001). Logistic regression showed that serum FGF23 levels were independently and positively correlated with the presence of LEAD (odds ratio 1.039, 95% confidence interval 1.012–1.067, P = 0.004). In addition, multiple liner regression analysis revealed that serum FGF23 levels were positively associated with F-IMT (standardized β = 0.175, P < 0.001). Furthermore, this relationship remained significant after additional adjustment for gender and factors potentially affecting serum FGF23 levels (serum calcium, serum phosphorus, and glomerular filtration rate), respectively (both P < 0.01).
Conclusions
In Chinese patients with T2DM, serum FGF23 levels were independently and positively correlated with the presence of LEAD.
Keywords: Type 2 diabetes mellitus, Lower extremity atherosclerotic disease, Fibroblast growth factor 23, Femoral intima-media thickness
Background
Lower extremity atherosclerotic disease (LEAD), a primary manifestation of peripheral arterial disease (PAD), represents systemic atherosclerosis involving the peripheral vascular [1] and thus, is associated with an increased risk of cardiovascular disease [2, 3]. Diabetes is an established risk factor for LEAD [4], and the prognosis of LEAD in patients with diabetes is worse than that for those without diabetes, with a more rapid progression, wider range of vasculature lesions, and greater susceptibility to stenosis and occlusion [5]. In diabetes patients, given the common concurrence of neuropathy, LEAD often remains clinically undetected in the early stage. Diabetes patients are often unaware of the early progression of LEAD due to the loss of pain sensation and lower frequency of intermittent claudication until the symptoms become aggravated and advance to ulceration or gangrene, which are usually presented at the terminal stage of LEAD, leading ultimately to amputation [6]. Therefore, an indicator of early-stage LEAD is needed for the earlier diagnosis and treatment of this disease in patients with diabetes, which will help to avoid amputation and improve patients’ quality of life.
Fibroblast growth factor (FGF) 23, a protein mainly expressed by osteocytes and osteoblasts in bone, plays an important role in the regulation of mineral metabolism (calcium–phosphate homeostasis). Basic research studies have demonstrated that FGF23 induces the onset and development of atherosclerosis through its effects on vascular calcification and endothelial dysfunction [7, 8]. Recently, clinical studies provided evidence supporting the relationship between increased circulating FGF23 levels and atherosclerotic cardiovascular disease [9, 10]. Our previous studies revealed that serum FGF23 levels were associated with not only subclinical atherosclerosis but also coronary artery disease [11–13], suggesting the involvement of FGF23 in the onset and progression of atherosclerosis. In addition, we have also found that serum FGF23 levels are closely associated with the presence of abdominal obesity [14]. However, the association between serum FGF23 levels and LEAD remains to be determined in a Chinese population.
Color Doppler ultrasound shows advantages in the visualization of intima-media thickness (IMT) and plaque, and therefore, is widely used in the clinical setting for noninvasive assessment of PAD (especially LEAD) in patients with diabetes [15]. Hence, color Doppler ultrasound imaging was used to detect abnormalities in the lower extremity arteries in the present study, in order to investigate the relationship between serum FGF23 levels and LEAD, as well as the related factors, in Chinese patients with type 2 diabetes mellitus (T2DM).
Methods
Study population
Between March 2015 and December 2016, 401 patients (203 men, 198 women, age range: 25–78 years) with T2DM who were hospitalized in the Department of Endocrinology and Metabolism of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital were enrolled in the present study. Patients with type 1 diabetes mellitus, gestational diabetes, or other specific types of diabetes were excluded. Additionally, individuals with hepatic dysfunction (acute vital hepatitis; alanine aminotransferase, or aspartate aminotransferase >1.5-fold the upper limit of normal), renal dysfunction (serum creatinine ≥115 µmol/L, or glomerular filtration rate [GFR] <60 mL/min/1.73 m2), hyper- or hypothyroidism, acute infection, malignant tumor, or psychiatric disease were also excluded. All participants were asked to report their clinical information regarding diabetes duration, alcohol consumption, smoking status, and medications. This study was approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. Informed consent was provided by all participants prior to enrollment.
Anthropometric measurements
The body mass index (BMI) of each subject was calculated as weight in kilograms divided by the square of height in meters. Blood pressure was measured with a mercury sphygmomanometer after the subject had rested for at least 10 min. Waist circumference (W) was measured midway between the lowest rib and the iliac crest with the subject in the standing position.
Laboratory measurements
Fasting blood samples were collected from each subject after 10 h of overnight fasting for measurement of fasting plasma glucose (FPG), glycated hemoglobin A1c (HbA1c), fasting C-peptide (FCP), total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c), C-reactive protein (CRP), calcium (Ca), and phosphorus (P) levels. Approximately 2 h after eating breakfast, 2-hour plasma glucose (2hPG) and 2-hour C-peptide (2hCP) levels were assessed. Standard laboratory measurements were performed as described previously [13]. A Kainos sandwich enzyme-linked immunosorbent assay kit (Kainos Laboratories Inc., Tokyo, Japan) was used to determine serum FGF23 levels, and the intra- and inter-assay coefficients of variations were 5.6 and 8.2%, respectively. Serum C-peptide levels were measured by an electrochemiluminescence immunoassay (Roche Diagnostics GmbH, Mannheim, Germany) using the Cobas e 601 analyzer. The HOMA Calculator v2.2.3 released by the University of Oxford was used to estimate the insulin resistance index (homeostasis model assessment 2 of insulin resistance [HOMA2-IR]) using the FPG and FCP levels [16]. The GFR was accurately determined by technetium-99m diethylene triamine pentaacetic acid (Tc99m-DTPA) clearance.
