Abstract
IMPORTANCE
Office-based opiate agonist therapy has dramatically expanded access to medication-assisted treatment over the past decade but has also led to increased buprenorphine diversion.
OBJECTIVE
Our study sought to characterize physicians who participate in office-based therapy (OBT) to assess patient access to OBT in Ohio 10 years after its introduction.
DESIGN/SETTING/PARTICIPANTS
Cross-sectional telephone survey of Drug Addiction Treatment Act–waivered physicians in Ohio listed by the Center for Substance Abuse Treatment (CSAT).
MAIN OUTCOMES
This study sought to determine what proportion of eligible physicians are actively prescribing buprenorphine, whether they accept insurance for OBT, and whether they accept insurance for non-OBT services. In addition, we evaluated what physician characteristics predicted those primary outcomes. We hypothesized that a significant minority of eligible physicians are not active prescribers of buprenorphine. In addition, we expected that a significant minority of OBT prescribers do not accept insurance, further restricting patient access. We further hypothesized that a large subset of OBT prescribers accept insurance in their regular practices but do not take insurance for OBT.
RESULTS
Of the 466 listed physicians, 327 (70.2%) practice representatives were reached for interview. Thirty-three physicians were excluded, with a true response rate of 75.5%. In total, 80.7% of providers reached were active OBT prescribers. Of these, 52.7% accepted insurance for OBT, 20.8% accepted insurance for non-OBT services but not for OBT, and 26.5% did not accept insurance for any services. Practices who did not accept insurance were more likely among dedicated addiction clinics located outside of Ohio’s 6 major cities. Practices who normally accepted insurance but did not for OBT services were more likely in urban locations and were not associated with dedicated addiction practices. Neither business practice was associated with physician specialty
CONCLUSIONS AND RELEVANCE
Access to OBT in Ohio is far lower than what the 466 listed physicians suggests. Nearly 1 in 5 of those physicians are not active OBT prescribers, and 1 in 2 active prescribers do not accept insurance for OBT. Further research is needed to determine whether practices who do not accept insurance provide care consistent with CSAT guidelines and whether such practice patterns contribute to buprenorphine diversion.
Keywords: Buprenorphine, insurance coverage, payment and office-based treatment, buprenorphine access
Introduction
Buprenorphine, a long-acting mu-opiate receptor partial agonist, was approved in 2002 by the Food and Drug Administration (FDA) for treatment of opiate addiction. Under the US Drug Addiction Treatment Act (DATA 2000), physicians may prescribe buprenorphine in regular office practices, provided they undergo approved training and receive an FDA waiver and separate Drug Enforcement Administration (DEA) number. Since the introduction of office-based therapy (OBT), the number of eligible prescribers has increased from 9000 in 2006 to more than 20 000 in 2012, and the total sales of buprenorphine/naloxone have increased 10-fold to peak at $1.4 billion (28th best-selling prescription drug in the United States).1–3
Nationally, there is increasing concern that buprenorphine misuse and abuse are on the rise.1–4 Even the lay press is reporting on buprenorphine abuse.5,6 Concern is increasing over a pattern of excessive doses of buprenorphine being prescribed, either by design or because of exaggeration of withdrawal symptoms by the patients, enabling this abuse phenomenon. There is the obvious risk that physicians can charge high fees for office visits, whereas the patients can divert the excess medication.2,7,8 There is greater concern that practices who do not accept insurance for OBT and require direct payment from patients may be over-represented in this diversion phenomenon.5
Although both medical and nonmedical use of buprenorphine are growing, universal access to OBT is still far from realized.9 Policymakers and oversight agencies are challenged with the need to expand access to effective treatment while curtailing diversion.10 Requiring prior authorization for buprenorphine is one strategy, whereas another involves encouraging more appropriate dosing with targets of 8 to 16 mg daily.11–14 Many organizations are looking beyond these measures to develop strategies to deal with the dual challenge of increasing access while minimizing diversion.
