Abstract
Background
IVC filters have been widely accepted as an effective method to prevent pulmonary embolism (PE) in patients with deep venous thrombosis (DVT). However, the placement of IVC filters is associated with significant complications and filter retrieval can be challenging when the filter struts are embedded into the caval wall.
Material/Methods
Over 26 months, we reviewed the safety and efficacy of the bidirectional pull-back technique for removing strut-embedded IVC filters in 15 consecutive patients. Retrieval procedural data such as in-dwell time, retrieval time, and fluoroscopy time were recorded. Clinical outcomes and procedure-related complications were evaluated by venography or enhanced computed tomography. Histologic tissue was analyzed to reveal the pathologic effects of chronic filter implantation. All patients underwent routine clinical follow-up at a mean time of 12 months (range, 8–14 months).
Results
Technical success of filter retrieval was achieved in 100%, with mean implantation of 46.6 days (range, 27–66 days). Filter types were as follows: OptEase (n=11) and Aegisy (n=4). The mean retrieval time and fluoroscopy time were 21.43±5.42 min and 7.63±2.67 min, respectively. Immediate postprocedure venography showed no procedure-related complications. Thirteen patients discontinued previously prescribed lifelong anticoagulation. There were no long-term complications during follow-up.
Conclusions
The bidirectional pull-back technique is safe and efficient for filter retrieval. This complex technique can be particularly useful in selected patients to remove strut-embedded cylindrical-shaped IVC filters previously considered irretrievable.
MeSH Keywords: Endovascular Procedures, Pulmonary Embolism, Vena Cava Filters, Venous Thrombosis
Background
Pulmonary embolism (PE) is a serious disease with significant morbidity and mortality rates and brings huge economic burden to society [1]. Inferior vena cava (IVC) filters were first developed in 1967 and now have been widely accepted as an effective method to prevent PE in patients with deep venous thrombosis (DVT) [2]. However, along with widespread application, the placement of IVC filters is associated with significant complications such as chronic IVC thrombosis, development of postthrombotic syndrome, IVC perforation, and filter tilting and migration [3].
Thus, the US Food and Drug Administration (FDA) in 2010 issued a safety alert recommending physicians and clinicians responsible for the ongoing care of patients with retrievable IVC filters consider removing the filter as soon as protection from pulmonary embolism is no longer needed.
This trend has led to attempting IVC filter retrievals with prolonged in-dwell times, particularly in patients who have long life expectancy. Although the successful retrieval rate for a retrievable filter was 70–100% [4], some filters could not be retrieved due to technical issues or patient-related problems [2]. Our study concentrates predominately on solving this technical problem.
The desire to retrieve filters has led to the development and use of various advanced retrieval techniques to increase the retrieval success rate. Several unconventional techniques, such as loop-snare technique and use of endobronchial forceps, have been described [5,6]. However, most of these advanced techniques are designed for cone-shaped tilted or tip-embedded filters. There are few techniques specifically described for retrieval of strut-embedded cylindrical-shaped filters, such as OptEase and Aegisy [7,8].
We performed a retrospective study of patients who underwent successful retrieval of strut-embedded retrievable filters using the bidirectional pull-back technique. Here, we present results from our single-center experience on endovascular filter retrieval with this technique.
Material and Methods
Patients
We reviewed medical records of all patients who received filter retrieval in our center from March 2014 to May 2016. The local institutional review board approved this retrospective review. Criteria for inclusion were patients who received filter implantation exceeding routine retrieval window of 12 days [9] and radiologically diagnosed with strut-embedded filter, and who finally underwent bidirectional pull-back technique after failed standard retrieval. A strut-embedded filter was defined as being refractory to standard snare techniques and nominal traction recommended by the manufacturer [10]. Over a 26-month period, 15 consecutive patients (mean age 44.07 years, range 30–59 years) were deemed appropriate candidates and underwent aggressive attempted filter retrieval involving bidirectional pull-back technique. All patients are listed in Table 1. Indications for filter placement were prophylactic for increased risk of thromboembolic disease (n=6), for massive pulmonary embolism (n=2), for complications of anticoagulation (n=3), or for protection during catheter-directed thrombolysis (n=4). In all attempted retrievals, the indication of an IVC filter was no longer present. Data were collected with regard to patient characteristics, treatment method, filter types, filter placement, and filter retrieval venograms. All patients were scheduled for routine clinical follow-up after discharge with inpatient examinations or outpatient visits.
Table 1.
