Abstract
Emergency laparotomy is a common high-risk surgical procedure, but with a few outcome data and few data on postoperative care. This was a hospital-based descriptive study of 376 consecutive emergency midline laparotomies performed in a tertiary care center. The aim of the study was to identify the clinical presentation, surgical indications, preoperative delay, intraoperative findings, and postoperative complications. Majority of the patients belonged to the 40–80-year age group. Broadly, the indications could be divided into acute abdomen and trauma. Most of the cases (82 %) presented with acute abdomen, out of which 57 % cases had gastrointestinal perforation, and 33 % had intestinal obstruction. In trauma laparotomies, 63 % of cases were done for blunt abdominal trauma and the rest for penetrating injury. The clinical features were analyzed, of which most frequent were abdominal tenderness (88.8 %), abdominal distension (88 %), tachycardia (74.2 %), and guarding (70.7 %). Nearly three fourths of the patients underwent laparotomy within 24 h of entry to the casualty. The most common condition that resulted in an emergency laparotomy was duodenal perforation which was seen in 93 patients, followed by gastric perforation in 60 patients. Postoperatively, 54.5 % of patients did not develop any complication. The most common complication encountered was wound infection (26.6 %). Mortality following emergency laparotomy was 13 %. Age-specific mortality was maximum in patients with age more than 80 years. The diagnosis-specific mortality was higher for large bowel perforation and mesenteric ischemia among the acute abdomen cases, and liver injury or great vessel injury among the trauma cases.
Keywords: Laparotomy, Acute abdomen, Intestinal obstruction, Intestinal perforation
Introduction
Laparotomies are one of the most commonly performed surgeries on an emergency basis [1]. It may be done on a patient presenting with acute abdomen or trauma [2]. Most of the time, it is done as a life-saving procedure. The decision to proceed with laparotomy is very important and crucial. It is done only after doing the necessary investigations, to reach a provisional diagnosis, provided the patient is clinically stable.
This study focuses on the etiology of emergency laparotomies happening in a tertiary care center. The common findings encountered during emergency laparotomy include perforation of hollow viscous, intestinal obstruction due to various causes, visceral organ injury, etc. [2, 3]. These conditions are of significance because any delay in surgical intervention may lead on to death of the patient. The site of origin of symptoms, etiology, duration from time of onset of symptoms to the time of laparotomy, general condition of the patient, comorbidities, anesthesia complications, and postoperative care, all play a role in the morbidity and mortality of the patients following emergency laparotomy [2]. We also studied the incidence of postoperative complications and the mortality following emergency laparotomy.
Materials and Methods
This was a hospital-based descriptive study. All patients who underwent emergency midline laparotomy for acute abdomen or trauma at Medical College Hospital were included in the study, and elective laparotomies were excluded. Study period was from 1 September 2013 to 31 August 2014, and the data were collected from hospital records.
Results
The study was done on 376 consecutive cases of emergency midline laparotomy. Of them, 310 were done for acute abdomen and 65 cases were done for trauma. On analysis, the majority of the cases were in the 40–60-year age group (30.6 %), closely followed by 60–80-year age group (29.8 %), 20–40-year age group (22.6 %), more than 80 years (9.6 %), and below 20 years (7.4 %). Out of the 376 cases, 284 patients were male and 92 patients were female.
In trauma laparotomies, 63 % of cases were done for blunt abdominal trauma and the rest for penetrating injury. Associated injuries other than abdominal injury were present in 46 (70.8 %) cases.
History of previous laparotomy was present in 71 (18.9 %) cases. Comorbidities present in 199 (52.9 %) cases. Any previous illness for which the patient was on medications or on frequent medical follow-up was considered comorbidity in this study. History of addiction was present in 155 (41.2 %) cases (alcoholism daily, smoking more than five cigarettes/day, and intravenous drug abuse were taken as addictions present).
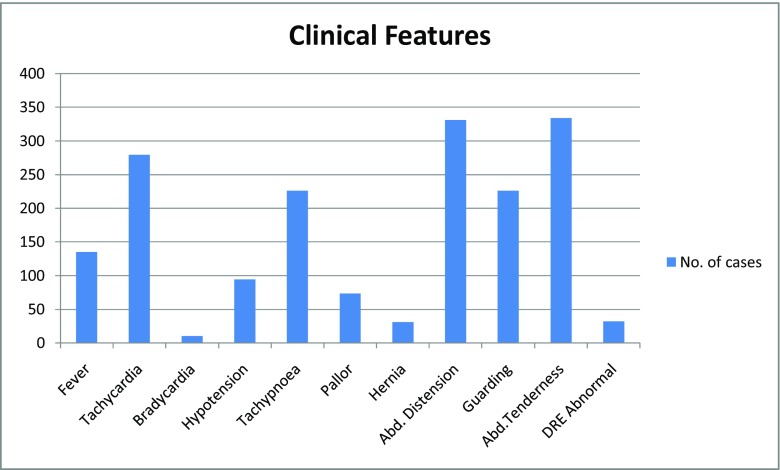
Clinical features of the patients taken for emergency laparotomy are summarized in Fig. 1.