This study is a cross-sectional telephone survey to characterize buprenorphine prescribers in the state of Ohio and the forms of payment that they accept. The study addresses issues of access by determining what proportion of publicly listed OBT-eligible physicians are currently engaged in OBT (⩾1 patient in treatment) and what forms of payment they accept. It also investigates the prevalence of factors that have been hypothesized to be associated with increased buprenorphine doses or diversion: cash-only practices, practices that accept insurance for non-OBT services but require cash for buprenorphine, and physicians with a history of previous medical board action.
Currently, there is concern in Ohio within the addiction treatment community, the law enforcement community, and licensing agencies about the dual problems of lack of buprenorphine access and the diversion and abuse of the drug. Access to quality buprenorphine/naloxone prescribing through health insurance is clearly limited and absolutely needs to be expanded. Simultaneously, there is great concern about abuse and diversion of buprenorphine/naloxone by patients and about the seemingly widespread practice of requiring cash payments for buprenorphine/naloxone services. This research project seeks to better describe the availability of insurance versus cash-only buprenorphine services in the State.
Methods
Data collection
A cross-sectional survey of all DATA-waivered physicians in Ohio listed on SAMHSA’s Center for Substance Abuse and Treatment (CSAT) Buprenorphine Physician and Treatment Program Locator was conducted.15 This list is not comprehensive because waivered physicians can opt out of the publicly available list; however, the complete DEA list was not available for this research project. National surveys with deidentified information from the DEA list show that 58% of all waivered prescribers opt out of the CSAT list.14 St. Vincent Charity Medical Center’s Institutional Review Board granted an expedited review of this survey project.
For each listed physician, researchers conducted a semis-tructured interview with any available office staff member regarding OBT services, including cost and availability. The interview assessed whether the office was accepting new patients, with or without insurance, what types of insurance were accepted, and what co-pays or cash requirements were needed for service. In addition, practices were questioned about whether they were an addiction dedicated provider, with addiction recovery services as the only services provided in that practice. If full information was not available during the initial interview, the practice was contacted a second time. All practices where a representative could not be reached on the first attempt were attempted to be contacted at least once more.
In addition to the survey, data were gathered on each physician from the State Medical Board’s Ohio License Center.16 The following fields were included: physician specialties (multiple could be listed, self-reported to the Medical Board), whether addiction medicine was listed as a specialty, and whether formal Board action exists.
Statistical analysis
Several outcome variables of interest were analyzed in separate multivariate logistic regression models. Each analysis determined those variables independently associated with the outcome variables of interest, after adjusting for the contributions of the other variables in the model. Statistical significance was taken as P < .05. Using the method of Bonferroni to correct for multiple testing of outcome data from a single respondent would remove nominal statistical significance from nominal P values in the multivariate analyses unless a nominal P value was less than .0125.
The outcome variables analyzed were as follows: whether the physician currently prescribes buprenorphine for OBT; whether the physician does not accept insurance for any services, including buprenorphine for OBT (ie, “cash only”); whether the physician accepts insurance for some services but does not accept insurance for OBT (ie, “buprenorphine exception”); and whether the physician has ever been the subject of formal action by the State Medical Board of Ohio. The following were considered as potential explanatory variables: psychiatrist versus primary care provider, addiction medicine subspecialty, dedicated addiction practice, pain management practice, and an office address in a city with a population greater than 100 000. χ2 tests were used to compare specialty characteristics and addiction medicine specialization between the population of all listed providers and providers reached.
