Abstract
Many conditions may affect the temporomandibular joint (TMJ), but its incidence in individual joint diseases is low. However, inflammatory arthropathies, particularly rheumatoid and psoriatic arthritis and ankylosing spondylitis, appear to have a propensity for affecting the joint. Symptoms include pain, restriction in mouth opening, locking, and noises, which together can lead to significant impairment. Jaw rest, a soft diet, a bite splint, and medical therapy, including disease-modifying antirheumatic drugs (DMARDs) and simple analgesia, are the bedrock of initial treatment and will improve most symptoms in most patients. Symptom deterioration does not necessarily follow disease progression, but when it does, TMJ arthroscopy and arthrocentesis can help modulate pain, increase mouth opening, and relieve locking. These minimally invasive procedures have few complications and can be repeated. Operations to repair or remove a damaged intra-articular disc or to refine joint anatomy are used in select cases. Total TMJ replacement is reserved for patients where joint collapse or fusion has occurred or in whom other treatments have failed to provide adequate symptomatic control. It yields excellent outcomes and is approved by the National Institute of Health and Care Excellence (NICE), UK. Knowledge of the assessment and treatment of the TMJ, which differs from other joints affected by inflammatory arthritis due to its unique anatomy and function, is not widespread outside of the field of oral and maxillofacial surgery. The aim of this article is to highlight the peculiarities of TMJ disease secondary to rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis and how to best manage these ailments, which should help guide when referral to a specialist TMJ surgeon is appropriate.
Keywords: Temporomandibular joint, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, arthroscopy, joint replacement
Introduction
The incidence of temporomandibular joint (TMJ) involvement in inflammatory arthritis is often underestimated, and experience in treatment among rheumatologists is limited. Three conditions have an affinity toward the TMJ: Rheumatoid arthritis (RA), psoriatic arthritis (PA), and ankylosing spondylitis (AS). The prevalence is the highest in RA, followed by PA (1–5).
The disease processes differ from those seen in osteoarthritis or following trauma, which are characterized by degeneration or ankylosis, respectively, as joint destruction occurs. Furthermore, inflammatory arthropathies are systemic diseases that can lead to a relapse in symptoms, despite initially successful treatment, as TMJ inflammation continues. Immunosuppressive therapies used to ameliorate systemic inflammation may also complicate treatment responses, particularly if surgical management is required, as there is a theoretical increased risk of infection. In contrast, osteoarthritis symptoms may stabilize, previous joint trauma tends not to deteriorate unless TMJ ankylosis ensues, and immunosuppression is not required. Therefore, a different management approach is required in patients with inflammatory arthropathy that addresses both the systemic illness and localized TMJ disease.
Pain, reduced mouth opening, joint noises, locking, and difficulty eating are the predominant symptoms and can be debilitating if left untreated. Pain originates from the TMJ itself, the associated masticatory muscles, or from both these areas, and it is manifested by tenderness on palpation of the respective anatomical area. Mouth opening is measured as the gap between the tips of the upper and lower incisors at maximal opening (interincisal distance) with less than 35 mm considered abnormal (6). Joint noises and locking result from the internal derangement of the joint mechanism, which consists of the mandibular condyle, intra-articular disc, and glenoid fossa, or from inflammatory debris deposited as part of the disease process. Combined with pain and restricted opening, these contribute toward problems in eating.
Management should be based on symptomatology, and medical therapy alone is often sufficient. Also, despite a diagnosis of inflammatory arthropathy, many patients have simple mechanical problems of the TMJ that usually can be treated by non-surgical regimes. The purpose of this review is to outline further treatments available when disease progression occurs in spite of pharmacological intervention, with a focus on minimally invasive and surgical management of the joint. The aim is to offer a practical guide for physicians rather than provide an exhaustive review of the medical management of the TMJ and the surgical procedures on offer.
Rheumatoid arthritis of the temporomandibular joint
As a synovial joint, patients with RA are at risk of TMJ involvement, and 67–71% patients will have at least one symptom; however, the true prevalence depends on the population studied, diagnostic criteria, and means of TMJ assessment (1, 2, 7). The likelihood of TMJ involvement correlates with the severity and duration of the systemic disease as tenderness in multiple peripheral joints is often accompanied by a painful TMJ (2, 8, 9). Typical clinical findings include joint pain, stiffness, sounds, and limitation of movement (2, 8). TMJ pain and masticatory muscle tenderness suggest an active disease (1).
Rheumatoid arthritis patients tend to have more frequent and severe symptoms, signs, and radiographic changes when compared with PA and AS (1, 7, 10). Crepitus, in particular, is considered to be an important sign of joint destruction (1, 7). Typical radiographic changes include cortical erosions, subcortical cysts, flattening of the condylar head and articular eminence, subcortical sclerosis, and narrowing of the joint space, but none of these are pathognomonic of RA (8, 10, 11).
Difficulty in mouth opening is common in RA due to pain, fibrous adhesions, anterior disc displacement, muscle contracture, inflammation, or more severe degeneration of the TMJ. However, when measured objectively, there is no statistically significant difference between the mouth opening of patients with RA and the general population, so this finding in itself does not yield a definitive diagnosis (1).
