ABSTRACT
Objectives: Neuroimaging is contributing to the rising costs of dizziness evaluation. This study examined the rate of central neurological causes of dizziness, relevant clinical predictors, and the costs and diagnostic yields of neuroimaging in dizziness assessment.
Methods: We retrospectively reviewed the records of 521 adult patients who visited the hospital during a 12-month period with dizziness as the chief complaint. Clinical findings were analyzed using Fisher’s exact test to determine how they correlated with central neurological causes of dizziness identified by neuroimaging. Costs and diagnostic yields of neuroimaging were calculated.
Results: Of the 521 patients, 1.5% had dizziness produced by central neurological causes. Gait abnormalities, limb ataxia, diabetes mellitus, and the existence of multiple neurological findings predicted central causes. Cases were associated with gait abnormalities, limb ataxia, diabetes mellitus, and the existence of multiple neurological findings . Brain computed tomography (CT) and magnetic resonance imaging (MRI) were performed in 42% and 9.5% of the examined cases, respectively, with diagnostic yields of 3.6% and 12%, respectively. Nine cases of dizziness were diagnosed from 269 brain scans, costing $607 914.
Conclusion: Clinical evaluation can predict the presence of central neurological causes of dizziness, whereas neuroimaging is a costly and low-yield approach. Guidelines are needed for physicians, regarding the appropriateness of ordering neuroimaging studies.
Abbreviations: OR: odds ratio; CI: confidence interval; ED: emergency department; CT: computed tomography; MRI: magnetic resonance imaging; HINTS: Head impulse, Nystagmus, Test of skew
KEYWORDS: Dizziness, stroke, neuroimaging, cost, vertigo
1. Introduction
Dizziness is the third most common complaint among outpatients [1]. One in five people aged 18–64 years and 24% of the population aged 75–83 years have experienced symptoms of dizziness in the previous month [2,3]. Dizziness/vertigo represented 2.5% of all emergency department (ED) admissions in the 10-year period from 1995–2004 [4]. Otologic and vestibular disorders are the most common causes of dizziness [5–10]. Medications and neurologic, cardiac, hematologic, ophthalmologic, and psychiatric disorders can also cause dizziness [3–11]. At least one in eight patients suffers from more than one cause of dizziness [12].
In 8–18.9% of patients, no cause for the dizziness can be identified [5–10]. In a seminal paper, Drachman and Hart [5] classified all complaints of dizziness into the following four types: (1) vertigo, which is a definite rotational sensation; (2) presyncope, which is a sensation of impending faintness or loss of consciousness; (3) disequilibrium, which is a loss of balance without head sensation; and (4) vague ‘lightheadedness’ that cannot be classified as vertigo, syncope, or disequilibrium. This approach suggests that vertigo has a vestibular cause, presyncope has a cardiovascular cause, disequilibrium has a neurological cause, and nonspecific dizziness has a psychiatric or metabolic cause [13,14]. However, patients’ descriptions of the quality of dizziness can be unreliable and inconsistent. One study showed that 62% of ED patients who experienced dizziness in the week before their visit selected more than one type of dizziness on a multi-response questionnaire, and approximately 52% of the patients chose a different type when retested six minutes later [13]. Vertebrobasilar ischemia and cerebellar stroke can present with vestibular neuritis-related symptoms [15,16]. Dizziness is listed as one of the stroke warning signs that requires an immediate 911 call according to the American Stroke Association website [17]. The use of brain computed tomography (CT) and magnetic resonance imaging (MRI) in ED visits for dizziness evaluation increased by 169% in the period between 1995 and 2004 [4]. The proportion of patients with serious central nervous system pathologies, including strokes that cause vertigo-dizziness, did not exceed 3.9% in two large studies [4,18]. The national cost of dizziness evaluations in EDs in the United States was $3.9 billion/year in 2011 compared with $1.1 billion/year in 1993 [19]. The increase in the proportion of dizziness cases receiving diagnostic imaging contributed to this cost [19]. The goal of this study was to examine the patterns of dizziness observed in patients admitted to the Lyndon B. Johnson General Hospital (LBJ), the predictors of central neurological causes based on findings from medical histories and physical examinations, and the impact of the neuroimaging studies on diagnosis and costs.