Results
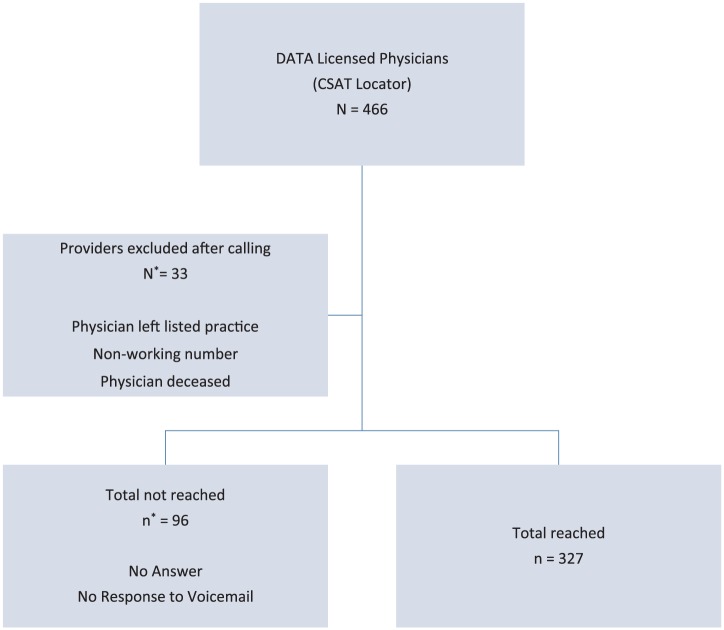
All 466 Ohio providers on the CSAT Buprenorphine Physician and Treatment Program Locator were called at least twice. Of these, 33 were excluded because of the following reasons: the listed number had been disconnected, the physician had left the listed practice without a forwarding address or contact information, the physician had left the state, or the physician was retired or deceased. Practices representing 327 providers were reached, with an overall response rate of 70.2% and a true response rate of 75.5% (Figure 1). They had a similar distribution of specialties compared with the CSAT list as a whole (Table 1). In all, 30.3% were psychiatrists, 53.5% primary care, and 4.9% anesthesiology; 32.4% listed an addiction specialization, compared with 30.0% of all providers on the CSAT list (P = .347); 11.9% had been the subject of Board action, compared with 13.7% of all listed providers (P = .344); and 40.7% listed an office address in a city with a population greater than 100 000, compared with 40.3% of all listed providers (P = .898).
Figure 1.
Buprenorphine prescriber response rates.
CSAT indicates Center for Substance Abuse Treatment; DATA, US Drug Addiction Treatment Act.
True response rate: 75.5% (n/n + n*, excluding N*).
Overall response rate: 70.2% (n/N).
Table 1.
Buprenorphine prescriber by specialty.
| ALL PROVIDERS (%) | PROVIDERS REACHED (%) | χ2 | P VALUE | |
|---|---|---|---|---|
| Total | 466 | 327 | ||
| Specialty | ||||
| Psychiatry | 138 (29.6) | 99 (30.3) | ||
| Primary carea | 244 (52.4) | 175 (53.5) | ||
| Anesthesiology | 32 (6.9) | 16 (4.9) | ||
| Otherb | 52 (11.2) | 37 (11.3) | ||
| 2.00 | .573 | |||
| Addiction medicine | 140 (30.0) | 106 (32.4) | 0.886 | .347 |
| Subject of medical board action | 64 (13.7) | 39 (11.9) | 0.897 | .344 |
| Office location in a major cityc | 188 (40.3) | 133 (40.7) | 0.016 | .898 |
Source: US Census Bureau: State and County QuickFacts (www.quickfacts.census.gov, accessed September 13, 2013).
Primary care specialties included the following: Family Practice, Internal Medicine, Medicine/Pediatrics, Pediatrics, Obstetrics/Gynecology, and General Practice.
Other specialties included the following: Addiction Medicine, Emergency Medicine, ENT, Neurology, Neurosurgery, Occupational Medicine, Ophthalmology, Orthopedic Surgery, Pain Medicine, Physical Medicine and Rehabilitation, and Radiology.
At least 1 office location identified in one of Ohio’s cities with population greater than 100 000 as of 2010 census: Akron, Cincinnati, Cleveland, Columbus, Dayton, Toledo.
Almost one-fifth (19.3%) of the providers contacted who were eligible to prescribe buprenorphine were not active in OBT (Table 2). On bivariate analysis, not being an active OBT prescriber was more likely for psychiatrists (P = .009) and was less likely for providers working in pain management practices (P = .011) or dedicated addiction practices (P < .001). Addiction specialization was not a significant predictor of not being active in OBT (P = .072). However, on multivariate analysis, the association with psychiatry disappeared (P = .466), whereas the association with not having addiction medicine specialization was stronger (P = .057). Neither primary care specialization nor practicing in an urban location was associated with not being active in OBT.
