Abstract
Lupus myelitis (LM) is a rare but serious complication of systemic lupus erythematosus (SLE). In 2009, Birnbaum et al. suggested that LM could be classified into two subtypes, namely gray and white matter myelitis, based on neurological examination findings. Here we describe three cases of this disorder, one with signs of white matter dysfunction and two with signs of gray matter dysfunction. We discuss the potential role of autoantibodies in the development of LM.
Keywords: Lupus myelitis, systemic lupus erythematosus, transverse myelitis, lupus anti-coagulant, anti-cardiolipin antibody, anti-cardiolipin beta-2 glicoprotein-1 antibody
Introduction
Lupus myelitis (LM) is a rare but serious condition reported in 1%–2% of patients with systemic lupus erythematosus (SLE) (1). Although more than half of patients with this disorder respond to therapy, a significant number of patients develop permanent paraplegia and sphincter dysfunction (2, 3). A recent systematic review showed that LM with anti-phospholipid antibodies (aPL) was significantly associated with a low frequency of paralysis at presentation (21% vs. 50% in LM without aPL) and tended to occur as an initial manifestation of SLE (45% vs. 23%). Here we describe three cases of this disorder and discuss a possible role of autoantibodies in the development of LM.
Case Presentations
Case 1
A 31-year-old Filipino woman with a 2-year history of lupus was admitted for severe abdominal pain due to bladder rupture. Three weeks previously, she presented with fever and cervical lymphadenopathy. A moderate dose of prednisolone improved her symptoms. At this visit, she also started to notice weakness in her lower extremities and urinary disturbance. On admission, neurological examination showed spastic paraparesis with brisk deep tendon reflex, which later caused her to become bedridden. Ophthalmologic examination revealed a defect of the central part of the visual field of her left eye, and she was diagnosed with retrobulbar optic neuritis. Cerebrospinal analysis revealed albuminocytologic dissociation. Although magnetic resonance imaging (MRI) was performed because of claustrophobia, she was diagnosed as having LM and optic neuritis. Intravenous cyclophosphamide (IVCY) and methyl prednisolone (IVMP) therapy improved her symptoms. At 18 months after the admission, she now walks with a stick by herself but needs urinary catheterization. Lupus-specific antibodies in the cases are listed in Table 1.
Table 1.
Antibody profile of the three cases with lupus myelitis
| Case | ANA | dsDNA | DNA | RNP | Sm | SSA | SSB | aCL | aCLB2GP1 | LA | BFP | DCT | AQP4 | RP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | (+) | (−) | (−) | (+) | (+) | (+) | (−) | (−) | (−) | (−) | (−) | (−) | (−) | NA |
| 2 | (+) | (+) | NA | (−) | (−) | (−) | (−) | NA | (+) | (+) | (+) | NA | (−) | (−) |
| 3 | (+) | (−) | (−) | (−) | (−) | (−) | (−) | (+) | (+) | (+) | (−) | NA | NA | NA |
ANA: anti-nuclear antibody; dsDNA: anti-double-strand deoxyribonucleic acid antibody; DNA: anti-deoxyribonucleic acid antibody (radioimmunoassay); RNP: anti-ribonucleoprotein antibody; Sm: anti-Smith antibody; SSA: anti-SSA/Ro antibody; SSB: anti-SSB/La antibody; aCL: anti-cardiolipin antibody; aCLB2GP1: anti-cardiolipin beta-2 glicoprotein-1 antibody; LA: lupus anticoagulant; BFP: biological false-positive for syphilis; DCT: direct Coombs test; AQP4: anti-aquaporin-4 antibody; RP: anti-ribosomal P antibody; NA: not available
Case 2
A 25-year-old Japanese woman with a 4-year-history of lupus was admitted with a diagnosis of aseptic meningitis. She presented with headache and vomiting for 4 days. Empiric antibiotic therapy was initiated. On the third hospital day, she noticed urinary disturbance. On the fourth hospital day, when she woke up, she had paresthesia below the T10 vertebrae and flaccid paraplegia. Spinal MRI revealed longitudinally extensive transverse myelitis (LETM) in the entire spinal cord (Figure 1). Treatment with IVMP, plasmapheresis, and IVCY never improved her symptoms. Seventy months after her admission, she was condemned to a wheelchair and requires urinary catheterization.
Figure 1 a–c.
