Abstract
Background
Suicidal adolescents are heterogeneous, which can pose difficulties in predicting suicidal behavior. The Youth Self-Report (YSR) psychopathology profiles predict the future onset of psychopathology and suicide-related outcomes. The present study examined the prevalence and correlates of YSR psychopathology profiles among suicidal adolescents and prospective associations with post-discharge rates of suicide attempts and psychiatric rehospitalization.
Methods
Participants were acutely suicidal, psychiatrically hospitalized adolescents (N=433 at baseline; n=355 at follow-up) who were enrolled in a psychosocial intervention trial during hospitalization. Psychopathology profiles were assessed at baseline. Suicide attempts and rehospitalization were assessed for up to 12 months following discharge.
Results
Latent profile analysis identified four psychopathology profiles: subclinical, primarily internalizing, and moderately and severely dysregulated. At baseline, profiles differed by history of non-suicidal self-injury (NSSI) and multiple suicide attempts (MA) as well as severity of suicide ideation, hopelessness, depressive symptoms, anxiety symptoms, substance abuse, and functional impairment. The dysregulation profiles predicted suicide attempts within 3 months post-discharge. The internalizing profile predicted suicide attempts and rehospitalization at 3 and 12 months.
Limitations
This study’s participants were enrolled in a randomized trial and were predominantly female, which limit generalizability. Additionally, only a history of NSSI was assessed.
Conclusions
The dysregulation profile was overrepresented among suicidal youth and associated with impairment in several domains as well as suicide attempts shortly after discharge. Adolescents with a severe internalizing profile also reported adverse outcomes throughout the study period. Psychopathology profiles warrant further examination in terms of their potential predictive validity in relation to suicide-related outcomes.
Keywords: Youth Self-Report, dysregulation profile, adolescent, suicidal behavior, hospitalization
Background
Suicidal adolescents present for mental health treatment with substantial demographic and clinical heterogeneity, which challenges the development of efficacious treatments and preventative interventions (Asarnow and Miranda, 2014; Brent et al., 2013). Limited resources for mental health services necessitate efficient triage decisions for these youth regarding level of care and appropriately personalized follow-up care (Troister et al., 2008). Above and beyond accumulative burden, understanding how multiple risk factors interact and co-occur may aid in the prediction of more imminent suicide-related outcomes (Asarnow and Miranda, 2014; Nock, 2010; Pena et al., 2012).
There are several obstacles in the prediction and prevention of adolescent suicidal behavior, the leading predictor of suicide. One challenge is that although adolescent suicide risk is one of the most common mental health emergencies, actual suicide attempts and mortality have relatively low prevalence rates within the general population (Hawton et al., 2012 As a result, most indices of suicide risk are overly sensitive, resulting in many false positives. Assessment of suicidal thoughts and behaviors only moderately bolsters prediction of future suicidal behaviors, and some measures in this area have predictive validity for some but not all suicidal youth (Ribeiro et al., 2016). For instance, the Suicide Ideation Questionnaire-Jr. (SIQ-Jr.) has shown one-year predictive validity for suicide attempts among psychiatrically hospitalized girls only (King et al., 2014).
In contrast, a substantial body of research indicates that assessment of multiple domains of impairment aids in characterizing risk for future suicidal behavior. For example, a recent study of adolescents in a general emergency department screened for suicide ideation/attempt, depressive symptoms, and alcohol/substance abuse found that youth endorsing all domains were most likely to engage in suicidal behavior two months later (King et al., 2015; Pena et al., 2012). Impairment due to alcohol/substance abuse may be a marker of a developmental trajectory with pervasive externalizing, disinhibited behavior and captures a group of individuals who are likely to engage in harmful mood-dependent behaviors (Zucker et al., 2011). Thus, assessing the co-occurrence of mental health concerns appears to be a promising approach to the prediction of suicidal behavior (Diamond et al., 2010; Wintersteen et al., 2007).
Comorbid internalizing and externalizing symptoms have long been recognized as being particularly relevant to suicidal behavior (Nock et al., 2016). Nationally representative studies indicate that some patterns of comorbidity are differentially associated with suicide-related outcomes among adolescents and adults (Nock et al., 2013, 2008). Internalizing disorders such as mood disorders predict suicidal thoughts but their co-occurrence with externalizing disorders also significantly elevates the probability of future impulsive and suicidal behavior as well as eventual suicide (Brezo et al., 2011; Brook et al., 2015; Kim et al., 2012; Seguin et al., 2014). Individuals affected by comorbid conditions may be at relatively higher risk due in part to an “acquired capacity” for engaging in suicidal behavior through a history of behavioral disinhibition (Van Orden et al., 2010) and experiencing severe agitation (Bentley et al., 2016; Rogers et al., 2016). This constellation of symptoms could lead to a faster transition from suicidal ideation to suicidal behavior (May and Klonsky, 2016; Nock et al., 2016). Advancing our understanding patterns of comorbidity bears substantial importance for the study of suicidal behavior.
One potentially informative comorbid internalizing/externalizing phenotype is the “dysregulation profile,” characterized by simultaneously elevated scores on the Anxious/Depressed, Attention Problems, and Aggressive Behavior subscales of the Youth Self-Report (YSR) and Child Behavior Checklist (CBCL).1 This YSR and CBCL symptom profile has been proposed as a marker of psychopathology as it prospectively predicts the future onset of anxious, mood, disruptive behavior, substance use, and personality disorders as well as suicide-related outcomes, i.e. suicidal ideation, suicide attempts, and psychiatric hospitalization (Althoff et al., 2010a, 2010b; Bellani et al., 2012; De Caluwé et al., 2013; Holtmann et al., 2011). The dysregulation profile may reflect an early-onset limited capacity to cope with aversive affective, cognitive, and behavioral states and risk for more chronic impairment (Beauchaine et al., 2009; Sharp and Fonagy, 2015). Youth who have been psychiatrically hospitalized are at high risk for suicide-related outcomes within months of discharge, and the dysregulation profile could differentiate youth who have relatively higher risk. However, no study to date has examined whether the dysregulation profile or other YSR symptom profiles (e.g. a primarily internalizing or externalizing profile) would aid in predicting recurrent risk.