2. Material and methods
We retrospectively reviewed the electronic records of adult patients aged 18 years or older who visited the ED between 1 January 2011 and 31 December 2011 with chief complaints of dizziness, spinning, disequilibrium, lightheadedness, giddiness, or imbalance. The hospital is a 328-bed community hospital that has been approved by the Accreditation Council for Graduate Medical Education (ACGME) as an accredited residency program. Informed consent was waived by the Institutional Review Board of our institute. We used codes from the International Classification of Diseases, ninth revision (ICD-9) in our search (780.4, 781.2, 386 to 386.2).
We reviewed medical histories, physical examination records, progress notes, consultations notes, neuroimaging (brain CT and MRI) reports, and discharge summaries. Vertigo was used in our study to describe the physical sensation of motion of self or the environment [5]. The neuroimaging findings were correlated with the clinical presentations, and the tests were considered to be diagnostic for dizziness if the imaging results were determined to be responsible for the patients’ complaints. The potential findings included acute infarctions, hemorrhages, demyelinating lesions, brain tumors, and infections. We excluded patients who did not have any of the above-listed symptoms as their chief complaint. Patients with an episode of syncope or loss of consciousness were excluded from the study. We reviewed all of the Harris electronic health records for the study population in the six-month period after the index visit to ensure that strokes and other central neurological diagnoses were not made during this period. We included patients with multiple eligible ED visits during the study period only once, using the time of their first visit for the data. We considered the documented neurological examination complete if it included an examination of the patient’s mental status, muscle power, sensation, deep tendon reflexes, cranial nerves, and coordination. We commented on the frequency of gait examinations and the presence of nystagmus separately from the neurological examinations. The health research program at Harris provided the billing charges that were used in the study.
2.1. Statistical analysis
The data retrieved from the hospital information system were exported to IBM SPSS Ver. 21 (IBM Corp, USA). The standardized data collection form included demographic information (age, sex, race, and smoking status), medical history information (hypertension; diabetes mellitus; arrhythmia; coronary artery disease; benign positional vertigo; previous stroke; history of the present illness, including presenting complaints, e.g., lightheadedness, dizziness, vertigo, giddiness, spinning, imbalance, and accompanying complaints (imbalance)), physical examination findings (nystagmus, limb ataxia, gait abnormalities, and focal neurologic findings), and neuroimaging results. The clinical variables were analyzed for associations with central neurological causes of dizziness identified on brain scans using Fisher’s exact test. Unadjusted odds ratios (ORs) were determined for factors found to have a significant association with the central neurological cause of dizziness (P < 0.05).
3. Results
3.1. Patient population
We reviewed the records of 1313 patients who visited the ED during the study period and identified 521 patients who met our inclusion criteria (Figure 1). The study population’s characteristics are presented in Table 1. The mean age of the patients was 49.3 ± 15.1 years. A total of 301 (57.8%) patients were female, and 220 (42.2%) patients were male. A total of 369 study patients utilized the Harris health system in the six months after the index visit. A total of 103 patients were admitted for additional management, 418 patients were discharged from the emergency room. There were 19 admissions to obtain MRI brain scans. The mean length of stay was 2.7 ± 2.6 days.
Figure 1.