Ultrasonography measurements
All participants underwent color Doppler ultrasound examinations of lower limb arteries using an Acuson Sequoia 512 scanner (Siemens Medical Solutions, Mountain View, CA, USA) equipped with a 5–13 MHz linear array transducer. Ultrasound examination included measurement of atherosclerotic plaque and femoral IMT (F-IMT). Seven arteries in each lower limb, including the femoral artery, deep femoral artery, superficial femoral artery, popliteal artery, anterior tibial artery, posterior tibial artery, and peroneal artery, were checked for atherosclerotic plaque. IMT was defined as the distance between the leading edge of the lumen-intima echo and the leading edge of the media-adventitia echo [17]. F-IMT was defined as the mean value of IMTs of the bilateral femoral arteries [18].
Diagnostic criteria
Diabetes was diagnosed based on the 2010 American Diabetes Association standards [19]. According to the Mannheim consensus [17], atherosclerotic plaque was defined as the presence of a focal structure encroaching into the arterial lumen at least 0.5 mm, or at least 50% greater than the thickness of the surrounding vessel wall, or an IMT ≥1.5 mm. LEAD was defined when atherosclerotic plaques were present in any of the lower limb artery segments listed above [20].
Statistical analysis
Statistical analyses were performed using SPSS 17.0 software package (SPSS Inc., Chicago, IL, USA). All variables underwent a normality test. Normally distributed data and F-IMT data are presented as mean ± standard deviation (SD), and skewed data are expressed as the median with interquartile range. Categorical variables are expressed as a percentage (%). Inter-group comparisons of normally distributed data and skewed data were carried out by the unpaired Student’s t test and Mann–Whitney U test, respectively. The Chi square test was used for inter-group comparisons of categorical variables. Subgroup analysis was performed separately in men and women. Logistic regression analysis was performed to identify multiple factors associated with LEAD. Odd ratio (OR) was calculated to determine whether the relevant factors were risk factors for LEAD. Multiple linear regression analysis was conducted to identify factors independently correlated with the serum FGF23 levels. A two-tailed P value of <0.05 was considered indicative of a statistically significant difference.
Results
Clinical characteristics of the study participants
A total of 401 T2DM participants were enrolled in the present study [median age: 58 (48–64) years], including 201 subjects with LEAD and 200 subjects without LEAD. As shown in Table 1, compared with those without LEAD, subjects with LEAD were older and had higher systolic blood pressure (SBP), F-IMT, and ratio of anti-hypertensive therapy (all P < 0.01), along with a lower GFR (P < 0.01). In addition, subjects with LEAD also exhibited a longer diabetes duration than those without LEAD (P < 0.01). Other variables did not differ significantly between the two groups (all P > 0.05).
Table 1.
Characteristics of the study participants
| Variable | Total | Without LEAD | With LEAD |
|---|---|---|---|
| n (men/women) | 401 (203/198) | 200 (101/99) | 201 (102/99) |
| Age (years) | 58 (48–64) | 50 (41–58) | 62 (59–68)** |
| BMI (kg/m2) | 25.59 ± 3.14 | 25.79 ± 3.27 | 25.38 ± 3.00 |
| W (cm) | 92.51 ± 9.51 | 91.61 ± 9.43 | 93.41 ± 9.52 |
| SBP (mmHg) | 130 (120–140) | 125 (118–134) | 130 (120–142)** |
| DBP (mmHg) | 80 (70–85) | 78 (70–82) | 80 (70–85) |
| FPG (mmol/L) | 7.72 (6.45–9.44) | 7.78 (6.44–9.63) | 7.65 (6.45–9.23) |
| 2hPG (mmol/L) | 13.10 ± 4.23 | 13.05 ± 4.47 | 13.15 ± 4.00 |