Ankylosis is a late and rare finding; in some cases, it affects both sides (12, 13). In severe cases, there is a loss of mandibular condylar support with resultant retrognathia, loss of posterior mandibular height, and anterior open bite (failure of the incisors to meet), which, at its worst, can cause intermittent airway obstruction, particularly when supine (1, 14). In one study, 66% patients with RA of the TMJ had severe arthritis of the cervical spine, and 50% with RA affecting the cervical spine had severe arthritis of the TMJ (15).
Psoriatic arthropathy of the temporomandibular joint
Traditionally, TMJ involvement in PA has been thought to be rare with fewer than 40 cases reported in the last 50 years. However, some studies have suggested that dysfunction occurs in 90% patients with PA (4, 5). More recently, Dervis and Dervis (3) found the TMJ to be symptomatic in 29% and 35% of patients with psoriasis and PA, respectively. This incidence is no higher than that found in the general population without psoriasis (TMJ dysfunction occurs in approximately one-third); therefore, PA does not necessarily increase the risk of TMJ dysfunction. However, when it occurs, the symptoms tend to be worse. PA can also affect the TMJ in the form of monoarthritis, rather than polyarthritis in 0.01–0.2% of the population (16).
The duration and severity of PA and the number of somatic joints affected are the main risk factors for TMJ symptoms and signs, but the degree of skin involvement is not (3, 4). Typical findings include clicking, crepitus, or other joint sounds; TMJ pain on mouth opening and chewing; morning stiffness; and muscle tenderness (3, 4, 17). As the disease progresses, pain is replaced by the limitation of movement due to the development of fibrosis. Like RA, crepitus is found in the latter stages and is associated with structural joint changes, which may progress to joint collapse or ankylosis.
Lundberg and Ericsson (18) first described the radiographic appearance of a TMJ affected by PA, and the most common manifestation is condylar head erosion secondary to osteolysis of the subchondral bone. Osteoporotic lesions are less frequently seen radiographically, while osteophyte formation, joint space narrowing, condylar head flattening, and subchondral sclerosis have also been reported (16, 17, 19). Although there is a strong correlation between TMJ symptom development and condylar erosions in PA, this and the other radiographic findings are not specific; therefore, they cannot be differentiated from other arthritic conditions or degeneration (16, 17). Furthermore, radiographic features often lag behind symptoms; therefore, a normal radiograph does not exclude PA and sometimes, the opposite is true as advanced radiographic changes can be asymptomatic (17).
Ankylosing spondylitis of the temporomandibular joint
Temporomandibular joint involvement occurs in 22% patients with AS, but its symptoms are not specific and most patients have no pain, so this is likely to be an underestimate (20). The most frequent clinical features are TMJ sounds, tenderness of the masticatory musculature (particularly, the lateral pterygoid muscles), hypertrophy of the masseters, and limitation of movement manifested as restricted mouth opening. These symptoms and signs are seen less often and are not as severe as those encountered in RA and PA (7). There have been 12 case reports of TMJ ankylosis in patients with AS, 5 of which were bilateral (21).
Management
Medical therapy
The first aim of management is to relieve pain, initially using conservative measures, which will resolve symptoms in over 80% patients (22). These include reassurance; jaw rest with a soft diet; avoidance of wide mouth opening; physiotherapy; non-steroidal anti-inflammatory drugs (NSAIDs), which can be prescribed topically; and soft occlusal splints made by the dentist (23). Effective management of the disease activity with disease-modifying antirheumatic drugs (DMARDs) and biologics appropriate to the underlying disease is vital.
Although there is no evidence of long-term benefits using physiotherapy, it is not harmful and can be used in the short-term management of the restriction of opening after an exacerbation of the condition, arthroscopy, or open surgery. Topical NSAIDs applied to the joint and masticatory musculature may produce the same benefits as oral preparations, but with fewer side effects in superficial joints, and they should be used 4 times a day for 4 weeks (22–24). Although data from these trials relate to NSAID use in osteoarthritis in clinical practice, they also have been used as a basis to treat inflammatory arthropathies affecting the TMJ. Low-dose tricyclic antidepressants are beneficial for myofascial pain related to the TMJ, but evidence of their use has been extrapolated from studies that employed these drugs for chronic pain elsewhere in the body (25).
Disease-modifying antirheumatic drugs (including biologics) can attenuate joint damage by suppressing inflammation in all of the inflammatory arthritides discussed, and the aim of the rheumatologist should be to achieve remission if possible (1, 26–30). The benefit of these therapies is that the TMJ is treated simultaneously with other joints as the systemic pathophysiology of the disease is targeted. The full extent of their application is beyond the scope of this review and is well reported elsewhere.
Bite splints, which are worn at night, permit masticatory muscle rest, reduce myofascial pain, and reduce the load on the TMJ, particularly in patients with a tendency for clenching or grinding their teeth. Cochrane analysis has shown that no type of bite splint delivers a better outcome, so an inexpensive, simple, lower occlusal soft splint made by the dentist is sufficient (31).
