Abstract
The synovium is a specialized tissue lining the synovial joints, bursae, and tendon sheaths of the body. It is affected by various localized or systemic disorders. Synovial diseases can be classified as inflammatory, infectious, degenerative, traumatic, hemorrhagic, and neoplastic. Damage in other intraarticular structures, particularly cartilages, generally occurs as a part of pathologic processes involving the synovium, leading to irreversible joint destruction. Imaging has an essential role in the early detection of synovial diseases prior to irreversible joint damage. Obtaining and understanding characteristic imaging findings of synovial diseases enables a proper diagnosis for early treatment. This article focuses on the recent literature that is related with the role of imaging in synovial disease.
Keywords: Synovium, synovial hypertrophy, synovitis, magnetic resonance imaging
Introduction
The synovium is a thin specialized membrane lining the diarthrodial joint surfaces, bursae, and tendon sheaths. Synovium coats the inner surface of the fibrous joint capsule, fat pads, and intraarticular ligaments. Other intraarticular structures such as the articular cartilage, menisci, labra, and small bone bare area are not covered by the synovium (1, 2). The synovium provides nutrition and lubrication to the joint cartilage by fluid secretion (3).
Synovial diseases are classified as inflammatory, infectious, degenerative, traumatic, hemorrhagic, and neoplastic. There are also tumor-like conditions such as pigmented villonodular synovitis, nodular synovitis, giant cell tumor of tendon sheath, synovial chondromatosis/osteochondromatosis, and lipoma arborescens (1, 3).
Damage in other intraarticular structures, particularly cartilages, generally occurs as a consequence of pathologic processes involving the synovium, leading to irreversible joint destruction (4). Imaging plays a crucial role in the early detection of synovial diseases prior to the occurrence of irreversible joint damage. Plain radiography, ultrasonography (US), and magnetic resonance imaging (MRI) are utilized in the diagnosis and follow-up of synovial diseases. Gadolinium-enhanced MRI is the best tool to diagnose synovial disorders (1, 3).
MRI findings of synovial diseases include thickening of the synovium, hyperintensity on T2-weighted images (T2WI) due to water accumulation, and prominent contrast enhancement on postcontrast T1-weighted images (T1WI). Because of the high soft-tissue contrast resolution of MRI, besides synovitis diagnosis, joint effusion, articular cartilage, subchondral bone, ligaments, muscles, and juxtaarticular soft tissues can be evaluated (5). Herein, each of these synovial diseases were explained in detail.
Rheumatoid arthritis
Rheumatoid arthritis (RA) is a joint-based chronic, progressively destructive inflammatory systemic disease. Synovial hypertrophy occurs initially, and locally invasive behavior causes cartilage destruction and bone erosions. RA proceeds progressively, ultimately causing multiple deformities. All synovial joints can be affected; however, metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints are the most frequently involved ones. Bilateral and symmetric involvement is a rule and atlantoaxial joint particularly involved in the spine (6, 7). RA also has extraarticular musculoskeletal manifestations such as rheumatoid nodules, enthesopathy, bursitis, tenosynovitis, and tendon rupture.
Radiographs show typical findings such as soft-tissue swelling, marginal erosions, periarticular osteopenia, joint space narrowing, and joint subluxation. Besides bone alterations, this imaging modality is unable to display synovitis at an early stage. Identification of early changes facilitate the prevention of joint damage via more effective therapies, promoting the importance of advanced imaging methods (3, 8).
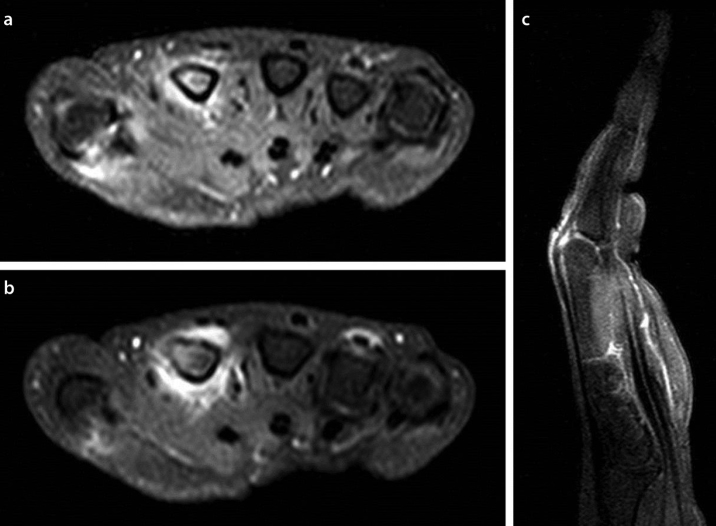
US and MRI can detect synovial proliferation, tenosynovitis, and bone erosions. Fat saturated T2WI and postcontrast fat saturated T1WI are useful for the evaluation of synovitis (Figure 1a), tenosynovitis (Figure 1 a–c), and adjacent soft tissues. Also, postcontrast fat saturated T1WI is essential to distinguish synovial proliferation from joint effusion (Figure 1a, b). Bone marrow edema and erosions are detected on MRI at the same time (6, 8). Dynamic MRI determinates active disease by demonstrating a synovial enhancement pattern (9). Pannus is defined as persistent synovitis, hypervascular synovial tissue, and destruction of cartilage and bone. This lesion is responsible for the irreversible joint destruction due to locally invasive properties. Pannus has similar MRI findings to synovitis with associated bone and cartilage disruption (10).
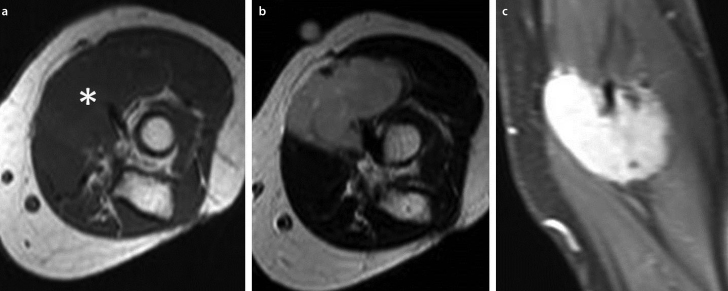
Figure 1.a–c.