Baseline characteristics of the patients.
| Case | Age/Sex | Filter type | Indwell time (d) | Potential risk factor for DVT | Radiographic findings |
|---|---|---|---|---|---|
| 1 | 30/F | Optease | 41 | Pregnancy | Filter struts adherent to IVC, |
| 2 | 47/M | Optease | 27 | Recent major surgery | Filter struts adherent to IVC |
| 3 | 41/F | Optease | 52 | Recent major surgery | Filter struts adherent to IVC |
| 4 | 44/F | Aegisy | 26 | Spontaneous | Filter struts adherent to IVC, Acute on chronic IVC thrombosis |
| 5 | 46/M | Optease | 39 | Recent major surgery | Filter struts adherent to IVC |
| 6 | 55/M | Optease | 67 | Spontaneous | Filter struts adherent to IVC |
| 7 | 30/M | Optease | 44 | Limb trauma | Filter struts adherent to IVC, Left leg thrombosis and right common iliac aneurysms and retroperitoneum hemorrhage |
| 8 | 39/M | Aegisy | 52 | Recent major surgery | Filter struts adherent to IVC |
| 9 | 47/F | Optease | 28 | Spontaneous | Filter struts adherent to IVC Acute on chronic IVC thrombosis |
| 10 | 55/M | Aegisy | 39 | Immobilization | Filter struts adherent to IVC, Left iliac venous stenosis |
| 11 | 51/F | Optease | 61 | Thrombophilia | Filter struts adherent to IVC |
| 12 | 36/M | Optease | 42 | Thrombophilia | Filter struts adherent to IVC |
| 13 | 32/F | Optease | 51 | Spontaneous | Filter struts adherent to IVC |
| 14 | 59/M | Optease | 66 | Immobilization | Filter struts adherent to IVC Left iliac venous stenosis |
| 15 | 49/M | Aegisy | 64 | History of DVT | Filter struts adherent to IVC |
IVC – inferior vena cava; DVT – deep venous thrombosis.
Before the procedure, the potential risks, such as caval perforation, thrombosis, and filter fracture, were explained. Written informed consent for the complexed retrieval of the IVC filter was obtained from all patients.
Technique and procedure
Before retrieval attempts, all patients were assessed by lower-extremity venous duplexes or conventional venography to exclude deep venous thrombosis or caval thrombus. IVC filter retrievals were all performed by experienced vascular surgeons in a dedicated suite. Occlusion balloons and vascular covered stents were prepared in case of emergency during the procedure.
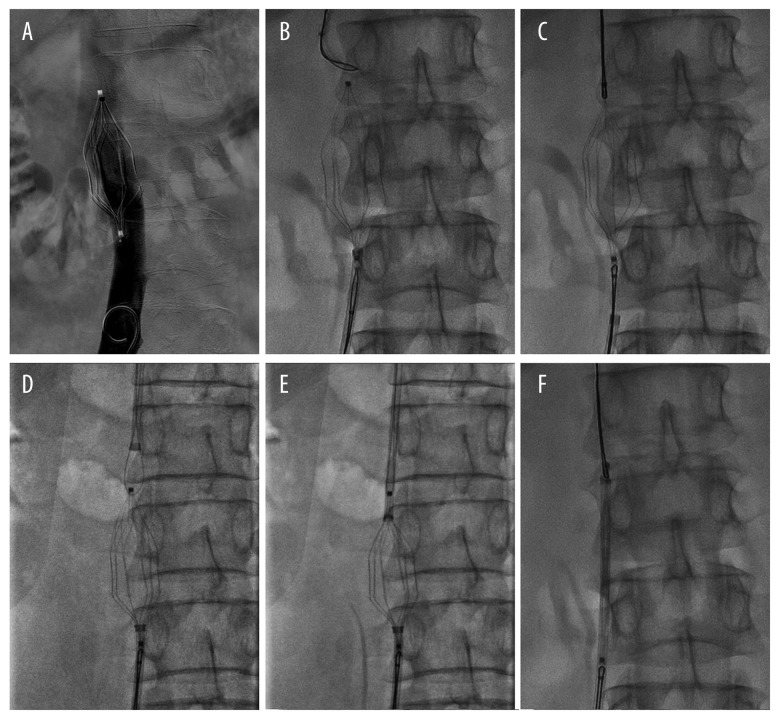
All patients received prior anticoagulation with either enoxaparin (4000 iu subcutaneously, twice daily) or warfarin (target international normalized ratio of 2–3). We also gave additional therapeutic anticoagulation with low molecular weight heparin (1 mg/Kg) during retrieval attempts to minimize intraprocedural thrombotic risk. All the procedures were performed under local anesthesia and the complex technique herein described was applied after the first failed attempt with standard technique. Under ultrasound guidance, the right femoral vein was punctured as the venous access. Using a small-gauge needle to avoid inadvertent puncture of the adjacent femoral artery, a 10-F introducer sheath (Cook, Bloomington, IN) was inserted through the vein in which all subsequent catheter and wire exchanges were performed. A 260-cm stiff wire (Terumo, Somerset, NJ) was placed with the tip positioned in the lower IVC, then a 5-F pig-tail catheter (Cook, Bloomington, IN) was advanced over the wire and formed below the level of the filter. Contrast medium was infused through the catheter to reconfirm the patency and position of the filter (Figure 1A). When excluding