Local anesthetic and steroid injections
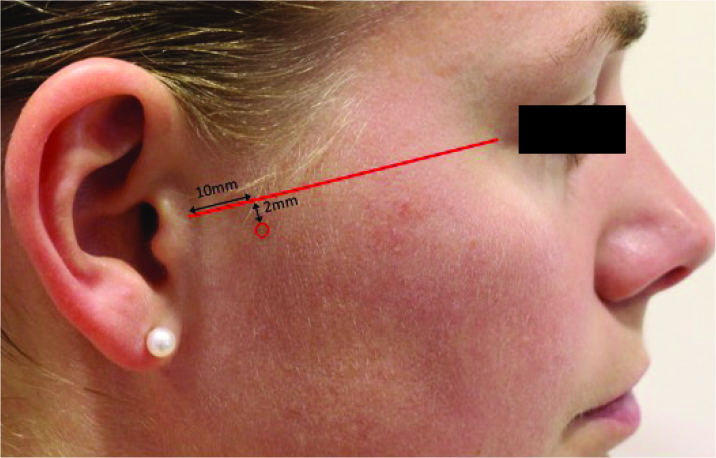
Pain emanating from the TMJ can be confirmed, and temporarily relieved, by infiltration of local anesthetic (lignocaine 1% or 2%) into the joint space. Resolution of the pain after 10 min establishes an intra-articular etiology rather than a muscular source. The site of injection is 10 mm along and 2 mm inferior to a straight line from the tragus to the lateral canthus of the eye (Figure 1).
Figure 1.
Anatomical location of the TMJ joint space for the injection of local anesthetic or steroid (red circle)
TMJ: temporomandibular joint
Intra-articular steroid injections can modulate TMJ synovitis. The senior author does not recommend this routinely unless there is proven joint inflammation on the magnetic resonance imaging (MRI) scan or during arthroscopy, as indiscriminate use may cause irreversible joint loss from thinning of the cartilage, which seems to be particularly susceptible to the effects of steroids in this region.
Myofascial pain and spasm can be temporarily relieved with the injection of a long-acting local anesthetic, such as bupivacaine 0.5% or botulinum toxin, into the masseter and temporalis muscles. The latter causes localized muscle paralysis for up to 6 months and reduces pain measured using a visual analog scale by at least 25% in 79% patients (32).
Arthroscopy and arthrocentesis
Where infiltration of the joint with local anesthetic relieves pain, TMJ arthroscopy with arthrocentesis, which was first described by Ohnishi in 1975, is indicated as a diagnostic and therapeutic aid in patients recalcitrant to medical treatment (33). Arthroscopy will elucidate any particular pathology and saline lavage of the joint under pressure, flushes out debris, and breaks down adhesions that prevent normal movement (34). Blunt release of adhesions, which can anchor the intra-articular disc, termed the “‘anchored disc phenomenon,” is also possible using arthroscopy.
The procedure is minimally invasive, well-tolerated, low cost, and can be carried out in a day-case environment (even under local anesthetic). There is marginal risk of causing long-term joint damage leading to degenerative change, but only the upper joint space can be entirely accessed. However, restricted mouth opening is usually secondary to upper joint space problems, particularly the anchored disc phenomenon and synovitis, where arthrocentesis is the most beneficial (22, 35). Three-dimensional computerized tomography (CT) supplements the assessment of the entire joint surface, and MRI will reveal an effusion or synovial inflammation, but neither can accurately demonstrate the disc pathology; this is only possible with arthroscopy.
The lower joint space tends to be affected by degenerative diseases, but access to managing these conditions requires an open operative procedure. Arthroscopy is difficult, if not impossible, in ankylosing conditions because the joint space cannot be accessed due to joint fusion of the ankylotic mass.
Fewer than 10% patients presenting to a TMJ clinic progress to arthroscopy and arthrocentesis, but symptoms settle in 70–86% of this subgroup when these techniques are used, while 10% require subsequent open joint surgery (22, 36, 37). A Cochrane review found that both arthroscopy and arthrocentesis reduced pain, but arthroscopy exhibited greater improvement in mouth opening after 12 months (38). In inflammatory arthritis, it is useful to combine the two techniques as arthroscopy aids diagnosis and treatment planning, while arthrocentesis allows debris to be flushed from the joint space.
Outcomes following the procedure seem less favorable in patients with an inflammatory arthritic disease affecting the TMJ, but there have been no definitive studies with sufficient numbers. Simple repeated arthrocentesis in a functional joint is often sufficient to keep the patient comfortable, with judicious use of intra-articular steroid as indicated by arthroscopically diagnosed synovitis.
Open joint surgery
Prior to the widespread use of arthroscopy and arthrocentesis, the management of TMJ problems unresponsive to simple treatments was done using open surgery. Synovectomy is a high-risk procedure due to the close proximity of the medial joint capsule to the trigeminal nerve branches, terminal carotid vessels, and internal jugular vein, which complicates complete synovial removal. In a series of patients from over 20 years ago, it was found that it successfully treated pain and restricted opening in patients with RA, PA, and AS affecting the TMJ, but was normally combined with discectomy that probably accounted for the majority of symptomatic relief (39–41).
The use of eminoplasty, eminectomy, disc plication, discectomy, and adhesiolysis via a preauricular incision made to approach the joint can directly address intra-articular pathology. Whilst successful in their own right, they are more likely to lead to iatrogenic degenerative changes, and hence, should be a second-line choice. These techniques have been reported to improve pain and mouth opening in a small series, but should not be tried before arthroscopy and arthrocentesis, particularly in previously unoperated joints (42–44).
More severe cases with very high initial pain scores and very restricted opening or joint collapse have a poorer prognosis from open joint surgery as they are likely to require total joint replacement (45). Ultimately, total joint replacement may be required, but repeated open operations prior to this end should be avoided as the risks of surgery are increased and arthroplasty outcomes are compromised. As such the number of surgical interventions should be minimized and preferably provided by an oral and maxillofacial surgeon specializing in the TMJ.