60 year old woman with RA; axial post-contrast fat-saturated T1W consecutive images (a, b) and sagittal image (c) of the right hand revealed contrast enhancement, indicating synovial hypertrophy of the second metacarpophalangeal (MCP) joint and tenosynovitis of flexor pollicis longus and extensor tendons of the third and fourth finger (from the courtesy of Dr. A. Turan)
Psoriatic arthritis
Psoriatic arthritis (PsA) is one of the seronegative spondyloarthropathy-spectrum diseases related with psoriasis. The prevalence is approximately 30% in psoriatic cases, and there is no gender predilection (11, 12).
Joint damage appears at the early stages of the disease; thus, the detection and treatment of joint inflammation is crucial. Clinical findings alone are generally insufficient to determinate the severity of the disorder. High-resolution US and MRI provide an accurate and early assessment of synovial inflammation. Imaging is also used to differentiate PsA from other arthropathies such as RA. Hand and feet finger joints are most commonly affected, but sacroiliac joints, spine, knees, elbows, ankles, and shoulders can be involved. Sausage digit is a form of dactylitis that is described as a swelling of the whole finger in PsA (11, 13).
On radiography images, the best diagnostic clue for PsA is the simultaneous presence of eccentric erosive changes and new bone formation at the same joints. PsA particularly affects the distal interphalangeal (DIP) joints. Periostitis, pencil-in-cup deformities, joint space narrowing, ankylosis, osteolysis, a rthritis mutilans, and ivory phalanx are the other radiographic manifestations of PsA. Axial skeletal involvement presents with syndesmophyte formation, sacroiliitis, atlantoaxial subluxation, apophysial joint ankylosis, and ligament calcification. DIP involvement and the asymmetric pattern without periarticular osteoporosis are the factors that differentiate PsA from RA. However, RA primarily affects MCP with osteoporosis, and bone proliferation is not a feature of RA (11, 14).
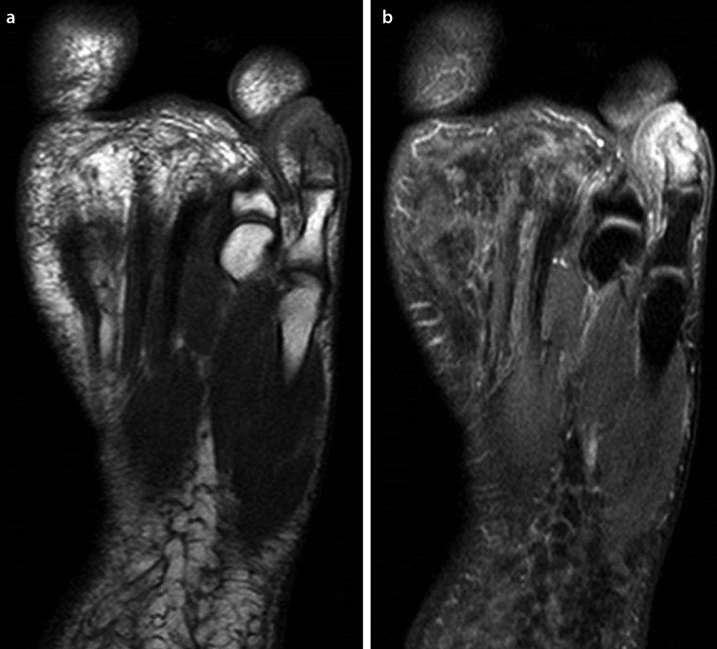
MRI is very sensitive to inflammatory and destructive changes in PsA. MRI allows the detection of synovitis, osteitis, erosions (Figure 2a, b), effusions, enthesitis, tenosynovitis, and dactylitis in addition to the involvement of axial skeleton and sacroiliitis. This method also determines disease activity and response to the treatment (11).
Figure 2.a, b.
28-year-old man with psoriasis; axial T1W (a) and proton-density SPAIR images (b) show bone erosion of the distal phalanges, inflammatory changes in adjacent soft tissues, and synovitis in the distal interphalangeal (DIP) joint of the fifth toe (from the courtesy of Dr. A. Turan)
Gout arthropathy
Gout is a disease that is characterized with deposition of monosodium urate (MSU) crystals in soft tissues and joints secondary to hyperuricemia. The deposition of MSU crystals activate the inflammatory process and cause gout tophi formation. Gout tophi are foreign body granulomas that include macrophages and MSU crystals. Arthropathy develops secondary to the inflammatory reaction. Chronic arthropathy develops after several years of recurring acute arthritis attacks. Thus, chronic gout arthritis generally affects older patients. The first MTP joints and knees are the most frequently affected joints. The diagnosis is generally straightforward and based on clinical, laboratory, and radiological evaluation. Sometimes, biopsy may be required (12, 15).
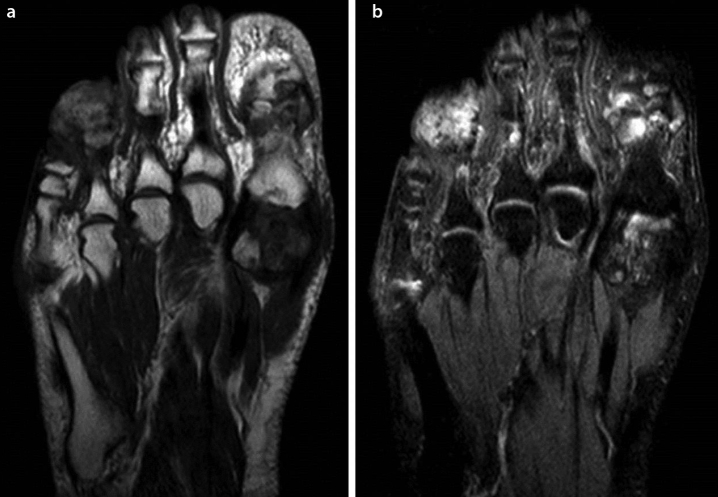
Radiographic findings include dense nodular soft tissue masses, well-defined bony erosions, and bony proliferation (12).
MRI findings are quite non-specific. Gout tophi frequently mimic other conditions such as tumor or infection (16) (Figure 3a, b). Dual-energy computed tomography (DECT) is a new technology that provides a non-invasive determination of MSU crystal deposits. DECT differentiates MSU crystals from calcium via specific attenuation characteristics. This technology is not only useful for diagnosis but also useful in monitoring of the disease (15, 17). Therefore, DECT is the test of choice in patients with suspected gouty arthritis.
Figure 3.a, b.