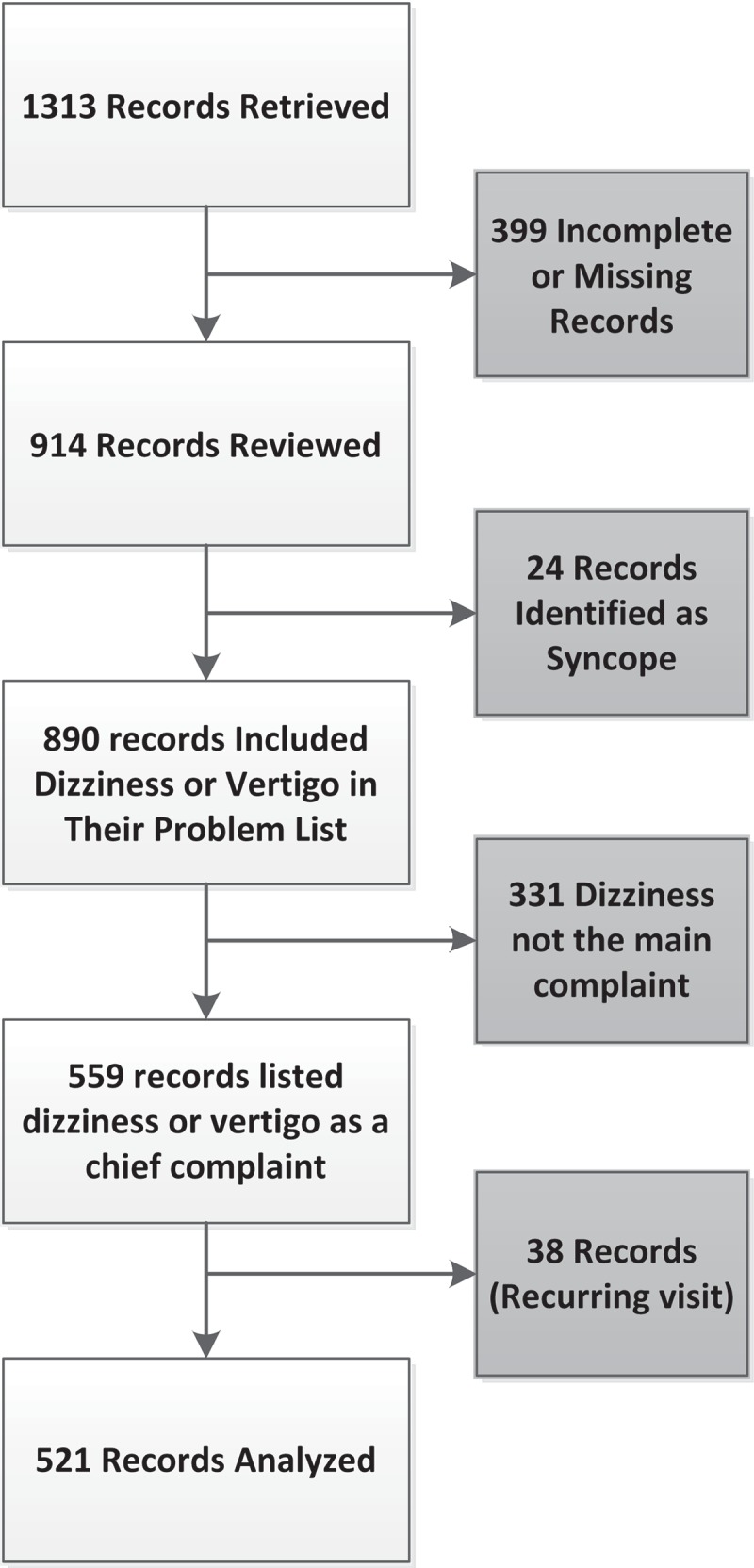
Flow diagram of inclusion of the 521 patients with dizziness.
Table 1.
Characteristics of the study patients.
| Characteristics | Number | Frequency (%) / Mean ± Standard deviation |
|---|---|---|
| Age (years) | 521 | 49.3 ± 15.1 |
| Length of stay (days) | 73 | 2.7 ± 2.6 |
| Gender | ||
| Male | 521 | 220 (42.2) |
| Female | 301 (57.8) | |
| Smoker | 454 | 112 (24.2) |
| No vertiginous dizziness | 521 | 308 (59.1) |
| Vertigo | 521 | 213 (40.9) |
| Past history of dizziness | 521 | 84 (16.1) |
| Diabetes mellitus | 521 | 137 (26.3) |
| Hypertension | 521 | 253 (48.6) |
| Arrhythmia | 521 | 13 (2.5) |
| Congestive heart failure | 521 | 21 (4.0) |
| Coronary artery disease | 521 | 22 (4.2) |
| History of stroke | 520 | 24 (4.6) |
| ER discharge | 521 | 418 (80.2) |
| Admitted | 521 | 103 (19.8) |
3.2. Medical history and physical examination
The medical histories and physical examinations were used to diagnose 60% (n = 316) of all of the study patients and 87% of all of the diagnosed patients. A total of 307 patients received complete neurological examinations. There were 43 patients with nystagmus, 45 with gait abnormalities, 3 with limb ataxia and 14 with more than one neurological finding.