Total temporomandibular joint replacement surgery
When symptoms return despite conservative and minimally invasive treatments, the final common pathway for all destructive, degenerative, and ankylotic TMJ disease is total joint replacement. It was developed during the 19th century, with current prostheses modified from those produced in the 1960s by Christensen. The initial Christensen joint replacement was a metal-on-acrylic prosthesis that was changed to a metal-on-metal one due to wear observed after 10–15 years. The subsequent metal-on-metal cobalt-chrome alloy has been withdrawn from the market because of the risk of early wear that has complicated metal replacements in other joints. In addition, approximately 10% patients developed a foreign-body reaction possibly due to material allergy (46).
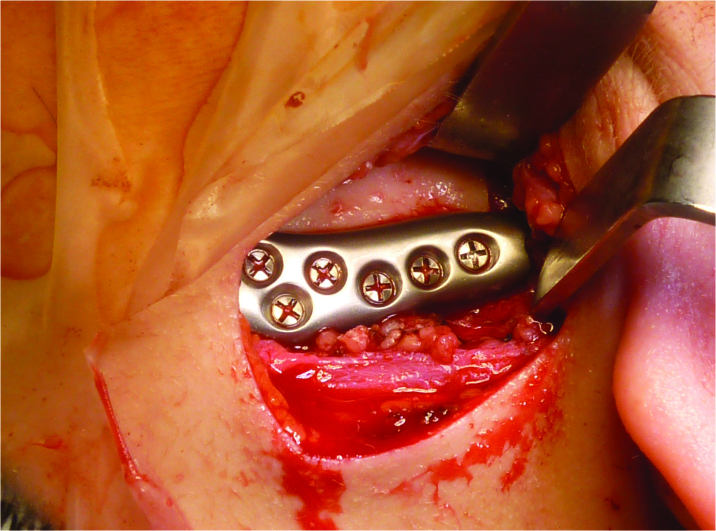
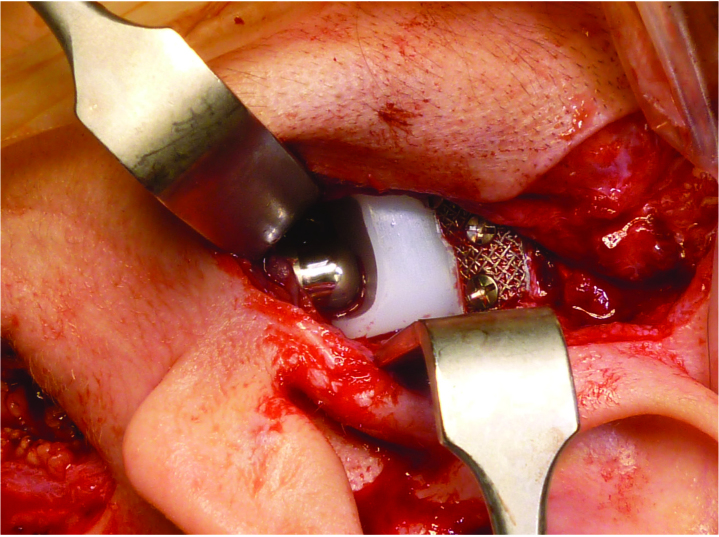
Currently, there are two systems with 20-year follow-up that are in widespread use (47, 48). The first is the TMJ Concepts (TMJ Concepts; Ventura, CA, USA) patient-fitted total TMJ replacement, which is custom-made for each patient using a computer-aided design and manufacture (CAD-CAM) model of the joint constructed from a three-dimensional CT scan. The diseased joint surfaces are resected and the replacement fixed to the mandibular ramus and the skull base with screws (Figure 2, 3). The prosthesis is made from a high-molecular-weight polyethylene and cobalt-chrome alloy, which is comparable to that used for total knee replacements, and costs are similar when hospital stay (2 days, postoperatively) is also considered. Hardened titanium may be used instead for the condylar component head in patients with an allergy to the cobalt-chromium alloy.
Figure 2.
TMJ Concepts (Ventura, CA, USA) custom-fitting total joint replacement in situ, showing the mandibular ramus component
Figure 3.
TMJ Concepts (Ventura, CA, USA) custom-fitting total joint replacement in situ, showing the condylar head articulating with the new prosthetic glenoid fossa
The second system is the Biomet (Biomet; Jacksonville, FL, USA) microfixation TMJ replacement, which is a stock prosthesis that the surgeon has to “fit” to the patient’s anatomy at implantation. Patient-fitted variants can also be constructed similar to the TMJ Concepts system.
Three outcome measures are routinely recorded to determine if TMJ replacement has been successful: pain and dietary function, which are gauged using a visual analog scale, and mouth opening measured in millimeters between the upper and lower incisors. Increasingly, quality of life measures are also being recorded. In a recent series of 84 patients reviewed for 3–5 years after replacement, there were significant improvements in pain and dietary function (by 90%) and mouth opening improved by 42–69% (49). Revision surgery was carried out in 2 patients due to prosthesis infection. Longer-term follow-up shows that these outcomes are maintained in 90% of patients aged up to 17 years (50).
Most patients undergoing replacement have degenerative or post-traumatic disease, but comparably significant improvements in pain, dietary function, and mouth opening have been demonstrated in those with inflammatory arthritis (51, 52). However, outcomes will be less satisfactory in these patients if multiple operations on the joint have been performed due to repeated trauma. Therefore, it is important they are referred early in the disease’s progression to an appropriately trained surgeon to determine if a lesser procedure is appropriate or whether this will compromise the outcome of joint replacement.