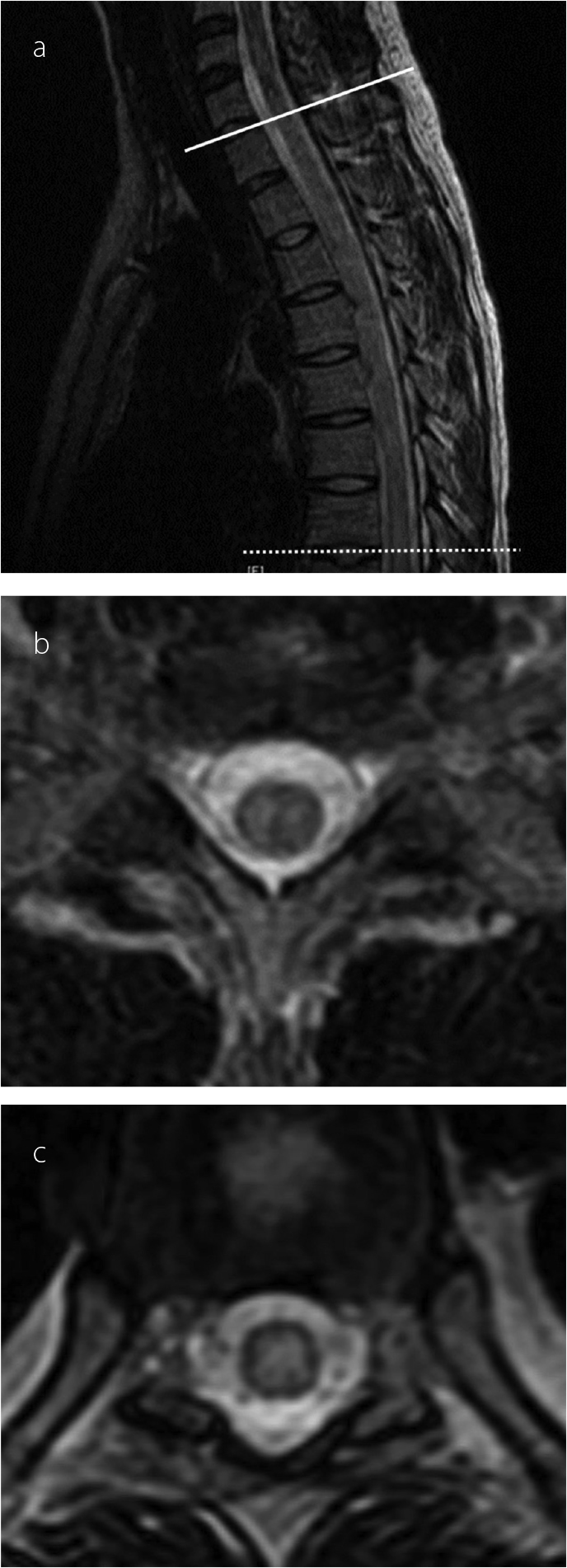
Sagittal T2-weighted magnetic resonance image of the spine in Case 2 demonstrating high intensity in the spinal cord. A solid line is drawn between the seventh cervical vertebra and the first thoracic vertebra, and a dotted line is drawn between the seventh and eighth thoracic vertebrae (a). Transverse views between the seventh cervical and first thoracic vertebrae (b) and between the seventh and eighth thoracic vertebrae (c) also show a high-intensity intraspinal area.
Case 3
A previously healthy 35-year-old Japanese woman presented with paraplegia. One day, she noticed urinary disturbance in the morning and had walking difficulty in the daytime. In the evening, she was admitted to the previous hospital. However, flaccid paraplegia developed the next morning. Laboratory data revealed lymphopenia, thrombocytopenia, aPL, and anti-nuclear antibody (1:160). Spinal MRI revealed LETM at C7 to Th7 (Figure 2). Because her myelitis could not be anatomically explained by the ischemic etiology owing to aPL, she was diagnosed with LM. Treatment with IVMP and plasmapheresis never improved her symptoms. Thirty-eight months after disease onset, she required a wheelchair and urinary catheterization.
Figure 2 a–c.