3.3. Imaging studies and consultations
CT scans were performed on 219 (42.0%) patients and yielded a diagnosis in eight (3.6%) patients: cerebellar stroke (n = 3); occipital lobe stroke (n = 1); brain metastases and tumors (n = 3); and cholesteatoma (n = 1). The majority of the abnormal brain CT scans revealed chronic ischemic changes. MRI scans were conducted on 50 patients and yielded a diagnosis in six (12%) patients: cerebellar stroke (n = 3) and brain metastases and tumors (n = 3). Both tests were performed in the same visit for 41 (7.8%) patients.
A neurological consultation was requested for 22 (4.2%) of the 521 patients, and an ENT consultation was requested for seven (1.3%) of the 521 patients.
3.4. Causes of dizziness
There were 363 (69.6%) diagnosed patients and 158 (30.3%) undiagnosed patients. The causes of dizziness and their frequencies in the study population are presented in Table 2.
Table 2.
Dizziness diagnoses in the study.
| Diagnoses | Number of patients (%) |
|---|---|
| Peripheral vestibular and otologic causes: | 199 (38.1%) |
| Benign paroxysmal positional vertigo | 75 (14.39%), |
| (otitis media, otitis externa, cerumen, labyrinthitis, cholesteatoma, Ménière’s disease) | 12 (2.3%), |
| Unspecified peripheral vestibular and otologic etiology | 112 (21.4%) |
| Undiagnosed or symptom-only diagnosis | 158 (30.3%) |
| Medications and illicit drugs | 49 (9.4%) |
| General medical disorders | 87 (16.6.%) |
| Dehydration, hypotension and orthostatic hypotension | 44 (8.4%) |
| Hyperglycemia | 18 (3.4%) |
| Hypertension | 9 (1.7%) |
| Anemia | 9 (1.7%) |
| Hepatic encephalopathy | 1 (0.19%) |
| URI | 2 (0.38%) |
| Uremia | 1 (0.19%) |
| Pregnancy | 1 (0.19%) |
| Lupus | 1 (0.19%) |
| Hyponatremia | 1 (0.19%) |
| Psychiatric diagnosis | 14 (2.6%) |
| Central neurological causes: | 8 (1.5%) |
| Cerebellar stroke | 4 (0.76%) |
| Occipital stroke | 1 (0.19%) |
| Brain tumor | 3 (0.57%) |
| Cardiac disorders | 5 (0.95%) |
| Refractive error | 1 (0.19%) |
3.5. Central neurological versus peripheral causes of dizziness
The patients with central neurological causes of dizziness and vertigo were significantly older and stayed in the hospital for a prolonged period of time (age, 61.1 ± 11.0 years vs. 49.1 ± 15.1 years; P = 0.026; hospital stay, 6.7 ± 6.9 days vs. 2.3 ± 1.6 days). Four (1.8%) of the 220 males and four (1.3%) of the 301 females had a central causes (P = 0.727). Table 3 displays the frequencies of physical examination findings among patients with central and non-central causes of dizziness. The history and physical examination elements that predicted the central causes of dizziness in the statistical analysis are presented in Table 3. These include gait abnormalities (OR, 39.605; 95% CI, 4.7–331.1), limb ataxia (OR, 24.583; 95% CI, 1.9–309.50), having more than one focal neurologic finding (OR, 15.9; 95% CI, 3.4–75.3), and diabetes mellitus (OR, 8.7481; 95% CI, 1.7–43.9). Only 70% of the study population had a follow up with Harris health system and there were no stroke or other central neurological diagnoses during the six-month follow-up period
Table 3.
