Abstract
Objectives
To describe racial/ethnic group differences in pain presentation and the prevalence of psychosocial factors among patients admitted to home health care, and to determine the extent of racial/ethnic group differences in the association of psychosocial factors with pain intensity and pain-related disability.
Methods
We analyzed cross-sectional data on 588 patients with activity-limiting pain admitted to home care for physical therapy. Three psychosocial factors were assessed: depressive symptoms, pain self-efficacy, and health literacy. Statistical methods included estimation of general linear models of pain intensity and pain-related disability.
Results
Hispanics and non-Hispanic blacks report a greater number of pain sites, worse pain intensity, and higher levels of pain-related disability than non-Hispanic whites and others. Racial/ethnic minority group patients also have a higher prevalence of adverse psychosocial factors than others, with evidence that race/ethnicity interacts with pain self-efficacy and depressive symptoms in their association with mean pain intensity and pain-related disability, respectively.
Discussion
The substantial racial/ethnic difference in the psychosocial profiles of older adults with activity-limiting pain highlights the importance of screening for these modifiable risk factors and tailoring interventions accordingly. Direct attention to the psychosocial needs of patients could help to address racial/ethnic disparities in pain outcomes.
Keywords: psychosocial factors, pain-related disability, community-based care
Pain is a widely recognized public health problem in the United States due to its prevalence and association with increased morbidity and disability. Older adults are disproportionately affected because of their higher rates of age-associated diseases where pain is often a cardinal symptom. Over half of the US community-dwelling older population in 2011 reported bothersome pain and it is strongly associated with reduced physical function.1 Further evidence of the strong link between pain with disability (ie, pain-related disability) includes the association of pain intensity and number of pain sites with lower levels of activity and difficulty with functional tasks that contribute to lower quality of life.2–5
The Institute of Medicine’s landmark report Relieving Pain in America highlights the challenge of pain including disparities in its presentation, prevalence, and management among specific populations.6 A large body of work has documented significant racial and ethnic disparities when comparing Hispanics, non-Hispanic blacks, and whites/others across diverse pain types and care settings.7–10 Disparities include differences in severe pain prevalence (27% Hispanics, 27% non-Hispanic blacks, 17% non-Hispanic whites among older community-dwelling adults) and the impact of pain on function including greater activity limitation among non-Hispanic blacks with mild pain than among Hispanics and non-Hispanic whites with the same level of pain.11–13
Psychosocial factors are important considerations for older adults with pain problems.6 We focus on depression, pain self-efficacy (PSE), and health literacy because they are modifiable and differences in the prevalence of depressed mood,14,15 low PSE,14,16 and low health literacy13,17 may help explain racial/ethnic group differences in pain intensity and pain-related disability.
Depression is a common comorbid condition among older adults presenting for treatment of chronic pain.18 Higher levels of depressive symptoms are associated with increased pain interference with activity, lower physical function, and increased health care utilization.19 Improvement in depression over a 12-month period is associated with a reduction in pain intensity and pain-related disability.20 There is considerable evidence of differences in the prevalence of depression among racial/ethnic minorities. For example, a comparison of black and white older adults with chronic pain showed a higher level of depressive symptoms in the black population.11,21 In a study comparing blacks, Spanish-speaking Hispanics, English-speaking Hispanics, and non-Hispanic white older adults with arthritis, the Spanish-speaking Hispanic group had twice the rate of “high” depressive symptoms than the other 2 minority groups, and >3 times the rate of non-Hispanic whites.15
PSE, the extent to which an individual feels able to perform daily activities despite pain, is negatively correlated with depression and pain-related disability, and is considered an important factor in recovery from illness or injury.22 There is some evidence of racial/ethnic disparities in PSE, with black Americans showing lower self-efficacy for managing pain symptoms than whites.22,23 In another study, non-Hispanic blacks had significantly higher PSE than Hispanics.24
Low health literacy is independently associated with poor physical function and mental health25; further, health literacy is an important predictor of decline in physical functioning, even after controlling for characteristics such as age, sex, education level, health risk factors (eg, smoking, drinking, obesity), and number of chronic conditions.26 Racial and ethnic minorities are particularly challenged by low health literacy, with Hispanic and black older adults having a “below basic” level of health literacy and whites a “basic” level.15,23,27
To reduce disparities in pain outcomes, it is critical to know the extent to which the above factors vary in terms of their prevalence and if they operate differently depending on race/ethnicity. The current study examines older adults with activity-limiting pain admitted to home health care for physical therapy (PT). This is a particularly appropriate study population because pain is a highly prevalent problem in home care with 53.4% of the 6.4 million home health patients in 2004 and 2005 reporting daily pain interfering with activity on admission.28 Physical therapists commonly provide care to older patients with pain problems and >40% of home care episodes provided to Medicare beneficiaries in 2013 included 6 or more therapy visits.29 Various forms of exercise are the most common PT interventions for older adults with chronic pain30 and there is evidence that multicomponent exercise can decrease disability in frail older adults. However, with increasing recognition of the association of psychological factors with pain and pain outcomes there is a need for “psychologically informed” PT to improve pain management.31
This paper first describes the characteristics of home health care patients on admission with particular attention to racial/ethnic group differences in pain presentation and the prevalence of psychosocial factors. We then examine the association of depressive symptoms, PSE, and health literacy with pain intensity and pain-related disability. Better information about the extent of racial/ethnic group differences in the prevalence and association of these factors could help to improve treatment and reduce disparities in pain and pain-related disability for older adults receiving home health care.
METHODS
Data for the analyses were drawn from a prospective study on pain in home care conducted at the Visiting Nurse Service of New York (VNSNY). VNSNY is a nonprofit certified home health agency providing services to patients residing in the 5 boroughs of New York City and the surrounding counties of Nassau, Suffolk, and Westchester. To be eligible for home health care, Medicare beneficiaries must meet coverage criteria that include needing intermittent or part-time skilled care as well as being home-bound and under a physician’s plan of care. The home services provided may include skilled nursing, PT, occupational therapy, speech-language pathology services, medical social work, and aide service.
The parent study examined the impact of a pain self-management program on older adults with activity-limiting pain admitted to home care with a referral for PT. Eligibility criteria included: (1) English speaking; (2) ages 55 and older; (3) admitted to home care with orders for PT; (4) pain intensity score of 3 or higher on a 0 to 10 scale; and (5) activity-limiting pain reported at the time of study enrollment. In addition, all study patients were required to pass a 6-item cognitive screen32 and provide written informed consent to participate.
Initial screening took place by phone. Potential study participants were first asked “Since starting home care, have you had any pain or discomfort that limits your mobility or other daily activities?” Patients were given examples such as pain or discomfort while walking around the house, walking around outside, going shopping, getting dressed, going to the bathroom, and cooking or preparing meals. In addition to ascertaining eligibility status, we asked about pain type. Screening and agency admission data were used to enroll a patient sample with a balance of 3 pain types within 3 racial/ethnic groups (see below). A comprehensive in-home interview was conducted by trained research assistants within 7 to 10 days of home health admission. Data reported here are drawn from the phone screen and baseline in-person interview. The VNSNY IRB first approved the study in May 2012.
