Abstract
Background and Purpose:
Originally, the Timed Up & Go (TUG) test was described as including a practice trial before a timed trial, but recent studies in individuals with hip fracture have reported that performance improved with a third trial and that high intertester reliability was achieved when the fastest of 3 timed trials was used. Thus, the fastest of 3 TUG trials is recommended when testing individuals with hip fracture. To our knowledge, no study has examined the number of trials needed to achieve performance stability on the TUG test (defined as no further improvement on subsequent trials) when performed by older individuals without hip fracture. The aim of the study, therefore, was to examine whether a third TUG trial is faster than either of 2 TUG trials conducted according to standardized TUG instructions and whether the fastest of 3 trials is the most appropriate measure to apply in hospitalized and community-dwelling older individuals.
Methods:
Eighty-two participants (50 from a geriatric hospital unit and 32 from an outpatient geriatric center; 52 women, 30 men) with a mean (SD) age of 83.6 (7.9) years were included in this cross-sectional study. All participants (except one from the hospital unit) performed 3 TUG trials, as fast as safely possible on the same day, and separated by up to 1-minute pauses. A rollator (4-wheeled rolling walker) was used as a standardized walking aid in the geriatric hospital unit, whereas participants used their normal walking aid (if any) in the outpatient geriatric center.
Results and Discussion:
The fastest trial was trial 3 for 47 (57%), trial 2 for 25 (31%), and trial 1 for 10 (12%). Repeated-measures analyses of variance with Bonferroni corrections showed that TUG times improved from trial 1 to trial 3 (P < .04). In addition, the fastest of the 3 timed trials was significantly (P < .001) faster than the other 2 trials.
Conclusion:
We suggest that the fastest of the 3 TUG trials is recorded instead of the second trial in both hospitalized and community-dwelling older individuals.
Keywords: geriatric assessment, inpatients, outcome assessment, outpatients, reproducibility of results
INTRODUCTION
The Timed Up & Go (TUG) test is used worldwide to examine functional mobility in older adults and various patient groups,1–4 but instructions for administering the TUG test differ.5 Thus, TUG times reported in recent studies have been based on 1 timed trial,6 1 timed trial after a practice trial,1,7,8 the mean of 2 timed trials,9 the average of 2 timed trials after a practice trial,10 the faster of 2 timed trials after a practice trial,9,11,12 the fastest of 3 timed trials,13 or the fastest of 3 timed trials after a practice trial.14 Despite these inconsistencies in testing, the TUG test is identified frequently for the evaluation of gait and balance deficits in falls screening in the clinical practice guidelines for the prevention of falls in older people published by the American Geriatrics Society and the British Geriatrics Society.15 A cutoff point of 13.5 seconds or more7 is frequently used to identify individuals at risk of falling in the community.16 However, a systematic review from 2014 and a meta-analysis by Barry et al16 evaluating this cutoff point to identify individuals at higher risk of falling concluded that the TUG test has a limited ability to predict falls and that the TUG test should not be used in isolation for this purpose in community-dwelling older individuals. Correspondingly, Beauchet et al17 reported a limited predictive ability (prediction requires a prospective design) for future falls in older adults. This review also reported that all retrospective studies found a significant and positive association between participants' TUG performance and their history of falls. Studies analyzed in the latter review showed that the TUG cutoff times for separating those who had fallen from those who had not fallen vary considerably from 10 to 32.6 seconds. A high negative predictive value for not falling was observed using a TUG cutoff time of 24 seconds when evaluating individuals within a period of 6 months after hip fracture.1 Both reviews reported large variations (eg, walk at a “usual pace” vs “as quickly as safely possible”) in the administration of the TUG test.16,17 However, despite these large variations in TUG instructions and the populations tested, the meta-analysis of these results reported an average reference value of 11.3 (95% confidence interval, 10.0-12.7) seconds for the TUG trials in individuals 80 to 99 years of age.5 Originally, the TUG test was described as including a practice trial before a timed trial,18 but recent studies by Kristensen et al19 in individuals with hip fracture reported high intertester reliability and low measurement error when reporting the fastest of 3 timed trials20 performed with a standardized walking aid.14 To our knowledge, it is unknown whether the findings of Kristensen et al20 are applicable to older individuals without hip fracture. Therefore, we hypothesized that older individuals without hip fracture attending physical rehabilitation at a geriatric hospital unit or an outpatient geriatric center in the municipality would exhibit performance stability (defined as no additional improvement in TUG times on subsequent trials following the third TUG trial). We further hypothesized that the fastest of the 3 trials would be a better assessment of functional mobility than using, for example, either only 1 trial or the faster of 2 trials. The aim of the study, therefore, was to determine whether a third TUG trial was faster than either of 2 earlier TUG trials conducted using standardized TUG instructions and whether the fastest of the 3 timed trials is the most appropriate measure to apply in hospitalized and community-dwelling older individuals.
