Abstract
This study aimed to evaluate the role of off-pump coronary artery bypass (CAB) surgery on the decrease of postoperative inflammatory responses in patients. We systematically searched databases of PubMed and Embase to select the related studies. Interleukin (IL) 6, 8, and 10 were used as outcomes and pooled analysis was performed using R 3.12 software. Standardized mean differences (SMDs) and their 95% confidence intervals (95% CIs) were considered as effect estimates. A total of 27 studies, including 1340 participants, were recruited in this meta-analysis. The pooled analyses showed that postoperative concentration of IL-10 at 12 hours was significantly lower in off-pump CAB group compared to on-pump CAB group (SMD = −1.3640, 95% CI = −2.0086-−0.7193). However, no significant differences were found in pre and postoperative concentrations of IL-6 and 8 between off-pump and on-pump CAB groups. These results suggest that there is no advantage of off-pump CAB surgery in the reduction of inflammation compared to on-pump CAB surgery.
KEY WORDS: Coronary artery bypass, interleukins, meta-analysis, IL-6, IL-8, IL-10, off-pump coronary artery bypass surgery, on-pump coronary artery bypass surgery
INTRODUCTION
Inflammation is a major complication after coronary artery bypass (CAB) surgery. On-pump CAB is the standard surgery for transmyocardial laser revascularization due to its merits of safety, good effect, and low mortality. However, on-pump CAB surgery can generate some unavoidable adverse reactions such as inflammation.
To reduce the inflammation induced by operation and to improve the clinical outcome, off-pump CAB surgery is proposed, where a surgeon sutures blood vessels while the heart is beating. The benefits of off-pump CAB surgery are reduced operative time, cost, and complications compared with on-pump CAB surgery [1]. A previous meta-analysis showed that off-pump CAB surgery can reduce the risk of postoperative stroke [2]. However, off-pump CAB surgery is more difficult to perform, and advanced operative skills are required. Although a number of benefits of off-pump CAB surgery have been reported, the effect of off-pump CAB surgery on the reduction of inflammation remains unclear. Some studies have shown that off-pump CAB surgery can significantly reduce the postoperative inflammation [3,4], while others reported contrasting results [5,6].
Interleukins (ILs) are a class of cytokines that are produced by leukocytes [7]. ILs have been shown to play important roles in a series of immunological and inflammatory responses [8,9]. For example, IL-6, 8, and 10 are common cytokines involved in inflammation. IL-6 is an anti-inflammatory cytokine which plays important roles in inducing acute phase reactions and controlling local or systemic acute inflammatory responses [10]. IL-8 is a major neutrophil chemotactic factor involved in the acute inflammation [11]. IL-10 is essential for regulating macrophage and neutrophil infiltration as well as cytokine production during the inflammatory response of cutaneous wound healing [12].
To evaluate the effect of off-pump CAB surgery on the reduction of postoperative inflammation, we systematically meta-analyzed the levels of IL-6, 8, and 10 in patients who underwent CAB surgery and compared the results between off-pump and on-pump CAB groups.
MATERIALS AND METHODS
Source of data
Up to April 2016, PubMed (http://www.ncbi.nlm.nih.gov/pubmed/) and Embase (http://www.embase.com) databases were searched systematically using the predesigned search strategy. The search terms included (“coronary artery bypass” OR “coronary artery bypass grafting” OR “CABG”) AND (“non-pump” OR “on-bypass”) AND (“off-pump” OR “off-bypass” OR “OPCAB”) AND (“interleukin” OR “IL”).
Inclusion criteria
The following inclusion criteria were applied: (1) Off-pump and on-pump CAB surgeries were reported and (2) ILs were detected as an outcome. Reviews, reports, comments, and letters were excluded from our study.
Data extraction
Two authors (FM and BL) independently extracted the following information from the included studies: the name of the first author, year of publication and study implementation, total number of the patients who had off-pump and on-pump CAB surgery, gender, age, body mass index (BMI), and length of stay in hospital and intensive care unit (ICU) for both, off-pump and on-pump CAB groups. The disagreements during data extraction were discussed with the third author and resolved by consensus.