57-year-old man with gouty arthritis; axial T1W (a) and proton-density SPAIR (b) images reveal tophi formation and bone erosions with accompanying bone marrow edema in the fourth proximal interphalangeal, first metatarsophalangeal, and interphalangeal joints with adjacent soft tissue involvement (from the courtesy of Dr. A. Turan)
Juvenile idiopathic arthritis
Juvenile idiopathic arthritis (JIA) is one of the most common manifestations of rheumatic disease with an unknown etiology in the pediatric group. This entity is composed of all cases of IA that occur before the age of 16 years and persist for at least 6 weeks. The knee is the most commonly affected joint (1).
The International League of Associations for Rheumatology classifies JIA into seven subgroups, which are listed below (18);
- Systemic arthritis: 10–20% of JIA cases are characterized with polyarticular involvement and may be associated with rash, hepatosplenomegaly, adenopathy, fever, myalgias, and serositis.
- Oligoarthritis: The most common subgroup in which 1–4 joints are affected in the first 6 months from the onset of the disease.
- Rheumatoid factor (RF)-negative polyarthritis: RF-negative patients with at least ≥5 joints affected.
- RF-positive polyarthritis: RF-positive patients with at least ≥5, similar to the adult form of RA.
- Psoriatic arthritis: Patients with arthritis and psoriasis or arthritis accompanied by ≥2 of the following: dactylitis, nail pitting, onycholysis, rash, or positive family history. Generally, the knee, ankle, DIP, and PIP joints of the hands and feet are affected.
- Enthesitis-related arthritis: Arthritis and enthesitis or arthritis or enthesitis accompanied by ≥2 of the following: inflammatory lower back pain; sacroiliac joint tenderness; positive HLA-B27 antigen; male over 6 years of age at onset; acute anterior uveitis; or positive family history of enthesitis-related arthritis, sacroilitis with inflammatory bowel disease, or Reiter syndrome.
- Undifferentiated arthritis: Remaining patients that fit into none or at least two subgroups.
Radiographic findings include bone erosions, joint space narrowing due to cartilage destruction, and growth retardation. Although radiography can demonstrate chronic irreversible joint damage, it is unable to display cartilage destruction. Cases should be identified during the preradiographic period to administer appropriate treatment. MRI is an effective imaging modality for this task (1, 18).
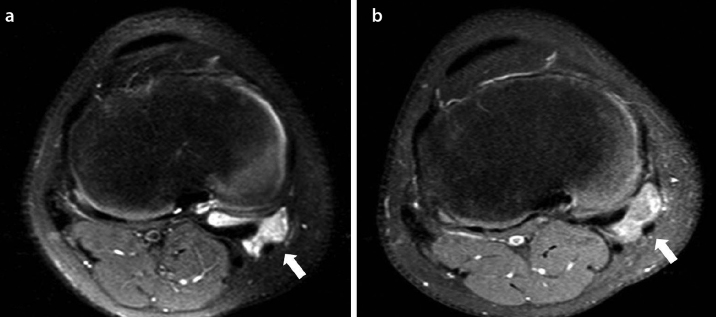
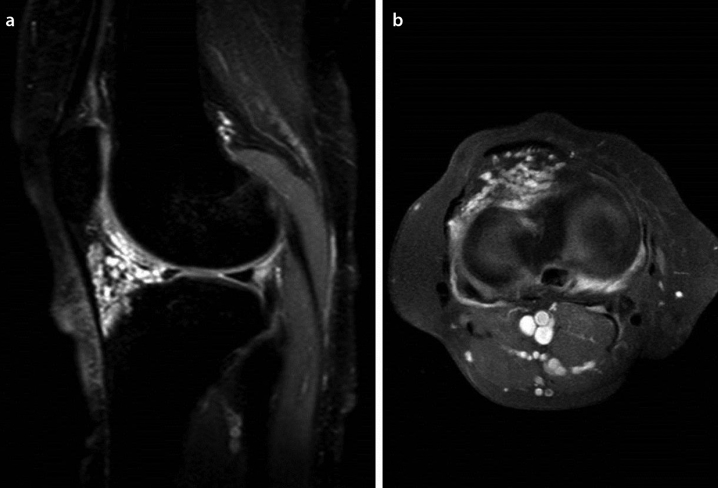
On MRI, the most common finding is synovitis that appears hypointense on T1WI, hyperintense on T2WI, and marked enhancement following intravenous (IV) contrast administration (Figure 4a, b, 5a, b). In some cases, the meniscus may be smaller in size because of synovial hypertrophy. Also, some additional findings are joint effusion, Baker cyst, lymphadenopathy in the popliteal fossa, extraarticular tenosynovitis, and rice bodies (Figure 4a) (18).
Figure 4.a, b.
15-year-old boy with oligoarticular juvenile idiopathic arthritis (JIA) who had knee pain for 1 year; proton-density SPAIR image (a) depicts Rice bodies inside Baker’s cyst (arrow). Post-contrast fat-saturated T1WI (b) displays enhancing of synovial proliferation (arrow) (from the courtesy of Dr. A. Turan)
Pigmented villonodular synovitis
Pigmented villonodular synovitis (PVNS) is a form of villonodular proliferation of synovium with hemosiderin pigment deposition. This entity may develop in the bursa and tendon sheaths as well and named as pigmented villonodular bursitis (PVNB) and pigmented villonodular tenosynovitis (PVNTS), respectively. PVNS is considered to be a benign neoplasm, but rare cases of a malignant transformation of PVNS is reported (19, 20).
The most common type of intraarticular PVNS is the diffuse form, but a localized form of PVNS may rarely be encountered. The clinical and radiological findings of these two forms are different (19).
Diffuse PVNS is most commonly presented with pain, swelling, and restriction of movement. The lesion generally affects the knee. Other joints such as the hip, ankle, shoulder, and elbow are rarely involved (19, 20).