| HbA1c (%) | 8.7 ± 1.9 | 8.8 ± 2.0 | 8.7 ± 1.8 |
| HbA1c (mmol/mol) | 72 ± 21 | 72 ± 22 | 72 ± 20 |
| FCP (ng/mL) | 1.84 ± 0.87 | 1.81 ± 0.84 | 1.87 ± 0.89 |
| 2hCP (ng/mL) | 4.13 (2.53–6.48) | 4.13 (2.39–6.53) | 4.09 (2.55–6.40) |
| HOMA2-IR | 1.57 ± 0.75 | 1.56 ± 0.76 | 1.59 ± 0.75 |
| TC (mmol/L) | 4.74 ± 1.01 | 4.83 ± 0.86 | 4.66 ± 1.14 |
| TG (mmol/L) | 1.47 (1.02–2.24) | 1.54 (1.02–2.39) | 1.36 (1.01–2.12) |
| HDL-c (mmol/L) | 1.05 (0.90–1.20) | 1.06 (0.90–1.22) | 1.05 (0.90–1.18) |
| LDL-c (mmol/L) | 2.86 ± 0.81 | 2.92 ± 0.72 | 2.80 ± 0.90 |
| CRP (mg/L) | 0.85 (0.40–1.85) | 0.89 (0.42–1.78) | 0.83 (0.37–1.92) |
| GFR (mL/min/1.73 m2) | 99.01 ± 20.37 | 105.43 ± 20.91 | 92.63 ± 17.69** |
| Ca (mmol/L) | 2.35 ± 0.10 | 2.35 ± 0.10 | 2.34 ± 0.10 |
| P (mmol/L) | 1.27 ± 0.17 | 1.29 ± 0.17 | 1.26 ± 0.16 |
| F-IMT (mm) | 0.79 ± 0.11 | 0.72 ± 0.12 | 0.85 ± 0.01** |
| Current smoker, n (%) | 103 (25.69) | 45 (22.50) | 58 (28.86) |
| Current drinker, n (%) | 58 (14.46) | 27 (13.50) | 31 (15.42) |
| Anti-hypertensive therapy, n (%) | 173 (43.14) | 72 (36.00) | 101 (50.25)** |
| Lipid-lowing therapy, n (%) | 66 (16.46) | 33 (16.50) | 33 (16.42) |
| Diabetes duration (years) | 8.00 (4.00–12.00) | 6.00 (3.00–10.00) | 10.00 (6.00–15.00)** |
Data are expressed as mean ± SD, median (interquartile range), or n (%)
BMI body mass index, W waist circumference, SBP systolic blood pressure, DBP diastolic blood pressure, FPG fasting plasma glucose, 2hPG 2-hour plasma glucose, HbA 1c glycated hemoglobin A1c, FCP fasting C-peptide, 2hCP 2-hour C-peptide, HOMA2-IR homeostasis model assessment 2 of insulin resistance, TC total cholesterol, TG triglyceride, HDL-c high-density lipoprotein cholesterol, LDL-c low-density lipoprotein cholesterol, CRP C-reactive protein, GFR glomerular filtration rate, Ca calcium, P phosphorus, F-IMT femoral intima-media thickness
** P < 0.01 versus without LEAD
Comparison of serum FGF23 levels
Among the entire study population, the median (interquartile range) serum FGF23 levels were 42.08 (35.59–49.17) pg/mL. There was no significant gender difference in serum FGF23 levels (44.00 [35.83–49.58] pg/mL in men versus 41.67 [34.17–47.92] pg/mL in women, P > 0.05). Subjects with LEAD had significantly higher serum FGF23 levels compared with those without LEAD (44.00 [37.54–51.30] pg/mL versus 40.42 [32.61–48.23] pg/mL, P < 0.001). Subgroup analysis confirmed the significant difference in serum FGF23 levels between subjects with and without LEAD separately in men and women (45.63 [37.57–53.41] pg/mL versus 40.83 [33.33–48.33] pg/mL in men, P = 0.001; 43.33 [37.50–47.92] pg/mL versus 39.58 [31.67–46.25] pg/mL in women, P = 0.009; Fig. 1).
Fig. 1.
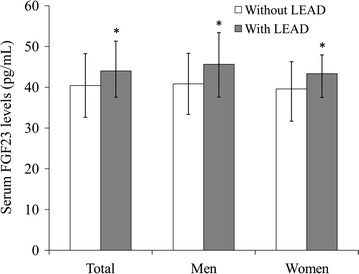
Comparison of serum FGF23 levels between diabetes patients with and without LEAD. Data are shown as median with 25th and 75th percentiles. *P < 0.05 versus without LEAD
Multiple factors related to LEAD
In multiple logistic analysis, the presence of LEAD was defined as the dependent variable and age, gender, BMI, W, SBP, diastolic blood pressure (DBP), HbA1c, HOMA2-IR, TC, TG, HDL-c, LDL-c, CRP, GFR, Ca, P, serum FGF23 levels, diabetes duration, current smoking, current alcohol use, anti-hypertensive therapy, and lipid-lowing therapy were defined as independent variables. The analysis identified the serum FGF23 levels (OR 1.039, 95% confidence interval [CI] 1.012–1.067, P = 0.004) as an independent and positive factor for LEAD, along with age (OR 1.180, 95% CI 1.137–1.225, P < 0.001), diabetes duration (OR 1.103, 95% CI 1.043–1.167, P = 0.001), and current smoking (OR 2.871, 95% CI 1.497–5.507, P = 0.002; Table 2).
Table 2.