Previous studies of the dysregulation profile have largely been conducted with community or outpatient clinical samples in which the prevalence and severity of suicide risk is relatively low to moderate (Bellani et al., 2012). As a result, it is unknown whether the dysregulation profile uniquely and specifically predicts suicide-related outcomes or whether it is simply sensitive enough to distinguish between youth in the community with and without psychopathology. Further research is needed to determine whether YSR symptom profiles are prospectively associated with suicide-related outcomes (e.g. suicide attempts and psychiatric hospitalization) among clinically high-risk adolescents. Although the YSR and CBCL are often administered as part of standard clinical practice, to our knowledge no study to date has prospectively examined YSR psychopathology profiles among suicidal youth receiving inpatient services. Such a study could have implications for the individual tailoring of safety planning and post-discharge treatment linkage for youth who experiencing an especially pernicious trajectory of psychopathology and concomitantly long-term mental health care needs. Moreover, the YSR may also be informative in identifying other patterns of psychopathology that predict post-hospitalization outcomes (e.g. pronounced internalizing or externalizing patterns).
The present study aims are to (1) examine the prevalence and clinical correlates of YSR symptom profiles among acutely suicidal adolescents at the time of psychiatric hospitalization, and (2) compare profiles in post-discharge rates of suicide attempts and psychiatric rehospitalization. Based on prior research (Bellani et al., 2012; Olino et al., 2012) we hypothesized that at least three YSR profiles will emerge: dysregulated, primarily internalizing, and primarily externalizing. Further, we hypothesized that the dysregulated youth will report more acute psychopathology at baseline and will be more likely to attempt suicide and to be rehospitalized after discharge.
Methods
Participants
This study’s sample included 433 suicidal adolescents at baseline (310 females, 123 males; 96.7% of overall sample) and 355 adolescents at follow-up (79.2% of overall sample), ages 13–17 years (M = 15.6 years, SD = 1.3). Participants were primarily White (85.9%), Black (7.6%), American Indian (2.3%), Asian American (1.2%), and Other (3.0%). Annual income for families ranged from less than $15,000 (5%) to more than $100,000 per year (16%), with the median income in the range of $40,000 - $59,000 per year. Participants with and without data at each time point did not differ on gender, age, race, use of public assistance, or intervention group. Parents and adolescents, respectively, provided informed consent and assent to IRB-approved study protocols.
Measures
Suicide attempts were assessed using items from the NIMH Diagnostic Interview Schedule (DISC; “Have you tried to kill yourself?”; Shaffer et al., 1998). Follow-up assessments of suicide attempts were conducted at 6 weeks, 3 months, 6 months, and 12 months. The period at each follow-up assessment was intended to capture data since the previous interview and was adjusted to cover any missed assessments. For example, the interviewer prefaced the prompt with “Since the last time we talked to you, which was in [month].”
The Suicidal Ideation Questionnaire—Junior (SIQ-JR; Reynolds and Mazza, 1999) is a 15-item self-report measure that assesses a range of suicidal thoughts on a 7-point time-referential scale ranging from “I never had this thought” to “almost every day”. It has excellent test-retest reliability and was predictive of suicidal thoughts and attempts 6 months post-hospitalization in an adolescent inpatient sample. In this sample, the SIQ-JR had an internal consistency of .92.
Baseline history of non-suicidal self-injury (NSSI) was assessed using an item from the Schedule for Affective Disorders and Schizophrenia for School-Aged Children—Present and Lifetime Versions (K-SADS-PL; Kaufman et al., 1997). NSSI was defined as report of “self-mutilation, or other acts done without intent of killing himself.”
The Youth Self Report (YSR; Achenbach, 1991) is a 119-item questionnaire that assesses a broad range of behavior problems and was assessed at baseline. The present analysis utilized 6 empirically-based syndrome scales as continuous indicators of internalizing and externalizing psychopathology: Anxious/Depressed, Withdrawn/Depressed, Somatic Complaints, Attention Problems, Aggressive Behavior, and Rule-Breaking Behavior.
The Beck Hopelessness Scale (BHS; Beck and Steer, 1988) is a 20-item self-report true/false questionnaire that assesses negative attitudes about the future (e.g., “I don’t expect to get what I really want”, “My future seems dark to me”). The BHS has demonstrated strong psychometric properties in adolescent samples and had an internal consistency of .91 in this sample.
The Children’s Depression Rating Scale—Revised (CDRS-R; Poznanski and Mokros, 1996) is a semi-structured interview that assesses depressive symptoms for the previous two weeks. The CDRS-R has demonstrated strong validity and reliability in studies with adolescents. Inter-interviewer reliability for total scores was very high (mean alpha across raters was .98).
The Multidimensional Anxiety Scale for Children (MASC; March, 1997) is a 39-item self-report scale designed to assess a broad spectrum of anxiety symptoms. The internal consistency coefficient for the total score used in this study was .73.
The Personal Experiences Screen Questionnaire (PESQ; Winters, 1991) is a self-report measure used to screen for adolescent abuse of alcohol or other substances. The PESQ Problem Severity scale has demonstrated adequate reliability and validity for identifying problem substance usage. The Problem Severity scale in this sample had an internal consistency of .94.
The Child and Adolescent Functional Assessment Scale (CAFAS; Hodges and Wong, 1996) is administered to parents and assesses their child’s functional impairment across settings (e.g., school, home, community). The CAFAS has established strong inter-rater reliability, as well as construct and concurrent validity. Inter-rater reliability for CAFAS subscales in this study were high (mean alpha across raters was .90).
Psychiatric rehospitalization was assessed using two questions inquiring if a participant was in a psychiatric hospital or a general hospital for psychiatric or emotional problems. Rehospitalization was assessed at 6 weeks, 3 months, 6 months, and 12 months.