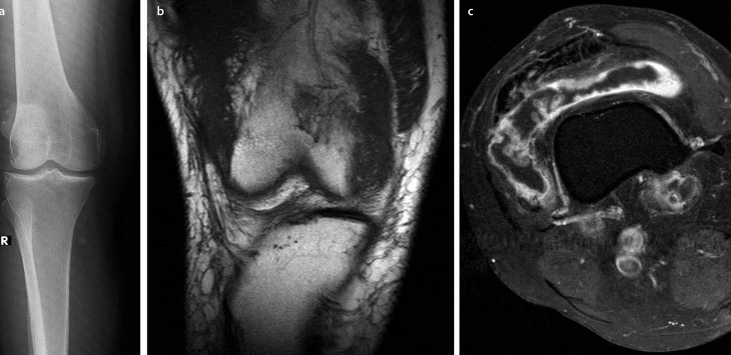
Radiographs are non-specific for diagnosis and can reveal soft-tissue swelling without calcification with preserved joint space (Figure 6a). Cartilage disruption and degenerative arthritis develops at the chronic stage (20).
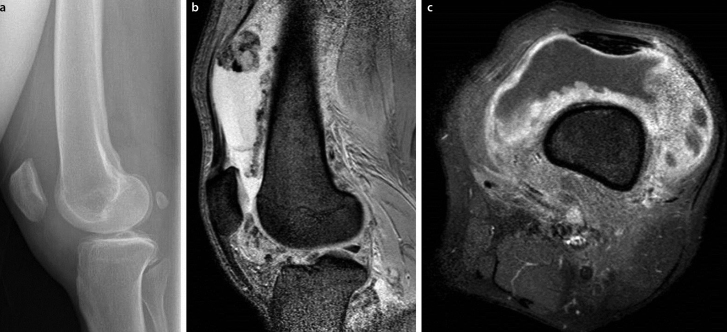
Figure 6.a–c.
25-year-old woman with diffuse pigmented villonodular synovitis (PVNS) of the knee; lateral radiograph (a) shows soft tissue swelling in the left knee. Sagittal GRE image (b) reveals an extensive suprapatellar effusion and diffuse synovial thickening with hypointense blooming artifacts. Axial post-contrast fat-saturated T1WI(c) displays enhancing villonodular synovial fronds (from the courtesy of Dr. A. Turan)
US findings of PVNS are joint effusion and synovial thickening with villous projections. The local form of appearance is different, in which only a nodulary soft tissue lesion is depicted. Doppler US shows hypervascularity of the lesions (20).
MRI reveals prominent diffuse villous or nodular proliferation of synovium and associated joint effusion. Synovial thickening is visualized as an intermediate to low signal intensity on T1WI. There are low signal intensity areas due to the hemosiderin on T2WI. Particularly, hemosiderin appears as blooming artifacts on gradient echo (GRE) images because of its magnetic susceptibility, which is is almost pathognomonic in all forms of PVNS (Figure 6b). Lesions show evident contrast enhancement after IV gadolinium administration (20, 21) (Figure 6c).
Surgical resection is the preferred treatment option, but recurrence rates are high.
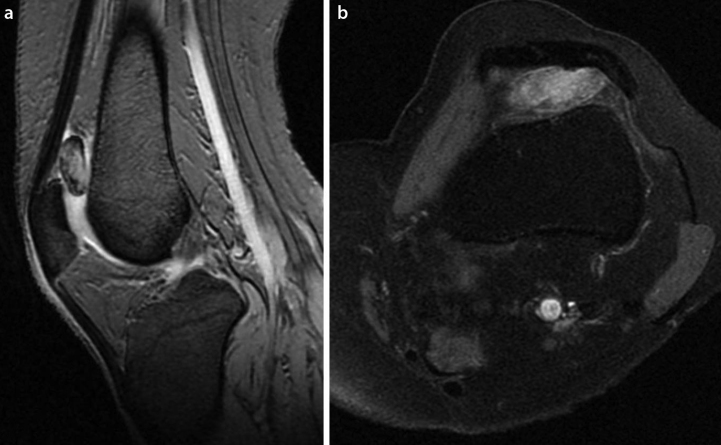
The localized form of PVNS commonly affects the knee, particularly the infrapatellar region, and also affects the suprapatellar and posterior intercondylar area at times. Generally, radiographs are negative, but soft-tissue opacity is occasionally observed. US reveals only a nodulary soft tissue lesion. On MRI, it is a well-defined nodulary lesion including hemosiderin pigments, and postcontrast images displays the contrast enhancement (22) (Figure 7a, b).
Figure 7.a, b.
29-year-old man with localized intraarticular PVNS; sagittal GRE image(a) shows a nodular lesion with millimetric blooming artifacts of hemosiderin in suprapatellar bursa. Axial post-contrast fat-saturated T1WI (b) displays a marked enhancement of the lesion (from the courtesy of Dr. A. Turan)
Giant cell tumor of the tendon sheath
Giant cell tumors of the tendon sheath (GCTTs) are known as a tumoral lesion; however, it is a benign proliferative lesion of synovium such as PVNS and PVNB.
Giant cell tumors of the tendon sheaths commonly occur in the hand and are the second most common soft tissue tumor of the hand after ganglion cyst. Women are frequently affected, and patients generally present with a slowly growing, painless mass (23, 24).
Radiography shows a soft tissue mass with adjacent bone erosion. US detects a well-defined lesion with a different echo texture, related to tendon sheath. GCTTs are hypervascular on Doppler US (23).
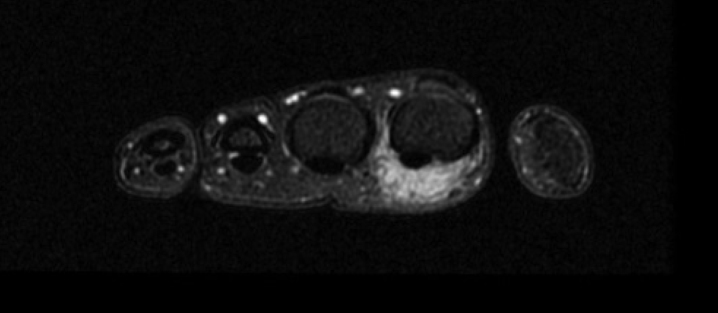
MRI depicts a well-defined tumor related to the tendon. Characteristically, the lesion contains hemosiderin pigments that cause a low to intermediate signal intensity on T1WI and T2WI. Moreover, on GRE images, the magnetic susceptibility of hemosiderin leads to the formation of blooming artifacts because of low signal intensity. After the contrast injection, the lesions show prominent enhancement (Figure 8). Additionally, MRI depicts the relationship of the tumor with soft tissues and joint space (23).
Figure 8.
