Abstract
Pigmented villonodular synovitis (PVNS) is a rare proliferative disorder of the synovial membrane. This condition is usually monoarticular, can be locally destructive, and involves muscles, tendons, bursae, bones, and skin. The most commonly affected joints are the knee and hip, followed by the ankle and shoulder. Patients often present with pain, swelling, and joint effusion; however, the duration of symptoms varies. Total synovectomy is the preferred treatment for PVNS. Subtotal synovectomy is a factor of recurrence, and in diffuse PVNS, total excision is very difficult to achieve. Radiotherapy may have an adjunctive role, particularly in incomplete resection or as a treatment of salvation in recurrent cases. This treatment modality has low toxicity levels and enables satisfactory joint function. This is a case report of a rare case of diffuse PVNS of the shoulder that was treated with partial arthroscopic synovectomy and adjuvant radiotherapy. A 74-year-old male patient presented with gradual onset pain, hemarthrosis, and functional impairment of the right shoulder without previous trauma history. Magnetic resonance imaging of the shoulder demonstrated a diffuse synovial thickening that was compatible with PVNS and rotator cuff destruction. The lesion was partially excised by arthroscopy. The patient underwent adjuvant radiation therapy with a total dose of 40 Gy/20 fractions/4 weeks. At the final follow-up, i.e., 1 month after treatment, the patient had increased shoulder mobility and no pain, with a mild change in cutaneous pigmentation. Radiation therapy is safe and effective in treating and preventing recurrence of diffuse PVNS, particularly after incomplete synovectomy.
Keywords: Radiotherapy, pigmented villonodular synovitis, arthroscopic synovectomy
Introduction
Pigmented villonodular synovitis (PVNS) is a rare proliferative disease that usually affects the synovial membrane of joints or tendon sheaths resulting in joint swelling and bone erosion, affecting 2.4% of cases the shoulder joint (1). The hip is the second most common joint to be affected, just behind the knee. Although recurrence is high, malignancy is rare (2).
Symptoms depend on the location of PVNS occurring. Localized extra-articular PVNS clinically presents as a painful soft tissue mass. Common symptoms that are associated with the intra-articular PVNS type are pain and swelling. PVNS can have a variable evolution, leading to local destruction and severe symptoms, including arthralgia, edema, joint effusion, erythema, and limitation in the range of motion.
Radiographs of patients with diffuse intra-articular PVNS may appear normal or may reveal joint effusion, soft tissue edema, or extrinsic erosion with associated sclerosis. The lesions are best visualized through magnetic resonance imaging (MRI). MRI is a useful non-invasive means of diagnosis based on hypodense, diffuse infiltrative lesion involving soft tissue structures in T1 and T2. Hemosiderin causes a decreased signal with both T1 and T2 images. Although MRI is very sensitive for diagnosing these lesions, PVNS is non-specific and is often confused with rheumatoid arthritis or soft tissue sarcomas (3).
Histologically, PVNS reveals a hypertrophic synovial process that is characterized by villous, nodular, or villonodular proliferation and hemosiderin pigmentation. The following two types are described: diffuse (when a compartment or the entire synovial membrane of a given joint is affected) or localized (single mass). Macroscopically, PVNS appears as a reddish-brown synovial thickening with numerous villous projections (4).
The ideal treatment of PVNS is surgical excision. Complete excision may be limited by the proximity of the neurovascular bundle. In patients with localized disease, a wide excision generally minimizes the chance of local recurrence.
Pathological synovial tissue should be removed as completely as possible. Complete synovectomy is the preferred treatment for PVNS. The incomplete removal can likely result in the recurrence of the lesion. Localized PVNS has an excellent prognosis and a low recurrence rate when surgically treated. Diffuse PVNS is more difficult to eradicate and is preferably treated with total or almost total synovectomy. Its recurrence rate is up to 46%, without an adjuvant treatment (5).