Fig. 1.
Clinical features of the patients taken up for emergency laparotomy
Investigations
Hemoglobin < 10 mg% in 106 cases (28.2 %); total count > 11,000/cumm in 238 cases (63.3 %); and renal function deranged in182 cases (48.4 %).
Plain abdominal radiograph was taken in all the cases, of which 159 (42.3 %) showed free gas under the diaphragm. Multiple air fluid levels were seen in 98 (26 %) patients and dilated bowel loops in 56 (14.9 %) patients, whereas no specific findings were seen in 63 (16.7 %) patients. Ultrasonography (USG) of the abdomen was done in 56 % of the cases, with 27 % of them showing features of intestinal obstruction and 16 % with evidence of free fluid. USG of the abdomen prior to the procedure was not required in 44 % of the patients. Various USG abdomen findings are given in Fig. 2. Contrast-enhanced computed tomography (CECT) abdominal findings are summarized in Table 1. Computed tomography prior to laparotomy was not required for evaluation in 299 (79.5 %) cases. Intestinal perforation which did not show an evidence of free intraperitoneal air in the plain radiograph was picked up by CT in 23 (6.1 %) cases.
Fig. 2.
Percentage distribution of USG abdomen findings
Table 1.
Contrast-enhanced CT abdomen findings
| Frequency | Percent | |
|---|---|---|
| Not done | 299 | 79.5 |
| Features of perforation | 23 | 6.1 |
| Features of intestinal obstruction | 21 | 5.6 |
| Free fluid | 8 | 2.1 |
| Splenic injury | 8 | 2.1 |
| Others (abscess, collections, vascular pathology) | 15 | 4.0 |
| No abnormality detected | 2 | 0.5 |
| Total | 376 | 100.0 |
As soon as the diagnosis that mandated a laparotomy was reached, patient was shifted to the operating room for laparotomy. Laparotomy was done in 33 % of cases within 8–24 h of entry to the casualty, 30 % within 4–8 h, and only 1 % within 1 h.
The patients were broadly classified into having 28 different diagnoses postoperatively, the most common among them being duodenal perforation, which was seen in 93 (24.7 %) patients, followed by gastric perforation in 60 (16 %) patients. Distribution of cases according to postoperative diagnosis is given in Table 2.
Table 2.
Frequency distribution based on postoperative diagnosis
| Frequency | Percent | |
|---|---|---|
| Gastric perforation | 60 | 16.0 |
| Duodenal perforation | 93 | 24.7 |
| Jejunal or ileal perforation | 8 | 2.1 |
| Appendicular perforation | 13 | 3.5 |
| Large bowel perforation | 4 | 1.1 |
| Large bowel obstruction | 41 | 10.9 |
| Small bowel obstruction | 37 | 9.8 |
| Intussusception | 8 | 2.1 |
| Obstructed hernia | 15 | 4.0 |
| Blunt liver trauma | 4 | 1.1 |
| Blunt splenic injury | 10 | 2.7 |
| Blunt bowel injury | 19 | 5.1 |
| Blunt bladder injury | 4 | 1.1 |
| Blunt mesenteric injury | 4 | 1.1 |
| Penetrating injury stomach | 10 | 2.7 |
| Penetrating injury small bowel | 10 | 2.7 |
| Penetrating injury large bowel | 3 | 0.8 |
| Great vessel injury | 2 | 0.5 |
| Appendicular abscess | 7 | 1.9 |
| Psoas abscess | 4 | 1.1 |
| Liver abscess | 2 | 0.5 |
| Splenic abscess | 2 | 0.5 |
| Retropritoneal abscess | 1 | 0.3 |
| Perinephric abscess | 1 | 0.3 |
| Mesenteric ischemia | 7 | 1.9 |
| Lower GI bleeda | 2 | 0.5 |
| Twisted ovarian cyst | 2 | 0.5 |
| Inoperable malignant lesion | 3 | 0.8 |
| Total | 376 | 100 |
aLower gastrointestinal bleed when the bleed occurring distal to the ligament of Treitz. Here, in both the cases, the bleed was localized preoperatively with angiography and angioembolization was tried but failed to stop the bleeding.