thrombus or other cava abnormity, the 10-F introducer sheath was exchanged for a 10-F-long sheath (Cook, Bloomington, IN) and the pig-tail catheter was replaced by an Amplatz gooseneck snare (ev3, Plymouth, MN). The gooseneck snare was advanced through the 10-F long sheath and attempts were made to engage the caudal hook of the filter. At the discretion of another surgeon, the right internal jugular vein was used as the second venous access. The other 10-F long sheath was introduced through the right jugular approach and a second gooseneck snare was slowly advanced toward the proximal IVC and opened within the cone of the filter to capture the cranial apex (Figure 1B). Because the filter lacked a cranial hook, the snare device was tightened while gentle traction was continuously applied on the snare once it engaged the cranial apex (Figure 1C). Either way, if the snare could not engage the apex firmly, the snare device was formed open below the upper apex, and the free end of the wire was threaded into the open snare device through an opposite interstice. The wire tip was then engaged and pulled through the filter interstice while the outer end of the wire was fed, forming a wire loop through the filter, which is similar to the snare-over-wire loop technique [11] (Figure 1D). Once the control of each tip was established, the same gentle tractions were applied on the 2 gooseneck snares in opposite directions, collapsing the filter into the caudal sheath. Alternatively, if the filter could not be removed, the jugular and femoral sheaths were advanced toward each other to produce parallel shear force. This motion had to be repeated several times to separate the embedded struts from the hyperplastic neointimal tissue (Figure 1E). With the help of bidirectional tractions and shear force, the filter was dissected from the caval wall and then retrieved into the inferior 10-F long sheath (Figure 1F). When the filter was removed, immediate venography was performed to confirm there was no contrast agent extravasation or IVC stenosis.
Figure 1.
Bidirectional pull-back technique. (A) A pig-tail catheter confirmed the patency and position of the filter. (B) An Amplatz gooseneck snare captured the caudal hook while the other one attempted to engage the proximal end of the filter. (C) The snare was tightened when it engaged the cranial apex. (D) A wire loop was formed through the filter to firmly engage the apex. (E) The coaxial 10-F long sheaths were advanced to supply pushability, which facilitated separating the embedded struts and caval wall. (F) The filter was removed into the inferior 10-F long sheath.
After retrieval, 2 patients continued therapeutic anticoagulation for underlying thrombophilia, whereas an attempt to discontinue anticoagulation was made in all other patients after successful filter removal. All filter-adherent specimens were submitted to pathological examination for histologic evaluation of vessel wall elements. All patients were scheduled for routine clinical follow-up to monitor any procedure-related complications. A CT was performed 1 month after the procedure and then annually to assess the patency rate after iliac vein stenting. All patients were contacted at a mean follow-up time of 12 months (range, 8–14 months) and were interviewed by telephone to assess quality of life after treatment and to obtain possible evidence of postthrombotic syndrome.