Procedure
Data for the present study were drawn from a randomized psychosocial intervention trial for suicidal adolescents following psychiatric hospitalization [citation removed for blind review]. Youth were consecutively enrolled. After consultation with hospital staff, study staff approached youth ages 13–17 who met inclusion/exclusion criteria for eligibility. Inclusion in the parent study was determined by parent or adolescent report of an adolescent suicide attempt during the past month, or suicidal ideation characterized by persistence or a specific plan, as reported on the Diagnostic Interview Schedule for Children—Version IV. Exclusion criteria included severe cognitive impairment, direct transfer to a medical unit or residential placement, residence more than a one-hour drive from the study site, and no legal guardian available. Of the 1,050 potentially eligible patients, 43% were enrolled in the intervention trial. The primary reasons for refusal included: no interest in research (60%); feeling too busy/overwhelmed at the time (21%); and other reasons (20%). Chi-square analyses indicated no demographic differences by consent status. Thirteen adolescents were excluded from all analyses because they did not complete the YSR. Eighty adolescents were missing data for post-discharge outcomes and were excluded from longitudinal analyses. Participants with and without data at each time point did not differ on demographic characteristics or YSR profile variables (all Chi-square tests p > .1). There were no intervention effects on likelihood of suicide attempts or rehospitalization compared to the control condition. Study findings did not change when covarying for intervention group (details available from authors).
Data Analysis
Data analysis proceeded in two steps to examine cross-sectional and longitudinal data. First, YSR psychopathology profiles were identified using latent profile analysis using Mplus version 6.1. Conceptually comparable to cluster analysis, latent profile analysis is a person-centered approach that identifies subgroups of participants on the basis of multiple characteristics and flexibly accommodates missing data. Indicators consisted of T-scores for YSR subscales: Anxious/Depressed, Withdrawn/Depressed, Somatic Complaints, Attention Problems, Aggressive Behavior, and Rule-Breaking Behavior. We determined the number of optimal profiles based on established statistical fit indices as well as the number of distinct and clinically meaningful subgroups. Specifically, the fit indices used were the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), sample-size adjusted BIC (aBIC), the Lo-Mendell-Rubin-Adjusted Likelihood Ratio Test (LMR-A LRT), and Bootstrapped Likelihood Ratio Test (BLRT). Lower AIC, BIC, and aBIC values and statistically significant LMR-A LRT and BLRT values indicate improved model fit. After identifying YSR profiles, we compared profiles on baseline clinical characteristics to examine concurrent validity utilizing one-way analysis of variance (ANOVA) with pairwise comparisons and Chi-square tests. On the basis of prior literature (Zahn-Waxler et al., 2008), we anticipated gender differences in psychopathology and YSR subscales. We conducted gender-stratified analyses to allow for greater sensitivity in detecting psychopathology profiles. Results were then consolidated following latent profile enumeration.
Second, two sets of longitudinal analyses were conducted to assess whether YSR psychopathology profiles prospectively predicted (1) suicide attempts and (2) psychiatric rehospitalization following discharge. Data were analyzed using multivariate logistic regressions for outcomes occurring within 3 months and 12 months of index hospitalization.2 All models included NSSI history and multiple attempter status as covariates because these are robust prospective predictors of suicide-related outcomes (Hamza et al., 2012; Lopez-Castroman et al., 2011; Mendez-Bustos et al., 2013) and their inclusion allows for inferences about the incremental predictive validity of YSR profiles.
Results
Baseline Latent Profile Analysis
Four psychopathology profiles emerged: moderately (n=74, 17.1%) and severely dysregulated (n=47, 10.9%), primarily internalizing (n=127, 29.3%), and subclinical (n=185, 42.7%; see Table 1).YSR subscale scores aligned with the profile enumerations (see Figure 1). The two dysregulated profiles had clinically elevated scores on the Anxious/Depressed, Attention Problems, and Aggressive Behavior subscales. The internalizing profile only had elevations on the Anxious/Depressed subscales, and the subclinical profile was characterized by scores that were below clinical thresholds. The prevalence trends were similar between males and females.
Table 1.
Model Fit Comparisons.
| Number of Profiles | Log Likelihood | AIC | BIC | aBIC | Entropy | LMR-A P Value | BLR P Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | |
| 1 | −3486.58 | −8897.21 | 7005.16 | 17826.41 | 7050.15 | 17886.20 | 6999.56 | 17835.45 | – | – | – | – | – | – |
| 2 | −3401.71 | −8620.97 | 6853.42 | 17291.95 | 6923.73 | 17385.36 | 6844.68 | 17306.07 | .81 | .81 | .01 | <.001 | <.0001 | <.0001 |
| 3 | −3371.46 | −8520.40 | 6810.92 | 17108.80 | 6906.54 | 17235.84 | 6799.03 | 17128.01 | .82 | .86 | .33 | <.001 | <.0001 | <.0001 |
| 4 | −3346.67 | −8480.39 | 6779.34 | 17046.78 | 6900.26 | 17207.45 | 6764.30 | 17071.07 | .87 | .82 | .39 | .19 | <.0001 | <.0001 |
| 5 | −3331.72 | −8457.10 | 6767.44 | 17018.20 | 6913.68 | 17212.50 | 6749.26 | 17047.58 | .82 | .84 | .47 | .44 | .04 | <.0001 |
Notes. AIC = Akaike Information Criterion. BIC = Bayesian Information Criterion. aBIC = sample-size adjusted BIC. LMR-A Lo-Mendell-Rubin-Adjusted Likelihood Ratio Test. BLR = Bootstrapped Likelihood Ratio Test. Lower AIC, BIC, and aBIC values and significant LMR-A and BLR p-values indicate relatively better model fit. As simulation studies have demonstrated that BIC and BLR are the relatively more robust indicators, these were weighted most heavily in model selection.
Figure 1.
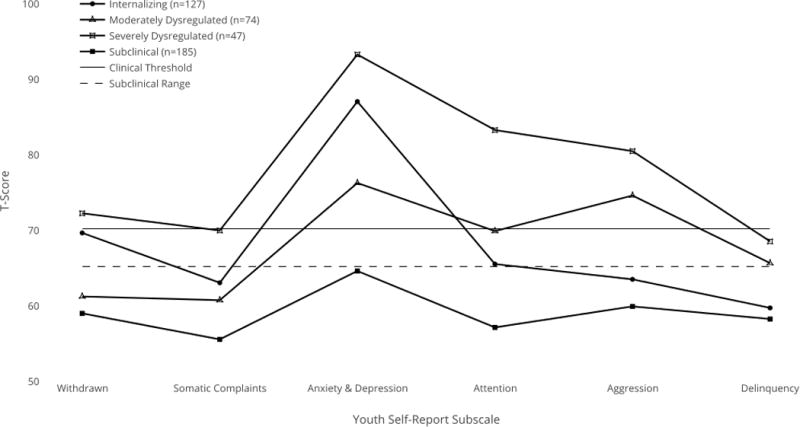
Youth Self-report T-Scores for each psychopathology profile. The profiles are: Internalizing (n=127); Moderately Dysregulated (n=74); Severely Dysregulated (47); and Subclinical (n=185). T-Scores above 70 indicate clinical severity.