METHODS
Settings and Participants
A consecutive sample consisting of 79 older individuals admitted to the geriatric hospital unit at Hvidovre Hospital from March 2011 to July 2011 was evaluated for inclusion in this study. Furthermore, a convenience sample of 32 community-dwelling older individuals was included from individuals who were referred to a physical therapy program at the outpatient geriatric center at the Frederiksberg Rehabilitation and Health Centre, Frederiksberg Municipality. The geriatric hospital unit is a specialized unit for older people admitted primarily because of medical illness or functional decline, whereas the outpatient geriatric center is a physical rehabilitation center in the municipality for home-dwelling older people with functional decline.
The inclusion criteria for both groups were as follows: aged 65 years or older; able to speak and understand Danish; and the ability to perform the TUG test. Individuals at the hospital unit were excluded if they were transferred to other hospital units because of acute illness or were unable to perform the TUG test because of a low functionality (eg, not able to rise from a chair without support) or had cognitive impairment. All participants gave informed consent for inclusion in this cross-sectional study. The study was conducted in accordance with the Declaration of Helsinki II and approved by local ethical committees. Performing the TUG trials was part of the clinical battery of tests in both settings.
TUG Test Procedure
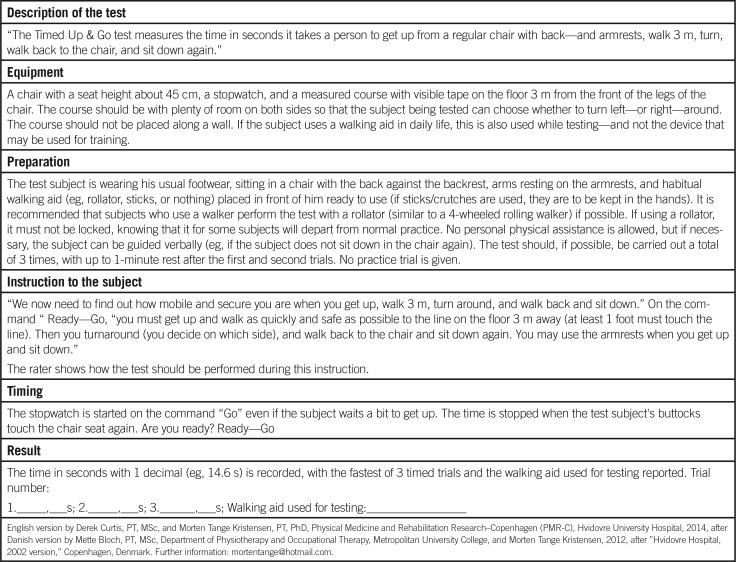
The TUG test was performed the day before discharge from the geriatric hospital unit or at the time of the first physical therapy assessment in the outpatient geriatric center. Before testing, the participants were informed that performing the TUG test was a standard procedure. They were also told that they were to perform the TUG test 3 times and, if necessary, they could rest for up to 1 minute while seated in between tests.20
The 6 physical therapists (3 at the hospital and 3 at the outpatient center) who tested the participants were aware of the hypothesis of the study. They were all trained how to instruct the participants to perform the test using the well-described standardized TUG instructions (see the Appendix).