Results
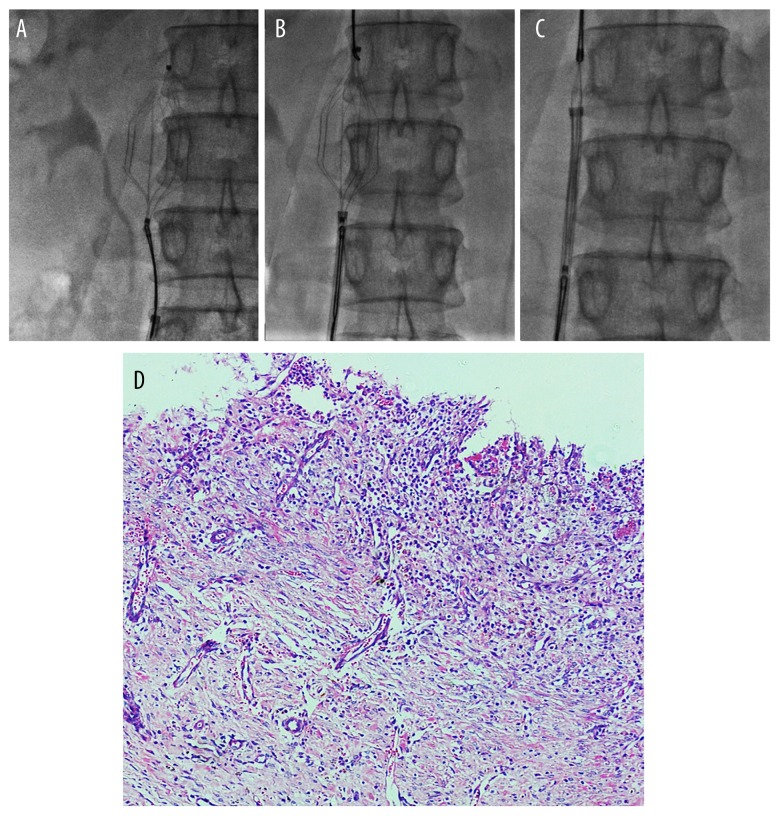
Over 26 months, 15 patients diagnosed with strut-embedded filter were refractory to standard methods. Six patients received filter implantation in the base hospitals. They had sought filter retrieval in regional hospitals, but failed. The filter was unable to be collapsed into sheath with a gooseneck snare. Intraoperative venography revealed that neither filter tilting, migration, nor penetration of the caval wall occurred. Failure to engage the filter was believed to be a result of neointimal hyperplasia and dense fibrosis attached to the filter struts. Adherent tissue did not allow the filter to be retrieved. One male patient received endovascular repair of iliac aneurysms previously due to co-morbidities of right common iliac aneurysms and retroperitoneum hemorrhage. Another patient underwent curettage before IVC placement. Two patients diagnosed with acute caval thrombosis underwent successfully secondary catheter-directed thrombolysis before filter retrieval. IVC filters were no longer medically needed in any patients before retrieval attempts. The mean in-dwell time for all filters was 46.60 days (median, 44 d; range, 27–66 d). Bidirectional pull-back technique was successful in all patients in which it was attempted. The mean retrieval time was 21.43 min (range, 16.20–30.25 min), and the mean fluoroscopy time for successful retrieval was 7.63 min (range, 5.10–12.15 min) (Table 2). The right internal jugular vein and femoral vein were patent and provided sufficient venous access in all patients. One patient complained of mild back pain but postoperative venography revealed no contrast media extravasation or caval narrowing. For 2 Aegisy filter retrievals, due to densely fibrinous tissue that prevented full collapse of the filter, attached tissue was removed along with the filter into the femoral sheath. Histologic analysis of adherent tissue from the retrieved specimens revealed a predominance of neointimal hyperplasia and organizing thrombus (Figure 2). During all retrieval attempts, there were no procedure-related complications. Immediate postprocedure venography showed no IVC stenosis or contrast extravasation.
Table 2.
Retrieval procedural data.
| Indwell time(d) | |
| Mean ±SD | 46.60±13.91 |
| Range | 27–66 |
| Retrieval time (min) | |
| Mean ±SD | 21.43±5.42 |
| Median | 20.10 |
| Range | 16.20–30.25 |
| Fluoroscopy time (min) | |
| Mean ±SD | 7.63±2.67 |
| Median | 7.15 |
| Range | 5.10–12.15 |
| Filter retrieval access site | |
| Right jugular vein and right femoral vein | 11 (73.3%) |
| Right jugular vein and left femoral vein | 4 (26.7%) |
SD – standard derivation.
Figure 2.
A 47-year-old woman with strut-embedded filter. (A) The caudal hook was engaged with a gooseneck snare. (B) Coaxial snares were used to capture the filter from opposite directions through 10-F sheaths. (C) The inferior sheath was put forward to dissect the embedded struts and caval wall. (D) The adherent tissue from the filter specimen, demonstrating neointimal hyperplasia.