There was a main effect of psychopathology profile for baseline scores on the SIQ-Jr., BHS, CDRS, MASC, PEQ-S, and CAFAS, with most pairwise comparisons being statistically significant in a Tukey test (see Table 2), providing further evidence of concurrent validity. Subclinical, internalizing, moderately dysregulated, and severely dysregulated profiles were largely distinguished by respectively more severe clinical presentations at baseline hospitalization. Severely dysregulated and primarily internalizing youth reported the highest rates of histories of NSSI and multiple suicide attempts at baseline.
Table 2.
Comparison of Psychopathology Profiles at Baseline Hospitalization
| Profile 1: | Profile 2: | Profile 3: | Profile 4: | |||
|---|---|---|---|---|---|---|
| Subclinical | Internalizing | Moderately Dysregulated | Severely Dysregulated | Significant | ||
| n=185 | n=127 | n=74 | n=47 | Test Statistic | Pairwise Comparisons | |
| Sex, n (%) | ||||||
| Female | 124 (67.0) | 85 (66.9) | 59 (79.7) | 42 (89.4) | 12.9** | – |
| Male | 61 (33.0) | 42 (33.1) | 15 (20.3) | 5 (10.6) | ||
| Non-Suicidal Self-Injury, n (%) | 94 (50.8) | 88 (69.2) | 38 (51.4) | 35 (74.5) | 17.1** | – |
| Suicide Attempt History | 21.0** | – | ||||
| Ideation | 48 (25.9) | 30 (23.6) | 26 (35.1) | 9 (19.1) | ||
| One Attempt | 80 (43.2) | 39 (30.7) | 21 (28.4) | 10 (21.3) | ||
| Multiple Suicide Attempts Youth Self-Report, Mean (SD) | 57 (30.8) | 58 (45.7) | 27 (36.5) | 28 (59.6) | ||
| Anxious/Depressed | 64.4 (7.4) | 86.9 (8.4) | 76.1 (9.0) | 93.1 (7.8) | 274.6*** | 1 < 2 < 3 < 4 |
| Withdrawn/Depressed | 58.8 (5.6) | 69.5 (7.8) | 61.1 (5.9) | 72.1 (8.9) | 90.8*** | 1 < 2, 3 < 4 |
| Somatic Complaints | 55.4 (5.8) | 62.9 (6.5) | 60.6 (7.2) | 69.8 (9.7) | 69.9*** | 1 < 2, 3 < 4 |
| Attention Problems | 56.9 (6.2) | 65.4 (7.2) | 69.7 (9.7) | 83.1 (7.7) | 178.1*** | 1 < 2 < 3 < 4 |
| Delinquency | 58.1 (5.9) | 59.6 (6.1) | 65.5 (5.3) | 68.4 (6.5) | 55.6*** | 1, 2 < 3 < 4 |
| Aggressive Behavior | 59.8 (7.3) | 63.3 (8.1) | 74.4 (6.7) | 80.3 (10.2) | 125.7*** | 1 < 2 < 3 < 4 |
| Suicide Ideation Questionnaire Jr, Mean (SD) | 36.0 (20.4) | 54.7 (16.8) | 47.7 (20.2) | 62.1 (18.1) | 36.8*** | 1 < 3 < 2, 4 |
| Beck Hopelessness Scale, Mean (SD) Children’s | 6.5 (5.2) | 11.3 (5.5) | 8.4 (5.8) | 11.5 (5.5) | 24.2*** | 1, 3 < 2, 4 |
| Depression Rating Scale, Mean (SD) | 53.5 (11.6) | 67.6 (10.5) | 62.2 (9.7) | 71.7 (9.9) | 61.1*** | 1 < 3 < 2 < 4 |
| Multidimensional Anxiety Scale for Children, Mean (SD) | 35.4 (15.5) | 55.4 (16.3) | 48.2 (17.1) | 59.7 (16.1) | 53.1*** | 1 < 3 < 2, 4 |
| Personal Experiences Screen Questionnaire, Mean (SD) | 25.8 (10.3) | 27.8 (11.4) | 32.8 (12.8) | 32.3 (13.1) | 8.9*** | 1, 2 < 3, 4 |
| Child and Adolescent Functional Assessment Scale, Mean (SD) | 101.3 (36.5 | 99.1 (30.8) | 122.2 (26.5) | 119.3 (38.9) | 10.5*** | 1, 2 < 3, 4 |
Note. Group difference statistics are for Chi-square tests for categorical variables and F-tests for continuous variables.
p < .10.
p < .05.
p < .01.
p < .001.
Longitudinal Analyses
The clinical differences between profiles observed at baseline were also observed at 3-month follow-up (see Table 3). Similar patterns were observed at 12 month-follow-up but were statistically attenuated. Sensitivity and specificity of screening criteria were also assessed within the sample (Table 4). Latent profiles demonstrated poor sensitivity and specificity in predicting future risk. In all logistic regressions, the subclinical profile served as the reference group and NSSI and multiple attempter status were included as covariates. YSR dysregulation profiles were trend-level predictors of suicide attempts at 3 months (moderately dysregulated odds ratio [OR] = 3.2, 95% confidence interval [CI]: .9–11.8; severely dysregulated OR = 3.6, 95% CI: .9–14.1) but not 12 months (moderately dysregulated OR = 1.7; 95% CI: 0.8–3.9; severely dysregulated OR 1.6, 95% CI: .6–4.0). The dysregulation profiles were not associated with rehospitalization post-discharge. In post-hoc analyses combining the two dysregulation groups into one group to increase statistical power, results were comparable. YSR dysregulation profile was a significant predictor of suicide attempts at 3 months (OR = 4.1; 95% CI: 1.2–13.6) but was not associated with suicide attempts at 12 months or rehospitalization at 3 or 12 months.
Table 3.