History and physical examination findings, comparison of the differences in covariates between the central and non-central causes of dizziness, and regression analysis for various predictors of the central cause of dizziness.
| History and physical examination findings | Central cause of dizziness |
P | Odds ratio | Confidence interval (CI) | P | |
|---|---|---|---|---|---|---|
| No | Yes | |||||
| History of dizziness/vertigo | 84/513 (16.4) | 0/8 | 0.366 | 0.2990 | 0.01 to 5.2 | 0.408 |
| Non-vertiginous dizziness | 303/513 (59.1) | 5/8 (62.5) | 1.000 | 1.551 | 0.3 to 4.8 | 0.844 |
| Vertigo | 210/513 (40.9) | 3/8 (37.5) | 1.000 | 0.865 | 0.204 to 3.666 | 0.844 |
| Imbalance | 420/531 (81.9) | 6/8 (75.0) | 0.001 | 0.074 | 0.015 to 0.37 | 0.002 |
| Diabetes mellitus | 131/513 (25.5) | 6/8 (75.0) | 0.005 | 8.7481 | 1.7 to 43.9 | 0.008 |
| Hypertension | 246/513 (48.0) | 7/8 (87.5) | 0.033 | 7.5976 | 0.9 to 62.2 | 0.058 |
| Arrhythmia | 12/513 (2.3) | 1/8 (12.5) | 0.184 | 5.9643 | 0.7 to 52.3 | 0.107 |
| Congestive heart failure | 21/513 (4.1) | 0/8 | 1.000 | 1.3475 | 0.1 to 24.1 | 0.839 |
| Coronary artery disease | 21/513 (4.1) | 1/8 (12.5) | 0.294 | 3.3469 | 0.4 to 28.5 | 0.268 |
| History of stroke | 23/512 (4.5) | 1/8 (12.5) | 0.317 | 3.0373 | 0.359 to 25.730 | 0.308 |
| Gait abnormality | 38/253 (15.0) | 7/8 (87.5) | 0.0005 | 39.605 | 4.7 to 331.1 | 0.0007 |
| Nystagmus | 41/300 (13.7) | 2/7 (28.6) | 0.255 | 2.5268 | 0.5 to 13.5 | 0.277 |
| Tremors/limb ataxia | 2/297 (0.7) | 2/8 14.3) | 0.0035 | 49.2 | 5.9 to 409.7 | 0.0003 |
| More than one neurological finding | 11/303 (3.6) | 3/8 (37.5) | 0.003 | 15.9273 | 3.4 to 75.3 | 0.0005 |
3.6. Costs
A total of $406 646 was spent on 219 brain CT scans, of which only eight yielded positive relevant findings. The billing charges for the eight positive CT scans were $14 848; hence, $50 830 was spent to yield one positive CT brain scan (Table 4).
Table 4.
Cost analysis of neuroimaging.
| Intervention | Number of scans | Total cost (a) | Positive yield | Total cost of positive yield (b) | Variance (a-b) |
|---|---|---|---|---|---|
| Brain CT | 219 | $406 464 | 8 | $14 848 | $391 616 |
| Brain MRI | 50 | $201 50 | 6 | $24 174 | $177 276 |
| CT+MRI | 269 | $607 914 | 14 | $39 022 | $568 892 |
A total of $201 450 was spent on 50 MRI brain scans, of which only six yielded positive relevant findings. The billing charges for the six positive MRI scans were $24 174; hence, $33 575 was spent to yield one positive MRI scan (Table 4).
4. Discussion
The current study obtained data on approximately 521 patients suffering from dizziness who attended the ED of an academic community hospital. The results show that the most common diagnostic categories included peripheral vestibular and otologic causes. Diagnoses based purely on symptoms (e.g., dizziness, lightheadedness, and vertigo) were given to 30% of patients; this constituted the second most common diagnostic category. Central neurological causes were responsible for only 1.5% of cases. CT and MRI brain scans obtained in 42% and 9.5% of the study patients, respectively, yielded diagnoses in 3.6% and 12% of the performed studies, respectively. Gait abnormalities, limb ataxia, the presence of multiple abnormal neurological findings (various combination of gait abnormalities, limb ataxia and nystagmus), and a diagnosis of diabetes mellitus predicted the presence of a central cause of dizziness in this study group. In a nationally representative study, otologic and vestibular diagnoses were the top diagnostic group, and symptom-only diagnoses represented 22.1% of the diagnostic categories [20]. In a prospective study, only 60% of patients who presented to the ED with dizziness had a specific dizziness diagnosis; symptom-only or nonspecific diagnoses were present in 21.1% of the patients [21]. The prevalence of central causes of dizziness and vertigo in the literature is generally low. Studies conducted in dizziness and ambulatory clinics have reported prevalence rates of 0.9–10% [5,7–9], while ED studies have recorded rates of 3.2–6% [4,18,20–23]. Stroke rates of 9.2–10.4% have been reported in studies from stroke units and MRI registries that included cerebellar stroke patients presenting with vertigo and dizziness [16,22]. An ED study that included 24 patients with a mean age of 62.6 years reported a stroke prevalence of 25% [24].