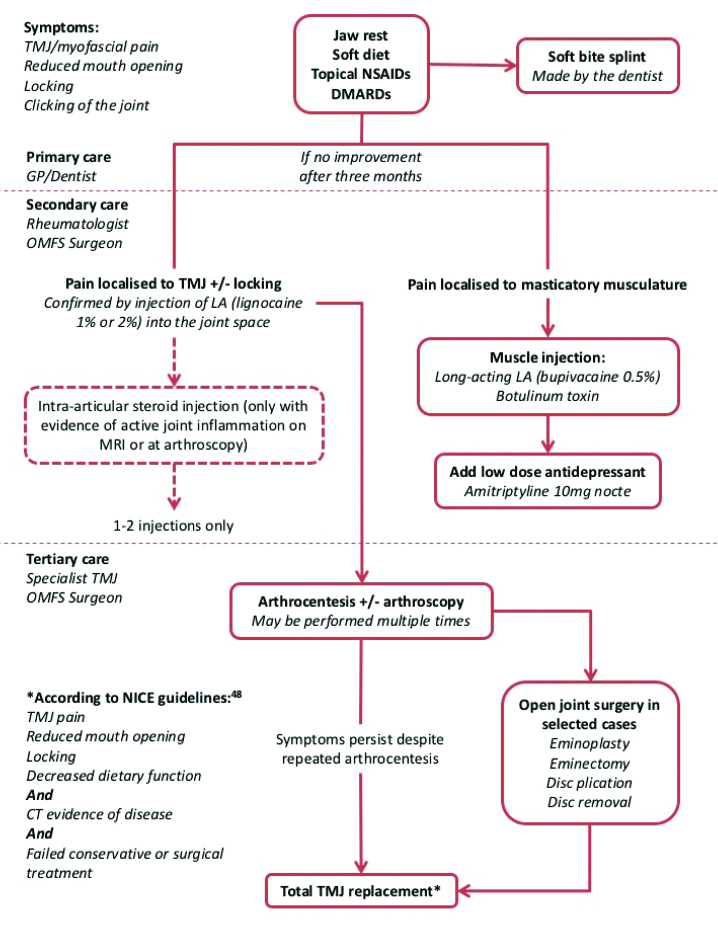
Guidelines for replacement are somewhat stricter than for other joints, but have been approved by the National Institute for Health and Care Excellence (NICE) (6, 53). Given that 100 joints are replaced each year in the UK, only surgeons with a subspecialist interest in the TMJ should undertake the procedure. Our management algorithm emphasizes when a referral is appropriate and highlights the optimal use of non-surgical and minimally invasive treatments (Figure 4).
Figure 4.
Treatment algorithm for patients with inflammatory arthritis affecting the TMJ
OMFS: oral and maxillofacial surgery; TMJ: temporomandibular joint
Conclusion
Inflammatory arthritis of the TMJ is uncommon, but it is debilitating when severe functional restriction occurs. Early advice and management from an oral and maxillofacial surgeon, particularly if symptoms have been confirmed to emanate from the joint, can help slow the progression to joint collapse or ankylosis, which causes malocclusion of the teeth. Even a late-stage disease can be suitably managed with open joint surgeries or total joint replacement to maintain a good quality of life.
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: N/A.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.J.S., F.F.; Design - A.J.S., R.O.C., R.S.; Supervision - A.J.S., F.F.; Data Collection and/or Processing - R.O.C., R.S., A.J.S.; Analysis and/or Interpretation - R.O.C., R.S.; Literature Search - R.O.C., R.S.; Writing Manuscript - R.O.C., R.S.; Critical Review - A.J.S., F.F.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Aliko A, Ciancaglini R, Alushi A, Tafaj A, Ruci D. Temporomandibular joint involvement in rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis. Int J Oral Maxillofac Surg. 2011;40:704–9. doi: 10.1016/j.ijom.2011.02.026. https://doi.org/10.1016/j.ijom.2011.02.026. [DOI] [PubMed] [Google Scholar]
- 2.Bessa-Nogueira RV, Vasconcelos BC, Duarte AP, Góes PS, Bezerra TP. Targeted assessment of the temporomandibular joint in patients with rheumatoid arthritis. J Oral Maxillofac Surg. 2008;66:1804–11. doi: 10.1016/j.joms.2007.08.037. https://doi.org/10.1016/j.joms.2007.08.037. [DOI] [PubMed] [Google Scholar]
- 3.Dervis E, Dervis E. The prevalence of temporomandibular disorders in patients with psoriasis with or without psoriatic arthritis. J Oral Rehabil. 2005;32:786–93. doi: 10.1111/j.1365-2842.2005.01521.x. https://doi.org/10.1111/j.1365-2842.2005.01521.x. [DOI] [PubMed] [Google Scholar]
- 4.Könönen M. Subjective symptoms from the stomatognathic system in patients with psoriatic arthritis. Acta Odontol Scand. 1986;44:377–83. doi: 10.3109/00016358609094348. https://doi.org/10.3109/00016358609094348. [DOI] [PubMed] [Google Scholar]
- 5.Könönen M. Clinical signs of craniomandibular disorders patients with psoriatic arthritis. Scand J Dent Res. 1987;95:340–6. doi: 10.1111/j.1600-0722.1987.tb01851.x. https://doi.org/10.1111/j.1600-0722.1987.tb01851.x. [DOI] [PubMed] [Google Scholar]
- 6.Sidebottom AJ. Guidelines for the replacement of temporomandibular joints in the United Kingdom. Br J O Maxillofac Surg. 2008;46:146–7. doi: 10.1016/j.bjoms.2006.12.001. https://doi.org/10.1016/j.bjoms.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Könönen M, Wenneberg B, Kallenberg A. Craniomandibular disorders in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. A clinical study. Acta Odontol Scand. 1992;50:281–7. doi: 10.3109/00016359209012774. https://doi.org/10.3109/00016359209012774. [DOI] [PubMed] [Google Scholar]
- 8.Celiker R, Gökçe-Kutsal Y, Eryilmaz M. Temporomandibular joint involvement in rheumatoid arthritis. Relationship with disease activity. Scand J Rheumatol. 1995;24:22–5. doi: 10.3109/03009749509095149. https://doi.org/10.3109/03009749509095149. [DOI] [PubMed] [Google Scholar]
- 9.Koh ET, Yap AU, Koh CK, Chee TS, Chan SP, Boudville IC. Temporomandibular disorders in rheumatoid arthritis. J Rheumatol. 1999;26:1918–22. [PubMed] [Google Scholar]