Multivariate Logistic Regression Analysis Predicting Post-Hospitalization Outcomes
| Rehospitalization | Suicide Attempt | ||||
|---|---|---|---|---|---|
|
| |||||
| 3 Months | 12 Months | 3 Months | 12 Months | ||
|
| |||||
| Youth Self-Report Profile | |||||
| Subclinical | Reference | Reference | Reference | Reference | |
| Internalizing | 2.1 (1.1–4.1)* | 2.6 (1.5–4.7)** | 4.7 (1.4–15.2)* | 2.8 (1.4–5.8)** | |
| Moderately Dysregulated | 1.3 (.6–2.7) | 1.4 (.7–2.7) | 3.2 (.9–11.8)^ | 1.7 (.8–3.9) | |
| Severely Dysregulated | 1.5 (0.6–3.5) | 1.5 (.7–3.1) | 3.5 (.9–14.1)^ | 1.6 (.6–3.9) | |
| Suicide Attempt History | |||||
| Absent | Reference | Reference | Reference | Reference | |
| Single Attempt | 1.4 (0.7–2.9) | 1.6 (0.8–3.0) | 0.9 (0.3–2.6) | 0.7 (0.3–1.5) | |
| Multiple Attempts | 1.4 (0.7–2.7) | 1.8 (0.9–3.3)^ | 1.3 (0.5–3.5) | 1.3 (0.6–2.5) | |
| NSSI History | |||||
| Absent | Reference | Reference | Reference | Reference | |
| Present | 1.1 (0.6–2.1) | 1.9 (1.1–3.2)* | 1.0 (0.4–2.6) | 1.1 (0.6–2.0) | |
p < .10.
p < .05.
p < .01.
Table 4.
Sensitivity and Specificity of Youth Self-Report Profile in Predicting Suicide Attempts and Rehospitalization
| Suicide Attempt | Rehospitalization | |||
|---|---|---|---|---|
|
|
||||
| Sensitivity | Specificity | Sensitivity | Specificity | |
| Subclinical | 0.27 (17/64) | 0.53 (284/289) | 0.31 (35/112) | 0.51 (124/241) |
| Moderately Dysregulated | 0.40 (26/64) | 0.85 (246/289) | 0.13 (15/112) | 0.83 (201/241) |
| Severely Dysregulated | 0.19 (12/64) | 0.89 (256/289) | 0.13 (15/112) | 0.89 (214/241) |
| Internalizing | 0.14 (9/64) | 0.73 (211/289) | 0.42 (47/112) | 0.76 (184/241) |
Sensitivity and specificity reflect the proportions of youth who did and did not report suicide attempts and rehospitalization during the follow-up period. Counts for each are provided in parentheses.
The internalizing profile was associated with suicide attempts and psychiatric hospitalizations post-discharge. The internalizing profile predicted suicide attempts at 3 months (OR = 4.7; 95% CI: 1.4–15.3) and at 12 months (OR = 2.9; 95% CI: 1.4–5.9). Additionally, the internalizing profile predicted psychiatric rehospitalization by 3 months (OR = 2.1; 95% CI: 1.1–4.1) and 12 months (OR = 2.6; 95% CI: 1.4–4.5). History of NSSI also predicted rehospitalization by 12 months (OR = 1.9; 95% CI: 1.1–3.2).
Discussion
Youth suicidal behavior is difficult to predict and to prevent, particularly among high risk samples (Asarnow and Miranda, 2014; Brent et al., 2013). A substantial body of literature has documented that adolescents receiving higher levels of care such as emergency room visits and psychiatric hospitalization are likely to have a recurrences of psychiatric crises and suicide attempts up to a year following discharge, with the initial 3 months being particularly high risk (Troister et al., 2008). Prior research has shown that varying comorbid psychopathology profiles are associated with multiple suicide-related outcomes (Brook et al., 2015; Olino et al., 2012). This study is the first, to our knowledge, to examine cross-sectional and longitudinal associations of the YSR psychopathology profiles with suicide-related outcomes among psychiatrically hospitalized suicidal adolescents. In keeping with study hypotheses, multiple psychopathology profiles emerged that were differentially associated with key suicide-related outcomes at baseline and over the one-year follow-up period. While dysregulated profiles characterized by comorbid internalizing and externalizing symptoms were associated with significant impairment at baseline, a primarily internalizing profile had much stronger associations with post-discharge suicide-related outcomes.
Contrary to study hypotheses, relationships between the dysregulation profile and suicide attempts and rehospitalization were weaker than anticipated (p < .1) and were attenuated over time. This may indicate a temporal clustering of suicidal behavior for youth with this profile. This profile was not associated with rehospitalization at any time point. Taken together, these results suggest that a pervasive psychopathology profile at psychiatric hospitalization may signal somewhat specific and time-limited relationships for the recurrence of suicidal crises among already suicidal adolescents. The dysregulation profile may also reflect a more labile and reactive structure of psychopathology that is driven by difficulty regulating intense but transient aversive states.
This pattern of findings also indicates that the dysregulation profile has weaker associations with suicide-related outcomes within a high risk sample than in community samples. As the dysregulation profile has been associated with personality disorder traits and diagnoses (Bellani et al., 2012), this symptom profile may capture suicidal youth who are prone to problematic disinhibited behavior in general. These youth may go on to have other behaviors that are also impairing but not necessarily captured here (e.g. relational and physical aggression, delinquency). The dysregulation profile at baseline may be associated with a more generalized course of behavior problems rather than ongoing suicidal behavior specifically.
Notably, a primarily internalizing psychopathology profile was also prevalent within this sample. This profile was characterized principally by elevations in anxious and depressed symptoms without clinically significant withdrawn/depressed, somatic, attention problem, aggressive, or rule-breaking behavior symptoms. The internalizing profile predicted future suicide attempts and rehospitalization across time. Given the breadth and persistence of outcomes for this group, marked anxious and depressed symptoms may reflect a pattern of chronic and treatment-resistant negative affect and hyper-arousal. Additionally, severe internalizing symptoms are associated with more ruminative cognitive styles (Nolen-Hoeksema, 2012). As duration of suicidal ideation predicts suicide attempts (Horwitz et al., 2015), youth with the internalizing profile may be more likely to transition from passive ideation to plans and attempts if their suicidal thoughts become perseverative in nature For youth with severe internalizing symptoms, interventions that facilitate greater cognitive flexibility and decreasing agitation may be helpful in interrupting suicidal rumination. More broadly, depressed mood is a key driver of suicide-related outcomes and morbidity. Sample inclusion criteria also contribute to these results. The overwhelming majority (87.9%) of participants met criteria for a depressive disorder, which likely strengthened the relationships between the internalizing profile and post-discharge outcomes.