Moderate dose external radiotherapy (RT) can improve the probability of local control in patients with refractory PVNS and in incompletely resected or unresectable cases. Moreover, adjuvant therapy with an intra-articular instillation of radioactive isotope or cryosurgery can be considered for patients who are believed to have a high risk of recurrence.
We report a case of diffuse PVNS of the shoulder that was treated with partial arthroscopic synovectomy and adjuvant RT.
Case Presentation
A 74-year-old male patient presented with pain and swelling of the right shoulder with 8 months of evolution. He had no history of trauma and required help from a third person for basic daily activities.
On examination, there were no inflammatory signs besides swelling of the shoulder. Furthermore, the patient had pain during mobilization and rotator cuff insufficiency. The neurological examination was normal.
The patient attended the emergency department several times because of acute episodes of pain and swelling of his right shoulder. Arthrocentesis was performed in some episodes, with repeated drainage of large amounts of hematic fluid giving immediate but temporary pain relief.
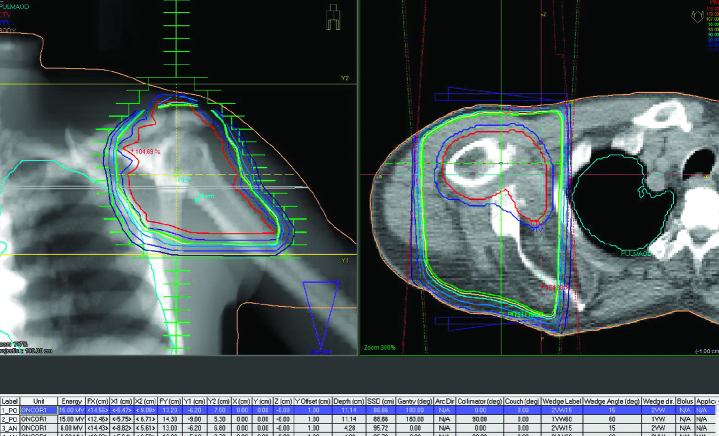
MRI revealed a generalized hypertrophy of the synovial membrane with low signal intensity on T1 and T2, as well as destruction of the acromioclavicular and glenohumeral joints, compatible with diffuse PVNS (Figure 1, 2).
Figure 1.
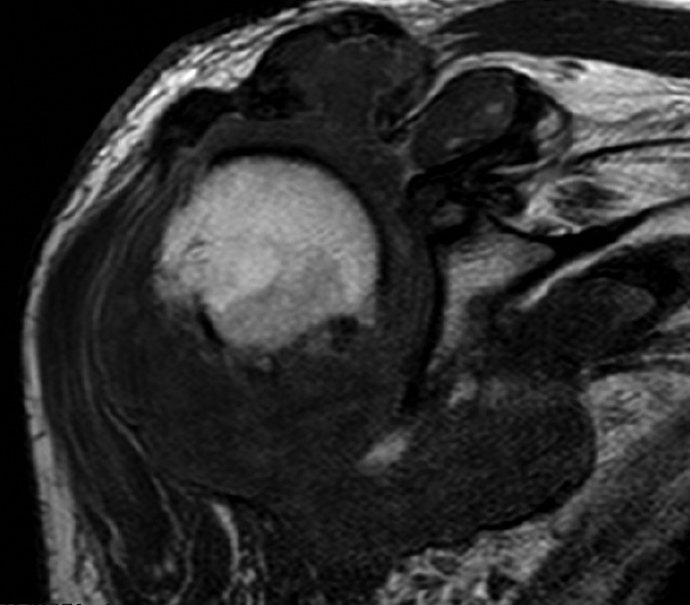
Pigmented villonodular synovitis of the shoulder. Coronal T1-weighted magnetic resonance imaging
Figure 2.