Independent factors for LEAD identified by multivariate logistic regression analysis
| Variable | β | SE | OR (95% CI) | P |
|---|---|---|---|---|
| Age | 0.165 | 0.019 | 1.180 (1.137–1.225) | <0.001 |
| FGF23 | 0.039 | 0.014 | 1.039 (1.012–1.067) | 0.004 |
| Diabetes duration | 0.098 | 0.029 | 1.103 (1.043–1.167) | 0.001 |
| Current smoking | 1.055 | 0.332 | 2.871 (1.497–5.507) | 0.002 |
Independent variables originally included: age, gender, BMI, W, SBP, DBP, HbA1c, HOMA2-IR, TC, TG, HDL-c, LDL-c, CRP, GFR, Ca, P, FGF23, diabetes duration, current smoking, current alcohol use, anti-hypertensive therapy, and lipid-lowing therapy
BMI body mass index, W waist circumference, SBP systolic blood pressure, DBP diastolic blood pressure, HbA 1c glycated hemoglobin A1c, HOMA2-IR homeostasis model assessment 2 of insulin resistance, TC total cholesterol, TG triglyceride, HDL-c high-density lipoprotein cholesterol, LDL-c low-density lipoprotein cholesterol, CRP C-reactive protein, GFR glomerular filtration rate, Ca calcium, P phosphorus, FGF23 fibroblast growth factor 23
Multiple stepwise regression analysis of serum FGF23 levels
Spearman correlation analysis showed that serum FGF23 levels were positively associated with age, FCP, 2hCP, W, and F-IMT (all P < 0.05). To further identify factors independently affecting serum FGF23 levels, a multiple liner regression model was used. The dependent variable was serum FGF23 levels, and the independent variables were age, FCP, 2hCP, W, and F-IMT. The analysis revealed that W (standardized β = 0.119, P = 0.016) and F-IMT (standardized β = 0.175, P < 0.001) were independently and positively correlated with serum FGF23 levels. Furthermore, these relationships remained significant after additional adjustment for gender and factors potentially affecting serum FGF23 levels (Ca, P, and GFR), respectively (both P < 0.05; Table 3).
Table 3.
Multivariate regression analyses of factors associated with serum FGF23 levels
| Variable | Standardized β | t | P |
|---|---|---|---|
| Model 1 | |||
| W | 0.119 | 2.411 | 0.016 |
| F-IMT | 0.175 | 3.582 | <0.001 |
| Model 2 (adjusted for gender) | |||
| W | 0.115 | 2.335 | 0.020 |
| F-IMT | 0.184 | 3.748 | <0.001 |
| Model 3 (adjusted for Ca, P, and GFR) | |||
| W | 0.134 | 2.717 | 0.007 |
| F-IMT | 0.184 | 3.485 | 0.001 |
Original variables included: age, FCP, 2hCP, W, and F-IMT
FCP fasting C-peptide, 2hCP 2-hour C-peptide, W waist circumference, F-IMT femoral intima-media thickness
Discussion
The present study demonstrated that serum FGF23 levels were significantly increased in Chinese T2DM patients with LEAD. Our analyses showed that increased serum FGF23 levels were an independent risk factor for LEAD and positively associated with F-IMT. Additionally, a positive correlation between serum FGF23 levels and W was observed.
Accumulating clinical evidence indicates a link between serum FGF23 levels and atherosclerosis [21–25], which is also supported by our previous findings. We previously demonstrated that serum FGF23 levels were not only independently and positively associated with the presence of CAD, but also increased with the cumulative number of stenotic vessels [11]. Moreover, a correlation between serum FGF23 levels and carotid IMT has been reported previously by our study team in a Chinese population without diabetes, even in individuals with normal glucose tolerance [12, 13]. In the present study, serum FGF23 levels were also shown to be independently and positively associated with F-IMT. Because IMT can serve as an indicator of early atherosclerosis, our findings suggest the application of serum FGF23 levels for indicating clinical atherosclerosis in the early stage.
LEAD is one of the clinical manifestations of atherosclerosis that involves the lower extremity arteries. Recently, some studies have explored the relationship between serum FGF23 levels and LEAD. Biscetti et al. [26] diagnosed PAD according to the ankle brachial index and defined its severity according to the Fontaine’s staging system. In 976 Italian patients with T2DM, they found that serum FGF23 levels were independently and positively correlated with the presence and severity of PAD, suggesting that elevated serum FGF23 levels were an important risk factor for PAD (including LEAD). Another study (through diagnostic algorithms and physician adjudication) conducted on community-based cohorts of 659 American women also observed that subjects in the highest FGF23 tertile had a nearly twofold greater risk for PAD compared with those in the lowest tertile [27]. Different from the studies described above, the present study evaluated the arterial wall and plaque deposition directly via color Doppler ultrasound and made the diagnosis of LEAD based on these measurements [28]. The results suggested that elevated serum levels of FGF23 in T2DM patients could help indicate the presence of LEAD.