- 10.Wenneberg B, Kononen M, Kallenberg A. Radiographic changes in the temporomandibular joint of patients with rheumatoid arthritis, psoriatic, arthritis, and ankylosing spondylitis. J Craniomandib Disord. 1990;4:35–9. [PubMed] [Google Scholar]
- 11.Ardic F, Gokharman D, Atsu S, Guner S, Yilmaz M, Yorgancioglu R. The comprehensive evaluation of temporomandibular disorders seen in rheumatoid arthritis. Aust Dent J. 2006;51:23–8. doi: 10.1111/j.1834-7819.2006.tb00396.x. https://doi.org/10.1111/j.1834-7819.2006.tb00396.x. [DOI] [PubMed] [Google Scholar]
- 12.Kobayashi R, Utsunomiya T, Yamamoto H, Nagura H. Ankylosis of the temporomandibular joint caused by rheumatoid arthritis: a pathological study and review. J Oral Sci. 2001;43:97–101. doi: 10.2334/josnusd.43.97. https://doi.org/10.2334/josnusd.43.97. [DOI] [PubMed] [Google Scholar]
- 13.Lurie R, Fisher JT, Lownie JF. Temporomandibular joint ankylosis in rheumatoid arthritis. A case report. S Afr Med J. 1988;73:57–8. [PubMed] [Google Scholar]
- 14.Redlund-Johnell I. Upper airway obstruction in patients with rheumatoid arthritis and temporomandibular joint destruction. Scand J Rheumatol. 1988;17:273–9. doi: 10.3109/03009748809098796. https://doi.org/10.3109/03009748809098796. [DOI] [PubMed] [Google Scholar]
- 15.Redlund-Johnell I. Severe rheumatoid arthritis of the temporomandibular joints and its coincidence with severe rheumatoid arthritis of the cervical spine. Scand J Rheumatol. 1987;16:347–53. doi: 10.3109/03009748709102506. https://doi.org/10.3109/03009748709102506. [DOI] [PubMed] [Google Scholar]
- 16.Koorbusch GF, Zeitler DL, Fotos PG, Doss JB. Psoriatic arthritis of the temporomandibular joints with ankylosis. Literature review and case reports. Oral Surg Oral Med Oral Pathol. 1991;71:267–74. doi: 10.1016/0030-4220(91)90297-p. https://doi.org/10.1016/0030-4220(91)90297-P. [DOI] [PubMed] [Google Scholar]
- 17.Könönen M. Craniomandibular disorders in psoriasis. Community Dent Oral Epidemiol. 1987;15:108–12. doi: 10.1111/j.1600-0528.1987.tb00494.x. https://doi.org/10.1111/j.1600-0528.1987.tb00494.x. [DOI] [PubMed] [Google Scholar]
- 18.Lundberg M, Ericson S. Changes in the temporomandibular joint in psoriasis arthropathica. Acta Derm Venereol. 1967;47:354–8. [PubMed] [Google Scholar]
- 19.Miles DA, Kaugars GA. Psoriatic involvement of the temporomandibular joint. Literature review and report of two cases. Oral Surg Oral Med Oral Pathol. 1991;71:770–4. doi: 10.1016/0030-4220(91)90290-s. https://doi.org/10.1016/0030-4220(91)90290-S. [DOI] [PubMed] [Google Scholar]
- 20.Locher MC, Felder M, Sailer HF. Involvement of the temporomandibular joints in ankylosing spondylitis (Bechterew's disease) J Craniomaxillofac Surg. 1996;24:205–13. doi: 10.1016/s1010-5182(96)80003-5. https://doi.org/10.1016/S1010-5182(96)80003-5. [DOI] [PubMed] [Google Scholar]
- 21.Manemi RV, Fasanmade A, Revington PJ. Bilateral ankylosis of the jaw treated with total alloplastic replacement using the TMJ concepts system in a patient with ankylosing spondylitis. Br J Oral Maxillofac Surg. 2009;47:159–61. doi: 10.1016/j.bjoms.2008.08.020. https://doi.org/10.1016/j.bjoms.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 22.Sidebottom AJ. Current thinking in temporomandibular joint management. Br J Oral Maxillofac Surg. 2009;47:91–4. doi: 10.1016/j.bjoms.2008.08.012. https://doi.org/10.1016/j.bjoms.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 23.Moore RA, Tramer MR, Carroll D, Wiffen PJ, McQuay HJ. Quantitative systematic review of topically applied non-steroidal anti-inflammatory drugs. BMJ. 1998;316:333–8. doi: 10.1136/bmj.316.7128.333. https://doi.org/10.1136/bmj.316.7128.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin J, Zhang W, Jones A, Doherty M. Efficacy of topical non-steroidal anti-inflammatory drugs in the treatment of osteoarthritis: meta-analysis of randomised controlled trials. BMJ. 2004;329:324. doi: 10.1136/bmj.38159.639028.7C. https://doi.org/10.1136/bmj.38159.639028.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cascos-Romero J, Vazquez-Delgado E, Vazquez- Rodriguez E, Gay-Escoda C. The use of tricyclic antidepressants in the treatment of temporomandibular joint disorders: systematic review of the literature of the last 20 years. Med Oral, Patol Oral Cir Bucal. 2009;14:E3–7. [PubMed] [Google Scholar]