40-year-old woman with a giant cell tumor of the tendon sheath in the volar aspect of the second finger of left hand; axial post-contrast fat-saturated T1WI shows an enhancing lesion that nearly surrounds the flexor tendon (from the courtesy of Dr. A. Turan)
The differential diagnosis of GCTTs include the other soft tissue tumors and tumor-like lesions such as ganglion cyst, hemangioma, nerve sheath tumor, foreign body granuloma, synovial sarcoma, desmoids, and fibromatosis (23).
Although GCTTs are considered to be a benign lesion, the recurrence rate is high (23).
Synovial chondromatosis/osteochondromatosis
Synovial chondromatosis/osteochondromatosis (SC/O) is a rare monoarticular benign neoplasm. This entity is characterized with chondroid metaplasia in the synovium, resulting in the formation of chondral-osseous bodies in the intraarticular space. SC/O commonly affects joints with a predilection to the knee. Also, the involvement of bursas and tendons were reported. SC/O is frequent in the third to fifth decades, and the etiology is unknown. The clinical findings include pain, swelling, and restriction of motion. Chondral-osseous bodies that are supplied by the synovial fluid may enlarge with time. The method of treatment is surgical resection; however, incomplete resection may result in recurrence. The local recurrence rate is approximately 25% following treatment (25, 26).
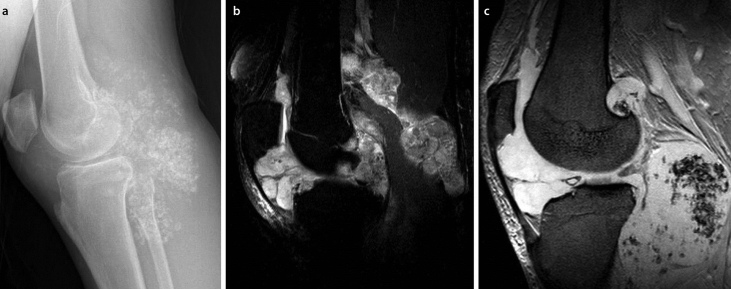
The radiographical appearance of SC/O is frequently pathognomonic. Typically, multiple chondral-osseous bodies that are similar in shape and size fill the joint space entirely. Moreover, these bodies may show a ring-and-arc pattern secondary to peripheral calcification or rarely form a conglomerate, mineralized mass form (Figure 9a). At the same time, joint effusion, osteopenia, and bone erosion can be present (25).
Figure 9.a–c.
53-year-old man with synovial osteochondromatosis of the knee; lateral radiograph (a) shows intraarticular calcification with a ring-and-arc shape appearance. Sagittal proton-density SPAIR image (b) displays hyperintense intraarticular osteochondral bodies. On GRE image (c), some of these bodies contain hypointense areas that indicate calcification (from the courtesy of Dr. A. Turan)
US reveals a heterogeneous mass with hyperechogenic foci, which resembles chondroid bodies. Osseous bodies show posterior acoustic shadowing. The Doppler sonographic appearance of SC/O is hypovascular. CT is the best diagnostic modality for the visualization of osseous bodies (25).
MRI appearance depends on the calcification. Only 30% of patients have unmineralized chondroid bodies. These appear iso-hypointense on T1WI and hyperintense on T2WI. Osseous bodies present as hypointense on both T1WI and T2WI (Figure 9b). GRE images reveal calcifications as a marked hypointensity due to the magnetic susceptibility effects (Figure 9c). In some cases, osseous bodies may contain fatty marrow and appear hyperintense on T1WI and T2WI (25).
Synovial sarcoma
Synovial sarcoma (SS) is the fourth most common type of soft tissue sarcomas. Both genders are equally affected. SS is frequently seen in young adults. The clinical findings are non-specific and generally presents with pain and a slowly growing tumor. Frequently, most tumors are larger than 5 cm at the time of diagnosis. However, superficial tumors can be detected when they are smaller in size, and they show smooth contours with a homogenous structure, mimicking benign lesions. The local recurrence and distant metastasis rate is very high. A tumor size larger than 5 cm is considered as a poor prognostic factor. SS may contain intratumoral calcification and necrosis. The most common location is lower extremities, specifically popliteal fossa. SS can be occasionally present in the intraarticular region (27, 28).
On the radiography images, there are generally specific findings. Soft tissue masses that contain calcification should suggest SS (3, 27).
US reveals a hypoechoic soft tissue mass. CT shows a soft tissue mass that contains necrosis, hemorrhagic areas, and punctate or peripheral calcifications (27).
MRI is the best imaging modality to characterize the lesion and its relationship with the adjacent structures. Generally, the mass is localized close to the bones and appears well-defined and shows low signal intensity on T1WI (Figure 10a). On T2WI, a prominently heterogeneous mass that contains hypointense calcifications or fibrosis, isointense solid component, and hyperintense (Figure 10b) hemorrhagic or necrosis areas are observed. These three different intensity findings compose the triple sign. Moreover, fluid-fluid levels secondary to hemorrhagic areas and adjacent bone or soft tissue invasion can be seen. Dynamic gadolinium-enhanced MRI shows an arterial phase enhancement as a result of the malignant features. Also, postcontrast images provide a distinction from cysts and hematomas by showing the enhancing solid compenent (3, 27) (Figure 10c).
Figure 10.a–c.
49-year-old man with synovial sarcoma of antecubital fossa; Axial T1WI (a) shows isointense soft tissue tumor adjacent to the muscle (asterisk). Axial T2WI (b) reveals a hyperintense mass. Coronal post-contrast fat-saturated T1WI (c) displays a marked enhancement of the lesion (from the courtesy of Dr. A. Turan)
Standardized uptake values (SUV) higher than 4.4 on the positron emission tomography (PET CT) is an evidence of higher cellularity, mitotic rate, and poor prognosis (27).
Following the lungs, the lymph nodes, liver, and brain are the other common locations for metastasis. A long-term follow-up is required because 50% of deaths occur within 5–10 years after diagnosis. Both early and late metastases are more frequent than any other sarcomas (27).
Surgical resection combined with radiotherapy and chemotherapy is an effective treatment methods. Imaging is useful in follow-up and assessing the response to the treatment (27).