Few studies have reported on findings from medical histories and physical examinations that predicted central causes of dizziness and vertigo [18,21–23]. Gait abnormalities were a predictor of central causes of dizziness in this study. Ataxia, unsteady gaits, slow gaits and inabilities to do tandem gaits were used to describe gait abnormalities in the patient records in our study. Gait abnormalities and imbalance have been strong predictors of central causes of dizziness in several studies [18,21–23]. Imbalance as a complaint was not a predictor in this study. Limb ataxia, which was another predictor in this study, was the second most common neurological examination finding in a study by Navi et al. [23]. This finding was also reported in a study by Drachman and Hart [5]. Having a combination of neurological findings was another predictor. All of our patients with central causes for their dizziness had abnormal findings on their neurological examinations, except for one patient with cerebellar infarction who was reported to have a normal neurological examination. There was no information regarding the presence or absence of nystagmus in this particular case. Chase et al. [22] reported a normal neurological examination, except for the occurrence of nystagmus in two patients with cerebellar infarctions. Lee et al. [16] found that 10.4% of patients with cerebellar stroke who presented with vertigo had only nystagmus and some degree of imbalance when they were examined. All of the patients in the study by Norrving et al. [25] had normal examinations, except for nystagmus. This particular study considered that gait assessment was difficult in patients with acute vertigo and did not comment on it [25].
Dizziness versus vertigo as the chief complaint did not predict a central cause in our study or in other studies [21,22]. Kerber et al. [18] and Navi et al. [23] reported a negative association between dizziness and stroke.
The associations between traditional stroke risk factors and cerebellar stroke in patients with dizziness vary in the literature. Diabetes mellitus was a predictor of central neurological cause in our study and in the study by Cheung et al. [21] Hypertension and a prior history of stroke did not predict stroke in this study or in other studies [22,23]. A prior history of stroke predicted a central cause in the study by Cheung et al. [21] At least two risk factors were present in 72% of patients with stroke in the study by Kerber et al. [18] The patients with central causes of dizziness in our study were older than 50 years of age. Older age has been significantly associated with stroke in several studies [7,18,22,23]. However, 50% of the patients with missed cerebellar infarction in one study that was limited by case selection bias were below 50 years of age [26].
CT/MRI scans were obtained for 18% of patients with dizziness who visited the ED in a nationally representative sample (1995–2004), and a cerebrovascular diagnosis was made in 3.9% of the patients in the study [4]. Recent studies have reported that brain imaging scans are ordered in 27–48% of visits by patients with dizziness, yielding diagnoses in 0.74–7% of patients [23,24,27]. The literature consistently shows that physicians order more CT brain scans than MRI scans in dizziness evaluations despite the known fact that MRI brain scans exhibit better sensitivity in diagnosing stroke (83% versus 26%), especially in posterior circulation stroke, which is usually the concern in these cases [28,29]. Savitz et al. [26] reported that 50% of patients with missed cerebellar stroke in their study had normal CT brain scans. CT brain scans diagnosed four of five patients with posterior circulation stroke in this study, and a scan was not ordered for the fifth patient. The late presentation of the patients could explain the high detection rate in our study. The MRI brain scan was not cost-effective for patients with vertigo who attended a specialized dizziness clinic [30]. Ahsan et al. [27] reported that the money spent on CT and MRI scans over three years for patients with dizziness totaled $1 230 840 and yielded 17 relevant abnormal findings. In the current study, $607 914 was spent on neuroimaging to yield 14 relevant findings in one year. A total of $1 190 864 was spent on brain scans that did not yield a diagnosis in the study by Ahsan et al. [27] versus $568 892 in this study.