Table 2.
Insurance acceptance by Buprenorphine prescribers.
| COUNT | ||
|---|---|---|
| Active prescribers | 264 | 80.7% |
| Inactive prescribers | 63 | 19.3% (of total providers reached) |
| Accept insurance alwaysa | 139 | 52.7% |
| Accept no insuranceb | 70 | 26.5% |
| OBT exceptionc | 55 | 20.8% |
| Total | 327 |
Abbreviation: OBT, office-based therapy.
Accept insurance for all services, including OBT.
Do not participate in insurance at all (“cash only”).
Accept insurance for most services, but not for OBT.
Only 52.7% of the survey respondents who were active OBT providers accepted insurance for OBT services (Table 2). In all, 26.5% of providers reported having cash-only practices. Multivariate analysis showed a strong association between dedicated addiction practices and accepting cash only (P < .001). There was also a significant inverse association between urban practice location and accepting cash only (P = .012). Physician specialty, addiction specialty and pain management practices were not predictive of cash-only status.
A further 20.8% of providers accepted insurance for their non-OBT services but required direct patient payments for their buprenorphine treatment (OBT exception). There was a highly significant association with practicing in a major city (P < .001) and OBT exception. Physician specialty, addiction specialty, and dedicated addiction or pain management practice were not associated with OBT exception.
Of the providers reached, 11.9% had been the subject of medical board action, compared with 1.6% of all Ohio physicians.5 On bivariate analysis, psychiatrists were less likely (P = .040) and primary care physicians were more likely (P = .041) to have been the subject of board action. None of the examined explanatory factors were associated with medical board action in multivariate analysis. We did not specifically identify the reasons for these prior medical board actions.
Discussion
This is the first study to characterize OBT prescribers of an entire state 10 years after the introduction of buprenorphine maintenance therapy in the United States. The findings demonstrate that for a new patient seeking OBT in Ohio, access is far more limited than what the 466 publicly listed physicians suggest. Only 80% of these physicians currently provide OBT, and of those, only slightly more than half accept insurance payments for services. In 1 northeast Ohio region with a population base of over 250 000, 13 of 14 active prescribers do not accept any insurance payment for OBT.
It is surprising that 47.3% of active OBT physicians in Ohio do not accept insurance payment. Historically, cash payments for medical services occur when the services are poorly covered by health insurance. This is not the case for OBT in Ohio, where insurance carriers typically reimburse fully as they do for any other chronic disease. Neither business practice (cash only or OBT exception) was associated with physician specialty, which suggests that these findings are not artifacts of specialty-wide considerations (ie, psychiatrists’ low participation in managed care due to low insurance reimbursement rates for mental health services).17 Addressing the high percentage of cash-related OBT services should be a major issue for those advocating raising the patient OBT limit above 100 patients per provider.
Cash-only practices were more likely among dedicated addiction clinics located outside of Ohio’s 6 major cities. Our survey questionnaire did not ask why these clinics required cash for all clinical services and chose not to accept insurances of any type. The differences in geographic distribution might be related to the fact that urban areas tend to have more university-affiliated or teaching hospital–affiliated practices which uniformly accepted insurance in our survey, whereas nonurban practices are more likely to be the aforementioned chain-type addiction clinics. Regardless, the nonacceptance of insurance is a practice pattern of great ethical concern to the Department of Mental Health & Addiction Services, as well as to the State Medical and Pharmacy Boards. The impression of the agencies is that a series of these clinics have the same full self-pay business model, all charge substantially more than typically reimbursed by private or governmental insurance (respectively 3–5 times more by most anecdotal patient reports), and all contract with local DATA 2000–waivered physicians for use of their prescriptive privileges and very part-time work. Although arguably legal, there is the obvious appearance that needy and even desperate insured opioid-addicted patients are being financially taken advantage of by these clinics and their part-time contracted physicians. A limitation of our study was that we ascertained whether buprenorphine prescribers accepted insurance or not, but we did not identify what was charged by cash-only providers.