Statistical analysis
Statistical analyses were performed using R software version 3.12 (http://cran.r-project.org/web/packages/Hmisc/index.html). Standardized mean differences (SMDs) and their 95% confidence interval (95% CI) were used as effect estimates. Heterogeneity was assessed using Q statistic and I2 test [13]. If significant heterogeneity was found (p < 0.1 or I2 > 50%), random effects model was used for pooled analysis. Otherwise, the fixed effects model was used. Sensitivity analysis was carried out by removing each study, step by step, to evaluate the stability of the pooled results. Egger’s test was used for detecting publication bias and p < 0.05 indicated a statistically significant publication bias.
RESULTS
Study selection
The study selection process is shown in Figure 1. A total of 180 studies were identified by the primary search. First, 47 repeated studies were excluded. Second, 79 irrelevant studies were removed from the remaining 133 records by reading titles and abstracts. Third, 27 studies were removed by reading the full-texts. Finally, 27 studies were included in this meta-analysis [3-6,14-36].
FIGURE 1.
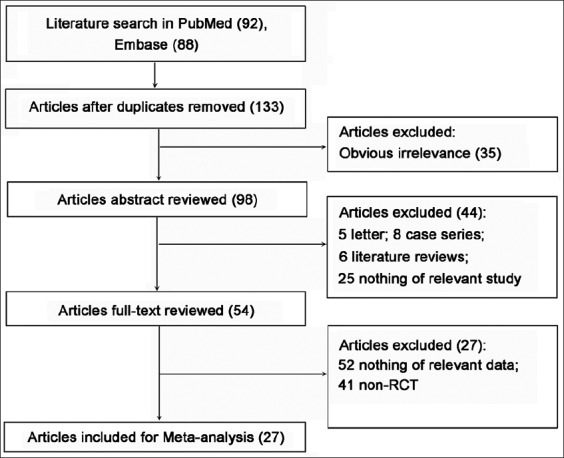
Literature search and study selection.
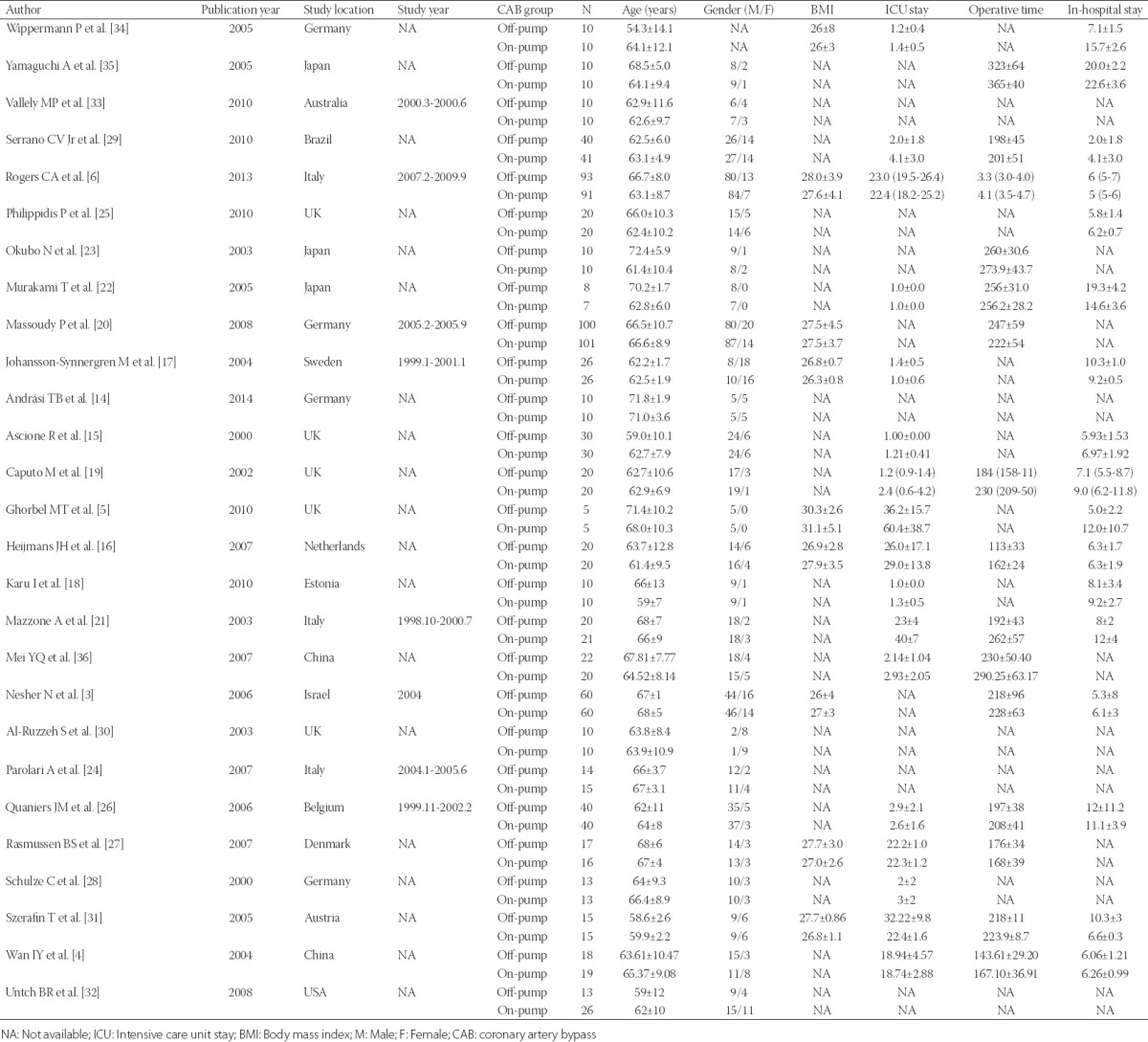
Characteristics of included studies