Measures
The baseline survey instrument included a variety of pain, disability, and psychosocial measures for assessing pain presentation, pain-related disability, and the prevalence of psychosocial factors. We assessed race and ethnicity status during the baseline interview to use self-report data to classify patients into 3 racial/ethnic groups: (1) Hispanics, (2) non-Hispanic blacks (NH blacks), and (3) non-Hispanic whites and others (NH Others).
Pain Presentation
Pain intensity was measured using a numeric pain rating scale with patients describing their average pain in the last week on a scale from 0 to 10 (0 = no pain, 10 = pain as bad as you can imagine).33 Its validity and reliability have been established in older adults using experimentally induced pain33,34 and in patients with a variety of diagnoses.35 Study patients reported pain location using the Margolis Pain Diagram.36 We also asked patients about pain chronicity (ie, whether their pain had lasted at least 3 mo).
Pain-related Disability
Pain-related disability was measured with the Roland-Morris Disability Questionnaire37 modified for use with a general pain population (M-RDQ).38 The M-RDQ is a 24-item instrument where respondents indicate whether pain limits a range of positions/activities (eg, walking, lying down, dressing). The total score ranges from 0 (no pain-related disability) to 24 (severe pain-related disability), with scores of 15 or more indicating a high level of disability. An Iranian study of the M-RDQ showed concurrent validity, internal consistency, and test-retest reliability.38 Preliminary evidence of acceptable validity has also been demonstrated in work conducted in the United States.39
Psychosocial Measures
We used 3 instruments to measure psychosocial factors: (1) the PHQ-8 Depression Scale,40,41 which rates depressive symptoms on a 0 (not at all) to 3 (nearly every day) scale with overall scores ranging from 0 to 24; (2) the 10-item PSE Questionnaire42 with scores ranging from 0 to 60; and (3) a 3-item Brief Health Literacy Screen (BHLS)43 with scores ranging from 3 to 15. The PHQ-8 has acceptable validity in diagnosing current depression in clinical41 and epidemiological studies,44 the latter included 21% non-white respondents. We grouped depressive symptom scores into 5 standard categories: none-minimal (0 to 4); mild (5 to 9); moderate (10 to 14); moderate-severe (15 to 19); and severe (20 to 24). We later collapsed the 2 upper categories as only 13 participants (2%) were classified as having severe depressive symptoms.
Psychometric properties of the English version of the PSE Questionnaire have been tested in an Australian study with patients with chronic pain showing acceptable internal consistency, test-retest reliability, and concurrent validity.42 We grouped PSE scores into 4 categories indicating low (0 to 17), modest (18 to 30), moderate (31 to 40), and high (41 to 60) PSE levels. The BHLS showed acceptable internal consistency and concurrent validity in a study with a sample that was 33% black, 66% white, and 1% other races.43 We created a 3-level BHLS variable indicating low (3 to 9), medium (10 to 14), and high health literacy (15).
Other Patient Characteristics
Other characteristics examined include the patient’s sex, age, marital status, and self-rated health (poor, fair, good, very good, and excellent), as well as whether the patient lived alone or had been hospitalized in the past 60 days. The comorbidity measure was a count of the number of self-reported conditions from a predefined list.45
Statistical Analysis
Our analyses included the 588 participants who completed the baseline interview and received at least 2 PT visits during their home health episode that was a requirement of the parent study protocol. We first assessed differences among the 3 racial/ethnic groups in the distribution of each patient characteristic using χ2 tests to assess differences in categorical variables and ANOVA for continuous variables. We then developed and estimated separate models for the dependent variables pain intensity and pain-related disability to examine the association of race/ethnicity, psychosocial factors (ie, depressive symptoms, PSE, and health literacy), and other patient characteristics with these 2 measures. In the model developmental phase, we estimated the bivariate association of each patient characteristic with each dependent variable using ANOVA with the exception of the number of comorbidities where we used a linear regression model with a single independent variable. We also examined the interaction of race/ethnicity and each psychosocial factor for each of the 2 dependent variables using ANOVA. Final models were estimated using general linear models and included as main effects all characteristics significantly associated with a dependent variable at a P≤0.10 level as well as any interactions associated with the dependent variable at P≤0.10.
The classification factors in the final model for pain intensity are: the 3 racial/ethnic groups; depressive symptom score grouped into none/minimal (< 5), mild (5 to 9), moderate (10 to 14), and moderate/severe or severe (≥ 15); PSE score grouped into low (0 to 17), modest (18 to 30), moderate (31 to 40), and high (≥ 41); health literacy score grouped into low (3 to 9), medium (10 to 14), and high (≥ 15); sex; age grouped into <65 and ≥ 65; marital status (married/partner, widowed, divorced/separated, and never married); and self-rated health (poor, fair, and good/very good/excellent). It also includes number of comorbidities as a covariate and the interaction of race/ethnicity with PSE. The final model for pain-related disability included the same factors and covariate as the model for pain intensity but the interaction term differed (the model included the interaction of race/ethnicity with depressive symptoms and not race/ethnicity with PSE).
We tested contrasts between pairs of racial/ethnic groups and levels of the psychosocial variables included in the final models, and the interaction of these contrasts partitioned from the overall interaction. We also tested for linear trend in average pain intensity and mean pain-related disability across psychosocial factor levels for each of the 3 racial/ethnic groups and tested the interaction of psycho-social factor linear trend with race/ethnicity.
FINDINGS
Sample Assembly
Agency data collected on new admissions were electronically screened and identified over 3000 potentially eligible patients during the enrollment period (October 12, 2012 to May 5, 2014). To achieve relatively equal numbers in each of the 3 racial/ethnic groups, Hispanics and NH blacks were substantially oversampled (relative to NH Others) in the new admission screening algorithm. They also were oversampled when selecting individuals for the telephone screen where 2047 patients were contacted by bilingual study staff. Of these, 361 refused to participate during the phone screening and 851 were deemed ineligible because they did not speak English, were cognitively impaired, or did not report activity-limiting pain. Subsequently, 76 refused to participate at the in-home baseline interview visit and 171 did not receive the number of PT visits (2 or more) required by the parent study protocol. The remaining 588 patients met all study criteria, were enrolled in the study, and are included in the analyses presented below.
Sample Description
Twenty-eight percent of the sample was Hispanic, with Puerto Rico the most common country of origin (69%). NH blacks constituted 32% of the sample, whereas the remaining 41% was categorized as NH Others. (The great majority of the NH Other group is white (90%) with Filipino and Asian Indian among the other races reported by the small number of other patients in this group.) The characteristics of the sample on admission to home health care are reported in Table 1 by race/ethnicity.
TABLE 1.