Office-based therapy exception practices, however, were more likely in urban locations and were not associated with dedicated addiction practices or teaching hospital–affiliated practices. They typically consisted of individual offices that provided multiple medical services, of which buprenorphine-based OBT was the only one where insurance coverage was not accepted. This 20% of physicians in our survey who reported accepting insurance reimbursement for other medical services yet still required cash payments from insured OBT patients are of greatest ethical and medicolegal concern. This practice is inconsistent with most, if not all, insurance contracts and has been found to be fraudulent in several cases in Ohio, resulting in catastrophic financial and licensure consequences to the physicians involved. Requiring cash for OBT services yet accepting insurance coverage for other clinical services may be construed as insurance fraud.
This study has several important limitations. Inability to reach the eligible physicians who opted out of CSAT’s public list limits the external validity of the survey. However, these nonlisted physicians are also invisible to potential patients and referring physicians. Although using the full list of all waivered physicians would provide a more complete picture of buprenorphine prescribing in Ohio, it would not necessarily be more typical of new patient access. Another limitation is that several different types of practice representatives were interviewed during the survey process. The majority of office responders were receptionists or office managers. This may have reduced the standardization of data collection, but it also allowed a high response rate compared with most surveys of physicians.9,14 Although data were collected related to the actual fees charged for office services, this information was not analyzed due to inconsistencies in how fees were structured and how the data were collected. For example, some physicians reported charging a flat fee for detoxification/induction and the first month of treatment, which may include weekly visits with the physician and in-house intensive outpatient counseling sessions, whereas others alter their appointment charges based on how long the patient has been on buprenorphine. For the purposes of this study, however, the range of dose prescribed was not a primary outcome, rather just the willingness to accept insurance for services provided.
There are multiple avenues for future research related to this study. Geospatial mapping of providers could give a more detailed view of geographic access barriers. More detailed information on the forms of insurance accepted (private vs Medicare Part B vs Medicaid) and the insurance status of their patients could have implications for access as well. Carefully profiling the cash payments and contrasting those with insurance reimbursement would be of great interest to supervisory agencies. Matching insurance accepting/cash-only/OBT exception physicians with deidentified prescription profiles from the Ohio Automated Rx Reporting System (the Ohio PMP) would provide trends regarding payment for services and average doses of buprenorphine prescribed.
This comprehensive cross-sectional survey of buprenorphine prescribers in Ohio demonstrates that 10 years after the introduction of OBT, despite the huge growth in buprenorphine use, access is far more limited than what the raw number of OBT-eligible physicians would predict. The phenomenon of requiring cash from insured patients in exchange for OBT services has great ethical, legal, and public policy implications for physicians, addiction organizations, and oversight agencies.
Acknowledgments
No external support was received for this study, including commercial support. Dr Parran had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
PEER REVIEW: Five peer reviewers contributed to the peer review report. Reviewers’ reports totaled 1284 words, excluding any confidential comments to the academic editor.
FUNDING: The author(s) received no financial support for the research, authorship, and/or publication of this article.
DECLARATION OF CONFLICTING INTEREST: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions
Study design by TVP, JZM, EC, CA and CMDR. Data collection by TVP, JZM and EC. Data analysis by TVP, JZM, DR and MK. Report preparation by TVP, CA, DR and MK. Report review by TVP, CA, CMDR, DR and MK.
REFERENCES
- 1.Johanson CE, Arfken CL, di Menza S, Schuster CR. Diversion and abuse of buprenorphine: findings from national surveys of treatment patients and physicians. Drug Alcohol Depend. 2012;120:190–195. doi: 10.1016/j.drugalcdep.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 2.Center for Substance Abuse Research Drug users, treatment providers, and law enforcement officers describe increasing Suboxone misuse in Ohio. CESAR Fax. 2012;21:49. [Google Scholar]
- 3.Ohio Department of Alcohol and Drug Addiction Services, Ohio Substance Abuse Monitoring Network OSAM-O-Gram: Surveillance of Drug Abuse Trends in the State of Ohio. June 2012–January 2013. [Accessed September 10, 2013]. www.mha.ohio.gov.