However, despite the relationships between elevated serum FGF23 levels and increased risk of LEAD demonstrated in an American follow-up study of 9.8 years, these relationships attenuated to be no longer statistically significant after additional adjustment for indexes of kidney function (estimated GFR and urinary albumin to creatinine ratio) [29]. Inconsistently, the present study showed that, after adjustment for GFR (accurately determined by Tc99m-DTPA clearance) as well as for Ca and P, the association between serum FGF23 levels and the presence of LEAD remained statistically significant. Recent studies suggested that higher levels of FGF23 are associated with diabetic nephropathy [30, 31]. In consideration of the influence of kidney function on serum FGF23 levels, the present study only enrolled subjects with normal kidney function (serum creatinine <115 µmol/L and GFR ≥60 mL/min/1.73 m2). Studies with larger sample sizes are needed to confirm whether this relationship is influenced by kidney function.
Usually, abdominal obesity is indicated by the simple index W or the more accurate index, visceral fat area. The association between increased circulating FGF23 levels and W has been demonstrated in the Framingham Heart Study, the Osteoporotic Fractures in Men Study, and the Prospective Investigation of the Vasculature in Uppsala Seniors study [32, 33]. Previously, we reported a relationship between the serum FGF23 levels and visceral fat area [14]. Consistent with these previous findings, serum FGF23 levels were independently and positively related to W in the present study, reminding that abdominal obesity should be taken into consideration when exploring abnormal serum FGF23 levels.
In addition, previous studies reported that age, diabetes duration, and current smoker status are risk factors for LEAD [4, 34]. Consistent with these studies, we also found that these traditional risk factors were positively and independently associated with the presence of LEAD in T2DM patients.
The underlying mechanism via which FGF23 may contribute to LEAD in patients with diabetes remained unclear. Basic studies have suggested that the effects of FGF23 on vascular calcification and endothelial dysfunction might explain the mechanism to some extent. Richter et al. [7] demonstrated that in human coronary artery endothelial cells, FGF23 promoted oxidative stress, which induced nitric oxide release, and its stimulating effects on reactive oxygen species production were counterbalanced by increased reactive oxygen species degradation and suppressed the nitric oxide bioavailability, thus leading to endothelial dysfunction. Research in an animal model detected increases in FGF23 expression at both the mRNA and protein levels in rats with vascular calcification, suggesting that FGF23 might enhance the vascular calcification [8]. In addition, current basic evidence links endothelial dysfunction to diabetes through demonstration of impaired endothelial-dependent vasodilation [35]. Due to multiple homeostatic imbalances occurring with hyperglycemia in diabetes, endothelial dysfunction might be induced by multifactorial etiologies, of which altered FGF23 might be one. The elevation in circulating FGF23 levels, which was also observed in diabetic animal models [36, 37], might aggravate the existing endothelial dysfunction and stimulate vascular calcification, ultimately leading to atherosclerosis in diabetes.
The present study was limited by the cross-sectional design and relatively small sample size, which made it difficult to clarify the causal relationship between increased serum FGF23 levels and the presence of LEAD. Secondly, the study population was restricted to patients with T2DM. Hence, further prospective studies are warranted to confirm and generalize the present findings in a larger population, including those without diabetes. Thirdly, the present study only investigated the relationship between serum FGF23 levels and LEAD. Future research is needed to explore the associations between serum FGF23 levels and other complications of diabetes, such as diabetic retinopathy and nephropathy. In addition, the present study design did not detect ankle brachial index, and the corresponding data are needed to further analyze the association of serum FGF23 levels with the early stage of LEAD in future studies.
Conclusions
As a conclusion, in Chinese patients with T2DM, serum FGF23 levels were significantly increased with the presence of LEAD, independent of other cardiovascular risk factors. Therefore, elevated serum FGF23 levels were associated with the presence of LEAD in this population.
Authors’ contributions
XM and JZ designed the study. XH, XH, HS, LY, and JP collected the data. XH performed statistical analysis and wrote the paper. XP performed the FGF23 measurements. XM, JZ, YB, and WJ revised the paper and contributed to discussion. XH and XH had equal contribution to this paper and were the guarantors. All authors read and approved the final manuscript.
Acknowledgements
We are very grateful to all the staff for helping with the present study. We are grateful to all participants for their dedication in data collection and laboratory measurements.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and analyzed during the current study are not publicly available due to the individual privacy of the patients included in this study, but are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. Informed consent was provided by all participants prior to enrollment.
Funding
This work was funded by the Natural Science Foundation of Shanghai (17ZR1421300), the Natural Science Foundation of Xinjiang Uygur Autonomous Region of China (2016D01C084), the Shanghai Municipal Education Commission—Gaofeng Clinical Medicine Grant Support (20161430), and the innovation foundation of translational medicine of Shanghai Jiao Tong University School of Medicine and Shanghai SJTUSM Biobank (15ZH4006).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- BMI
body mass index
- Ca
calcium
- CRP
C-reactive protein
- DBP
diastolic blood pressure
- FCP
fasting C-peptide
- FGF
fibroblast growth factor
- F-IMT
femoral intima-media thickness
- FPG
fasting plasma glucose
- GFR
glomerular filtration rate
- HbA1c
glycated hemoglobin A1c
- HDL-c
high-density lipoprotein cholesterol
- HOMA2-IR
homeostasis model assessment 2 of insulin resistance
- IMT
intima-media thickness
- LDL-c
low-density lipoprotein cholesterol
- LEAD
lower extremity atherosclerotic disease
- P
phosphorus
- PAD
peripheral arterial disease
- SBP
systolic blood pressure
- T2DM
type 2 diabetes mellitus
- TC
total cholesterol
- Tc99m-DTPA
technetium-99m diethylene triamine pentaacetic acid
- TG
triglyceride
- W
waist circumference
- 2hCP
2-hour C-peptide
- 2hPG
2-hour plasma glucose
Footnotes
Xingxing He and Xiang Hu contributed equally to this work
Contributor Information
Xingxing He, Email: dbxx20130201@163.com.