Sample Characteristics by Race/Ethnicity
| n (%) |
P | ||||
|---|---|---|---|---|---|
| Full Sample (N = 588) |
Hispanic (n = 162) |
Non-Hispanic Black (n = 187) |
Non-Hispanic Other (n = 239) |
||
| Female sex | 410 (70) | 115 (71) | 134 (72) | 161 (68) | 0.58 |
| Mean age (SD) (y) | 73.0 (9.9) | 68.3 (8.7) | 72.4 (9.9) | 76.7 (9.1) | < 0.001 |
| Marital status | < 0.001 | ||||
| Married/partner | 176 (30) | 45 (28) | 31 (16) | 100 (42) | |
| Widowed | 180 (31) | 35 (22) | 72 (39) | 73 (30) | |
| Divorced/separated | 135 (23) | 52 (32) | 48 (26) | 35 (15) | |
| Never married | 96 (16) | 30 (18) | 35 (19) | 31 (13) | |
| Lives alone | 257 (44) | 64 (40) | 88 (47) | 105 (44) | 0.39 |
| Hospital stay before home care | 381 (65) | 126 (78) | 115 (62) | 140 (59) | < 0.001 |
| Mean no. comorbidities (SD)* | 2.6 (1.5) | 2.9 (1.6) | 2.7 (1.5) | 2.3 (1.3) | < 0.001 |
| Self-rated health | < 0.001 | ||||
| Poor | 134 (23) | 54 (33) | 44 (24) | 36 (15) | |
| Fair | 223 (38) | 63 (39) | 82 (44) | 78 (33) | |
| Good | 140 (24) | 30 (19) | 43 (23) | 67 (28) | |
| Very good/excellent | 89 (15) | 15 (9) | 16 (9) | 58 (24) | |
| Pain characteristics | |||||
| Pain type (balanced by design) | 0.18 | ||||
| Arthritis but no surgical pain | 199 (34) | 49 (30) | 69 (37) | 81 (34) | |
| Arthritis and surgical pain | 197 (33) | 55 (34) | 52 (28) | 90 (38) | |
| Other pain type | 192 (33) | 58 (36) | 66 (35) | 68 (28) | |
| Mean no. pain sites (SD)† | 5.3 (5.1) | 6.2 (5.6) | 5.6 (6.1) | 4.4 (3.7) | 0.002 |
| Chronic pain | 408 (69) | 125 (77) | 127 (69) | 156 (67) | 0.09 |
| Average pain intensity (SD)‡ | 5.2 (2.2) | 5.9 (2.0) | 5.3 (2.2) | 4.6 (2.1) | < 0.001 |
| Mean pain-related disability score (SD)§ | 16.1 (5.5) | 17.4 (5.1) | 16.4 (5.6) | 15.0 (5.5) | < 0.001 |
| Psychosocial factors | |||||
| Mean depressive symptom score (SD)‖ | 8.0 (5.2) | 9.3 (5.5) | 7.7 (5.1) | 7.4 (4.9) | 0.002 |
| Depressive symptom level‖ | 0.03 | ||||
| None/minimal (< 5) | 161 (29) | 37 (24) | 55 (30) | 69 (31) | |
| Mild (5–9) | 200 (36) | 46 (29) | 66 (36) | 88 (40) | |
| Moderate (10–14) | 125 (22) | 43 (28) | 39 (22) | 43 (19) | |
| Moderate/Severe-Severe (15 +) | 74 (13) | 30 (19) | 22 (12) | 22 (10) | |
| Mean pain self-efficacy (SD)¶ | 28.9 (14.0) | 26.4 (13.3) | 27.7 (14.1) | 31.6 (13.9) | < 0.001 |
| Pain self-efficacy¶ | 0.03 | ||||
| Low (0–17) | 128 (24) | 41 (28) | 49 (28) | 38 (17) | |
| Modest (18–30) | 159 (30) | 47 (32) | 51 (29) | 61 (29) | |
| Moderate (31–40) | 132 (24) | 36 (24) | 43 (25) | 53 (25) | |
| High (41–60) | 116 (22) | 24 (16) | 31 (18) | 61 (29) | |
| Mean health literacy score (SD)# | 11.2 (3.5) | 10.2 (3.5) | 10.7 (3.5) | 12.2 (3.3) | < 0.001 |
| Health literacy score# | < 0.001 | ||||
| Low (3–9) | 186 (33) | 71 (45) | 63 (36) | 52 (22) | |
| Medium (10–14) | 226 (40) | 60 (38) | 72 (42) | 94 (41) | |
| High (15) | 149 (27) | 26 (17) | 38 (22) | 85 (37) | |
Count of comorbidities (see the Methods section).
Based on Margolis Pain Diagram; number of pain sites range from 0 to 45.
Brief Pain Inventory Mean Pain Intensity score estimated as the average level of pain experienced during the past week ranging from 0 (no pain) to 10 (pain as bad as you can imagine).
Roland-Morris scale modified for general pain; range is 0 to 24 with higher values indicating greater pain-related disability.
PHQ-8 with depressive symptom scores ranging from 0 to 24 with higher values indicating greater depressive symptom severity.
Pain self-efficacy (PSE) questionnaire with scores ranging from 0 to 60 with higher values indicating greater PSE.
See the Methods section for health literacy questions and scoring.
Demographics and Health Status
There are relatively large differences in mean age and marital status among the 3 racial/ethnic groups (overall F-test P < 0.001 in each case). Hispanics were significantly younger than NH blacks and NH Others (mean ages of 68.3, 72.4, and 76.7, respectively), and NH blacks also were significantly younger than NH Others (P < 0.001 for all pair-wise tests). Hispanics were much more likely to have been admitted to home care following a hospitalization compared with NH blacks (78% vs. 62%; P = 0.001) and NH Others (78% vs. 59%; P < 0.001). Hispanics reported a mean of 2.9 comorbidities compared with 2.3 for NH Others (P < 0.001); NH blacks reported 2.7 comorbidities (P = 0.02 for the comparison with NH Others; P = 0.26 for the comparison with Hispanics). There also were large and statistically significant differences in self-rated health among the racial/ethnic groups (overall F-test P < 0.001). A third of Hispanics (33%) rated their health as “poor” compared with 24% of NH blacks (P = 0.049) and 15% of NH Others (P < 0.001). The difference between NH blacks and NH Others also is statistically significant (P = 0.02). These data suggest that, despite being younger, the general health status of racial/ethnic minorities is worse than that of NH Others and in some cases it is worse for Hispanics relative to NH blacks.
Pain Characteristics
The pain experience reported by both racial/ethnic minority groups was worse than that of the NH Other group despite all 3 having a similar share of patients with arthritis as well as the combination of arthritis and surgical pain. Hispanics reported a mean of 6.2 pain sites compared with 4.4 for NH Others (P < 0.001); and NH blacks reported 5.6 pain sites (P = 0.01 for the comparison with NH Others). A test of the difference between Hispanics and NH blacks in number of sites was not statistically significant (P = 0.31). Average pain intensity was 5.9 for Hispanics versus 4.6 for NH Others (P < 0.001), and 5.3 for NH blacks (P = 0.01 for the comparison with NH Others). The difference in pain intensity between Hispanics and NH blacks approached statistical significance (P = 0.06). Finally, pain-related disability averaged 17.4 for Hispanics compared with 15.0 for NH Others (P < 0.001); among NH blacks, it averaged 16.4 (P = 0.02 for the comparison with NH Others). Pain-related disability did not differ significantly between Hispanics and NH blacks (P = 0.26).