Hemophilic arthropathy
Hemophilia is an X-linked autosomal recessively inherited disease; however, approximately one-third of all cases are associated with spontaneous mutations. The prevalence of the disease is 1 in 10,000 males. The level of clotting factors determines the severity of the bleeding. The most common sites of hemorrhage are joints, particularly the knees, ankles, and elbows. Hemorrhage may occur spontaneously or as a result of trauma. Recurrent hemarthrosis causes hemosiderin deposition and synovial hypertrophy, which results in cartilage destruction and degenerative changes in the bones, ligaments, and joint capsules. The early detection of disease has a critical importance because the replacement of deficient factors prevents hemorrhage (29, 30).
Radiography only shows the late bone alterations such as osteopenia, overgrowth of the epiphysis, erosions, squaring of the patella, widening of the intercondylar notch, subchondral cysts, and joint space narrowing and contracture (29).
US easily detects joint effusions and synovitis, whereas cartilage damage could not be recognized. Hemarthrosis can appear in different echogenicities according to the age of bleeding (1, 3, 29).
MRI not only detects the early soft tissue findings but also evaluates the bone changes and cartilage damage. T1WI reveals structural bone deformity, and fat-saturated T2WI displays bone marrow edema. Intraarticular hemosiderin appears as blooming artifacts on GRE images (1, 3, 29) (Figure 11). The use of a contrast agent for the demonstration of synovitis is not recommended because the deposition of hemosiderin restricts the visualization of the enhancement (29).
Figure 11.
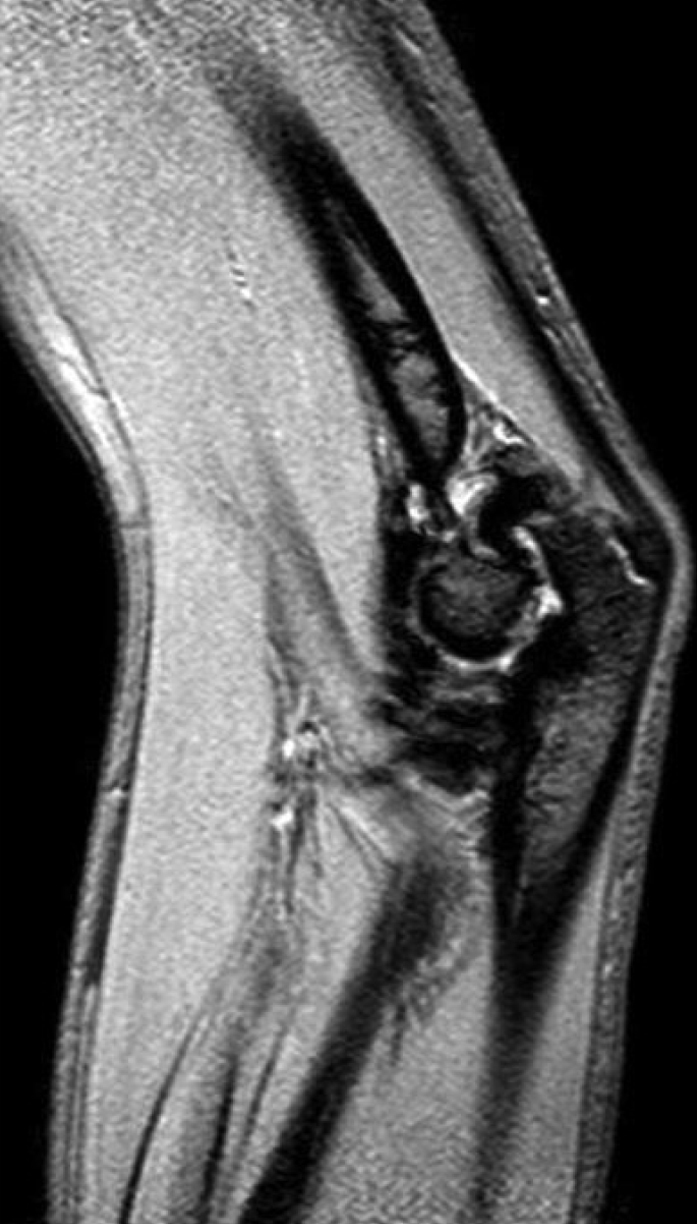
15-year-old boy with hemophilic arthropathy; sagittal GRE image of the left elbow displays blooming artifacts of hemosiderin deposition within the joint and slight joint effusion with synovitis (from the courtesy of Dr. A. Turan)
Synovial vascular malformation
Vascular malformations (VMs) are classified as capillary, venous, arterial, lymphatic, or mixed form. VMs involving the synovium are present at birth and grow slowly. Synovial VMs are generally encountered in children and young adults presenting with pain and swelling. The knee is the most commonly affected joint. In addition, the elbows, wrists, and ankles can be affected as well (16, 31).
Radiography shows nonspecific soft tissue swelling accompanied by phlebolithis and osteoporosis. US reveals a heterogeneous lesion containing vascular channels (31).
MRI is the most useful modality in which synovial VMs appear hypointense on T1WI and hyperintense on T2WI (Figure 12a). High-flow vessels within the lesion are seen as flow void tubular structures on T2WI. The contrast enhancement pattern differs according to the type of vascular content of the malformation. For instance, although the venous component shows homogenous intense enhancement (Figure 12b), lymphatic areas have a cystic nature, tending to enhance peripherally (31).
Figure 12.a, b.
29-year-old man with synovial venous malformation; sagittal proton-density SPAIR image (a) demonstrates a hyperintense tubular structured lesion in Hoffa fat pad. Axial post-contrast fat-saturated T1WI (b) displays a contrast enhancement of the lesion (from the courtesy of Dr. A. Turan)
Lipoma arborescens
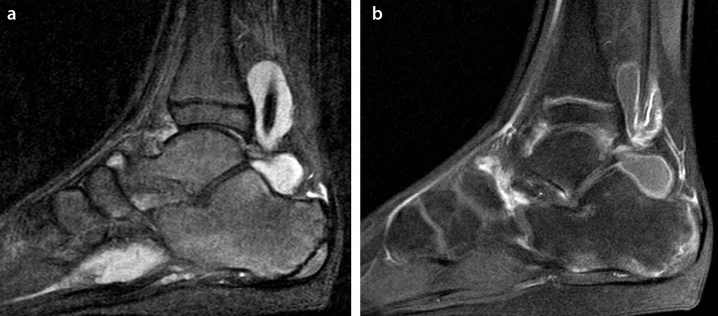
Lipoma arborescens (LA) is a rare, idiopathic, intra/extraarticular disorder. LA can affect any joint, with knee joints being the most common. Villous lipomatous proliferation of the synovium is typical (3, 32).