As shown in Table 1, the included studies were published from 2000 to 2014. The selected studies were conducted in different regions, including China, Brazil, Italy, Japan, Israel, and England. A total of 1340 participants were considered. Among these participants, there were 664 off-pump CAB and 676 on-pump CAB patients. The majority of the patients were elderly (>60 years), and no significant difference was found in the age between the two groups. The baseline information showed that most of the patients were male, with mean BMI >24. In most of the included studies operative time, ICU stay, and hospital stay were slightly longer in on-pump CAB group compared to off-pump CAB group.
TABLE 1.
The characteristics of the included studies
Pooled analysis
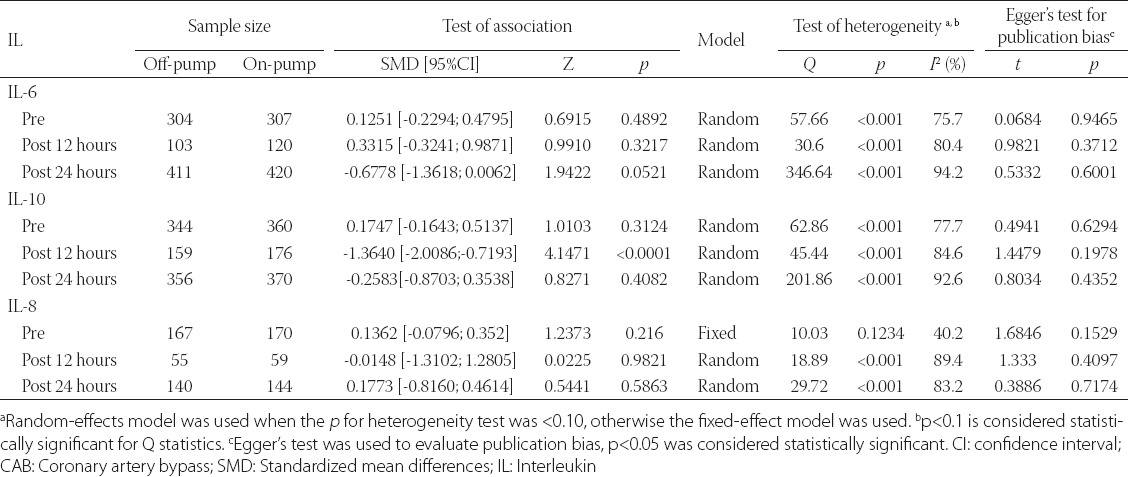
The pre and postoperative concentrations (at 12 and 24 hours) of IL-6, 8, and 10 were considered as outcomes. Due to inapparent heterogeneity (p = 0.1234, I2 = 40.2%), pooling analysis of preoperative IL-8 concentration was performed using fixed effects model. The remaining outcomes were pooled using random effects model. The pooled results were summarized in Table 2. The postoperative concentration of IL-10 at 12 hours in off-pump CAB group was significantly lower compared to on-pump CAB group (SMD = −1.3640, 95% CI = −2.0086-−0.7193). However, there were no obvious differences in the preoperative concentrations of IL-10 and those assessed 24 hours postoperatively, between off-pump and on-pump CAB groups. In addition, there were no significant differences in the pre and postoperative concentrations of IL-6 and 8 between the two groups. All of the pooled results showed no significant publication bias.