Because most participants from the geriatric hospital unit used a rollator (a 4-wheeled rolling walker, wheel diameter 7.5 in with 2 handles and handbrakes) as an assistive device,14 they were all instructed to use a rollator during testing,14 whereas participants in the outpatient geriatric center used their normal walking aid, if any.
The participants were not aware of the hypothesis of the study. They received no verbal encouragement during testing, and they decided how long they would rest between trials (up to 1 minute). Participants were not informed of their TUG test results during testing.
Analyses
Descriptive data were reported including the age, sex, use of a walking aid, and primary reason for hospitalization/referral to the outpatient geriatric center. The χ2 and Student t tests were used to evaluate differences between groups of participants. We used repeated-measures analysis of variance, followed by post hoc comparisons with the Bonferroni correction, to compare TUG trial 1 with trial 2, trial 2 with trial 3, and trial 1 with trial 3. We also compared the fastest of the 3 TUG trials with the 2 slower trials. Follow-up polynomial contrast analysis was used to determine a significant linear trend of differences between the TUG performances. Data are reported as the number (percentages) of participants and as the mean (SD). All data analyses were conducted using SPSS 19.0 (SPSS Inc, Chicago, Illinois), with a significance level of P = .05.
RESULTS
Twenty-nine of 79 hospitalized individuals were excluded for various reasons; the results for the remaining 50 participants are reported. Reasons for exclusion included inability to rise from a chair or walk independently (n = 12), inability to provide consent (n = 1), low cognitive status (n = 1), transfer to another hospital unit (n = 5), sudden discharge without notice (n = 4), death (n = 4), and logistics (n = 2). The characteristics of the 29 individuals who did not perform the TUG tests were comparable with those included in the study. Baseline characteristics of the 50 in-hospital and 32 outpatient participants are given in Table 1. The 2 groups were comparable with regard to age and sex (P > .8), whereas more participants from the hospital habitually used a walking aid (P = .007).
Table 1. Baseline Characteristics of Participants.
| Variables | Geriatric Hospital Unit (n = 50) | Outpatient Geriatric Center (n = 32) |
|---|---|---|
| Sex (women), n (%) | 32 (64) | 20 (63) |
| Age, mean (SD), y | 83.8 (7.2) | 83.4 (8.6) |
| Living in their own home, n (%) | 47 (94) | 32 (100) |
| Habitual use of a walking aid, n (%) | 31 (62) | 10 (31) |
| Primary reason for hospitalization/referral to physical therapy | ||
| Medical illness, n (%) | 23 (46) | N/A |
| Surgical illness, n (%) | 2 (4) | N/A |
| Decreased functional level, n (%) | 25 (50) | 32 (100) |
Abbreviation: N/A, not available.
TUG Performances
All participants completed 3 TUG trials except for 1 participant from the geriatric hospital unit (due to fatigue), and no significant difference (P > .2) was seen in TUG performances between the 2 settings (Table 2). A significant difference (P > .2) was not observed when comparing the performances of men to women between the 2 locations. Because no significant differences were observed, the TUG data from the 2 settings were combined and analyzed together. Trial 3 for 47 (57%), trial 2 for 25 (31%), and trial 1 for 10 (12%) of the 82 participants were the fastest. The repeated-measures analysis of variance with Bonferroni corrections comparing TUG1, TUG2, and TUG3 trials showed a significant difference (P < .04) for all comparisons (F2,160 = 15.75, P < .001), as presented in Table 2.
Table 2. Timed Up & Go Test Performances of Participants (N = 82).
| TUG Trial Number | Geriatric Hospital Unit (n = 50) Mean (SD) | Outpatient Geriatric Center (n = 32) Mean (SD) | P Value Between Settings | Mean TUG, Both Settings (n = 81) Mean (SD) | Repeated-Measures ANOVAsa |
|---|---|---|---|---|---|
| TUG1, s | 26.4 (15.5) | 22.9 (12.9) | .292 | 25.0 (14.6) | P < .04b |
| TUG2, s | 23.9 (14.1)c | 21.2 (11.8) | .368 | 22.9 (13.3) | |
| TUG3, s | 22.5 (11.6)c | 20.7 (12.0) | .498 | 21.8 (11.6) | |
| Fastest of the 3 TUG trials, s | 21.8 (11.1) | 20.1 (11.5) | .505 | 21.0 (11.2) | P < .001d |
Abbreviations: ANOVA, analysis of variance; TUG, Timed Up & Go.
aBonferroni adjusted analysis in 81 participants.
bComparison of TUG1 with TUG2, TUG2 with TUG3, and TUG1 with TUG3.
cn = 49.
dComparison of the fastest of the 3 TUG trials with the 2 slower trials.