This study is limited by its retrospective design, which restricts our ability to interpret the available data. It is likely that we missed stroke and dizziness cases that were not coded with the ICD codes used in our search criteria. The majority of the patients in this study were not examined by a neurologist; hence, a stroke diagnosis might have been missed during the clinical evaluation. The absence of new stroke diagnoses during the six-month follow-up period for 70% of the patients in this study made this possibility less likely. This study took place in a community hospital and reflects the actual experiences in many other community hospitals; many of the previous studies were conducted in tertiary and university centers [15,16,21–23,25,26].
5. Conclusion
Medical history and physical examination were only enough to diagnose two-thirds of our patients. A good medical history and physical examination can improve the selection criteria for brain neuroimaging for evaluating patients with dizziness. In the clinical evaluation of dizziness patients, special attention should be given to research findings that predict central neurological causes. More prospective studies are needed. According to recent research, a three-step bedside oculomotor examination (Head impulse, Nystagmus, Test of Skew [HINTS]) can reliably predict stroke for patient populations with acute vestibular syndrome [31,32]. There is a need to develop guidelines for educating physicians regarding the appropriateness of ordering neuroimaging studies to assess patients with dizziness and vertigo.
Acknowledgments
None.
Biography
All the authors conceived and designed the study, interpreted the data, and critically revised the manuscript for important intellectual content. HA and RG acquired the data. WZ did the analyses, HA and RF wrote the manuscript. All the authors participated in interpretation of the result and critical revision of the manuscript. HA is the guarantor.
Disclosure statement
No potential conflict of interest was reported by the authors.
Disclaimers
This manuscript has not been previously published and is not under consideration for publication elsewhere. We have no conflicts of interest to disclose. All of the authors have read and approved the final version of the manuscript and have provided sufficient contributions to the paper
Sources of support
None
References
- [1].Kroenke K, Mangelsdorff AD.. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989;86:262–266. [DOI] [PubMed] [Google Scholar]
- [2].Yardley L, Owen N, Nazareth I, et al. Prevalence and presentation of dizziness in a general practice community sample of working age people. Br J Gen Pract. 1998;48:1131–1135. [PMC free article] [PubMed] [Google Scholar]
- [3].Tinetti ME, Williams CS, Gill TM. Dizziness among older adults: a possible geriatric syndrome. Ann Intern Med. 2000;132:337–344. [DOI] [PubMed] [Google Scholar]
- [4].Kerber KA, Meurer WJ, West BT, et al. Dizziness presentations in U.S. emergency departments, 1995-2004. Acad Emerg Med. 2008;15:744–750. [DOI] [PubMed] [Google Scholar]
- [5].Drachman DA, Hart CW. An approach to the dizzy patient. Neurology. 1972;22:323–334. [DOI] [PubMed] [Google Scholar]
- [6].Herr RD, Zun L, Mathews JJ. A directed approach to the dizzy patient. Ann Emerg Med. 1989;18:664–672. [DOI] [PubMed] [Google Scholar]
- [7].Kroenke K, Lucas CA, Rosenberg ML, et al. Causes of persistent dizziness. A prospective study of 100 patients in ambulatory care. Ann Intern Med. 1992;117:898–904. [DOI] [PubMed] [Google Scholar]
- [8].Nedzelski JM, Barber HO, McIlmoyl L. Diagnoses in a dizziness unit. J Otolaryngol. 1986;15:101–104. [PubMed] [Google Scholar]
- [9].Skiendzielewski JJ, Martyak G. The weak and dizzy patient. Ann Emerg Med. 1980;9:353–356. [DOI] [PubMed] [Google Scholar]
- [10].Kroenke K, Hoffman RM, Einstadter D. How common are various causes of dizziness? A critical review. South Med J. 2000;93:160–167. [PubMed] [Google Scholar]
- [11].Sullivan M, Clark MR, Katon WJ, et al. Psychiatric and otologic diagnoses in patients complaining of dizziness. Arch Intern Med. 1993;153:1479–1484. [PubMed] [Google Scholar]