- 4.Wish ED, Artigiani E, Billing A, et al. The emerging buprenorphine epidemic in the United States. J Addict Dis. 2012;31:3–7. doi: 10.1080/10550887.2011.642757. [DOI] [PubMed] [Google Scholar]
- 5.Sontag D. Addiction treatment with a dark side. The New York Times. [Accessed November 23, 2013]. www.nytimes.com/2013/11/17/health/in-demand-in-clinics-and-on-the-street-bupe-can-be-savior-or-menace.html?hp&_r=0. Published November 16, 2013.
- 6.Sontag D. At clinics, tumultuous lives and turbulent care. The New York Times. [Accessed December 30, 2013]. www.nytimes.com/2013/11/18/health/at-clinics-tumultuous-lives-and-turbulent-care.html?hpw&rref=us&pagewanted=print. Published November 17, 2013.
- 7.Daniulaityte R, Falck R, Carlson RG. Illicit use of buprenorphine in a community sample of young adult non-medical users of pharmaceutical opioids. Drug Alcohol Depend. 2012;122:201–207. doi: 10.1016/j.drugalcdep.2011.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wisniewski AM, Dlugosz MR, Blondell RD. Reimbursement and practice policies among providers of buprenorphine-naloxone treatment. Subst Abus. 2013;34:105–107. doi: 10.1080/08897077.2012.677753. [DOI] [PubMed] [Google Scholar]
- 9.Tesema L, Bergeron G, Yeh J, et al. Auditing access to office-based therapy for opioid addiction in Massachusetts; American Public Health Association Annual Meeting; November 4, 2013; [Accessed January 2, 2013]. https://apha.confex.com/apha/141am/webprogramadapt/Paper290933.html. [Google Scholar]
- 10.Clarke RE, Baxter JD. Responses of state Medicaid programs to buprenorphine diversion: more harm than good? [published online ahead of print July 22, 2013] JAMA Internal Med. doi: 10.1001/jamainternmed.2013.9059. [DOI] [PubMed] [Google Scholar]
- 11.Ohio Department of Job and Family Services (ODJFS) Drug Utilization Board http://mha.ohio.gov/Portals/0/assets/Learning/Fact%20Sheets/Opiate%20Fact%20Sheet.pdf.
- 12.Center for Substance Abuse Treatment . Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Rockville, MD: Substance Abuse and Mental Health Services Administration; (Treatment Improvement Protocol (TIP) Series 40). DHHS Publication No. (SMA) 04–3939. Published 2004. https://store.samhsa.gov/shin/content/SMA05-4003/SMA05-4003.pdf. [PubMed] [Google Scholar]
- 13.Reckitt Benckiser Pharmaceuticals Inc Suboxone Product Label. [Accessed September 10, 2013]. http://www.suboxone.com/pdfs/SuboxonePI.pdf.
- 14.Arfken CL, Johanson CE, di Menza S, Schuster CR. Expanding treatment capacity for opioid dependence with office-based treatment with buprenorphine: national surveys of physicians. J Subst Abuse Treat. 2010;39:96–104. doi: 10.1016/j.jsat.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Substance Abuse and Mental Health Services Administration Buprenorphine Physician and Treatment Program Locator. https://www.samhsa.gov/medication-assisted-treatment/physician-program-data/treatment-physician-locator.
- 16.State Medical Board of Ohio, Ohio License Center [Accessed June-August 2013]. https://license.ohio.gov/lookup/default.asp.
- 17.Bookus RE, Cassil A, O’Malley AS. A snapshot of U.S. physicians: key findings from the 2008 Health Tracking Physician Survey. Data Bull (Cent Stud Health Syst Change) 2009. [Accessed June 10, 2013]. p. 35. http://www.hschange.com/CONTENT/1078/ [PubMed]