Postoperative intensive care unit (ICU) admission was required in 42 % cases. The purpose of ICU care varied. It was either for ventilation (27 %), postoperative monitoring (48 %), or postoperative hypotension that needed inotropic support (25 %). Postoperatively, 54.5 % of patients did not develop any complication. The most common complication encountered was wound infection (26.6 %). Frequency distribution of postoperative complications is given in Table 3. Relaparotomy was required in six patients. Postoperatively, 13 % of the patients died within the same hospital admission and 87 % of cases got discharged. The percentage of mortality was maximum in the 60–80-year age group. However, the age-specific mortality was highest in the above 80-year age group.
Table 3.
Frequency distribution of postoperative complications
| Frequency | Percent | |
|---|---|---|
| Wound infection | 100 | 26.6 |
| Wound dehiscence | 7 | 1.9 |
| Anastomotic leak | 4 | 1.1 |
| Intra abdominal abscess | 11 | 2.9 |
| Post operative bleeding | 6 | 1.6 |
| Enterocutaneous fistula | 5 | 1.3 |
| No complications | 205 | 54.5 |
| Others (DVT, pneumonia, ACS, etc.) | 38 | 10.1 |
| Total | 376 | 100.0 |
DVT deep vein thrombosis, ACS acute coronary syndrome
In patients with gastrointestinal perforation, plain abdominal radiographs were diagnostic most of the time. The finding of free intraperitoneal air was present in 81 % of patients with perforation peritonitis, so they were not in need of further diagnostic investigations to assess the need for laparotomy.
Discussions
Laparotomies are one of the commonly performed surgeries in an emergency operating room. The indications for this procedure can broadly be divided into those done for acute abdomen and those done for trauma. Recently, with the advent of modern diagnostics, laparotomies done in cases of trauma are on the descent. Surgeons find it safer to avoid a laparotomy in patients who are hemodynamically stable and in conditions that usually get resolved by itself as in splenic and hepatic injuries of lower grade. Sometimes emergency laparotomies are termed exploratory laparotomies as the exact diagnosis will not be certain before surgery, and only on opening the abdomen, pathology is identified. Most exploratory laparotomies are performed in an emergency situation where the value of exhaustive investigations has to be balanced against any deterioration which may occur in the patient’s general condition due to the inevitable delay [1]. Conversely, a short delay during which active resuscitation and preliminary investigations are performed is however beneficial, as surgery on severely shocked or septic patients carry a significantly high mortality [1].
The most significant development of modern surgery is its comparative safety [2]. Our main concern next to safety of operation is the removal of pathology with minimum trauma so as to make for the restoration of function and the final cure of the patient. The patient may be optimized as far as the situations allow for a better outcome following surgery. In abdominal trauma, hypovolemic shock is a major cause of death. Blood pressure and pulse rate are the easily and quickly measureable indicators of the circulatory state [3]. Focused abdominal sonography in trauma (FAST) as a routine diagnostic tool for detection of free fluid in the abdominal cavity helped a great extent in decision making [4].
According to Pfeifer et al., overall prevalence of early death due to hemorrhage has decreased from 25 to 15 % during the past 10 years [5]. This improvement is probably multifactorial and may be due to the widespread implementation of Advanced Trauma Life Support (ATLS) principles and the concept of damage control surgery [3]. The damage control principle was introduced by Rotondo et al. in 1993 and is based on a staged approach in treating trauma patients. The concept of damage control was described as a method to save patients with severe injuries accepting that definitive surgical management would not be achieved at the first operation. Severe injuries requiring operative interventions are almost always associated with the lethal triad of hypothermia, acidosis, and coagulopathy. Each of the three elements fuels the other two, creating a vicious cycle that leads to death if left unbroken [6]. It has got three phases. In the first phase, the aim is to control the bleeding and contamination by rapid surgical maneuvers like packing, vessel ligation, vessel shunting, and bowel resection without anastomosis. In the second phase, the patient is shifted to a critical care unit for resuscitation, correction of coagulopathy, and rewarming. During the third phase, patient is taken back to the operating room for definitive repair of the injuries by reconstituting the vascular and bowel continuity, completing the resection of injured organs, unpacking, and closing the abdomen. The abdomen is the most common site for damage control procedures. In almost all the patients managed by damage control procedures, the abdomen is left open at the end of the first operation [6].