- [12].Drachman DA. A 69-year-old man with chronic dizziness. Jama. 1998;280:2111–2118. [DOI] [PubMed] [Google Scholar]
- [13].Newman-Toker DE, Cannon LM, Stofferahn ME, et al. Imprecision in patient reports of dizziness symptom quality: a cross-sectional study conducted in an acute care setting. Mayo Clin Proc. 2007;82:1329–1340. [DOI] [PubMed] [Google Scholar]
- [14].Stanton VA, Hsieh YH, Camargo CA Jr., et al. Overreliance on symptom quality in diagnosing dizziness: results of a multicenter survey of emergency physicians. Mayo Clin Proc. 2007;82:1319–1328. [DOI] [PubMed] [Google Scholar]
- [15].Gomez CR, Cruz-Flores S, Malkoff MD, et al. Isolated vertigo as a manifestation of vertebrobasilar ischemia. Neurology. 1996;47:94–97. [DOI] [PubMed] [Google Scholar]
- [16].Lee H, Sohn SI, Cho YW, et al. Cerebellar infarction presenting isolated vertigo: frequency and vascular topographical patterns. Neurology. 2006;67:1178–1183. [DOI] [PubMed] [Google Scholar]
- [17].American Stroke Association Stroke warning signs and symptoms [Internet]. American Stroke Association. [cited 2014. February 14]. Available from: www.strokeassociation.org/STROKEORG/WarningSigns/Learn-More-Stroke-Warning-Signs-and-Symptoms_UCM
- [18].Kerber KA, Brown DL, Lisabeth LD, et al. Stroke among patients with dizziness, vertigo, and imbalance in the emergency department: a population-based study. Stroke. 2006;37:2484–2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tehrani ASS, Coughlan D, Hsieh YH, et al. Rising annual costs of dizziness presentations to U.S. emergency departments. Acad Emerg Med. 2013;20:689–696. [DOI] [PubMed] [Google Scholar]
- [20].Newman-Toker DE, Hsieh YH, Camargo CA Jr., et al. Spectrum of dizziness visits to US emergency departments: cross-sectional analysis from a nationally representative sample. Mayo Clin Proc. 2008;83:765–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Cheung CS, Mak PS, Manley KV, et al. Predictors of important neurological causes of dizziness among patients presenting to the emergency department. Emerg Med J. 2010;27:517–521. [DOI] [PubMed] [Google Scholar]
- [22].Chase M, Joyce NR, Carney E, et al. ED patients with vertigo: can we identify clinical factors associated with acute stroke? Am J Emerg Med. 2012;30:587–591. [DOI] [PubMed] [Google Scholar]
- [23].Navi BB, Kamel H, Shah MP, et al. Rate and predictors of serious neurologic causes of dizziness in the emergency department. Mayo Clin Proc. 2012;87:1080–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kim AS, Sidney S, Klingman JG, et al. Practice variation in neuroimaging to evaluate dizziness in the ED. Am J Emerg Med. 2012;30:665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Norrving B, Magnusson M, Holtas S. Isolated acute vertigo in the elderly; vestibular or vascular disease? Acta Neurol Scand. 1995;91:43–48. [DOI] [PubMed] [Google Scholar]
- [26].Savitz SI, Caplan LR, Edlow JA. Pitfalls in the diagnosis of cerebellar infarction. Acad Emerg Med. 2007;14:63–68. [DOI] [PubMed] [Google Scholar]
- [27].Ahsan SF, Syamal MN, Yaremchuk K, et al. The costs and utility of imaging in evaluating dizzy patients in the emergency room. Laryngoscope. 2013;123:2250–2253. [DOI] [PubMed] [Google Scholar]
- [28].Chalela JA, Kidwell CS, Nentwich LM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007;369:293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Simmons Z, Biller J, Adams HP Jr., et al. Cerebellar infarction: comparison of computed tomography and magnetic resonance imaging. Ann Neurol. 1986;19:291–293. [DOI] [PubMed] [Google Scholar]
- [30].Stewart MG, Chen AY, Wyatt JR, et al. Cost-effectiveness of the diagnostic evaluation of vertigo. Laryngoscope. 1999;109:600–605. [DOI] [PubMed] [Google Scholar]
- [31].Kattah JC, Talkad AV, Wang DZ, et al. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009;40:3504–3510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Cnyrim CD, Newman-Toker D, Karch C, et al. Bedside differentiation of vestibular neuritis from central “vestibular pseudoneuritis”. J Neurol Neurosurg Psychiatry. 2008;79:458–460. [DOI] [PubMed] [Google Scholar]