Limitations
Findings from this study should be interpreted with caution due to several limitations. Patterns of findings differed somewhat for suicide attempts and rehospitalization, which are necessarily correlated. Adolescents in this study were psychiatrically hospitalized and enrolled in a randomized trial of a psychosocial intervention. Although youth and families declining study participation were similar in demographic characteristics, they may differ in other aspects that may influence clinical outcomes. That is, higher risk youth and families may be more likely to opt out of research studies. Further, the gender distribution of this sample is a limitation. The majority (72%) of youth in this sample were female. Additionally, our measure of NSSI was limited to the presence or absence of NSSI and did not capture more nuanced aspects that may be more proximally related to suicidal behavior such as frequency of episodes or number of methods (Hamza et al., 2012). Similarly, our measurement of suicidal behavior was limited to actual suicide attempts. Preparatory behavior, interrupted attempts, and aborted attempts are also clinically meaningful post-discharge outcomes but were not assessed within this study. Further, although the rates of suicide attempts and rehospitalization are comparable to prior research, the relatively small number of YSR profiles limited statistical power. These findings should be examined within larger high-risk samples to disentangle differences between dysregulation profiles. Additionally, the clinical utility of these YSR psychopathology profiles should be subjected to further examination in randomized controlled trials to assess potential differential treatment responses to intervention.
Strengths
These cross-sectional and longitudinal findings replicate and extend past research in several notable ways. First, the use of multiple indices of psychopathology across internalizing and externalizing domains facilitated the identification of several clinically distinct profiles of psychopathology within a high-risk clinical sample. Many past studies have noted elevated rates of many forms of psychopathology among suicidal adolescents, and our results indicate that the YSR is one means by which to parse heterogeneity. Second, the psychopathology profiles, particularly the internalizing profile, had short-term predictive validity with respect to relevant clinical outcomes. Although the YSR may be prohibitively long for use in emergency services for screening and triage, it may be informative for planning interventions. For many suicidal adolescents, the period following discharge from psychiatric hospitalization is marked by a pronounced need for services. Third, we examined YSR psychopathology profiles within a clinically high-risk sample. Previous examinations have been with samples in which there is low to moderate risk for suicide specifically. We found modest and time-limited associations between the dysregulation profile and suicide attempts and psychiatric rehospitalization. This may reflect state- and trait-level impulsivity in general rather than marked risk for suicidal behavior in particular. Fourth, the sample size is large relative to most studies of youth suicidal behavior, particularly those involving clinical and higher risk samples. All youth within the study reported recent suicide ideation, and the majority reported at least one lifetime attempt. The large and high-risk aspects of the sample facilitated the multivariate analyses to be conducted with greater precision. The latent variable analyses conducted accommodated missing data, which prevented biasing results that may have arisen from omission of partial cases. Furthermore, the utilization of both cross-sectional and longitudinal analyses facilitates inferences across time rather than being circumscribed within the time of psychiatric crisis.
Future Directions
It is well-established that more severe psychopathology in general (including co-occurring internalizing and externalizing symptoms) confers greater risk for suicidal behavior among population, community, and outpatient clinical samples (May and Klonsky, 2016; Mendez-Bustos et al., 2013; Nock et al., 2008). This study extends these findings by examination of YSR psychopathology profiles within an inpatient sample. Less is known specifically about acutely suicidal youth and factors that differentiate whose risk will remit or recur. This is particularly concerning as crises are disruptive for several reasons including a number of safety concerns for the youth and their families, further financial burden for health services, and disruptions in adolescents’ usual routine (e.g. school, peer involvement). Similar to the broader literature, studies examining recurrent risk have identified more severe psychopathology and related factors (e.g. trauma exposure, poverty, family history) rather than combinations that may uniquely contribute to risk. Further, previous studies have implicated behavioral disinhibition and a potential driver of future risk (May and Klonsky, 2016; Nock et al., 2013; Van Orden et al., 2010). This study finds that both dysregulated and internalizing symptom profiles are markers of chronicity within an already high risk sample. However, impairment in the dysregulation profile was most pronounced at baseline with some associations shortly after discharge.
The severe internalizing symptom group was associated with enduring and recurrent risk at all time points. Clinically, this is notable because the absence of behavioral risk indicators does not necessarily indicate a less chronic risk pattern. Previous research has implicated behavioral impulsivity as a salient marker of risk but our findings suggest that acute depressed/anxious states also warrant attention. This particular symptom profile may be indicative of an internal agitation and implacable psychache that drives suicidal thoughts and behavior. Among youth who have already experienced acute psychiatric crisis, pronounced internalizing symptoms at hospitalization may signal an unrelenting trajectory that may be resistant to outpatient treatment and prone to persistent suicide risk. Further research should examine the aspects of the severe internalizing profile that exhibit continuity over time.
Future research should examine both shorter-term and longer-term outcomes of youth with varying psychopathology profiles including the internalizing profile. As demonstrated here and in other studies, marked impairment in multiple domains is associated with suicide-related outcomes. Within high-risk samples the relationship between mood and externalizing symptoms may vary somewhat in predicting acute and chronic risk. Future behavior may differ as a function of the etiology of externalizing symptoms. For instance, mood symptoms in the presence of reactive aggression driven by PTSD may predict a different trajectory of suicidal behavior compared to proactive aggression in conduct disorder (Seguin et al., 2014). When examining sensitivity and specificity of the YSR profiles, profiles did not clearly differentiate risk, underscoring the need for future efforts. Future research should consider use of data reduction methods to identify the subset of items on the YSR and similar broadband instruments that predict suicidal behavior in the short-term.
As longitudinal cohort studies have also found that the dysregulation profile predicts suicide-related outcomes (Bellani et al., 2012), these data could be joined with national population registries to assess relative mortality rates as well. Mental health service providers utilizing the YSR could examine the extent to which YSR profiles may be informative for treatment matching (e.g. cognitive behavioral vs. interpersonal psychotherapy),sequencing of multimodal interventions (e.g. parent-based interventions preceding vs. concurrent with individual therapy), and length. More generally, youth with severe internalizing symptoms and comorbid psychopathology have pronounced vulnerability to other adolescent risk behaviors including but not limited to problematic substance use, eating pathology, HIV-transmission behaviors, and delinquency (Pena et al., 2012). Future studies should examine mechanisms by which youth with internalizing and comorbid psychopathology patterns have a generalized liability to adverse outcomes and ascertain which mechanisms would be amenable to treatment and preventative intervention.