Psychosocial Factors
Higher levels of depressive symptoms were most common among Hispanics. Roughly half (47%) reported moderate or greater depressive symptoms compared with 34% of NH blacks (P = 0.01) and 29% of NH Others (P < 0.001). Both racial/ethnic minority groups were more likely to be in the lowest PSE category and less likely to be in the highest category compared with NH Others (P = 0.02 for Hispanics vs. NH Others; P = 0.03 for NH blacks vs. NH Others). The racial/ethnic minority groups also had higher rates of low health literacy compared with NH Others: 45% for Hispanics, 36% for NH blacks, and 22% for NH Others (P< 0.001 Hispanics vs. NH Others; P = 0.002 NH blacks vs. NH Others; P = 0.10 for Hispanics vs. NH blacks).
Model of Average Pain Intensity
A final model of average pain intensity was estimated that included the interaction of race/ethnicity with PSE, the only psychosocial factor where the interaction with race/ethnicity approached statistical significance (Table 2). The association of race/ethnicity with average pain intensity, after adjusting for other factors, is statistically significant (P = 0.04). The adjusted mean pain intensities for the 3 racial/ethnic groups are: 5.5 for Hispanics, 5.3 for NH blacks, and 4.9 for NH Others (P = 0.01 for Hispanics vs. NH Others; P = 0.12 for NH blacks vs. NH Others).
TABLE 2.
Final Model for Average Pain Intensity
| Mean Pain Intensity (95% CI) |
P | |
|---|---|---|
| Race/ethnicity | 0.04 | |
| Hispanic | 5.49 (5.14, 5.85) | |
| NH black | 5.25 (4.88, 5.61) | |
| NH other | 4.90 (4.55, 5.25) | |
| Race/ethnicity group comparisons (difference in means) | ||
| Hispanic vs. NH other | 0.59 | 0.01 |
| NH black vs. NH other | 0.35 | 0.12 |
| Psychosocial factors | ||
| Depressive symptom level | 0.006 | |
| None/minimal (< 5) | 4.60 (4.20. 4.99) | |
| Mild (5–9) | 5.29 (4.94, 5.64) | |
| Moderate (10–14) | 5.45 (5.05, 5.85) | |
| Mod./severe-severe (15 +) | 5.52 (4.99, 6.05) | |
| Pain self-efficacy score (PSE) | 0.008 | |
| Low (0–17) | 5.69 (5.29, 6.08) | |
| Modest (18–30) | 5.46 (5.10, 5.83) | |
| Moderate (31–40) | 4.98 (4.58, 5.39) | |
| High (41–60) | 4.72 (4.25, 5.19) | |
| Interaction of race/ethnicity with PSE | 0.09 | |
| Hispanic: 0–17 | 5.93 (5.29, 6.57) | |
| Hispanic: 18–30 | 5.82 (5.22, 6.41) | |
| Hispanic: 31–40 | 5.48 (4.80, 6.16) | |
| Hispanic: 41–60 | 4.76 (3.94, 5.57) | |
| NH black: 0–17 | 5.19 (4.61, 5.77) | |
| NH black: 18–30 | 5.39 (4.78, 6.00) | |
| NH black: 31–40 | 5.18 (4.54, 5.82) | |
| NH black: 41–60 | 5.22 (4.44, 6.00) | |
| NH other: 0–17 | 5.94 (5.26, 6.62) | |
| NH other: 18–30 | 5.18 (4.64, 5.72) | |
| NH other: 31–40 | 4.30 (3.69, 4.91) | |
| NH other: 41–60 | 4.19 (3.57, 4.80) | |
| Health literacy score | ||
| Low (3–9) | 5.43 (5.08, 5.78) | 0.18 |
| Medium (10–14) | 5.25 (4.93, 5.57) | |
| High (15) | 4.96 (4.56, 5.37) | |
| Other characteristics | ||
| Sex | < 0.001 | |
| Female | 5.57 (5.32, 5.82) | |
| Male | 4.86 (4.49, 5.22) | |
| Age | 0.26 | |
| < 65 | 5.34 (4.95, 5.74) | |
| 65 + | 5.08 (4.83, 5.33) | |
| Marital status | 0.80 | |
| Married/partner | 5.32 (4.96, 5.68) | |
| Widowed | 5.10 (4.71, 5.47) | |
| Divorced/separated | 5.15 (4.76, 5.54) | |
| Never married | 5.28 (4.83, 5.73) | |
| No. comorbidities (0–10)* | 4.81 + 0.11 | 0.10 |
| Self-rated health | 0.10 | |
| Poor | 5.51 (5.07, 5.98) | |
| Fair | 5.22 (4.89, 5.56) | |
| Good/very good/excellent | 4.91 (4.56, 5.26) | |
Reported on this line are the model intercept and the incremental change in mean pain intensity per additional comorbidity.
CI indicates confidence interval; NH black, non-Hispanic black; NH other, non-Hispanic others.
Depressive symptom level is highly associated with pain intensity (P = 0.006) with adjusted mean pain intensity scores ranging from a low of 4.6 for those with none or minimal depressive symptoms to a high of 5.5 for patients reporting more than moderate symptoms (P = 0.008; not shown). PSE also is highly associated with pain intensity (P = 0.008). The adjusted mean pain intensity is 5.7 for patients in the lowest PSE category versus 4.7 for individuals with high PSE (P = 0.003). The third psychosocial factor, health literacy, is not significantly associated with pain intensity after adjusting for other factors (P = 0.18).
Figure 1 presents graphically the interaction of race/ethnicity with PSE. For each racial/ethnic group, the adjusted mean pain intensity score is reported as PSE goes from low to high. Of particular note is the lack of change in adjusted mean pain intensity values among NH blacks (P = 0.96 for the difference in mean pain intensity between the low and high PSE groups; P = 0.93 for a test of linear trend between pain intensity and PSE). In contrast, the adjusted means decline substantially as PSE increases for the other 2 racial/ethnic groups. This is particularly the case for the NH Other group where those with low self-efficacy have an adjusted mean pain intensity score of 5.9 compared with 4.2 in the group with high PSE (P < 0.001 for low vs. high for NH Others; P = 0.03 for low vs. high for Hispanics). The test of linear trend, in addition, is statistically significant for NH Others (P < 0.001) and Hispanics (P = 0.02).
FIGURE 1.
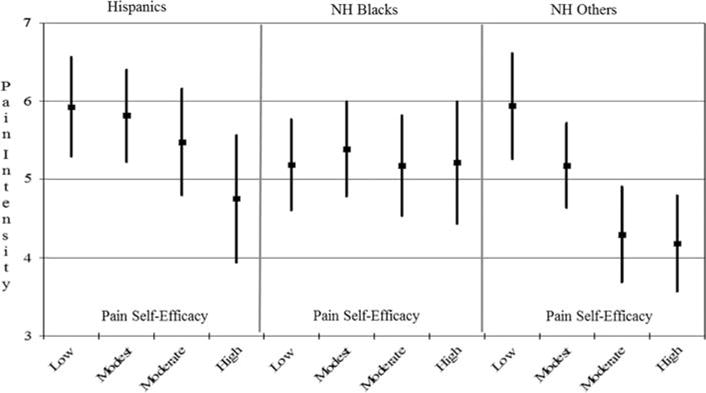
Adjusted average pain intensity as pain self-efficacy increases by race-ethnicity. All data points and SEs in the figure have been adjusted by the factors included in the model presented in Table 2. Within each race/ethnicity group, the difference in mean pain intensity between the lowest (0 to 17) and highest (41 to 60) PSE groups is: Hispanic 1.17 (P = 0.03); NH black −0.03 (P = 0.96); NH other 1.75 (P < 0.001). The test for linear trend by race/ethnicity groups is: Hispanic −0.96 (P = 0.02); NH black −0.03 (P = 0.93); NH other −1.54 (P < 0.001). The difference between race/ethnicity groups in linear trend is: Hispanic versus NH other −0.58 (P = 0.38); NH black versus NH other −1.78 (P = 0.006); Hispanic versus NH black 1.20 (P = 0.08). NH black indicates non-Hispanic black; NH other, non-Hispanic others.