Acute Abdomen
The acute abdomen is a term used to encompass a spectrum of surgical, medical, and gynecological conditions, ranging from trivial to life threatening, which require hospital admission, investigation, and treatment [7]. It is a very common clinical entity and has been estimated that it constitutes about 50 % of emergency general surgical admissions. The common acute abdominal conditions which need admission includes acute appendicitis, acute cholecystitis, peptic ulcer disease, gastrointestinal perforation, small and large bowel obstruction, gynecological disorders, acute pancreatitis, malignant diseases, etc. [8].
Gastrointestinal perforation causes considerable mortality and requires surgical intervention. The type and degree of peritoneal contamination depend on the site, size, and duration of perforation, also on the physiologic state, including the time from last meal, mechanical bowel preparation before perforation, coexistent diseases, and the presence or absence of an ileus or bowel obstruction with accompanying bacterial growth [9–11]. The anatomic site of perforation significantly affects the type and burden of enteric contamination. Microbiological colonization increases from proximal to distal, with stomach showing the lowest (less than 103 organisms per gram of luminal contents) due to the hostile local milieu from acidic, biliary, and pancreatic secretions [10, 11]. The microbiologic load progressively increases from approximately 104 per gram of jejunal luminal contents to 1012 organisms per gram of colonic luminal contents, which is the highest [10, 11]. The microorganism load is inversely proportional to the relative toxicity of the organ fluid composition. The stomach and duodenal secretions contain acidic contents or erosive biliary and pancreatic fluid, whereas distal small bowel and colon contain a relatively neutral environment [11]. Therefore, the patients with gastric or duodenal perforation present rapidly and have sudden clinical deterioration due to the chemical peritonitis while those with colonic perforation present late [8, 12, 13].
A thorough history and physical examination are critical [12, 14, 15]. Although it may fail to identify the specific anatomic source of pathology with gastrointestinal perforation, they can rapidly determine patient’s acuteness, differentiate surgical emergencies from benign disease processes, evaluate surgical risk, guide supplemental diagnostic testing and intervention, and tailor the therapeutic preoperative optimization to the individual patient.
Radiographic evaluation of acute abdomen characteristically begins with a three view acute abdominal series consisting of an upright chest and abdominal radiograph and a supine abdominal radiograph. The presence of free intraperitoneal air on a routine radiograph indicates bowel perforation. Studies have shown that even 1 ml of gas below the right hemi-diaphragm can be detected by good-quality erect chest radiograph. However, sensitivity of a plain film radiograph is only 50–70 % and the probable site of perforation is never elucidated [16]. Other modalities include ultrasound, which may be particularly useful in patient groups where radiation burden should be limited as in children and pregnant women. However, it should not be considered definitive in excluding pneumoperitoneum. Computed tomography (CT) is useful in detecting extraluminal gas. A study of multidetector CT (MDCT) showed 86 % accuracy in predicting the site of perforation [13, 17]. The treatment of gastrointestinal perforation includes fluid resuscitation, antibiotics, source control, organ system support, and nutrition [18, 19].
Intestinal obstruction is another common surgical emergency that is associated with a high mortality if the diagnosis is delayed or managed inappropriately. Large bowel obstruction constitutes about 80 % of all intestinal obstructions, adenocarcinoma colon being the most common cause [20]. Strangulated obstruction of the intestine is a surgical emergency.
Principles of management of intestinal obstruction are provision of analgesia, intestinal decompression, intravenous administration of fluids and electrolytes, and if appropriate, surgery [20]. Up to 75 % of patients with adhesive obstruction of small bowel will settle with conservative management, so it is attempted initially in all patients without overt signs of strangulation. However, it is unusual for obstruction of the small bowel to resolve spontaneously without surgery if it has not done so within 48 h of conservative management.