TABLE 2.
Overall pooled analyses of pre and postoperative IL-6, 8 and 10 between off- and on-pump CAB groups
Sensitivity analyses
The results of sensitivity analyses are shown in Figures 2, 3, and 4. After omitting the studies by Caputo et al. [19] and Vallely et al. [33], the outcomes were reversed for the IL-6 concentration (SMD = 0.56, 95% CI = 0.12-1.01 [Figure 2B]) and IL-8 concentration (SMD = 0.70, 95% CI = 0.27-1.13 [Figure 4B]) 12 hours after operation. Other results of sensitivity analysis were consistent with the overall pooled results.
FIGURE 2.
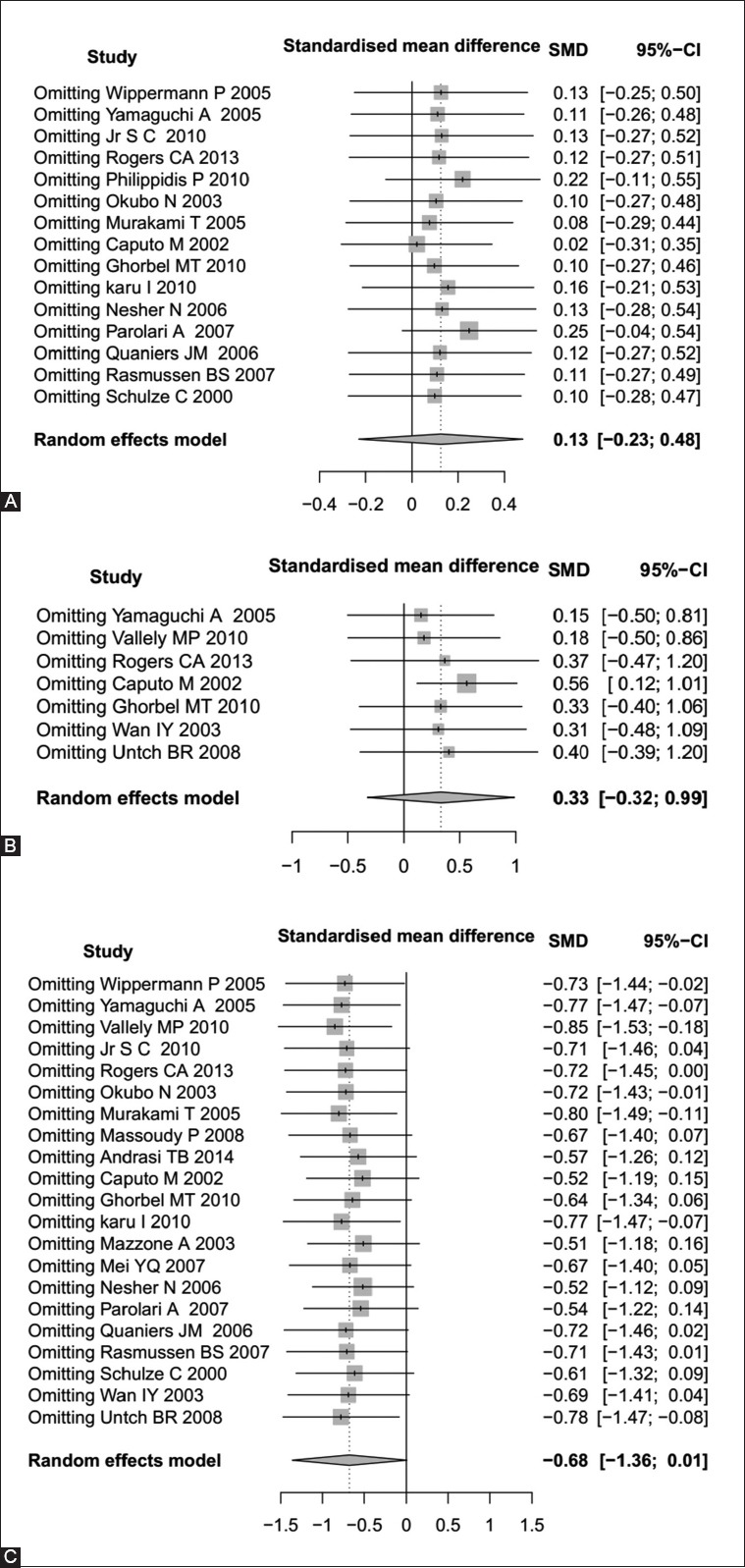
Sensitivity analyses of interleukin-6 (IL-6) in preoperative conditions (A), at 12 hours postoperatively (B), and at 24 hours postoperatively (C).