Xiang Hu, Email: xxbg_hx@163.com.
Xiaojing Ma, Phone: 86-21-64369181, Email: maxiaojing@sjtu.edu.cn.
Hang Su, Email: suhang911203@126.com.
Lingwen Ying, Email: cynthia.ying613@gmail.com.
Jiahui Peng, Email: pengjh0511@163.com.
Xiaoping Pan, Email: panxiaoping1309@163.com.
Yuqian Bao, Email: yqbao@sjtu.edu.cn.
Jian Zhou, Phone: 86-21-64369181, Email: zhoujian@sjtu.edu.cn.
Weiping Jia, Email: wpjia@sjtu.edu.cn.
References
- 1.Writing Committee to Develop Clinical Data Standards for Peripheral Atherosclerotic Vascular Disease. Creager MA, Belkin M, Bluth EI, Casey DE, Jr, Chaturvedi S, Dake MD, Fleg JL, Hirsch AT, Jaff MR, Kern JA, Malenka DJ, Martin ET, Mohler ER, Murphy T, Olin JW, Regensteiner JG, Rosenwasser RH, Sheehan P, Stewart KJ, Treat-Jacobson D, Upchurch GR, Jr, White CJ, Ziffer JA, Hendel RC, Bozkurt B, Fonarow GC, Jacobs JP, Peterson PN, Roger VL, Smith EE, Tcheng JE, Wang T, Weintraub WS. 2012 ACCF/AHA/ACR/SCAI/SIR/STS/SVM/SVN/SVS key data elements and definitions for peripheral atherosclerotic vascular disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards (writing committee to develop clinical data standards for peripheral atherosclerotic vascular disease) Circulation. 2012;125:395–467. doi: 10.1161/CIR.0b013e31823299a1. [DOI] [PubMed] [Google Scholar]
- 2.Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, Fleisher LA, Fowkes FG, Hamburg NM, Kinlay S, Lookstein R, Misra S, Mureebe L, Olin JW, Patel RA, Regensteiner JG, Schanzer A, Shishehbor MH, Stewart KJ, Treat-Jacobson D, Walsh ME. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: areport of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2016;135:e726–e779. doi: 10.1161/CIR.0000000000000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohammedi K, Woodward M, Hirakawa Y, Zoungas S, Colagiuri S, Hamet P, Harrap S, Poulter N, Matthews DR, Marre M, Chalmers J, ADVANCE Collaborative Group Presentations of major peripheral arterial disease and risk of major outcomes in patients with type 2 diabetes: results from the ADVANCE-ON study. Cardiovasc Diabetol. 2016;15:129. doi: 10.1186/s12933-016-0446-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fowkes FG, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, Norman PE, Sampson UK, Williams LJ, Mensah GA, Criqui MH. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382:1329–1340. doi: 10.1016/S0140-6736(13)61249-0. [DOI] [PubMed] [Google Scholar]
- 5.Yang SL, Zhu LY, Han R, Sun LL, Li JX, Dou JT. Pathophysiology of peripheral arterial disease in diabetes mellitus. J Diabetes. 2017;9:133–140. doi: 10.1111/1753-0407.12474. [DOI] [PubMed] [Google Scholar]
- 6.Jude EB, Eleftheriadou I, Tentolouris N. Peripheral arterial disease in diabetes—a review. Diabet Med. 2010;27:4–14. doi: 10.1111/j.1464-5491.2009.02866.x. [DOI] [PubMed] [Google Scholar]
- 7.Richter B, Haller J, Haffner D, Leifheit-Nestler M. Klotho modulates FGF23-mediated NO synthesis and oxidative stress in human coronary artery endothelial cells. Pflugers Arch. 2016;468:1621–1635. doi: 10.1007/s00424-016-1858-x. [DOI] [PubMed] [Google Scholar]
- 8.Zheng S, Zhang S, Song Y, Guo W, Zhai W, Qiu X, Li J. MicroRNA-297a regulates vascular calcification by targeting fibroblast growth factor 23. Iran J Basic Med Sci. 2016;19:1331–1336. doi: 10.22038/ijbms.2016.7920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah NH, Dong C, Elkind MS, Sacco RL, Mendez AJ, Hudson BI, Silverberg S, Wolf M, Rundek T, Wright CB. Fibroblast growth factor 23 is associated with carotid plaque presence and area: the Northern Manhattan Study. Arterioscler Thromb Vasc Biol. 2015;35:2048–2053. doi: 10.1161/ATVBAHA.115.305945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lutsey PL, Alonso A, Selvin E, Pankow JS, Michos ED, Agarwal SK, Loehr LR, Eckfeldt JH, Coresh J. Fibroblast growth factor-23 and incident coronary heart disease, heart failure, and cardiovascular mortality: the Atherosclerosis Risk in Communities study. J Am Heart Assoc. 2014;3:e000936. doi: 10.1161/JAHA.114.000936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu X, Ma X, Pan X, Hao Y, Luo Y, Lu Z, Bao Y, Jia W. Fibroblast growth factor 23 is associated with the presence of coronary artery disease and the number of stenotic vessels. Clin Exp Pharmacol Physiol. 2015;42:1152–1157. doi: 10.1111/1440-1681.12467. [DOI] [PubMed] [Google Scholar]