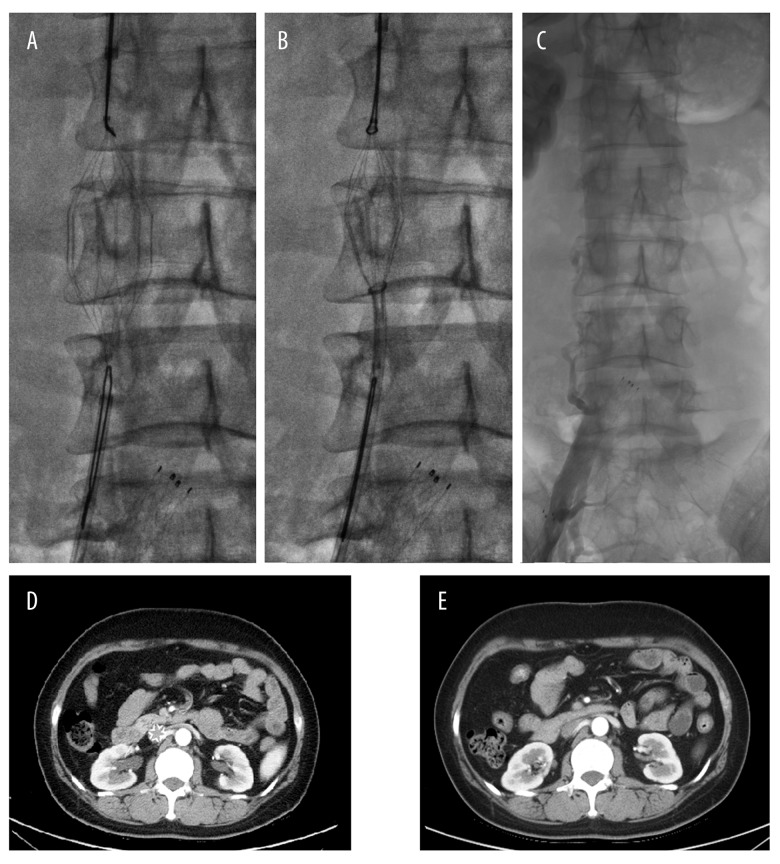
Thirteen patients were completely weaned from anticoagulation after discharge, and the other 2 patients continued oral warfarin due to thrombophilia. Two cases diagnosed as May-Thurner syndrome received recanalization of iliac vein stenosis with balloon angioplasty and stent placement after retrieval. Additional radiographic follow-up was performed in 1 patient who underwent stent placement in the right common iliac artery. Computed tomography (CT) examination at 1-month follow-up showed no evidence of adjacent aortic injury or retroperitoneal hematoma (Figure 3). The remaining patients were followed up by inpatient examinations or outpatient visits at a mean follow-up time of 12 months. After successful retrieval, none of the patients had back pain, abdominal pain, or other discomfort, except 1 woman who complained of intermittent leg heaviness at 2-month follow-up.
Figure 3.
A 30-year-old male patient who received endovascular repair of iliac aneurysms before IVC filter placement. (A, B) The procedure of filter retrieval using bidirectional pull-back technique. (C) The intactness of the caval wall after filter retrieval. (D) Preprocedure CT revealed the filter in IVC. (E) CT obtained postprocedure demonstrated intactness of IVC.
Discussion
Although short-term benefits of preventing PE have been shown in patients receiving IVC filters, the long-term benefits and risks from IVC filtration remain uncertain. The PREPIC study, which enrolled 400 patients with proximal DVT with or without PE to receive IVC filter, indicated that filters reduced the frequency of PE at the cost of a long-term increase in DVT and IVC thrombosis with no reduction in mortality [12]. The potential problems and complications related to long-term implantation of filter retrieval were gradually realized with the increasing use of retrievable IVC filters. Adverse outcomes following filter placement included recurrence of DVT, IVC thrombosis, IVC penetration, filter migration, filter tilt, and filter fracture. The estimated incidence of DVT was reported in the PREPIC study to be up to 8.5%, with IVC thrombosis in 1.6% to 8% [12]. The other complications, especially acute procedure-related complications, were rare in published articles [13].
Incidence of complications differed among various individual filter types. Filter types of all the patients included 11 OptEase vena cava filters (Cordis) and 4 Aegisy vena cava filters (Life-Tech), which both had cylindrical-shape and double-basket design. Unlike most available retrieval filters of conical shape, it has 6 struts and barbs to provide resistance to migration. Limited penetration of the IVC wall was necessary to ensure adequate filter anchoring; however, the extensive contact of the filter struts with the caval wall increased the risk of being trapped by neointimal tissue with prolonged in-dwell times. Prompt filter retrieval may decrease potential complications and avoid lifelong anticoagulation in patients with IVC filter.