Surgery is indicated if there is
A primary underlying disease process that must be treated like hernia, obstructing carcinoma
Failure of adhesive obstruction to settle
Signs of peritoneal irritation [20]
Conclusion
Emergency laparotomies are most commonly performed in cases of acute abdomen, where perforation peritonitis is the most common indication for a laparotomy. In our study, duodenal perforation was the most common cause of perforation peritonitis. The diagnosis-specific mortality was higher for large bowel perforation and mesenteric ischemia among the acute abdomen cases and liver injury or great vessel injury among the trauma cases. Most of the laparotomies were done within 24 h of seeking medical attention in the institution. Sophisticated time-consuming investigations are not a necessity for making a decision to proceed with laparotomy.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Rintoual R. Farquharson’s textbook of operative surgery. London: Churchill Livingstone; 1986. [Google Scholar]
- 2.Deaver JB. When and when not to open the abdomen in acute surgical conditions. Ann Surg. 1929;89:340–353. doi: 10.1097/00000658-192903000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lund H, Kofoed SC, Hillingso JG, Falck-Larsen C, Svendsen LB. High mortality after emergency room laparotomy in haemodynamically unstable trauma patients. Dan Med Bull. 2011;58:A4275. [PubMed] [Google Scholar]
- 4.Farahmand N, Sirlin CB, Brown MA, Shragg GP, Fortlage D, Hoyt DB, Casola G. Hypotensive patients with blunt abdominal trauma: performance of screening US. Radiology. 2005;235:436–443. doi: 10.1148/radiol.2352040583. [DOI] [PubMed] [Google Scholar]
- 5.Pfeifer R, Tarkin IS, Rocos B, Pape HC. Patterns of mortality and causes of death in polytrauma patients—has anything changed? Injury. 2009;40:907–911. doi: 10.1016/j.injury.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 6.George C. Velmahos M, Hasan B. Alam (2011) Damage Control Operation. Curr Surg Ther Tenth Edition. 970–974.
- 7.Gordon PH, Nivatvongs S, Mulholland MW. Principles and practice of surgery for the colon, rectum, and anus. Shock. 1999;12:328. doi: 10.1097/00024382-199910000-00019. [DOI] [Google Scholar]
- 8.Nathens AB, Rotstein OD. Therapeutic options in peritonitis. Surg Clin North Am. 1994;74:677–692. [PubMed] [Google Scholar]
- 9.Putcha RV, Burdick JS. Management of iatrogenic perforation. Gastroenterol Clin N Am. 2003;32:1289–1309. doi: 10.1016/S0889-8553(03)00094-3. [DOI] [PubMed] [Google Scholar]
- 10.Guarner F, Malagelada J-R. Gut flora in health and disease. Lancet. 2003;361:512–519. doi: 10.1016/S0140-6736(03)12489-0. [DOI] [PubMed] [Google Scholar]
- 11.Guarner F. Enteric flora in health and disease. Digestion. 2006;73:5–12. doi: 10.1159/000089775. [DOI] [PubMed] [Google Scholar]
- 12.Martin RF, Rossi RL. The acute abdomen: an overview and algorithms. Surg Clin N Am. 1997;77:1227–1243. doi: 10.1016/S0039-6109(05)70615-0. [DOI] [PubMed] [Google Scholar]
- 13.Fultz PJ, Skucas J, Weiss SL. CT in upper gastrointestinal tract perforations secondary to peptic ulcer disease. Gastrointest Radiol. 1992;17:5–8. doi: 10.1007/BF01888496. [DOI] [PubMed] [Google Scholar]
- 14.Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74:1537–1544. [PubMed] [Google Scholar]
- 15.Gerhardt RT, Nelson BK, Keenan S, Kernan L, MacKersie A, Lane MS. Derivation of a clinical guideline for the assessment of nonspecific abdominal pain: the Guideline for Abdominal Pain in the ED Setting (GAPEDS) Phase 1 Study. Am J Emerg Med. 2005;23:709–717. doi: 10.1016/j.ajem.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 16.MacKersie AB, Lane MJ, Gerhardt RT, Claypool HA, Keenan S, Katz DS, Tucker JE. Nontraumatic acute abdominal pain: unenhanced helical CT compared with three-view acute abdominal series 1. Radiology. 2005;237:114–122. doi: 10.1148/radiol.2371040066. [DOI] [PubMed] [Google Scholar]
- 17.Urban BA, Fishman EK. Tailored helical CT evaluation of acute abdomen 1: (CME available in print version and on RSNA link) Radiographics. 2000;20:725–749. doi: 10.1148/radiographics.20.3.g00ma12725. [DOI] [PubMed] [Google Scholar]
- 18.Wittmann DH, Schein M, Condon RE. Management of secondary peritonitis. Ann Surg. 1996;224:10. doi: 10.1097/00000658-199607000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ordoñez CA, Puyana JC. Management of peritonitis in the critically ill patient. Surg Clin N Am. 2006;86:1323–1349. doi: 10.1016/j.suc.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Macutkiewicz C, Carlson GL. Acute abdomen: intestinal obstruction. Surgery (Oxford) 2005;23:208–212. doi: 10.1383/surg.23.6.208.66558. [DOI] [Google Scholar]