- 26.Bruce IN, Gladman DD. Psoriatic arthritis: recognition and management. BioDrugs. 1998;9:271–8. doi: 10.2165/00063030-199809040-00002. https://doi.org/10.2165/00063030-199809040-00002. [DOI] [PubMed] [Google Scholar]
- 27.Nell VP, Machold KP, Eberl G, Stamm TA, Uffmann M, Smolen JS. Benefit of very early referral and very early therapy with disease-modifying anti-rheumatic drugs in patients with early rheumatoid arthritis. Rheumatology (Oxford) 2004;43:906–14. doi: 10.1093/rheumatology/keh199. https://doi.org/10.1093/rheumatology/keh199. [DOI] [PubMed] [Google Scholar]
- 28.Sokka T, Mäkinen H. Drug management of early rheumatoid arthritis - 2008. Best Pract Res Clin Rheumatol. 2009;23:93–102. doi: 10.1016/j.berh.2008.08.003. https://doi.org/10.1016/j.berh.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Saad AA, Symmons DP, Noyce PR, Ashcroft DM. Risks and benefits of tumor necrosis factor-alpha inhibitors in the management of psoriatic arthritis: systematic review and metaanalysis of randomized controlled trials. J Rheumatol. 2008;35:883–90. [PubMed] [Google Scholar]
- 30.Callhoff J, Sieper J, Weiss A, Zink A, Listing J. Efficacy of TNFα blockers in patients with ankylosing spondylitis and non-radiographic axial spondyloarthritis: a meta-analysis. Ann Rheum Dis. 2015;74:1241–8. doi: 10.1136/annrheumdis-2014-205322. https://doi.org/10.1136/annrheumdis-2014-205322. [DOI] [PubMed] [Google Scholar]
- 31.Al-Ani MZ, Davies SJ, Gray RJ, Sloan P, Glenny AM. Stabilisation splint therapy for temporomandibular pain dysfunction syndrome. The Cochrane Database of Systematic Reviews. 2004:Cd002778. doi: 10.1002/14651858.CD002778.pub2. https://doi.org/10.1002/14651858.cd002778.pub2. [DOI] [PubMed] [Google Scholar]
- 32.Sidebottom AJ, Patel AA, Amin J. Botulinum injection for the management of myofascial pain in the masticatory muscles. A prospective outcome study. Br J Oral Maxillofac Surg. 2013;51:199–205. doi: 10.1016/j.bjoms.2012.07.002. https://doi.org/10.1016/j.bjoms.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 33.Onishi M. Arthroscopy of the temporomandibular joint. The Journal of the Stomatological Society. 1975;42:207–13. https://doi.org/10.5357/koubyou.42.207. [PubMed] [Google Scholar]
- 34.Guo C, Shi Z, Revington P. Arthrocentesis and lavage for treating temporomandibular joint disorders. The Cochrane database of systematic reviews. 2015:CD004973. doi: 10.1002/14651858.CD004973.pub2. https://doi.org/10.1002/14651858.cd004973.pub3. [DOI] [PubMed] [Google Scholar]
- 35.Nitzan DW, Dolwick MF, Heft MW. Arthroscopic lavage and lysis of the temporomandibular joint: a change in perspective. J Oral Maxillofac Surg. 1990;48:798–801. doi: 10.1016/0278-2391(90)90335-y. discussion 802. https://doi.org/10.1016/0278-2391(90)90335-Y. [DOI] [PubMed] [Google Scholar]
- 36.Ahmed N, Sidebottom A, O’Connor M, Kerr HL. Prospective outcome assessment of the therapeutic benefits of arthroscopy and arthrocentesis of the temporomandibular joint. Br J Oral Maxillofac Surg. 2012;50:745–8. doi: 10.1016/j.bjoms.2012.01.004. https://doi.org/10.1016/j.bjoms.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 37.Brennan PA, Ilankovan V. Arthrocentesis for temporomandibular joint pain dysfunction syndrome. J Oral Maxillofac Surg. 2006;64:949–51. doi: 10.1016/j.joms.2006.02.010. https://doi.org/10.1016/j.joms.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 38.Rigon M, Pereira LM, Bortoluzzi MC, Loguercio AD, Ramos AL, Cardoso JR. Arthroscopy for temporomandibular disorders. The Cochrane database of systematic reviews. 2011:CD006385. doi: 10.1002/14651858.CD006385.pub2. https://doi.org/10.1002/14651858.cd006385.pub2. [DOI] [PubMed] [Google Scholar]
- 39.Bjørnland T, Larheim TA. Synovectomy and diskectomy of the temporomandibular joint in patients with chronic arthritic disease compared with diskectomies in patients with internal derangement. A 3-year follow-up study. Eur J Oral Sci. 1995;103:2–7. doi: 10.1111/j.1600-0722.1995.tb00002.x. https://doi.org/10.1111/j.1600-0722.1995.tb00002.x. [DOI] [PubMed] [Google Scholar]