However, the Mauchly test indicated that the assumption of sphericity was violated because χ21 = 27.98 and P < .001. Therefore, the degrees of freedom were corrected using Huynh-Feldts estimates of sphericity(∊ = 0.782). The performance times still showed a significant improvement with increased TUG trials (F1.57,125 = 15.75, P < .001). Follow-up polynomial contrast analysis indicated a significant linear trend (F3 = 20.43, P < .001).
Performance improvements between TUG2 and TUG3 trials were seen for 74% of participants. The participant who improved performance the most walked 19.8 seconds faster during the TUG3 trial (64.8 seconds) than in the TUG2 trial (84.6 seconds). In addition, the fastest of the 3 timed trials, average of 21.0 (11.2) seconds, was significantly (P < .001, Bonferroni corrected) faster than the slower 2 trials (mean difference of 1.9 seconds [when compared with the second slowest trial] and 4.8 seconds [when compared with the slowest trial]). Performance differences among the fastest TUG trial and the other 2 trials increased with the time taken to perform the TUG test (r ≥ 0.550, P < .001). Only 16 participants (19.5%) performed their fastest TUG trial in less than 12.7 seconds (upper limit of reported TUG confidence intervals for 80-99 years old individuals).5
DISCUSSION
Three timed trials are needed to ensure performance stability for the TUG test when used in individuals with hip fracture.20 To our knowledge, no previous studies examining the number of TUG trials needed to achieve performance stability when evaluating older individuals without hip fracture have been conducted. We found that introducing a third TUG trial produced significantly faster performance times than just 2 trials in hospitalized and community-dwelling older participants. Furthermore, participants did not uniformly achieve their fastest time in the third trial because some participants were faster in trial 1 or 2. However, the fastest of the 3 timed trials was significantly faster than the other 2 trials, regardless of the order, when we used the same standardized TUG instructions as those used when testing patients with hip fracture.19,20
Furthermore, the present study showed that older individuals completed the TUG tests more easily than the originally described 2 times,18 if allowed a pause of up to 1 minute between trials.
Other studies have documented the need for 3 or more trials to accurately measure performance. For example, Robinson and Gribble21 reported stability after 4 practice trials for the Star Excursion Balance Test, whereas 3 practice trials were needed for postural control measurements during weight-shifting in community-living older adults.22 In contrast, Mesquita et al2 reported that individuals with advanced chronic organ failure needed to perform the TUG test 2 times in order to account for possible learning effects. A mean difference of only 0.1 (1.2) seconds between the second and third TUG trials was reported. This is probably explained by the faster TUG times reported in their study (mean of the third trial <13 seconds)2 than those in the present study (mean of the third trial >20 seconds). Larger variations in TUG times are reported for individuals with slower TUG performances,19,23 which is consistent with our data. To minimize measurement error, we recommend that 3 TUG trials be performed during each assessment. This recommendation is supported by the observed low measurement error in a recent intertester reliability study of 50 individuals with hip fracture (standard error of measurement = 11%); this study reported the fastest of 3 TUG trials, mean of 21.8 (10.8) seconds, in their reliability analysis.19
One might question our replacement of the phrase “comfortable pace,” which was originally used by Podsiadlo and Richardson,18 with the phrase “fast speed” in our TUG instructions. However, the literature reports many variations of the TUG instructions.5,16,17 We believe that introducing a stopwatch and timing the performances automatically encourage people to perform their best (walk faster). Also, “fast speed” might be considered “comfortable” by some people, and the age, height, and strength of 4 lower extremity muscle groups correlate better with the maximum walking speed (r = 0.292-0.558) than to the comfortable walking speed (r = 0.190-251).24