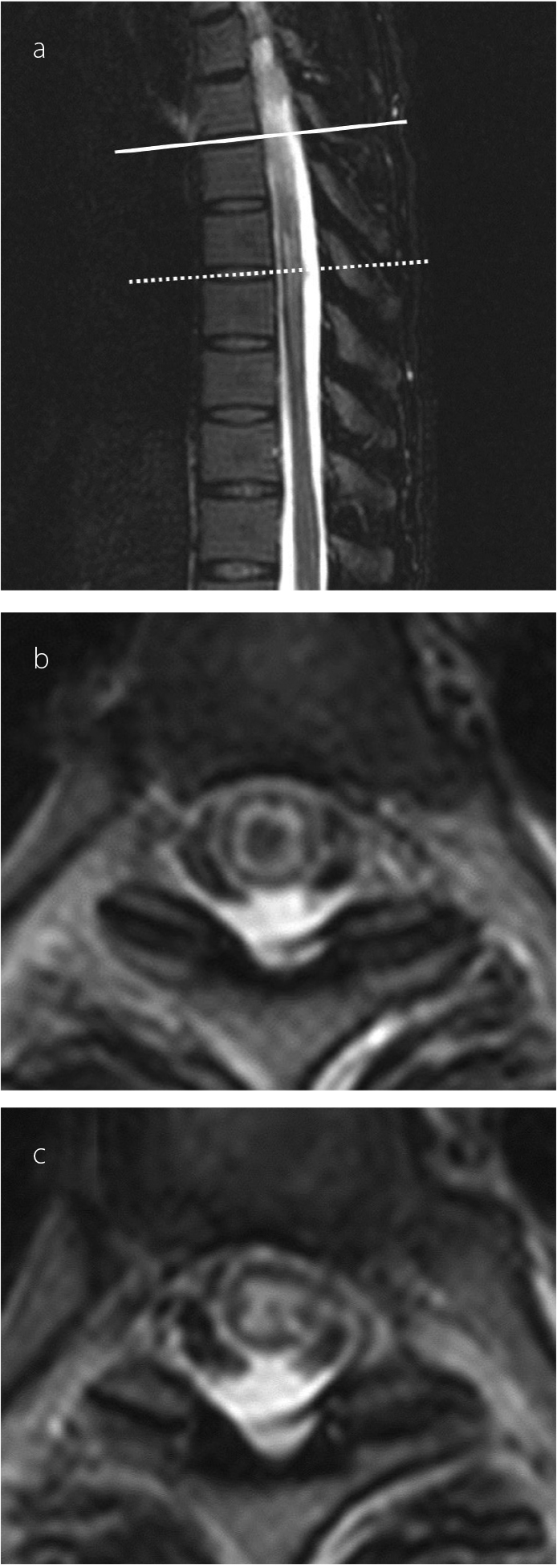
Sagittal T2-weighted magnetic resonance image of the spine in Case 3 demonstrating high intensity in the spinal cord. A solid line is drawn between the fourth and fifth thoracic vertebrae, and a dotted line is drawn between the sixth and seventh thoracic vertebrae (a). Transverse views between the fourth and fifth thoracic vertebrae (b) and between the sixth and seventh thoracic vertebrae (c) also show a high-intensity intraspinal area.
Informed consent for the study was obtained from all our patients at the initial visit. Lupus-specific antibodies in the cases are listed in Table 1.
Discussion
The clinical manifestation of LM is characterized by acute or subacute onset of weakness and paraesthesia of the limbs, especially the lower limbs, in synchronization with or independent of lupus activity (1, 2). Birnbaum et al. (2) retrospectively analyzed 22 LM cases and classified them into two subtypes: 11 cases each of gray matter myelitis (i.e., flaccidity and hyporeflexia) and white matter myelitis (i.e., spasticity and hyperreflexia). Patients with gray matter myelitis deteriorated more rapidly to a clinical nadir within 6 h and had a poor outcome (persistent paraplegia in 10 of the 11 cases). However, patients with white matter myelitis frequently responded to therapy and had a favorable outcome (no persistent paraplegia). As their observation, case 1, with signs of white matter dysfunction, presented with progressive weakness of the lower extremities within 3 weeks and responded to therapy. Cases 2 and 3, with signs of gray matter dysfunction, had acute onset of paraplegia within 12 h, never responded to therapy, and subsequently had persistent paraplegia.
In their study, six (55%) of 11 patients with white matter myelitis had lupus anti-coagulant (LAC), which was negative in all the 11 patients with gray matter myelitis. In contrast to their observation, LAC was positive in our two cases of gray matter myelitis. Furthermore, cases similar to our cases of gray matter myelitis and LAC have been reported (4, 5).
One of our cases (case 1) with signs of white matter dysfunction also had optic neuritis in the right eye, but the patient’s condition did not satisfy the revised 2006 neuromyelitis optica (NMO) diagnostic criteria because MRI was not performed (6). The test result for anti-aquaporin-4 antibody was negative in the two cases (case 1 and 2). In the study by Birnbaum et al, five (46%) of 11 cases of white matter myelitis met the criteria, whereas none of the 11 cases of gray matter myelitis met the criteria (p=0.04). However, several cases of gray matter myelitis and optic neuritis have also been reported, including cases that satisfied the NMO criteria (7–9).