Radiography is generally nonspecific with degenerative alterations (Figure 13a). MRI exhibits a synovial proliferation and frond-like fatty content, which is similar to subcutaneous fat on all sequences and shows a suppression on fat-saturated images (1, 3) (Figure 13b, c).
Figure 13.a–c.
55-year-old woman with lipoma arborescens of the knee; radiography (a) demonstrates degenerative osteoarthritis of the right knee. Coronal T1WI (b) reveals frond-like fatty content, and axial post-contrast fat-saturated T1WI (c) displays enhancing synovial proliferation (from the courtesy of Dr. A. Turan)
Reactive synovitis
Synovitis has primary or secondary causes. The term for secondary causes of synovitis is reactive synovitis (RS). RS develops as result of joint pathology such as trauma, foreign body, bone infarction, osteochondrondritis dissecans, and bone tumor of the epiphysis, i.e., juxtaarticular osteoid osteoma. Imaging findings include primary lesions with concomitant synovitis and joint effusion (1) (Figure 14a, b).
Figure 14.a, b.
9-year-old girl with reactive synovitis secondary to trauma; coronal precontrast T1WI (a) shows slight hyperintense hemorrhagic effusion in the suprapatellar bursa, and coronal post-contrast fat-saturated T1WI (b) demonstrates enhancing synovitis
Conclusion
Synovitis is one of the most common clinical scenarios in daily practice of rheumatologists with diverse differential diagnosis. Although a clinical assessment is generally adequate for diagnosis, US and gadolinium-enhanced MRI are helpful imaging modalities for the diagnosis and follow-up of synovial diseases. Radiography and DECT can contribute as well in some particular diseases. Definitive diagnosis by imaging alone is generally not possible, except in some specific conditions. However, imaging modalities provide information on synovial proliferation and accompanying findings that guides the clinician in differential diagnosis.
Figure 5.a, b.
12-year-old boy with familial Mediterranean fever and accompanying oligoarticular JIA of the right ankle. Sagittal proton-density SPAIR image (a) shows joint and tenosynovial effusion. Sagittal post-contrast fat-saturated T1WI (b) displays enhancing of synovial proliferation (from the courtesy of Dr. A. Turan)
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.T.; Design - A.T., P.Ç.; Supervision - A.T.; Materials - A.T.; Data Collection and/or Processing - A.T., P.Ç.; Analysis and/or Interpretation - A.T.; Literature Review -A.T.; Writer - A.T., P.Ç.; Critical Review - A.T., M.A.Ö.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Kim HK, Zbojniewicz AM, Merrow AC, Cheon JE, Kim IO, Emery KH. MR findings of synovial disease in children and young adults: Part 1. Pediatr Radiol. 2011;41:495–511. doi: 10.1007/s00247-011-1971-0. https://doi.org/10.1007/s00247-011-1971-0. [DOI] [PubMed] [Google Scholar]
- 2.Cassidy JT, Petty RE. Synovium. In: Cassidy JT, Petty RE, Laxer R, Lindlsy C, editors. Textbook of pediatric rheumatology. 5th edition. Elsevier Sanders; Philadelphia: 2005. p. 13. [Google Scholar]
- 3.Jaganathan S, Goyal A, Gadodia A, Rastogi S, Mittal R, Gamanagatti S. Spectrum of synovial pathologies: a pictorial assay. Curr Probl Diagn Radiol. 2012;41:30–42. doi: 10.1067/j.cpradiol.2011.07.002. https://doi.org/10.1067/j.cpradiol.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Buchmann RF, Jaramillo D. Imaging of articular disorders in children. Radiol Clin North Am. 2004;42:151–68. doi: 10.1016/S0033-8389(03)00159-3. https://doi.org/10.1016/S0033-8389(03)00159-3. [DOI] [PubMed] [Google Scholar]
- 5.McQueen FM. The MRI view of synovitis and tenosynovitis in inflammatory arthritis: implications for diagnosis and management. Ann N Y Acad Sci. 2009;1154:21–34. doi: 10.1111/j.1749-6632.2009.04382.x. https://doi.org/10.1111/j.1749-6632.2009.04382.x. [DOI] [PubMed] [Google Scholar]
- 6.Rowbotham EL, Grainger AJ. Rheumatoid arthritis: ultrasound versus MRI. AJR Am J Roentgenol. 2011;197:541–6. doi: 10.2214/ajr.11.6798. [DOI] [PubMed] [Google Scholar]
- 7.Villeneuve E, Emery P. Rheumatoid arthritis: what has changed? Skeletal Radiol. 2009;38:109–12. doi: 10.1007/s00256-008-0579-4. https://doi.org/10.1007/s00256-008-0579-4. [DOI] [PubMed] [Google Scholar]
- 8.Tan YK, Conaghan PG. Imaging in rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2011;25:569–84. doi: 10.1016/j.berh.2011.10.002. https://doi.org/10.1016/j.berh.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 9.Hodgson RJ, O Connor P, Moots R. MRI of rheumatoid arthritis: dynamic contrast enhanced MRI. Rheumatology. 2008;47:13–21. doi: 10.1093/rheumatology/kem250. https://doi.org/10.1093/rheumatology/kem250. [DOI] [PubMed] [Google Scholar]
- 10.Xanthopoulos E, Hutchinson CE, Adams JE, Bruce IN, Nash AF, Holmes AP, et al. Improved wrist pannus volume measurement from contrast-enhanced MRI in rheumatoid arthritis using shuffle transform. Magn Reson Imaging. 2007;25:110–6. doi: 10.1016/j.mri.2006.10.018. https://doi.org/10.1016/j.mri.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 11.Anandarajah A. Imaging in psoriatic arthritis. Clin Rev Allergy Immunol. 2013;44:157–65. doi: 10.1007/s12016-012-8304-4. https://doi.org/10.1007/s12016-012-8304-4. [DOI] [PubMed] [Google Scholar]