Various techniques have been described for complex retrieval of embedded, fracture, or penetrating filters, including stiff wire displacement technique for cone-shaped IVC filters, dual-access technique to displace the tilted filter, and balloon displacement technique using an interposed angioplasty balloon [14,15]. Apart from the above techniques, Sugiura et al. reported successful retrieval of a Günther Tulip IVC filter surrounded by minor clots, using a loop wire technique [16]. Rubenstein used sling technique in 8 tilted IVC filters that could not be retrieved with standard technique [17].
Although alternative methods are well-described for managing tip-embedded, tilted, or fracture filters, strut-embedded cylindrical-shaped filters are not routinely retrieved [18,19]. The reasons are as follows: first, the cylindrical-shaped filter is less widely used in Europe and North America. Most commercially available retrievable filters are cone-shaped, such as the Günther Tulip filter (Cook, Bloomington, IN) and the G2 filter (Bard Peripheral Vascular, Tempe, AZ) [7], and less use led to less retrieval experience. Second, the recommend in-dwell time is shorter in cylinder-shaped filters than in cone-shaped filters. The recommended in-dwell time of the OptEase filter is 12 days, which prompts clinicians to retrieve the filter within the retrieval time window. Masaya Nakashima reported 2 successful cases using disposable biopsy forceps to remove OptEase filters [20] . Thuong also reported 3 cases of attempted OptEase filter retrieval using rigid endobronchial forceps dissection and a wire-through-loop snare [7]. However, this technique was naturally more invasive than the simpler snare techniques because of the increased risk of vessel perforation or rupture [21]. Ramsey Al-Hakim reported 2 complications of 17 cases with the use of endobronchial biopsy forceps, demonstrating a high rate of complications with this technique [22]. In contrast, bidirectional pull-back technique is safer because its coaxial bidirectional tractions do not tear the caval wall in the horizontal plane. The parallel shear forces in each direction, combined with counter advancement of sheaths, provide blunt dissection to separate the embedded struts from the caval wall. Moreover, the sheaths, guiding wire, and gooseneck snares are much softer than rigid biopsy forceps, which causes less damage to the vascular wall and adjacent tissue. Kuo et al. described the use of an endovascular laser sheath as a thermal dissection tool for free-embedded filters and the retrieval was successful in 98% of attempts. However, the only 2 retrieval failures were associated with cylinder-shaped filter [23], possibly because the larger adherent surface area to the caval wall led to substantial scar tissue formation within the filter struts and eventually hindered filter collapse. In our current series, no special apparatus was required, which relieved the economic burden on patients. Moreover, the application of the 10-F sheath caused less risk of venous pseudoaneurysm in the access site. Out of all cases, attached tissue was removed along with the filter into the femoral sheath in just 2 patients; however, the postprocedure venography demonstrated the intactness of IVC and the patients had no complaints of discomfort. We postulate that dense fibrous tissue may have protected the caval wall from rupture. Histological examination also revealed predominance of neointimal hyperplasia.
It is clear that fluoroscopy time will be increased when the complexity of retrieval leads to longer attempts. The mean fluoroscopy time was 7.63±2.67 min in our study. Keller et al. reported OptEase retrieval with a mean fluoroscopy time of 6.2 min (range, 1.2–51.4) [24]. Pellerin et al. reported a mean fluoroscopy time of 16 min (range, 7–28) with ALN device retrieval [25]. Stavropoulos et al. reported the mean fluoroscopy time for successful retrieval was 6.4 min (range, 1–69 min) [26]. Our mean fluoroscopy time for successful removal showed a comparatively longer time compared with these data. The reason was that the studies above contained conventional retrieval, which took a much shorter time than that with complex retrieval. Although longer than that of conventional methods, the fluoroscopy time was shorter compared with that of 25.2 min for complex OptEase filter retrieval reported by Uri Rimon et al. [27]. Prolonged caval wall collapse while constraining the adherent filter struts was believed to be associated with procedure-related thrombotic complications [10]. In our observation, the slightly increased retrieval time did not lead to recurrent caval thrombus. We gave therapeutic anticoagulation to all patients to minimize thrombotic complication.
The retrieval time window of different filtration devices varies among devices. The OptEase vena cave filter and Aegisy vena cava filter are both available as retrievable filters with short recommended in-dwell time due to extensive contact of the filter side struts with the inferior vena cava wall and subsequent neointimal hyperplasia leading to incorporation. Histologic evidence of specimens confirmed this mechanism. With prompt clinical follow-up evaluation for timely filter removal, the number of required aggressive retrieval procedures has decreased. However, an estimated 15% of retrievable IVC filters cannot be removed in a timely manner for various reasons [9]. Our results clearly demonstrate that the filter can be removed without complications after a longer period of time than the recommended retrieval window with bidirectional pull-back technique.