A possible role of autoantibodies, especially aPL, in the subtypes of LM has been only based on this retrospective study with a small number of samples. Therefore, a systematic review with a meta-analysis that includes a larger number of cases of LM and focuses on the role of autoantibody in the development of LM and its subtype is needed. In conclusion, the present cases of lupus myelitis had similar characteristics in terms of the clinical course and outcomes of gray and white matter myelitis but not the pattern of autoantibodies.
Acknowledgements
The authors thank Dr. Akira Kuriyama for his helpful advice for this article.
Footnotes
Ethics Committee Approval: The patients in this report were among the participants of Cohort of rheumatic diseases in Hiroshima City Hospital (CORCH) study. This study was approved by the institutional review board at our hospital.
Informed Consent: Written informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - H.O.; Design - H.O.; Supervision - E.S.; Resources - H.O., E.S.; Materials - H.O., T.Y., M.K., Y.M., D.A., T.Y., E.S.; Data Collection and/or Processing - H.O.; Analysis and/or Interpretation - H.O.; Literature Search - H.O.; Writing Manuscript - H.O.; Critical Review - E.S.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: Dr. Oiwa reports lecture fees from Astellas, Ayumi, Daiichi-Sankyo, Eisai, and Dainippon Sumitomo, outside the submitted work; Dr. Kawashima reports lecture fees from Pfizer, Takeda, Abbvie, Eisai, Chugai, Jansen, Kyowa Kirin, outside the submitted work.
References
- 1.Bhat A, Naguwa S, Cheema G, Gershwin ME. The epidemiology of transverse myelitis. Autoimmun Rev. 2010;9:A395–9. doi: 10.1016/j.autrev.2009.12.007. https://doi.org/10.1016/j.autrev.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 2.Birnbaum J, Petri M, Thompson R, Izbudak I, Kerr D. Distinct subtypes of myelitis in systemic lupus erythematosus. Arthritis Rheum. 2009;60:3378–87. doi: 10.1002/art.24937. https://doi.org/10.1002/art.24937. [DOI] [PubMed] [Google Scholar]
- 3.Katsiari CG, Giavri I, Mitsikostas DD, Yiannopoulou KG, Sfikakis PP. Acute transverse myelitis and antiphospholipid antibodies in lupus. No evidence for anticoagulation. Eur J Neurol. 2011;18:556–63. doi: 10.1111/j.1468-1331.2010.03208.x. https://doi.org/10.1111/j.1468-1331.2010.03208.x. [DOI] [PubMed] [Google Scholar]
- 4.Téllez-Zenteno JF, Remes-Troche JM, Negrete-Pulido RO, Dávila-Maldonado L. Longitudinal myelitis associated with systemic lupus erythematosus: clinical features and magnetic resonance imaging of six cases. Lupus. 2001;10:851–6. doi: 10.1191/096120301701548490. https://doi.org/10.1191/096120301701548490. [DOI] [PubMed] [Google Scholar]
- 5.Deodhar AA, Hochenedel T, Bennett RM. Longitudinal involvement of the spinal cord in a patient with lupus related transverse myelitis. J Rheumatol. 1999;26:446–9. [PubMed] [Google Scholar]
- 6.Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology. 2006;66:1485–9. doi: 10.1212/01.wnl.0000216139.44259.74. https://doi.org/10.1212/01.wnl.0000216139.44259.74. [DOI] [PubMed] [Google Scholar]
- 7.Hernando Rubio I, Belzunegui Otano J, Máiz Alonso O, Alvarez Rodríguez B. Transverse myelitis and bilateral optic neuritis in a patient with systemic lupus erythematosus. Reumatol Clin. 2012;8:298–9. doi: 10.1016/j.reuma.2012.01.005. https://doi.org/10.1016/j.reuma.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 8.Hagiwara N, Toyoda K, Uwatoko T, Yasumori K, Ibayashi S, Okada Y. Successful high dose glucocorticoid treatment for subacute neuromyelitis optica with systemic lupus erythematosus. Intern Med. 2005;44:998–1001. doi: 10.2169/internalmedicine.44.998. https://doi.org/10.2169/internalmedicine.44.998. [DOI] [PubMed] [Google Scholar]
- 9.Neuromyelitis optica (Devic’s syndrome) in systemic lupus erythematosus: a case report.