- 40.Bjørnland T, Larheim TA, Haanaes HR. Surgical treatment of temporomandibular joints in patients with chronic arthritic disease: preoperative findings and one-year follow-up. Cranio. 1992;10:205–10. doi: 10.1080/08869634.1992.11677911. https://doi.org/10.1080/08869634.1992.11677911. [DOI] [PubMed] [Google Scholar]
- 41.Haanaes HR, Larheim TA, Nickerson JW, Pahle JA. Discectomy and synovectomy of the temporomandibular joint in the treatment of rheumatoid arthritis: case report with three-year follow-up study. J Oral Maxillofac Surg. 1986;44:905–10. doi: 10.1016/0278-2391(86)90231-4. https://doi.org/10.1016/0278-2391(86)90231-4. [DOI] [PubMed] [Google Scholar]
- 42.Miloro M, Henriksen B. Discectomy as the primary surgical option for internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 2010;68:782–9. doi: 10.1016/j.joms.2009.09.091. https://doi.org/10.1016/j.joms.2009.09.091. [DOI] [PubMed] [Google Scholar]
- 43.Vasconcelos BC, Porto GG, Bessa-Nogueira RV. Condylar disk plication for temporomandibular joint internal derangement treatment: surgical technique and results. Med Oral Patol Oral Cir Bucal. 2005;10(Suppl 2):E133–8. [PubMed] [Google Scholar]
- 44.Nyberg J, Adell R, Svensson B. Temporomandibular joint discectomy for treatment of unilateral internal derangements--a 5 year follow-up evaluation. Int J Oral Maxillofac Surg. 2004;33:8–12. doi: 10.1054/ijom.2002.0453. https://doi.org/10.1054/ijom.2002.0453. [DOI] [PubMed] [Google Scholar]
- 45.Tzanidakis K, Sidebottom AJ. Outcomes of open temporomandibular joint surgery following failure to improve after arthroscopy: is there an algorithm for success? Br J Oral Maxillofac Surg. 2013;51:818–21. doi: 10.1016/j.bjoms.2013.04.013. https://doi.org/10.1016/j.bjoms.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 46.Sidebottom AJ, Speculand B, Hensher R. Foreign body response around total prosthetic metal-on-metal replacements of the temporomandibular joint in the UK. Br J Oral Maxillofac Surg. 2008;46:288–92. doi: 10.1016/j.bjoms.2007.12.003. https://doi.org/10.1016/j.bjoms.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 47.Wolford LM, Mercuri LG, Schneiderman ED, Movahed R, Allen W. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg. 2015;73:952–60. doi: 10.1016/j.joms.2014.10.032. https://doi.org/10.1016/j.joms.2014.10.032. [DOI] [PubMed] [Google Scholar]
- 48.Mercuri LG. Alloplastic temporomandibular joint replacement: rationale for the use of custom devices. Int J Oral Maxillofac Surg. 2012;41:1033–40. doi: 10.1016/j.ijom.2012.05.032. https://doi.org/10.1016/j.ijom.2012.05.032. [DOI] [PubMed] [Google Scholar]
- 49.Gruber EA, McCullough J, Sidebottom AJ. Medium-term outcomes and complications after total replacement of the temporomandibular joint. Prospective outcome analysis after 3 and 5 years. Br J Oral Maxillofac Surg. 2015;53:412–5. doi: 10.1016/j.bjoms.2014.12.010. https://doi.org/10.1016/j.bjoms.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 50.Mercuri LG, Edibam NR, Giobbie-Hurder A. Fourteen-year follow-up of a patient-fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg. 2007;65:1140–8. doi: 10.1016/j.joms.2006.10.006. https://doi.org/10.1016/j.joms.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 51.Saeed NR, McLeod NM, Hensher R. Temporomandibular joint replacement in rheumatoid-induced disease. Br J Oral Maxillofac Surg. 2001;39:71–5. doi: 10.1054/bjom.2000.0565. https://doi.org/10.1054/bjom.2000.0565. [DOI] [PubMed] [Google Scholar]
- 52.O’Connor RC, Saleem S, Sidebottom AJ. Prospective outcome analysis of total replacement of the temporomandibular joint with the TMJ Concepts system in patients with inflammatory arthritic diseases. Br J Oral Maxillofac Surg. 2016;54:604–9. doi: 10.1016/j.bjoms.2016.03.005. https://doi.org/10.1016/j.bjoms.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 53.Total prosthetic replacement of the temporomandibular joint. National Institute of Clinical Excellence; 2014. [Google Scholar]