Model of Pain-related Disability
A final model of pain-related disability (M-RDQ score) was estimated that included the interaction of race/ethnicity with depressive symptoms, the only psychosocial factor where the interaction with race/ethnicity approached statistical significance (Table 3). The association of race/ethnicity with pain-related disability, after adjusting for other factors, is highly statistically significant (P = 0.001). The adjusted mean pain-related disability score is 17.4 for Hispanics, 17.6 for NH blacks, and 15.9 for NH Others (P = 0.003 Hispanics vs. NH Others; P= 0.001 NH blacks vs. NH Others).
TABLE 3.
Final Model for Pain-related Disability (Modified Roland-Morris Score)
| Roland-Morris Score 95% CI | P | |
|---|---|---|
| Race/ethnicity | 0.001 | |
| Hispanic | 17.44 (16.69, 18.20) | |
| NH black | 17.55 (16.74, 18.36) | |
| NH other | 15.87 (15.08, 16.66) | |
| Race/ethnicity group comparisons (difference in means) | ||
| Hispanic vs. NH other | 1.57 | 0.003 |
| NH black vs. NH other | 1.67 | 0.001 |
| Psychosocial factors | ||
| Depressive symptom level | < 0.001 | |
| None/minimal (< 5) | 14.82 (13.94, 15.69) | |
| Mild (5–9) | 16.69 (15.94, 17.44) | |
| Moderate (10–14) | 17.51 (16.67, 18.35) | |
| Moderate/severe-severe (15 +) | 18.81 (17.66, 19.96) | |
| Interaction of race/ethnicity with depression | 0.07 | |
| Hispanic: none/minimal | 15.55 (13.99, 17.11) | |
| Hispanic: mild | 16.49 (15.20, 17.78) | |
| Hispanic: moderate | 18.39 (17.01, 19.76) | |
| Hispanic: moderate/severe-severe | 19.35 (17.74, 20.95) | |
| NH black: none/minimal | 14.92 (13.68, 16.16) | |
| NH black: mild | 16.78 (15.60, 17.95) | |
| NH black: moderate | 18.64 (17.22, 20.06) | |
| NH black: moderate/severe-severe | 19.86 (17.81, 21.91) | |
| NH other: none/minimal | 13.98 (12.70, 15.26) | |
| NH other: mild | 16.78 (15.75, 17.85) | |
| NH other: moderate | 15.50 (14.15, 16.86) | |
| NH other: moderate/severe-severe | 17.21 (15.34, 19.08) | |
| Pain self-efficacy (PSEQ) | ||
| Low (0–17) | 18.84 (17.99, 19.69) | < 0.001 |
| Modest (18–30) | 18.37 (17.59, 19.18) | |
| Moderate (31–40) | 16.47 (15.60, 17.34) | |
| High (41–60) | 14.13 (13.14, 15.11) | |
| Health literacy score | 0.09 | |
| Low (3–9) | 16.36 (15.60, 17.12) | |
| Medium (10–14) | 16.96 (16.28, 17.64) | |
| High (15) | 17.55 (16.68, 18.42) | |
| Other characteristics | ||
| Sex | 0.13 | |
| Female | 17.28 (16.72, 17.84) | |
| Male | 16.63 (15.85, 17.40) | |
| Age | 0.18 | |
| < 65 | 17.29 (16.42, 18.15) | |
| 65+ | 16.62 (16.09, 17.16) | |
| Marital status | 0.80 | |
| Married/partner | 17.29 (16.51, 18.07) | |
| Widowed | 16.89 (16.05, 17.73) | |
| Divorced/separated | 16.80 (15.95, 17.64) | |
| Never married | 16.85 (15.87, 17.82) | |
| No. comorbidities (0–10)* | 15.48 + 0.04 | 0.80 |
| Self-rated health | 0.31 | |
| Poor | 17.01 (16.07, 17.94) | |
| Fair | 17.29 (16.57, 18.01) | |
| Good/very good/excellent | 16.57 (15.82, 17.32) | |
Reported on this line are the model intercept and the incremental change in Modified Roland-Morris Score per additional comorbidity.
CI indicates confidence interval; NH black, non-Hispanic black; NH other, non-Hispanic others.
Depressive symptom level is highly associated with pain-related disability (P < 0.001) with adjusted mean M-RDQ scores ranging from a low of 14.8 for those reporting none or minimal depressive symptoms to a high of 18.8 for patients reporting more than moderate symptoms (P = < 0.001; not shown). PSE also is highly associated with pain-related disability (P < 0.001). The adjusted mean M-RDQ score is 18.8 for patients in the lowest PSE category versus 14.1 for individuals with high PSE (P < 0.001; not shown). Health literacy approaches conventional levels of statistical significance (P = 0.09).
Figure 2 presents graphically the interaction of race/ethnicity with depressive symptom level (P = 0.07). For each racial/ethnic group, the adjusted mean pain-related disability score is reported as depressive symptom level goes from low to high. The pattern is very similar for Hispanics and NH blacks with the mean pain-related disability score increasing as depressive symptom level increases. The tests of linear trend are highly statistically significant (P’s < 0.001) for both Hispanics and NH blacks. There is a less pronounced linear trend for the NH Other group (P = 0.02) although the differences in linear trend between the racial/ethnic minority and NH Other groups only approaches statistical significance for NH black versus NH Other (P = 0.09). The differences in adjusted mean M-RDQ scores between the 2 racial/ethnic minority groups and NH Others are, or approach, statistical significance for those with moderate depressive symptoms (P = 0.003 Hispanics vs. NH Others, and P = 0.001 NH blacks vs. NH Others; not shown) and those in the highest category (P = 0.07 Hispanics vs. NH Others, and P= 0.049 NH blacks vs. NH Others; not shown).
FIGURE 2.