FIGURE 3.
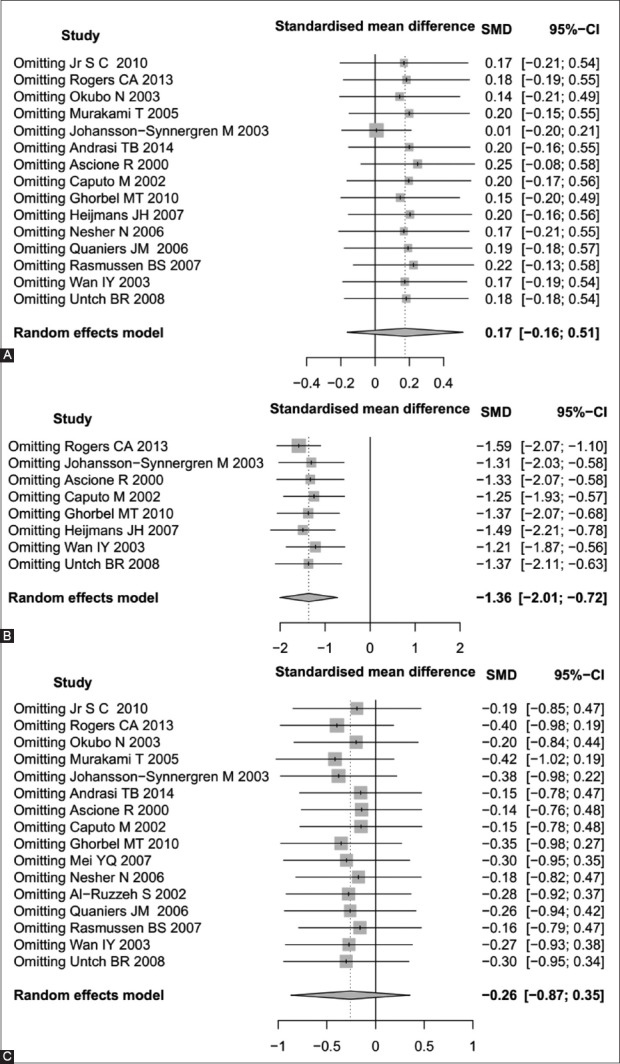
Sensitivity analyses of interleukin-10 (IL-10) in preoperative conditions (A), at 12 hours postoperatively (B), and at 24 hours postoperatively (C).
FIGURE 4.
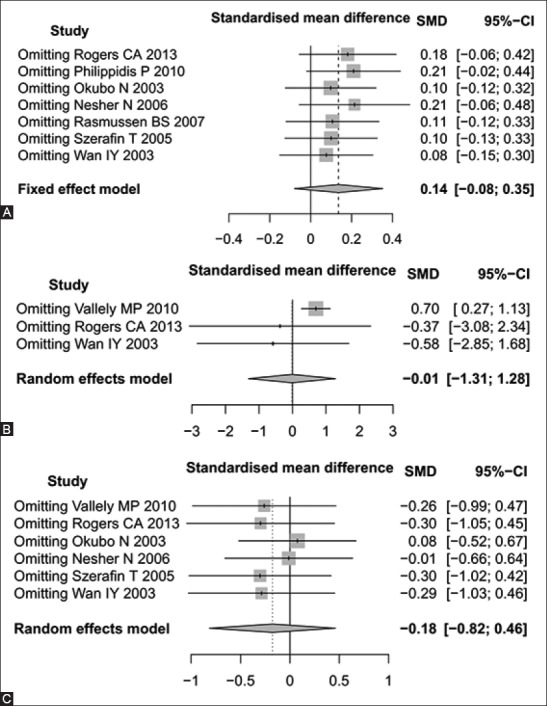
Sensitivity analyses of interleukin-8 (IL-8) in preoperative conditions (A), at 12 hours postoperatively (B), and at 24 hours potoperatively (C).