Study Limitations and Strengths
We found a tendency toward performance stability simply by introducing a third TUG trial. Our study design included only 3 trials and does not give us a definitive answer to the “TUG performance stability” question because one could argue that introducing a fourth or fifth trial would have resulted in further performance improvement. However, the results obtained in the hip fracture study,20 which served as the inspiration for the present study, indicate that 3 TUG trials are sufficient to establish performance stability also when testing individuals in a geriatric setting. Although our study participants were hospitalized or community-dwelling older people without a hip fracture, they were comparable with respect to age, sex, decreased functional level, and TUG performances. Sixty-five percent of patients older than 80 years performed best in the third trial in the hip fracture study;20 in our study, 57% of participants had the best performance time in the third trial and the mean age of our study population was 83.6 (7.9) years. Although more patients in the hip fracture study performed better in the third trial than in the present study, participants did not improve their performances in the fourth trial. Including more than 3 TUG trials in future studies could therefore be irrelevant to the test score because no improvement was observed in the fourth test. Also, more than 3 TUG trials are likely too time-consuming for everyday clinical practice because conducting 3 TUG trials takes approximately 5 minutes.
As mentioned in the “Methods” section, the physical therapists administering the test were trained how to instruct the participants to perform the TUG test according to well-described instructions (see the Appendix), which strengthens the present study. Although participants were blinded to the hypothesis of the study, the physical therapists were not.
CONCLUSION
These results cast some doubt on the use of the original TUG instructions (which describe a practice trial, followed by a single timed trial) when the test is used in older individuals with mobility deficiencies. We suggest standardizing the TUG instructions and that 3 TUG trials be used for the assessment of functional mobility in hospitalized and community-dwelling older individuals. Furthermore, we suggest that the fastest trial time be reported for both clinical practice and research studies. This will enable valid comparisons of TUG times reported by different investigators at various institutions. The reliability of the standardized TUG instructions awaits investigation in older individuals.
ACKNOWLEDGMENTS
The authors thank the physical therapists at the Hvidovre Hospital and at the Exercise and Rehabilitation Unit, Frederiksberg Health Center, for the recruitment and testing of the participants. The authors thank Derek Curtis, PT, PhD, MSc, for his insightful comments on the manuscript.
Appendix: Timed Up & Go test: Instructions
Footnotes
The study was presented at the Congress of the Danish Physical Therapist Association, March 2012, Odense, Denmark.
The authors declare no conflicts of interest.
Richard Bohannon was the Decision Editor.
REFERENCES
- 1.Kristensen MT, Foss NB, Kehlet H. Timed “Up & Go” test as a predictor of falls within 6 months after hip fracture surgery. Phys Ther. 2007;87(1):24–30. [DOI] [PubMed] [Google Scholar]
- 2.Mesquita R, Janssen DJA, Wouters EFM, Schols JMGA, Pitta F, Spruit MA. Within-day test-retest reliability of the Timed Up & Go test in patients with advanced chronic organ failure. Arch Phys Med Rehabil. 2013;94(11):2131–2138. [DOI] [PubMed] [Google Scholar]
- 3.Nocera JR, Stegemöller EL, Malaty IA, Okun MS, Marsiske M. Using the Timed Up & Go test in a clinical setting to predict falling in Parkinson's disease. Arch Phys Med Rehabil. 2013;94(7):1300–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee H-C, Chang K-C, Tsauo J-Y, Hung J-W, Hung Y-C, Lin S-I. Effects of a multifactorial fall prevention program on fall incidence and physical function in community-dwelling older adults with risk of falls. Arch Phys Med Rehabil. 2013;94(4):606–615, 615.e1. [DOI] [PubMed] [Google Scholar]