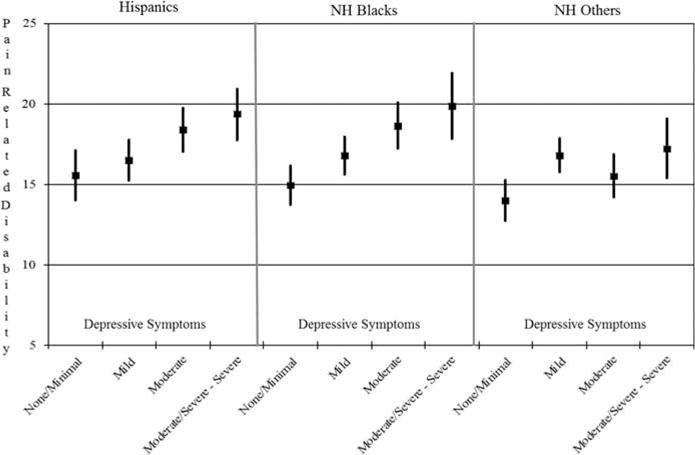
Adjusted mean pain-related disability score as depressive symptoms increase by race-ethnicity. All data points and SEs in the figure have been adjusted by the factors included in the model presented in Table 3. Within each race/ethnicity group, the difference in mean pain-related disability between lowest (none/minimal) and highest (moderate/severe or severe) depressive symptom groups is: Hispanic −3.80 (P = 0.001); NH black −4.94 (P < 0.001); NH other −3.23 (P =0.006). The test for linear trend by race/ethnicity groups is: Hispanic 3.32 (P < 0.001); NH black 4.17 (P < 0.001); NH other 2.10 (P = 0.02). The difference between race/ethnicity groups in linear trend is: Hispanic versus NH other 1.22 (P = 0.30); NH black versus NH other 2.07 (P = 0.09); Hispanic versus NH black −0.85 (P = 0.50). NH black indicates non-Hispanic black; NH other, non-Hispanic others.
DISCUSSION
This study examines the characteristics of, to the best of our knowledge, the largest sample of older adults with activity-limiting pain being treated in the home health setting in the United States. A particular strength of the work is the enrollment of large numbers of adults who identify as racial/ethnic minorities as well as the extensive array of pain, pain-related disability, and psychosocial measures collected to characterize the sample. Our results are consistent with prior research showing that pain presentation differs by race/ethnicity.7,11,13,14 Hispanics and NH blacks report a greater number of pain sites, worse pain intensity, and higher levels of pain-related disability than NH Others despite a study design where the relative distribution of broad pain types is the same within each racial/ethnic group. The pain intensity and pain-related disability differences persist after controlling for other factors with the exception of the difference in pain intensity between NH blacks and NH Others. As high levels of pain at the outset of a course of rehabilitation are associated with poor outcomes such as functional decline,46,47 it seems likely that racial/ethnic minority older adults with pain problems starting a course of PT are at greater risk of decline than others.
The prevalence of psychosocial factors also differs among the racial/ethnic groups. Hispanics, in general, report higher levels of depressive symptoms than either NH blacks or NH Others. Both Hispanics and NH blacks are more likely to report low and less likely to report high levels of PSE than NH Others. The 2 racial/ethnic minority groups also are more likely to be in the lowest health literacy group compared with NH Others. Although our sample was limited to individuals who speak English, 45% of the Hispanic group and 36% of NH blacks are in the lowest health literacy group compared with only 22% of NH Others.
We also found evidence of racial/ethnic group differences in the relationship between psychosocial factors and both pain intensity and pain-related disability. In particular, there is a more pronounced effect of depressive symptom level on pain-related disability among racial and ethnic minorities relative to NH Others. Furthermore, increasing levels of PSE are not associated with a reduction in average pain intensity scores among NH blacks in contrast to the findings for the other 2 racial/ethnic groups. The reasons why the established relationship between higher PSE and lower pain intensity scores was not found among NH blacks in our sample remains unclear. Possible explanations include viewing pain levels as outside of their control (ie, external locus of control), differences in religious views regarding the meaning of suffering, greater use of passive coping strategies (eg, prayer), and difficulty accessing health care resources. These factors either alone or in combination could work to diminish the association between PSE and pain levels among NH blacks.
The relatively high level of modifiable psychosocial risk factors found among racial/ethnic minority patients in the study underscores the importance of educating clinical staff members about disparities in the prevalence of psychosocial factors and how they impact patient outcomes. Reducing depressive symptoms improves pain intensity and function among older adults in general,48 and study results suggest that the benefits will be even greater among minorities. This could help to reduce current disparities in treatment outcomes. There are, however, significant challenges to achieving this goal including racial/ethnic disparities in diagnosis and treatment of depressive symptoms.49
A critical first step is improving the assessment of depressive symptoms in home health care where patients often have complex medical needs that “camouflage” mental health problems50 and treating physical conditions typically takes priority.51 Patients with significant depressive symptoms should be referred for further evaluation and subsequent depression-related care as appropriate. Limited access to mental health providers, however, is a potential barrier to further evaluation,51,52 and cultural differences and receptivity to evidence-based interventions may limit their use among racial/ethnic minorities.53 It is particularly important, therefore, for home health staff to educate racial/ethnic minority patients and their families about depressive symptoms and to encourage them to become more active in their treatment.52 Staff also should help arrange community-based services for patients with mental health needs that are still present at the time of discharge from home care.
There was no difference among the 3 racial/ethnic groups in the association of PSE with pain-related disability. As PSE level increased, pain-related disability declined. Prior work indicates that PSE is a stronger determinant of pain-related disability than age, sex, chronicity, and pain intensity,54 and mediates the relationship between pain intensity and disability55 and physical activity.56 PSE is modifiable through interventions that teach active coping strategies and graded exposure to challenging activities. There is some evidence of racial/ethnic differences in the impact of these types of interventions with Hispanic older adults showing improvement in self-efficacy, whereas other racial/ethnic groups do not.57,58 The extent to which home health staff currently teaches coping strategies to patients with activity-limiting pain (eg, deep breathing, activity pacing) is unknown. Further work is needed to develop evidence-based protocols for increasing PSE among older adults in general and racial/ethnic minority groups in particular.
Our findings suggest that it is important for clinicians to routinely assess patients with activity-limiting pain for depressive symptoms, PSE, and health literacy, and to tailor their treatment approaches accordingly. Tailoring interventions may be particularly important for racial/ethnic minority patients to reduce disparities in outcomes in light of their higher prevalence of certain psychosocial factors and possible differences in how these factors moderate or mediate the effect of interventions. Optimal treatment aimed at addressing health disparities requires attention to the multifactorial nature of these differences.59 Interventions designed for individual behavior change (eg, adopting self-management behaviors) typically use peer educators to deliver health education and counseling in a culturally relevant manner.60 Such culturally leveraged interventions use behavioral norms of the targeted group to develop culturally specific materials that guide program instruction and may have community members assist in the development of the intervention.56
Obtaining input from racial/ethnic minority group members, therefore, is critical to tailoring interventions in home health care in the absence of evidence-based culturally appropriate interventions to improve pain outcomes. Home care agencies may be able to draw on internal staff for some target populations but in other cases external community organizations serving racial/ethnic minority populations (eg, senior centers, local social service agencies) could be asked for advice when developing new programs. Although the physical therapist may not be able to serve as a “peer educator” when providing instruction in a tailored intervention, there is increasing interest in training home health aides—in many cases from the same racial/ethnic group as minority patients—to serve as peer health coaches.61 An iterative process of evaluation and modification of new tailored interventions is likely to be necessary to develop effective programs that reduce disparities in pain outcomes.