- 12.Hu X, Ma X, Luo Y, Xu Y, Xiong Q, Pan X, Bao Y, Jia W. Contribution of fibroblast growth factor 23 to Framingham risk score for identifying subclinical atherosclerosis in Chinese men. Nutr Metab Cardiovasc Dis. 2017;27:147–153. doi: 10.1016/j.numecd.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Hu X, Ma X, Luo Y, Xu Y, Xiong Q, Pan X, Bao Y, Jia W. Elevation in fibroblast growth factor 23 and its value for identifying subclinical atherosclerosis in first-degree relatives of patients with diabetes. Sci Rep. 2016;6:34696. doi: 10.1038/srep34696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu X, Ma X, Luo Y, Xu Y, Xiong Q, Pan X, Xiao Y, Bao Y, Jia W. Associations of serum fibroblast growth factor 23 levels with obesity and visceral fat accumulation. Clin Nutr. 2016. (Epub ahead of print). [DOI] [PubMed]
- 15.American Institute of Ultrasound in Medicine (AIUM) American College of Radiology (ACR) Society of Radiologists in Ultrasound (SRU) AIUM practice guideline for the performance of peripheral arterial ultrasound examinations using color and spectral doppler imaging. J Ultrasound Med. 2014;33:1111–1121. doi: 10.7863/ultra.33.6.1111. [DOI] [PubMed] [Google Scholar]
- 16.Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21:2191–2192. doi: 10.2337/diacare.21.12.2191. [DOI] [PubMed] [Google Scholar]
- 17.Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Desvarieux M, Ebrahim S, Fatar M, Hernandez Hernandez R, Kownator S, Prati P, Rundek T, Taylor A, Bornstein N, Csiba L, Vicaut E, Woo KS, Zannad F. Mannheim intima-media thickness consensus. Cerebrovasc Dis. 2004;18:346–349. doi: 10.1159/000081812. [DOI] [PubMed] [Google Scholar]
- 18.Li LX, Lu JX, Shuai HP, Xia HF, Zhang R, Wang JW, Chen MY, Li TT, Bao YQ, Jia WP. Decreased urine uric acid excretion is associated with diabetic retinopathy but not with lower limb atherosclerosis in hospitalized patients with type 2 diabetes. Atherosclerosis. 2015;242:13–18. doi: 10.1016/j.atherosclerosis.2015.06.051. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(Suppl 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li MF, Zhao CC, Li TT, Tu YF, Lu JX, Zhang R, Chen MY, Bao YQ, Li LX, Jia WP. The coexistence of carotid and lower extremity atherosclerosis further increases cardio-cerebrovascular risk in type 2 diabetes. Cardiovasc Diabetol. 2016;15:43. doi: 10.1186/s12933-016-0360-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiao Y, Luo X, Huang W, Zhang J, Peng C. Fibroblast growth factor 23 and risk of all-cause mortality and cardiovascular events: a meta-analysis of prospective cohort studies. Int J Cardiol. 2014;174:824–828. doi: 10.1016/j.ijcard.2014.04.138. [DOI] [PubMed] [Google Scholar]
- 22.Batra J, Buttar RS, Kaur P, Kreimerman J, Melamed ML. FGF-23 and cardiovascular disease: review of literature. Curr Opin Endocrinol Diabetes Obes. 2016;23:423–429. doi: 10.1097/MED.0000000000000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brandenburg VM, Kleber ME, Vervloet MG, Tomaschitz A, Pilz S, Stojakovic T, Delgado G, Grammer TB, Marx N, März W, Scharnagl H. Fibroblast growth factor 23 (FGF23) and mortality: the Ludwigshafen Risk and Cardiovascular Health Study. Atherosclerosis. 2014;237:53–59. doi: 10.1016/j.atherosclerosis.2014.08.037. [DOI] [PubMed] [Google Scholar]