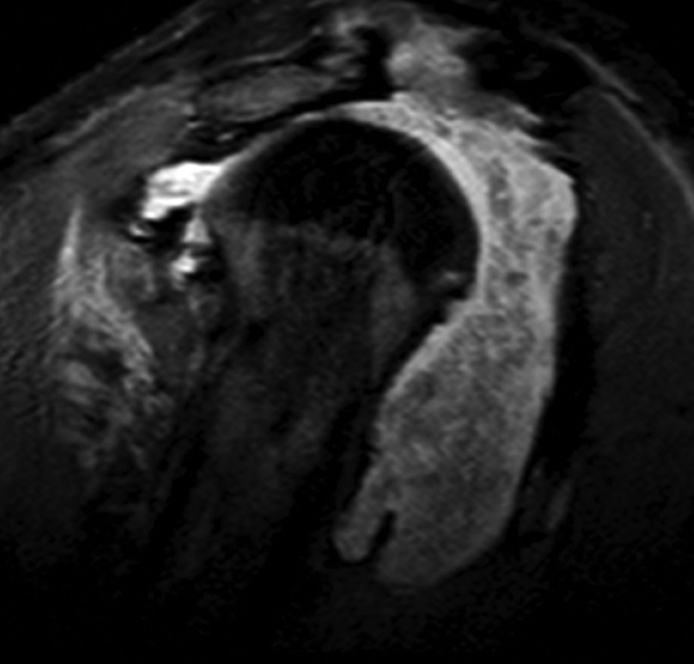
Pigmented villonodular synovitis of the shoulder. Sagittal T2-weighted magnetic resonance imaging
The patient underwent shoulder arthroscopy, which verified the presence of an extensive synovial lesion and destruction of the acromioclavicular and glenohumeral joints. Near-total synovectomy and subacromial space shaving were performed (Figure 3, 4). There were no surgical complications, and there was pain relief and a mild increase in the shoulder range of motion at discharge from the hospital on the postoperative day 7.
Figure 3.
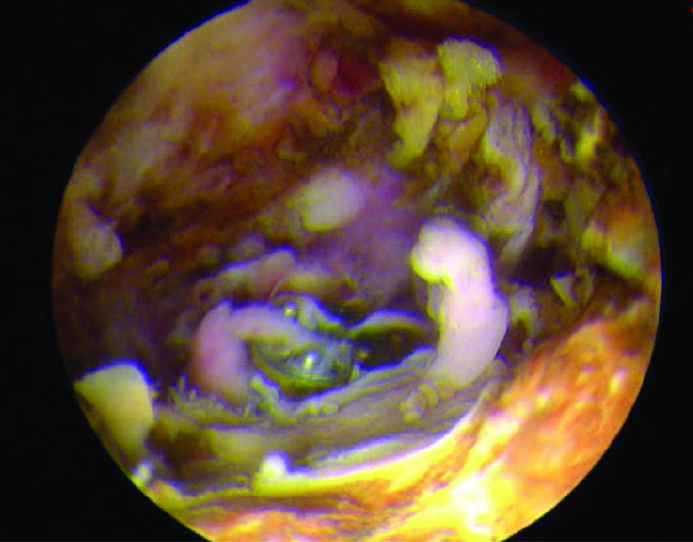
Intraoperative arthroscopic pictures demonstrating synovial proliferation suggestive of pigmented villonodular synovitis
Figure 4.
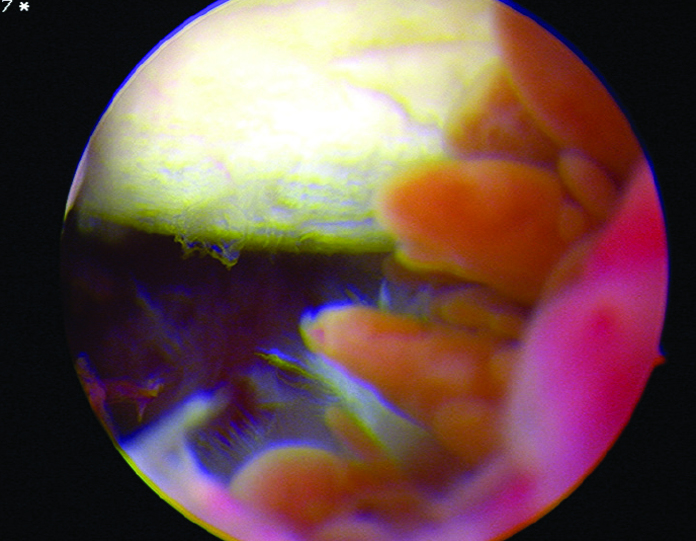
Intraoperative arthroscopic pictures demonstrating synovial proliferation suggestive of pigmented villonodular
Histological examination of the excision piece described characteristics compatible with PVNS, with areas of extensive necrosis and the presence of hemosiderin deposits.