Conclusion
The present study is among the first to examine YSR psychopathology profiles among acutely suicidal, psychiatrically hospitalized adolescents. Both severe internalizing and dysregulated (comorbid internalizing and externalizing) patterns were observed. An internalizing profile predicted future suicide attempts and rehospitalization at follow-up whereas dysregulated profiles had time-limited associations with suicide attempts. These findings highlight a need for examining the heterogeneous presentations of suicidal youth. Future studies examining how psychopathology profiles differentially respond to intervention would assist in more effective treatment matching for high risk youth.
Highlights.
The Youth Self-Report psychopathology profiles predict suicide-related outcomes
The dysregulation profile is common among hospitalized suicidal youth
Dysregulated profiles predict suicide attempts within three months of discharge
Internalizing profiles predict suicide attempts and rehospitalization following discharge
Future research into psychopathology profiles may facilitate treatment matching
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
We discuss comorbid internalizing and externalizing disorder symptoms broadly as well as particular patterns of comorbidity. For consistency with prior literature, our use of the term “dysregulated” refers specifically to the co-occurrence of elevated scores on the Anxious/Depressed, Attention Problems, and Aggressive Behavior subscales of the Youth Self-Report (YSR) and Child Behavior Checklist (CBCL).
The results of logistic regression are consistent with Cox regression predicting time to suicide attempt. See supplemental table for details. Dates of rehospitalizations were not recorded.
References
- Achenbach TM. Manual for the Youth Self-Report and 1991 rofile 1991 [Google Scholar]
- Althoff RR, Ayer LA, Rettew DC, Hudziak JJ. Assessment of dysregulated children using the Child Behavior Checklist: A receiver operating characteristic curve analysis. Psychol Assess. 2010a;22:609–617. doi: 10.1037/a0019699.Assessment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Althoff RR, Rettew DC, Ayer LA, Hudziak JJ. Cross-informant agreement of the Dysregulation Profile of the Child Behavior Checklist. Psychiatry Res. 2010b;178:550–5. doi: 10.1016/j.psychres.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Miranda J. Improving care for depression and suicide risk in adolescents: innovative strategies for bringing treatments to community settings. Annu Rev Clin Psychol. 2014;10:275–303. doi: 10.1146/annurev-clinpsy-032813-153742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: A biology × sex × environment interaction model of antisocial and borderline traits. Dev Psychopathol. 2009;21:735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck hopelessness scale. San Antonio, TX: Psychol Corp; 1988. [Google Scholar]
- Bellani M, Negri G, Brambilla P. The dysregulation profile in children and adolescents: A potential index for major psychopathology? Epidemiol Psychiatr Sci. 2012;21:155–9. doi: 10.1017/S2045796011000849. [DOI] [PubMed] [Google Scholar]
- Bentley KH, Franklin JC, Ribeiro JD, Kleiman EM, Fox KR, Nock MK. Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: A meta-analytic review. Clin Psychol Rev. 2016;43:30–46. doi: 10.1016/j.cpr.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, McMakin DL, Kennard BD, Goldstein TR, Mayes TL, Douaihy AB. Protecting Adolescents From Self-Harm: A Critical Review of Intervention Studies. J Am Acad Child Adolesc Psychiatry. 2013;52:1260–1271. doi: 10.1016/j.jaac.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brezo J, Barker ED, Paris J, Hébert M, Vitaro F, Tremblay RE, Turecki G, He M, Vitaro F, Tremblay RE, Turecki G, Hébert M. Childhood Trajectories of Anxiousness and Disruptiveness as Predictors of Suicide Attempts. Arch Pediatr. 2011;162:1015–1021. doi: 10.1001/archpedi.162.11.1015. [DOI] [PubMed] [Google Scholar]
- Brook JS, Lee JY, Finch SJ, Brook DW. Conjoint trajectories of depressive symptoms and delinquent behavior predicting substance use disorders. Addict Behav. 2015;42:14–19. doi: 10.1016/j.addbeh.2014.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Caluwé E, Decuyper M, De Clercq B. The child behavior checklist dysregulation profile predicts adolescent DSM-5 pathological personality traits 4 years later. Eur Child Adolesc Psychiatry. 2013;22:401–411. doi: 10.1007/s00787-013-0379-9. [DOI] [PubMed] [Google Scholar]
- Diamond G, Levy S, Bevans KB, Fein JA, Wintersteen MB, Tien A, Creed T. Development, validation, and utility of internet-based, behavioral health screen for adolescents. Pediatrics. 2010;126:e163–e170. doi: 10.1542/peds.2009-3272. [DOI] [PubMed] [Google Scholar]
- Hamza CA, Stewart SL, Willoughby T. Examining the Link between Nonsuicidal Self-Injury and Suicidal Behavior: A Review of the Literature and an Integrated Model. Clin Psychol Rev. 2012;32:482–495. doi: 10.1016/j.cpr.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Hawton K, Saunders KEA, Connor RCO. Self-harm and suicide in adolescents. Lancet. 2012;379:2373–2382. doi: 10.1016/S0140-6736(12)60322-5. [DOI] [PubMed] [Google Scholar]
- Hodges K, Wong MM. Psychometric characteristics of a multidimensional measure to assess impairment: The Child and Adolescent Functional Assessment Scale. J Child Fam Stud. 1996;5:445–467. [Google Scholar]
- Holtmann M, Buchmann AF, Esser G, Schmidt MH, Banaschewski T, Laucht M. The Child Behavior Checklist-Dysregulation Profile predicts substance use, suicidality, and functional impairment: A longitudinal analysis. J Child Psychol Psychiatry. 2011;52:139–47. doi: 10.1111/j.1469-7610.2010.02309.x. [DOI] [PubMed] [Google Scholar]