Conclusions
In conclusion, since we cannot determine a method to resolve all filter retrieval of various types, the choice of which advanced technique to use was operator-dependent and not objectively assigned. The emphasis on an individualized plan will be helpful for filter retrieval. The bidirectional pull-back technique is safe and efficient, which would be especially advantageous for strut-embedded cylinder-shaped filters such as the OptEase and Aegisy after a failed standard attempt. Additionally, this method may also be helpful in retrieving cylinder-shaped permanent filter such as the TrapEase when no longer needed.
Footnotes
Source of support: This work was supported by grants from the National Natural Science Foundation of China (No. 81400345, No. 30972941), Jiangsu Provincial Health Department’s Medical Science Program (H201211), and the Graduate Research and Innovation Program in Colleges and Universities of Jiangsu Province (No. 1265)
References
- 1.Fanikos J, Rao A, Seger AC, et al. Hospital costs of acute pulmonary embolism. Am J Med. 2013;126(2):127–32. doi: 10.1016/j.amjmed.2012.07.025. [DOI] [PubMed] [Google Scholar]
- 2.Al-Hakim R, Kee ST, Olinger K, et al. Inferior vena cava filter retrieval: Effectiveness and complications of routine and advanced techniques. J Vasc Interv Radiol. 2014;25(6):933–39. doi: 10.1016/j.jvir.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 3.Jiang J, Tu J, Jia Z, et al. Incidence and outcomes of inferior vena cava filter thrombus during catheter-directed thrombolysis for proximal deep venous thrombosis. Ann Vasc Surg. 2017;38:305–9. doi: 10.1016/j.avsg.2016.05.108. [DOI] [PubMed] [Google Scholar]
- 4.Stein PD, Matta F, Hull RD. Increasing use of vena cava filters for prevention of pulmonary embolism. Am J Med. 2011;124(7):655–61. doi: 10.1016/j.amjmed.2011.02.021. [DOI] [PubMed] [Google Scholar]
- 5.Ross J, Allison S, Vaidya S, Monroe E. Günther Tulip inferior vena cava filter retrieval using a bidirectional loop-snare technique. Diagn Interv Radiol. 2016;22(5):460–62. doi: 10.5152/dir.2016.15475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stavropoulos SW, Ge BH, Mondschein JI, et al. Retrieval of tip-embedded inferior vena cava filters by using the endobronchial forceps technique: Experience at a single institution. Radiology. 2015;275(3):900–7. doi: 10.1148/radiol.14141420. [DOI] [PubMed] [Google Scholar]
- 7.Van Ha TG, Kang L, Lorenz J, et al. Difficult OptEase filter retrievals after prolonged indwelling times. Cardiovasc Intervent Radiol. 2013;36(4):1139–43. doi: 10.1007/s00270-013-0619-x. [DOI] [PubMed] [Google Scholar]
- 8.Kuo WT, Odegaard JI, Louie JD, et al. Photothermal ablation with the excimer laser sheath technique for embedded inferior vena cava filter removal: Initial results from a prospective study. J Vasc Intervent Radiol. 2011;22(6):813–23. doi: 10.1016/j.jvir.2011.01.459. [DOI] [PubMed] [Google Scholar]
- 9.Ray CE, Jr, Mitchell E, Zipser S, et al. Outcomes with retrievable inferior vena cava filters: A multicenter study. J Vasc Intervent Radiol. 2006;17(10):1595–604. doi: 10.1097/01.RVI.0000239102.02956.65. [DOI] [PubMed] [Google Scholar]
- 10.Kuo WT, Tong RT, Hwang GL, et al. High-risk retrieval of adherent and chronically implanted IVC filters: techniques for removal and management of thrombotic complications. J Vasc Intervent Radiol. 2009;20(12):1548–56. doi: 10.1016/j.jvir.2009.08.024. [DOI] [PubMed] [Google Scholar]
- 11.Al-Hakim R, Mcwilliams JP, Derry W, Kee ST. The hangman technique: A modified loop snare technique for the retrieval of inferior vena cava filters with embedded hooks. J Vasc Intervent Radiol. 2015;26(1):107–10. doi: 10.1016/j.jvir.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 12.PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d’Embolie Pulmonaire par Interruption Cave) randomized study. Circulation. 2005;112(3):416–22. doi: 10.1161/CIRCULATIONAHA.104.512834. [DOI] [PubMed] [Google Scholar]