Our study has several limitations. First, because the data are cross-sectional, we describe associations and no causal inferences can be drawn directly from our results. Second, this work was conducted at a large urban home care agency and the findings may not be generalizable to other outpatient settings or areas of the country. A related issue is that the racial/ethnic minority groups in our study are broadly defined. There is considerable diversity in the culture and background of individuals who report Hispanic origin as well as those identifying as NH blacks both in the community served by the agency and across the country. Our results may not be generalizable to more precisely defined racial/ethnic minority groups. In addition, we are unable to examine differences among the race/ethnicity groups in the percent of patients who were ineligible and the percent refusing to participate during the phone screen because of limitations in the administrative race/ethnicity data used in the screening process. We also note that the psychometric properties of 2 of the measures examined (PSE and M-RDQ) have not been tested with samples that include significant representation of the minority groups enrolled in our study. Finally, due to resource constraints, our sample was limited to English-speaking older adults.
In summary, we found substantial racial/ethnic disparities in pain and pain-related disability as well as in modifiable psychosocial factors that may moderate or mediate the impact of interventions among older adults receiving treatment in the home setting. Tailoring interventions to address these factors requires screening of patients first to identify factors that can limit treatment success and then addressing them in the context of the intervention to achieve optimal outcomes.
Acknowledgments
The authors gratefully acknowledge contributions made by MaryGrace Trfilio, Research Analyst, Center for Home Care Policy & Research, Visiting Nurse Service of NY New York, NY; to the development of data collection instruments, patient recruitment, and other aspects of primary data collection. The authors also would like to thank the study interviewers.
This project was supported by grant number R01HS020648 from the Agency for Healthcare Research and Quality, Rockville, MD.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
The authors declare no conflict of interest.
References
- 1.Patel KV, Guralnik JM, Dansie EJ, et al. Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154:2649–2657. doi: 10.1016/j.pain.2013.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker TA, Green CR. Intrarace differences among black and white Americans presenting for chronic pain management: the influence of age, physical health, and psychosocial factors. Pain Med. 2005;6:29–38. doi: 10.1111/j.1526-4637.2005.05014.x. [DOI] [PubMed] [Google Scholar]
- 3.Lacey RJ, Belcher J, Rathod T, et al. Pain at multiple body sites and health-related quality of life in older adults: results from the North Staffordshire Osteoarthritis Project. Rheumatology (Oxford) 2014;53:1–9. doi: 10.1093/rheumatology/keu240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soldato M, Liperoti R, Landi F, et al. Non malignant daily pain and risk of disability among older adults in home care in Europe. Pain. 2007;129:304–310. doi: 10.1016/j.pain.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 5.Weiner DK, Rudy TE, Morrow L, et al. The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med. 2006;7:60–70. doi: 10.1111/j.1526-4637.2006.00091.x. [DOI] [PubMed] [Google Scholar]
- 6.Pizzo P, Clark N, Carter-Pokras OD, et al. Relieving Pain in America: A Blueprint for Transforming Prevention, Care. Washington, D.C: Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education; 2011. [Google Scholar]
- 7.Green CR, Anderson KO, Baker TA, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4:277–294. doi: 10.1046/j.1526-4637.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 8.Heins JK, Heins A, Grammas M, et al. Disparities in analgesia and opioid prescribing practices for patients with musculoskeletal pain in the emergency department. J Emerg Nurs. 2006;32:219–224. doi: 10.1016/j.jen.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Lavin R, Park J. A characterization of pain in racially and ethnically diverse older adults: a review of the literature. J Appl Gerontol. 2014;33:258–290. doi: 10.1177/0733464812459372. [DOI] [PubMed] [Google Scholar]
- 10.Mossey JM. Defining racial and ethnic disparities in pain management. Clin Orthop Relat Res. 2011;469:1859–1870. doi: 10.1007/s11999-011-1770-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allen KD, Oddone EZ, Coffman CJ, et al. Racial differences in osteoarthritis pain and function: potential explanatory factors. Osteoarthritis Cartilage. 2010;18:160–167. doi: 10.1016/j.joca.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Grubert E, Baker TA, McGeever K, et al. The role of pain in understanding racial/ethnic differences in the frequency of physical activity among older adults. J Aging Health. 2013;25:405–421. doi: 10.1177/0898264312469404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reyes-Gibby CC, Aday LA, Todd KH, et al. Pain in aging community-dwelling adults in the United States: non-Hispanic whites, non-Hispanic blacks, and Hispanics. J Pain. 2007;8:75–84. doi: 10.1016/j.jpain.2006.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allen KD, Helmick CG, Schwartz TA, et al. Racial differences in self-reported pain and function among individuals with radiographic hip and knee osteoarthritis: the Johnston County Osteoarthritis Project. Osteoarthritis Cartilage. 2009;17:1132–1136. doi: 10.1016/j.joca.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Song J, Chang HJ, Tirodkar M, et al. Racial/ethnic differences in activities of daily living disability in older adults with arthritis: a longitudinal study. Arthritis Care Res. 2007;57:1058–1066. doi: 10.1002/art.22906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen KD, Coffman CJ, Golightly YM, et al. Comparison of pain measures among patients with osteoarthritis. J Pain. 2010;11:522–527. doi: 10.1016/j.jpain.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 17.Cano A, Mayo A, Ventimiglia M. Coping, pain severity, interference, and disability: the potential mediating and moderating roles of race and education. J Pain. 2006;7:459–468. doi: 10.1016/j.jpain.2006.01.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leong IY, Farrell MJ, Helme RD, et al. The relationship between medical comorbidity and self-rated pain, mood disturbance, and function in older people with chronic pain. J Gerontol A Biol Sci Med Sci. 2007;62:550–555. doi: 10.1093/gerona/62.5.550. [DOI] [PubMed] [Google Scholar]
- 19.Mossey JM, Gallagher RM. The longitudinal occurrence and impact of comorbid chronic pain and chronic depression over two years in continuing care retirement community residents. Pain Med. 2004;5:335–348. doi: 10.1111/j.1526-4637.2004.04041.x. [DOI] [PubMed] [Google Scholar]
- 20.Scott EL, Kroenke K, Wu J, et al. Beneficial effects of improvement in depression, pain catastrophizing, and anxiety on pain outcomes: a 12-month longitudinal analysis. J Pain. 2016;17:215–222. doi: 10.1016/j.jpain.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Green CR, Baker TA, Smith EM, et al. The effect of race in older adults presenting for chronic pain management: a comparative study of black and white Americans. J Pain. 2003;4:82–90. doi: 10.1054/jpai.2003.8. [DOI] [PubMed] [Google Scholar]