DISCUSSION
Off-pump CAB surgery is likely to have some advantages over on-pump CAB surgery, such as reduced operative time and cost [1]. However, whether off-pump CAB surgery can significantly reduce the postoperative inflammation, is controversial. In this study, we found that only concentration of IL-10, 12 hours after operation, was significantly lower in off-pump CAB group compared to on-pump CAB group. There were no significant differences in the concentrations of IL-6, 8, and other concentrations of IL-10 between off-pump and on-pump CAB groups, suggesting that off-pump CAB surgery has no advantage over on-pump CAB surgery, in reducing postoperative inflammatory responses in patients.
Nevertheless, in our analysis, IL-6, 8, and 10 levels were significantly decreased in off-pump CAB group at 24 hours postoperatively. However, the IL concentrations at 12 hours postoperatively showed inconsistent results, which might be related to a small number of included studies or divergent effects of different types of ILs on the inflammatory response during surgery. For example, in patients with coronary artery disease serum levels of IL-6 are significantly higher, but the concentration of IL-10 is significantly lower compared to healthy people [37]. Furthermore, the physical condition of a patient is also an important factor influencing the IL levels. Shi et al. [38] found that IL-6 could induce obesity-related inflammatory response. In addition, some pro-inflammatory markers, including IL-6, were positively related to the obesity-independent insulin resistance and metabolic syndrome features [39-41]. Therefore, more clinical characteristics of participants should be considered when carrying out experiment design in these studies.
In this study, significant heterogeneities were observed in all outcomes except preoperative IL-8 concentrations. The following reasons could be the source of this heterogeneity: (1) participants from different regions may differ with regard to culture, living environment, and customs; (2) potential factors that may increase inflammatory responses, such as comorbidity interference, were not excluded; (3) many of the included studies compared only postoperative IL levels between off-pump and on-pump CAB groups. Therefore, the diversity of baseline levels between the two groups could be the source of heterogeneity.
This is the first meta-analysis systematically comparing the preoperative and postoperative IL-6, 8 and 10 concentrations between off-pump and on-pump CAB groups. No publication biases were found in the outcomes. However, there are several limitations in this study. First, the subgroup analyses and meta-regression analysis could not be conducted due to the incomplete covariates provided in the included studies. Second, only the outcomes in pre and postoperative periods were pooled. The post-discharge outcomes were not analyzed due to lack of data. Thus, further studies with a strict experimental design are required to verify our observation.
In the present meta-analysis, the sensitivity analyses showed that most of the pooled results were stable after omitting one study. However, the studies by Caputo et al. [19] and Vallely et al. [33] showed a large effect on the pooled results. This may be due to the small sample sizes. Thus, more studies with larger sample size and strict experimental design should be performed to evaluate the inflammatory response between off-pump and on-pump CAB patients.
Overall, there are no significant differences in the concentrations of IL-6, 8 and 10 between off-pump and on-pump CAB groups, suggesting that the off-pump CAB surgery may have no beneficial effect on the reduction of inflammatory response in these patients. However, this result should be verified by other studies with high quality and large samples.
DECLARATION OF INTERESTS
The authors declare no conflict of interests.