- Horwitz AG, Czyz EK, King CA. Predicting future suicide attempts among adolescent and emerging adult psychiatric emergency patients. J Clin Child Adolesc Psychol. 2015;44:751–761. doi: 10.1080/15374416.2014.910789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan ND. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kim J, Carlson Ga, Meyer SE, Bufferd SJ, Dougherty LR, Dyson MW, Laptook RS, Olino TM, Klein DN. Correlates of the CBCL-dysregulation profile in preschool-aged children. J Child Psychol Psychiatry. 2012;53:918–26. doi: 10.1111/j.1469-7610.2012.02546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Berona J, Czyz EK, Horwitz AG, Gipson PY. Identifying Adolescents at Highly Elevated Risk for Suicidal Behavior in the Emergency Department. J Child Adolesc Psychopharmacol. 2015;25:100–108. doi: 10.1089/cap.2014.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Jiang Q, Czyz EK, Kerr DCR. Suicidal ideation of psychiatrically hospitalized adolescents has one-year predictive validity for suicide attempts in girls only. J Abnorm Child Psychol. 2014;42:467–477. doi: 10.1007/s10802-013-9794-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Castroman J, Perez-Rodriguez MDLM, Jaussent I, Alegria Aa, Artes-Rodriguez A, Freed P, Guillaume S, Jollant F, Leiva-Murillo JM, Malafosse A, Oquendo Ma, de Prado-Cumplido M, Saiz-Ruiz J, Baca-Garcia E, Courtet P. Distinguishing the relevant features of frequent suicide attempters. J Psychiatr Res. 2011;45:619–25. doi: 10.1016/j.jpsychires.2010.09.017. [DOI] [PubMed] [Google Scholar]
- March JS. Manual for the Multidimensional Anxiety Scale for Children (MASC) 1997 doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- May AM, Klonsky ED. What Distinguishes Suicide Attempters From Suicide Ideators? A Meta-Analysis of Potential Factors. Clin Psychol Sci Pract. 2016;23:5–20. doi: 10.1111/cpsp.12136. [DOI] [Google Scholar]
- Mendez-Bustos P, De Leon-martinez V, Miret M, Baca-Garcia E, Lopez-castroman J, de Leon-Martinez V, Miret M, Baca-Garcia E, Lopez-Castroman J. Suicide reattempters: A systematic review. Harv Rev Psychiatry. 2013;21:281–95. doi: 10.1097/HRP.0000000000000001. [DOI] [PubMed] [Google Scholar]
- Nock MK. Self-injury. Annu Rev Clin Psychol. 2010;6:339–63. doi: 10.1146/annurev.clinpsy.121208.131258. [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and Suicidal Behavior. Epidemiol Rev. 2008;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Kessler RC, Franklin JC. Risk Factors for Suicide Ideation Differ From Those for the Transition to Suicide Attempt: The Importance of Creativity, Rigor, and Urgency in Suicide Research. Clin Psychol Sci Pract. 2016;23:31–34. doi: 10.1111/cpsp.12133. [DOI] [Google Scholar]
- Nolen-Hoeksema S. Emotion regulation and psychopathology: The role of gender. Annu Rev Clin Psychol. 2012;8:161–187. doi: 10.1146/annurev-clinpsy-032511-143109. [DOI] [PubMed] [Google Scholar]
- Olino TM, Klein DN, Farmer RF, Seeley JR, Lewinsohn PM. Examination of the structure of psychopathology using latent class analysis. Compr Psychiatry. 2012;53:323–332. doi: 10.1016/j.comppsych.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pena JB, Matthieu MM, Zayas LH, Masyn KE, Caine ED. Co-occurring risk behaviors among White, Black, and Hispanic US high school adolescents with suicide attempts requiring medical attention, 1999–2007: Implications for future prevention initiatives. Soc Psychiatry Psychiatr Epidemiol. 2012;47:29–42. doi: 10.1007/s00127-010-0322-z. [DOI] [PubMed] [Google Scholar]
- Poznanski EO, Mokros HB. Children’s Depression Rating Scale - Revised (CDRS-R) 1996 [Google Scholar]
- Reynolds WM, Mazza JJ. Assessment of suicidal ideation in inner-city children and young adolescents: Reliability and validity of the Suicidal Ideation Questionnaire-JR. School Psych Rev. 1999;28:17–30. [Google Scholar]
- Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, Nock MK. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychological Medicine. 2016;46(2):225–36. doi: 10.1017/S0033291715001804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers ML, Ringer FB, Joiner TE. A meta-analytic review of the association between agitation and suicide attempts. Clin Psychol Rev. 2016;48:1–6. doi: 10.1016/j.cpr.2016.06.002. [DOI] [PubMed] [Google Scholar]
- Seguin M, Beauchamp G, Robert M, DiMambro M, Turecki G. Developmental model of suicide trajectories. Br J Psychiatry. 2014;205:120–126. doi: 10.1192/bjp.bp.113.139949. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas C. Parent-informant. New York Columbia Univ; 1998. NIMH DISC-IV. Diagnostic interview schedule for children. [Google Scholar]
- Sharp C, Fonagy P. Practitioner Review: Borderline personality disorder in adolescence - Recent conceptualization, intervention, and implications for clinical practice. J Child Psychol Psychiatry Allied Discip. 2015;56:1266–1288. doi: 10.1111/jcpp.12449. [DOI] [PubMed] [Google Scholar]
- Troister T, Links PS, Cutcliffe J. Review of predictors of suicide within 1 year of discharge from a psychiatric hospital. Curr Psychiatry Rep. 2008;10:60–65. doi: 10.1007/s11920-008-0011-8. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE, Jr, Joiner TE. The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC. Personal experience screening questionnaire. Western psychological services; 1991. [Google Scholar]
- Wintersteen MB, Diamond G, Fein J. Screening for suicide risk in the pediatric emergency and acute care setting. Curr Opin Pediatr. 2007;19:398–404. doi: 10.1097/MOP.0b013e328220e997. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Shirtcliff EA, Marceau K. Disorders of childhood and adolescence: Gender and psychopathology. Annu Rev Clin Psychol. 2008;4:275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Heitzeg MM, Nigg JT. Parsing the Undercontrol/Disinhibition Pathway to Substance Use Disorders: A Multilevel Developmental Problem. Child Dev Perspect. 2011;5:248–255. doi: 10.1111/j.1750-8606.2011.00172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