Because of incomplete synovial excision and histological confirmation of PVNS diagnosis, the patient was referred to the Radiation Oncology Department.
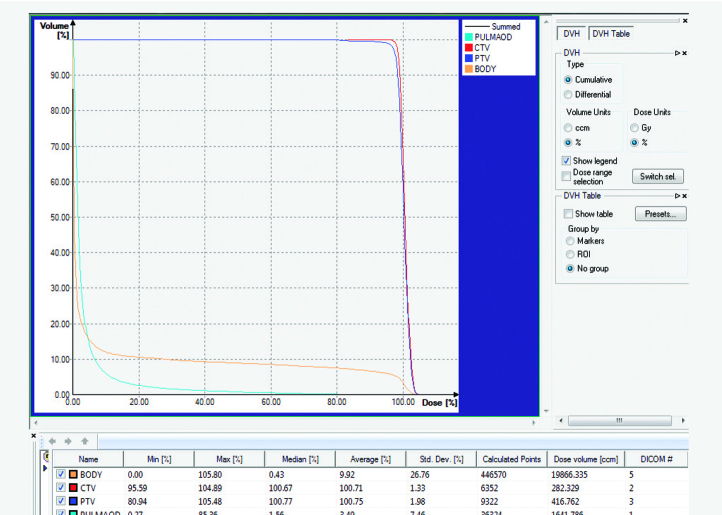
Eight weeks after surgery, the patient was evaluated in the Radiation Oncology Department for further treatment. At examination, the patient presented with impaired shoulder mobilization without associated pain or other symptoms. A computed tomography-based treatment planning system was performed to ensure optimal dose distribution. The patient underwent RT treatment in the supine position with an axillar wedge to ensure a reproducible positioning using a linear accelerator and 15 and 6 MV photons. A total dose of 40 Gy/20 fractions/4 weeks was prescribed as the planning target volume, which was defined as the whole synovial space and residual lesion as evidenced by a preoperative MRI plus a margin of 1 cm (Figure 5, 6). RT was performed on an outpatient basis, and the treatment was well tolerated with only an acute grade I axillary radiodermitis and a mild painless swelling of the right shoulder.
Figure 5.
Multi-plane view of dose distribution on the shoulder
Figure 6.
Dose-volume histogram
The patient was observed at 1-month follow-up consultation by a radiation oncology physician and an orthopedic surgeon and remained painless, with increased right shoulder mobility, and only a mild change in skin pigmentation of the irradiated area without fibrosis or joint stiffness. The patient refused further follow-up because of the absence of symptoms and because of economic issues. Informed consent was obtained from the patient for publication of the present case.
Discussion
Pigmented villonodular synovitis is a rare but locally invasive benign disease with significant potential for articular severe morbidity. A combination of clinical, radiological, and histological correlation is needed for the diagnosis of PVNS.
Published experience regarding RT treatment in PVNS has been confined to small case reports or small series.
Radiotherapy for benign diseases generally causes skepticism because of potential somatic changes. RT inevitably harbors the risk of the subsequent development of second primary tumors, but malignant induction is a rare event in absolute terms. Despite these concerns, there has been a failure to identify any cases of malignant transformation after RT in the literature (6).
The indication criteria for postoperative treatment of PVNS are not clearly defined. However, a recurrent and aggressive behavior of diffuse PVNS is usually considered an indication to perform further treatment.