- 22.Turner JA, Ersek M, Kemp CA. Self-efficacy for managing pain is associated with disability, depression, and pain coping among retirement community residents with chronic pain. J Pain. 2005;6:471–479. doi: 10.1016/j.jpain.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 23.Tan G, Jensen MP, Thornby J, et al. Ethnicity, control appraisal, coping, and adjustment to chronic pain among black and white Americans. Pain Med. 2005;6:18–28. doi: 10.1111/j.1526-4637.2005.05008.x. [DOI] [PubMed] [Google Scholar]
- 24.Townley S, Papaleontiou M, Amanfo L, et al. Preparing to implement a self-management program for back pain in New York City senior centers: what do prospective consumers think? Pain Med. 2010;11:405–415. doi: 10.1111/j.1526-4637.2009.00783.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 26.Smith SG, O’Conor R, Curtis LM, et al. Low health literacy predicts decline in physical function among older adults: findings from the LitCog cohort study. J Epidemiol Community Health. 2015;69:474–480. doi: 10.1136/jech-2014-204915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bennett IM, Chen J, Soroui JS, et al. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med. 2009;7:204–211. doi: 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murtaugh C, Peng T, Moore S, et al. Assessing Home Health Quality for Post-Acute and Chronically Ill Patients. Washington, D.C: Office of the Assistant Secretary for Planning and Evaluation: US Department of Health and Human Services; 2008. [Google Scholar]
- 29.Commission MPA report to Congress: Medicare payment policy. Washington, DC: 2015. [Google Scholar]
- 30.Beissner K, Henderson CR, Papaleontiou M, et al. Physical therapists’ use of cognitive-behavioral therapy for older adults with chronic pain: a nationwide survey. Phys Ther. 2009;89:456–469. doi: 10.2522/ptj.20080163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nicholas MK, George SZ. Psychologically informed interventions for low back pain: an update for physical therapists. Phys Ther. 2011;91:765–776. doi: 10.2522/ptj.20100278. [DOI] [PubMed] [Google Scholar]
- 32.Callahan CM, Unverzagt FW, Hui SL, et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Herr KA, Spratt K, Mobily PR, et al. Pain intensity assessment in older adults: use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clin J Pain. 2004;20:207–219. doi: 10.1097/00002508-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41:1073–1093. doi: 10.1016/j.jpainsymman.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 35.Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- 36.Margolis RB, Tait RC, Krause SJ. A rating system for use with patient pain drawings. Pain. 1986;24:57–65. doi: 10.1016/0304-3959(86)90026-6. [DOI] [PubMed] [Google Scholar]
- 37.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Asghari A. Psychometric properties of a modified version of the Roland-Morris Disability Questionnaire (M-RMDQ) Arch Iran Med. 2011;14:327–331. [PubMed] [Google Scholar]
- 39.Senske J, Harris M. Initial validation of a modified version of the Roland-Morris Disability Questionnaire (RMDQ) in a general chronic pain population. J Pain. 2013;14:S2. [Google Scholar]
- 40.Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care. 2010;33:1034–1036. doi: 10.2337/dc09-2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kroenke K, Spitzer RL, Williams JBW. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Nicholas MK. The Pain Self-Efficacy Questionnaire: taking pain into account. Eur J Pain. 2007;11:153–163. doi: 10.1016/j.ejpain.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 43.Wallston KA, Cawthon C, McNaughton CD, et al. Psychometric properties of the Brief Health Literacy Screen in clinical practice. J Gen Intern Med. 2013;29:1–8. doi: 10.1007/s11606-013-2568-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kroenke K, Strine TW, Spitzer RL, et al. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114:163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 45.Chaudhry S, Jin L, Meltzer D. Use of a self-report-generated Charlson Comorbidity Index for predicting mortality. Med Care. 2005;43:607–615. doi: 10.1097/01.mlr.0000163658.65008.ec. [DOI] [PubMed] [Google Scholar]
- 46.Gatchel RJ, Mayer TG, Theodore BR. The Pain Disability Questionnaire: relationship to one-year functional and psychosocial rehabilitation outcomes. J Occup Rehab. 2006;16:75–94. doi: 10.1007/s10926-005-9005-0. [DOI] [PubMed] [Google Scholar]
- 47.McGeary DD, Mayer TG, Gatchel RJ. High pain ratings predict treatment failure in chronic occupational musculoskeletal disorders. J Bone Joint Surg Am. 2006;88:317–325. doi: 10.2106/JBJS.D.02968. [DOI] [PubMed] [Google Scholar]
- 48.Lin EHB, Katon W, Von Korff M, et al. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290:2428–2429. doi: 10.1001/jama.290.18.2428. [DOI] [PubMed] [Google Scholar]
- 49.Akincigil A, Olfson M, Siegel M, et al. Racial and ethnic disparities in depression care in community-dwelling elderly in the United States. Am J Public Health. 2012;102:319–328. doi: 10.2105/AJPH.2011.300349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bruce ML, Brown EL, Raue PJ, et al. A randomized trial of depression assessment intervention in home health care. J Am Geriatr Soc. 2007;55:1793–1800. doi: 10.1111/j.1532-5415.2007.01419.x. [DOI] [PubMed] [Google Scholar]
- 51.Liebel DV, Powers BA. Home health care nurse perceptions of geriatric depression and disability care management. Gerontologist. 2015;55:448–461. doi: 10.1093/geront/gnt125. [DOI] [PubMed] [Google Scholar]
- 52.Bruce ML, Raue PJ, Sheeran T, et al. Depression care for patients at home (depression CAREPATH): home care depression care management protocol. Home Healthc Nurse. 2011;29:480. doi: 10.1097/NHH.0b013e318229d75b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Voorhees BWV, Walters AE, Quinn MT. Reducing health disparities in depressive disorders between non-Hispanic whites and ethnic minorities a call for pragmatic strategies over the life course. Med Care Res Rev. 2007;64:157S–194S. doi: 10.1177/1077558707305424. [DOI] [PubMed] [Google Scholar]
- 54.Denison E, Åsenlöf P, Lindberg P. Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain. 2004;111:245–252. doi: 10.1016/j.pain.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 55.Costa LDCM, Maher CG, McAuley JH, et al. Self-efficacy is more important than fear of movement in mediating the relationship between pain and disability in chronic low back pain. Eur J Pain. 2011;15:213–219. doi: 10.1016/j.ejpain.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 56.Sperber N. The role of symptoms and self-efficacy in predicting physical activity change among older adults with arthritis. J Phys Act Health. 2014;11:528–535. doi: 10.1123/jpah.2012-0030. [DOI] [PubMed] [Google Scholar]
- 57.Beissner K, Parker S, Henderson CR, Jr, et al. Implementing a combined cognitive-behavioral + exercise therapy protocol for use by older adults with chronic back pain: evidence for a possible race/ethnicity effect. J Aging Phys Act. 2012;20:246. doi: 10.1123/japa.20.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Parker S, Vasquez R, Kahoe E, et al. A comparison of the arthritis foundation self-help program across three race/ethnicity groups. Ethn Dis. 2011;21:444. [PMC free article] [PubMed] [Google Scholar]
- 59.Chin MH, Walters AE, Cook SC, et al. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev. 2007;64:7S–28S. doi: 10.1177/1077558707305413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fisher TL, Burnet DL, Huang ES, et al. Cultural leverage: interventions using culture to narrow racial disparities in health care. Med Care Res Rev. 2007;64:243S–282SS. doi: 10.1177/1077558707305414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Feldman PH, McDonald MV, Trachtenberg MA, et al. Center for stroke disparities solutions community-based care transition interventions: study protocol of a randomized controlled trial. Trials. 2015;16:32. doi: 10.1186/s13063-015-0550-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