- 13.Sarosiek S, Crowther M, Sloan JM. Indications, complications, and management of inferior vena cava filters: the experience in 952 patients at an academic hospital with a level I trauma center. JAMA. 2013;173(7):513–17. doi: 10.1001/jamainternmed.2013.343. [DOI] [PubMed] [Google Scholar]
- 14.Van Ha TG, Vinokur O, Lorenz J, et al. Techniques used for difficult retrievals of the Gunther Tulip inferior vena cava filter: Experience in 32 patients. J Vasc Intervent Radiol. 2009;20(1):92–99. doi: 10.1016/j.jvir.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 15.Iliescu B, Haskal ZJ. Advanced techniques for removal of retrievable inferior vena cava filters. Cardiovasc Intervent Radiol. 2012;35(4):741–50. doi: 10.1007/s00270-011-0205-z. [DOI] [PubMed] [Google Scholar]
- 16.SS, NY, AT Successful retrieval by loop-J-type wire technique for useless superior hook of the Günther Tulip inferior vena cava filter surrounded by the clot. Jpn J Phlebol. 2009;20:257–63. [Google Scholar]
- 17.Rubenstein L, Chun AK, Chew M, Binkert CA. Loop-snare technique for difficult inferior vena cava filter retrievals. J Vasc Intervent Radiol. 2007;18(10):1315–18. doi: 10.1016/j.jvir.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Stavropoulos SW, Dixon RG, Burke CT, et al. Embedded inferior vena cava filter removal: Use of endobronchial forceps. J Vasc Intervent Radiol. 2008;19(9):1297–301. doi: 10.1016/j.jvir.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 19.Van Ha TG, Chien AS, Funaki BS, et al. Use of retrievable compared to permanent inferior vena cava filters: A single-institution experience. Cardiovasc Intervent Radiol. 2008;31(2):308–15. doi: 10.1007/s00270-007-9184-5. [DOI] [PubMed] [Google Scholar]
- 20.Nakashima M, Kobayashi H, Kobayashi M. Troubleshooting OptEase inferior vena cava filter retrieval. Asian Cardiovasc Thorac Ann. 2016;24(1):36–38. doi: 10.1177/0218492314534251. [DOI] [PubMed] [Google Scholar]
- 21.Stavropoulos SW, Solomon JA, Trerotola SO. Wall-embedded recovery inferior vena cava filters: Imaging features and technique for removal. J Vasc Intervent Radiol. 2006;17(2 Pt 1):379–82. doi: 10.1097/01.RVI.0000196354.45643.5A. [DOI] [PubMed] [Google Scholar]
- 22.Al-Hakim R, Kee ST, Olinger K, et al. Inferior vena cava filter retrieval: Effectiveness and complications of routine and advanced techniques. J Vasc Intervent Radiol. 2014;25(6):933–40. doi: 10.1016/j.jvir.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 23.Kuo WT, Odegaard JI, Rosenberg JK, Hofmann LV. Excimer laser-assisted removal of embedded inferior vena cava filters: A single-center prospective study. Circ Cardiovasc Interv. 2013;6(5):560–66. doi: 10.1161/CIRCINTERVENTIONS.113.000665. [DOI] [PubMed] [Google Scholar]
- 24.Keller IS, Meier C, Pfiffner R, et al. Clinical comparison of two optional vena cava filters. J Vasc Intervent Radiol. 2007;18(4):505–11. doi: 10.1016/j.jvir.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 25.Pellerin O, Barral FG, Lions C, et al. Early and late retrieval of the ALN removable vena cava filter: results from a multicenter study. Cardiovasc Intervent Radiol. 2008;31(5):889–96. doi: 10.1007/s00270-008-9357-x. [DOI] [PubMed] [Google Scholar]
- 26.Stavropoulos SW, Sing RF, Elmasri F, et al. The DENALI trial: An interim analysis of a prospective, multicenter study of the denali retrievable inferior vena cava filter. J Vasc Intervent Radiol. 2014;25(10):1497–505. doi: 10.1016/j.jvir.2014.07.001. e1491. [DOI] [PubMed] [Google Scholar]
- 27.Rimon U, Bensaid P, Golan G, et al. Optease vena cava filter optimal indwelling time and retrievability. Cardiovasc Intervent Radiol. 2011;34(3):532–35. doi: 10.1007/s00270-010-9920-0. [DOI] [PubMed] [Google Scholar]