The German Cooperative Group on Radiotherapy in Benign Diseases performed a study that collected data from one of the largest cohorts of patients ever reported on the use of RT for PVNS. 41 patients were included in the study: 30 (73.2%) received postoperative RT, because of primary incomplete resection, and 11 (26.8%) as an adjunct after complete resections of recurrences or unclear resection status. The total doses ranged from 30 to 50 Gy. Local control was achieved in 95.1% of patients and 82.9% had no or only slight functional impairment (7).
Surgical synovectomy remains the treatment of choice for PVNS. Local synovectomy should be performed only in localized, early-stage disease. As the disease progresses, total synovectomy or total shoulder arthroplasty are indicated. Mahieu et al. (8) reported two cases of PVNS of the shoulder treated with arthroscopy, where neither of the patients had a recurrence of the disease.
In patients with a diffuse form of the disease, ample synovectomy may minimize the probability of local recurrence. Shoulder arthroscopy enables easier exploration for synovectomy. Radiotherapy is a safe and effective postoperative option in the treatment of diffuse PVNS after partial synovectomy and has an excellent prognosis and provides local control of the disease.
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: Written informed consent was obtained from patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - T.S., J.M.; Design - T.S., J.M.; Supervision - F.A., M.H., G.M.; Resources - T.S., J.M., Z.G., F.A.; Materials - T.S., J.M., Z.G.; Data Collection and/or Processing - T.S., J.M., Z.G.; Analysis and/or Interpretation - T.S., J.M., Z.G.; Literature Search - T.S., J.M.; Writing Manuscript - T.S., J.M.; Critical Review - F.A., M.H., G.M.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Rao A, Vigorita V. Pigmented villonodular synovitis (giant-cell tumor of the tendon sheath and synovial membrane). A review of eighty-one cases. J Bone Joint Surg Am. 1984;66:76–94. https://doi.org/10.2106/00004623-198466010-00012. [PubMed] [Google Scholar]
- 2.Bertoni F, Unni KK, Beabout JW, Sim FH. Malignant giant cell tumor of the tendon sheaths and joints. Am J Surg Pathol. 1997;21:153–63. doi: 10.1097/00000478-199702000-00004. https://doi.org/10.1097/00000478-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Harris O, Ritchie DA, Maginnis R, Lamb GR, Helliwell T, Jane M, et al. MRI of giant cell tumor of tendon sheath and nodular synovitis of the foot and ankle. Foot. 2003;13:19–29. https://doi.org/10.1016/S0958-2592(02)00116-5. [Google Scholar]
- 4.Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch Pathol. 1941;31:731–65. [Google Scholar]
- 5.Flandry F, Hughston JC. Pigmented villonodular synovitis. J Bone Joint Surg Am. 1987;69:942–9. https://doi.org/10.2106/00004623-198769060-00026. [PubMed] [Google Scholar]
- 6.Mollon B, Lee A, Busse J, Griffin A, Ferguson P, Wunder J, et al. The effect of surgical synovectomy and radiotherapy on the rate of recurrence of pigmented vollonodular synovitis of the knee. Bone Joint J. 2015;97:550–7. doi: 10.1302/0301-620X.97B4.34907. https://doi.org/10.1302/0301-620X.97B4.34907. [DOI] [PubMed] [Google Scholar]
- 7.Heyd R, Micke O, Berger B, Eich H, Ackermann H, Seegenschmiedt M, et al. Radiation therapy for treatment of pigmented villonodular synovitis: results of a national patterns of care study. Int J Radiation Oncology Biol Phys. 2010;78:199–204. doi: 10.1016/j.ijrobp.2009.07.1747. https://doi.org/10.1016/j.ijrobp.2009.07.1747. [DOI] [PubMed] [Google Scholar]
- 8.Mahieu X, Chaouat G, Blin J, Frank A, Hardy P. Arthroscopic treatment of pigmented villonodular synovitis of the shoulder. Arthroscopy. 2001;17:81–7. doi: 10.1053/jars.2001.7803. https://doi.org/10.1053/jars.2001.7803. [DOI] [PubMed] [Google Scholar]