- 12.O’Connor PJ. Crystal deposition disease and psoriatic arthritis. Semin Musculoskelet Radiol. 2013;17:74–9. doi: 10.1055/s-0033-1333940. https://doi.org/10.1055/s-0033-1333940. [DOI] [PubMed] [Google Scholar]
- 13.Wassenberg S, Fischer-Kahle V, Herborn G, Rau R. A method to score radiographic change in psoriatic arthritis. Z Rheumatol. 2001;60:156–66. doi: 10.1007/s003930170064. https://doi.org/10.1007/s003930170064. [DOI] [PubMed] [Google Scholar]
- 14.Ory PA, Gladman DD, Mease PJ. Psoriatic arthritis and imaging. Ann Rheum Dis. 2005;64(Suppl II):ii55–ii7. doi: 10.1136/ard.2004.033928. https://doi.org/10.1136/ard.2004.033928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desai MA, Peterson JJ, Garner HW, Kransdorf MJ. Clinical utility of dual-energy CT for evaluation of tophaceous gout. Radiographics. 2011;31:1365–75. doi: 10.1148/rg.315115510. https://doi.org/10.1148/rg.315115510. [DOI] [PubMed] [Google Scholar]
- 16.Kim HK, Zbojniewicz AM, Merrow AC, Cheon JE, Kim IO, Emery KH. MR findings of synovial disease in children and young adults: Part 2. Pediatr Radiol. 2011;41:512–24. doi: 10.1007/s00247-011-2007-5. https://doi.org/10.1007/s00247-011-1971-0. [DOI] [PubMed] [Google Scholar]
- 17.Dalbeth N, Choi HK. Dual-energy computed tomography for gout diagnosis and management. Curr Rheumatol Rep. 2013;15:301. doi: 10.1007/s11926-012-0301-3. https://doi.org/10.1007/s11926-012-0301-3. [DOI] [PubMed] [Google Scholar]
- 18.Sheybani EF, Khanna G, White AJ, Demertzis JL. Imaging of juvenile idiopathic arthritis: a multimodality approach. Radiographics. 2013;33:1253–73. doi: 10.1148/rg.335125178. https://doi.org/10.1148/rg.335125178. [DOI] [PubMed] [Google Scholar]
- 19.Ottaviani S, Ayral X, Dougados M, Gossec L. Pigmented villonodular synovitis: a retrospective single-center study of 122 cases and review of the literature. Semin Arthritis Rheum. 2011;40:539–46. doi: 10.1016/j.semarthrit.2010.07.005. https://doi.org/10.1016/j.semarthrit.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis: radiologic-pathologic correlation. Radiographics. 2008;28:1493–518. doi: 10.1148/rg.285085134. https://doi.org/10.1148/rg.285085134. [DOI] [PubMed] [Google Scholar]
- 21.Huang GS, Lee CH, Chan WP, Chen CY, Yu JS, Resnick D. Localized nodular synovitis of the knee: MR imaging appearance and clinical correlates in 21 patients. AJR Am J Roentgenol. 2003;181:539–43. doi: 10.2214/ajr.181.2.1810539. https://doi.org/10.2214/ajr.181.2.1810539. [DOI] [PubMed] [Google Scholar]
- 22.Cheng XG, You YH, Liu W, Zhao T, Qu H. MRI features of pigmented villonodular synovitis (PVNS) Clin Rheumatol. 2004;23:31–4. doi: 10.1007/s10067-003-0827-x. https://doi.org/10.1007/s10067-003-0827-x. [DOI] [PubMed] [Google Scholar]
- 23.Wan JM, Magarelli N, Peh WC, Guglielmi G, Shek TW. Imaging of giant cell tumour of the tendon sheath. Radiol Med. 2010;115:141–51. doi: 10.1007/s11547-010-0515-2. https://doi.org/10.1007/s11547-010-0515-2. [DOI] [PubMed] [Google Scholar]
- 24.Di Grazia S, Succi G, Fragetta F, Perrotta RE. Giant cell tumor of tendon sheath: study of 64 cases and review of literature. G Chir. 2013;34:149–52. doi: 10.11138/gchir/2013.34.5.149. https://doi.org/10.11138/gchir/2013.34.5.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murphey MD, Vidal JA, Fanburg-Smith JC, Gajewski DA. Imaging of synovial chondromatosis with radiologic-pathologic correlation. Radiographics. 2007;27:1465–88. doi: 10.1148/rg.275075116. https://doi.org/10.1148/rg.275075116. [DOI] [PubMed] [Google Scholar]
- 26.McKenzie G, Raby N, Ritchie D. A pictorial review of primary synovial osteochondromatosis. Eur Radiol. 2008;18:2662–9. doi: 10.1007/s00330-008-1024-8. https://doi.org/10.1007/s00330-008-1024-8. [DOI] [PubMed] [Google Scholar]
- 27.Bakri A, Shinagare AB, Krajewski KM, Howard SA, Jagannathan JP, Hornick JL, et al. Synovial sarcoma: imaging features of common and uncommon primary sites, metastatic patterns, and treatment response. Am J Roentgenol. 2012;199:W208–15. doi: 10.2214/AJR.11.8039. https://doi.org/10.2214/AJR.11.8039. [DOI] [PubMed] [Google Scholar]
- 28.Bixby SD, Hettmer S, Taylor GA, Voss SD. Synovial sarcoma in children: imaging features and common benign mimics. AJR Am J Roentgenol. 2010;195:1026–32. doi: 10.2214/AJR.10.4348. https://doi.org/10.2214/AJR.10.4348. [DOI] [PubMed] [Google Scholar]
- 29.Cross S, Vaidya S, Fotiadis N. Hemophilic arthropathy: a review of imaging and staging. Semin Ultrasound CT MR. 2013;34:516–24. doi: 10.1053/j.sult.2013.05.007. https://doi.org/10.1053/j.sult.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 30.Adams JE, Reding MT. Hemophilic arthropathy of the elbow. Hand Clin. 2011;27:151–63. doi: 10.1016/j.hcl.2011.01.007. https://doi.org/10.1016/j.hcl.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 31.Legiehn GM, Heran MK. Classification, diagnosis, and interventional radiologic management of vascular malformations. Orthop Clin North Am. 2006;37:435–74. doi: 10.1016/j.ocl.2006.04.005. https://doi.org/10.1016/j.ocl.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 32.Xue J, Alario AJ, Nelson SD, Wu H. Progressive bilateral lipoma arborescens of the knee complicated by juvenile spondyloarthropathy: a case report and review of the literature. Semin Arthritis Rheum. 2013;43:259–63. doi: 10.1016/j.semarthrit.2012.12.022. https://doi.org/10.1016/j.semarthrit.2012.12.022. [DOI] [PubMed] [Google Scholar]