- 24.Biscetti F, Straface G, Porreca CF, Bertoletti G, Vincenzoni C, Snider F, Stigliano E, Arena V, Angelini F, Pecorini G, Bianchi A, Landolfi R, Flex A. Increased FGF23 serum level is associated with unstable carotid plaque in type 2 diabetic subjects with internal carotid stenosis. Cardiovasc Diabetol. 2015;14:139. doi: 10.1186/s12933-015-0301-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freedman BI, Divers J, Russell GB, Palmer ND, Bowden DW, Carr JJ, Wagenknecht LE, Hightower RC, Xu J, Smith SC, Langefeld CD, Hruska KA, Register TC. Plasma FGF23 and calcified atherosclerotic plaque in African Americans with type 2 diabetes mellitus. Am J Nephrol. 2015;42:391–401. doi: 10.1159/000443241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Biscetti F, Straface G, Pitocco D, Angelini F, Tinelli G, Landolfi R, Flex A. Fibroblast growth factor 23 serum level in type 2 diabetic italian subjects with peripheral arterial disease and critical limb ischemia. Eur Rev Med Pharmacol Sci. 2016;20:4048–4054. [PubMed] [Google Scholar]
- 27.Dalal M, Sun K, Cappola AR, Ferrucci L, Crasto C, Fried LP, Semba RD. Relationship of serum fibroblast growth factor 23 with cardiovascular disease in older community-dwelling women. Eur J Endocrinol. 2011;165:797–803. doi: 10.1530/EJE-11-0577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hwang JY. Doppler ultrasonography of the lower extremity arteries: anatomy and scanning guidelines. Ultrasonography. 2017;36:111–119. doi: 10.14366/usg.16054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garimella PS, Ix JH, Katz R, Chonchol MB, Kestenbaum BR, de Boer IH, Siscovick DS, Shastri S, Hiramoto JS, Shlipak MG, Sarnak MJ. Fibroblast growth factor 23, the ankle-brachial index, and incident peripheral artery disease in the Cardiovascular Health Study. Atherosclerosis. 2014;233:91–96. doi: 10.1016/j.atherosclerosis.2013.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Titan SM, Zatz R, Graciolli FG, dos Reis LM, Barros RT, Jorgetti V, Moysés RM. FGF-23 as a predictor of renal outcome in diabetic nephropathy. Clin J Am Soc Nephrol. 2011;6:241–247. doi: 10.2215/CJN.04250510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Inci A, Sari F, Coban M, Olmaz R, Dolu S, Sarıkaya M, Yılmaz N. Soluble Klotho and fibroblast growth factor 23 levels in diabetic nephropathy with different stages of albuminuria. J Investig Med. 2016;64:1128–1133. doi: 10.1136/jim-2016-000142. [DOI] [PubMed] [Google Scholar]
- 32.Haring R, Enserro D, Xanthakis V, Mitchell GF, Benjamin EJ, Hamburg NM, Sullivan L, Nauck M, Wallaschofski H, Vasan RS. Plasma fibroblast growth factor 23: clinical correlates and association with cardiovascular disease and mortality in the Framingham Heart Study. J Am Heart Assoc. 2016;5:e003486. doi: 10.1161/JAHA.116.003486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mirza MA, Alsiö J, Hammarstedt A, Erben RG, Michaëlsson K, Tivesten A, Marsell R, Orwoll E, Karlsson MK, Ljunggren O, Mellström D, Lind L, Ohlsson C, Larsson TE. Circulating fibroblast growth factor-23 is associated with fat mass and dyslipidemia in two independent cohorts of elderly individuals. Arterioscler Thromb Vasc Biol. 2011;31:219–227. doi: 10.1161/ATVBAHA.110.214619. [DOI] [PubMed] [Google Scholar]
- 34.Zhang X, Hu Y, Zeng H, Li L, Zhao J, Zhao J, Liu F, Bao Y, Jia W. Serum fibroblast growth factor 21 levels is associated with lower extremity atherosclerotic disease in Chinese female diabetic patients. Cardiovasc Diabetol. 2015;14:32. doi: 10.1186/s12933-015-0190-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roberts AC, Porter KE. Cellular and molecular mechanisms of endothelial dysfunction in diabetes. Diab Vasc Dis Res. 2013;10:472–482. doi: 10.1177/1479164113500680. [DOI] [PubMed] [Google Scholar]
- 36.Thrailkill KM, Nyman JS, Bunn RC, Uppuganti S, Thompson KL, Lumpkin CK Jr, Kalaitzoglou E, Fowlkes JL. The impact of SGLT2 inhibitors, compared with insulin, on diabetic bone disease in a mouse model of type 1 diabetes. Bone. 2016. (Epub ahead of print). [DOI] [PMC free article] [PubMed]
- 37.Zanchi C, Locatelli M, Benigni A, Corna D, Tomasoni S, Rottoli D, Gaspari F, Remuzzi G, Zoja C. Renal expression of FGF23 in progressive renal disease of diabetes and the effect of ACE inhibitor. PLoS ONE. 2013;8:e70775. doi: 10.1371/journal.pone.0070775. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are not publicly available due to the individual privacy of the patients included in this study, but are available from the corresponding author on reasonable request.