- 5.Bohannon RW. Reference values for the Timed Up and Go test: a descriptive meta-analysis. J Geriatr Phys Ther. 2006;29(2):64–68. [DOI] [PubMed] [Google Scholar]
- 6.Mendelsohn ME, Leidl DS, Overend TJ, Petrella RJ. Specificity of functional mobility measures in older adults after hip fracture: a pilot study. Am J Phys Med Rehabil. 2003;82(10):766–774. [DOI] [PubMed] [Google Scholar]
- 7.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Phys Ther. 2000;80(9):896–903. [PubMed] [Google Scholar]
- 8.Kristensen MT, Bandholm T, Holm B, Ekdahl C, Kehlet H. Timed Up & Go test score in patients with hip fracture is related to the type of walking aid. Arch Phys Med Rehabil. 2009;90(10):1760–1765. [DOI] [PubMed] [Google Scholar]
- 9.Lusardi MMP, Pellecchia GLP, Schulman MP. Functional performance in community living older adults. J Geriatr Phys Ther. 2003;26(3):14–22. [Google Scholar]
- 10.Stivala A, Hartley G. The effects of a Pilates-based exercise rehabilitation program on functional outcome and fall risk reduction in an aging adult status-post traumatic hip fracture due to a fall. J Geriatr Phys Ther. 2014;37(3):136–145. [DOI] [PubMed] [Google Scholar]
- 11.Brooks D, Davis AM, Naglie G. Validity of 3 physical performance measures in inpatient geriatric rehabilitation. Arch Phys Med Rehabil. 2006;87(1):105–110. [DOI] [PubMed] [Google Scholar]
- 12.Fisken AL, Waters DL, Hing WA, Steele M, Keogh JW. Comparative effects of 2 aqua exercise programs on physical function, balance, and perceived quality of life in older adults with osteoarthritis. J Geriatr Phys Ther. 2014;37(3):1–11. [DOI] [PubMed] [Google Scholar]
- 13.Bijlsma AY, Meskers CGM, van den Eshof N, Westendorp RG, Sipila S, Stenroth L. Diagnostic criteria for sarcopenia and physical performance. Age (Dordr, Neth). 2014;36(1):275–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bischoff HA, Stähelin HB, Monsch AU, et al. Identifying a cut-off point for normal mobility: a comparison of the Timed “Up and Go” test in community-dwelling and institutionalised elderly women. Age Ageing. 2003;32(3):315–320. [DOI] [PubMed] [Google Scholar]
- 15.Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. [DOI] [PubMed] [Google Scholar]
- 16.Barry E, Galvin R, Keogh C, Horgan F, Fahey T. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr. 2014;14:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beauchet O, Fantino B, Allali G, Muir SW, Montero-Odasso M, Annweiler C. Timed Up and Go test and risk of falls in older adults: a systematic review. J Nutr Health Aging. 2011;15(10):933–938. [DOI] [PubMed] [Google Scholar]
- 18.Podsiadlo D, Richardson S. The Timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. [DOI] [PubMed] [Google Scholar]
- 19.Kristensen MT, Henriksen S, Stie SB, Bandholm T. Relative and absolute intertester reliability of the Timed Up and Go test to quantify functional mobility in patients with hip fracture. J Am Geriatr Soc. 2011;59(3):565–567. [DOI] [PubMed] [Google Scholar]
- 20.Kristensen MT, Ekdahl C, Kehlet H, Bandholm T. How many trials are needed to achieve performance stability of the Timed Up & Go test in patients with hip fracture? Arch Phys Med Rehabil. 2010;91(6):885–889. [DOI] [PubMed] [Google Scholar]
- 21.Robinson RH, Gribble PA. Support for a reduction in the number of trials needed for the star excursion balance test. Arch Phys Med Rehabil. 2008;89(2):364–370. [DOI] [PubMed] [Google Scholar]
- 22.Jbabdi M, Boissy P, Hamel M. Assessing control of postural stability in community-living older adults using performance-based limits of stability. BMC Geriatr. 2008;8:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nordin E, Rosendahl E, Lundin-Olsson L. Timed “Up & Go” test: reliability in older people dependent in activities of daily living—focus on cognitive state. Phys Ther. 2006;86(5):646–655. [PubMed] [Google Scholar]
- 24.Bohannon RW. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determinants. Age Ageing. 1997;26(1):15–19. [DOI] [PubMed] [Google Scholar]