REFERENCES
- 1.Brinkman WT, Squiers JJ, Covington KR, Wheeler DA, Arsalan M, Smith RL, et al. Mini-extracorporeal circulation and off-pump techniques associated with less inflammatory gene expression as compared to on-pump in the 24-hour postoperative window following coronary artery bypass grafting. J Cardiothorac Surg. 2015;10(Suppl 1):A101. https:/doi.org/10.1186/1749-8090-10-S1-A101. [Google Scholar]
- 2.Afilalo J, Rasti M, Ohayon SM, Shimony A, Eisenberg MJ. Off-pump vs. On-pump coronary artery bypass surgery: An updated meta-analysis and meta-regression of randomized trials. Eur Heart J. 2012;33(10):1257–67. doi: 10.1093/eurheartj/ehr307. https:/doi.org/10.1093/eurheartj/ehr307. [DOI] [PubMed] [Google Scholar]
- 3.Nesher N, Frolkis I, Vardi M, Sheinberg N, Bakir I, Caselman F, et al. Higher levels of serum cytokines and myocardial tissue markers during on-pump versus off-pump coronary artery bypass surgery. J Card Surg. 2006;21(4):395–402. doi: 10.1111/j.1540-8191.2006.00272.x. https:/doi.org/10.1111/j.1540-8191.2006.00272.x. [DOI] [PubMed] [Google Scholar]
- 4.Wan IY, Arifi AA, Wan S, Yip JH, Sihoe AD, Thung KH, et al. Beating heart revascularization with or without cardiopulmonary bypass: Evaluation of inflammatory response in a prospective randomized study. J Thorac Cardiovasc Surg. 2004;127(6):1624–31. doi: 10.1016/j.jtcvs.2003.10.043. https:/doi.org/10.1016/j.jtcvs.2003.10.043. [DOI] [PubMed] [Google Scholar]
- 5.Ghorbel MT, Cherif M, Mokhtari A, Bruno VD, Caputo M, Angelini GD. Off-pump coronary artery bypass surgery is associated with fewer gene expression changes in the human myocardium in comparison with on-pump surgery. Physiol Genomics. 2010;42(1):67–75. doi: 10.1152/physiolgenomics.00174.2009. https:/doi.org/10.1152/physiolgenomics.00174.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rogers CA, Pike K, Angelini GD, Reeves BC, Glauber M, Ferrarini M, et al. An open randomized controlled trial of median sternotomy versus anterolateral left thoracotomy on morbidity and health care resource use in patients having off-pump coronary artery bypass surgery: The Sternotomy Versus Thoracotomy (STET) trial. J Thorac Cardiovasc Surg. 2013;146(2):306–16.e9. doi: 10.1016/j.jtcvs.2012.04.020. DOI: 10.1016/j.jtcvs.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 7.Brocker C, Thompson D, Matsumoto A, Nebert DW, Vasiliou V. Evolutionary divergence and functions of the human interleukin (IL) gene family. Hum Genomics. 2010;5(1):30–55. doi: 10.1186/1479-7364-5-1-30. https:/doi.org/10.1186/1479-7364-5-1-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cua DJ, Sherlock J, Chen Y, Murphy CA, Joyce B, Seymour B, et al. Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature. 2003;421(6924):744–8. doi: 10.1038/nature01355. https:/doi.org/10.1038/nature01355. [DOI] [PubMed] [Google Scholar]
- 9.Kuilman T, Michaloglou C, Vredeveld LC, Douma S, van Doorn R, Desmet CJ, et al. Oncogene-induced senescence relayed by an interleukin-dependent inflammatory network. Cell. 2008;133(6):1019–31. doi: 10.1016/j.cell.2008.03.039. https:/doi.org/10.1016/j.cell.2008.03.039. [DOI] [PubMed] [Google Scholar]
- 10.Xing Z, Gauldie J, Cox G, Baumann H, Jordana M, Lei XF, et al. IL-6 is an antiinflammatory cytokine required for controlling local or systemic acute inflammatory responses. J Clin Invest. 1998;101(2):311–20. doi: 10.1172/JCI1368. https:/doi.org/10.1172/JCI1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harada A, Sekido N, Akahoshi T, Wada T, Mukaida N, Matsushima K. Essential involvement of interleukin-8 (IL-8) in acute inflammation. J Leukoc Biol. 1994;56(5):559–64. [PubMed] [Google Scholar]
- 12.Sato Y, Ohshima T, Kondo T. Regulatory role of endogenous interleukin-10 in cutaneous inflammatory response of murine wound healing. Biochem Biophys Res Commun. 1999;265(1):194–9. doi: 10.1006/bbrc.1999.1455. https:/doi.org/10.1006/bbrc.1999.1455. [DOI] [PubMed] [Google Scholar]
- 13.Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127(9):820–6. doi: 10.7326/0003-4819-127-9-199711010-00008. https:/doi.org/10.7326/0003-4819-127-9-199711010-00008. [DOI] [PubMed] [Google Scholar]
- 14.Andrási TB, Mertens F, Barabás B, Blázovics A. Effect of haemodynamic changes on epithelium-related intestinal injury in off-pump coronary surgery. Heart Lung Circ. 2014;23(2):144–51. doi: 10.1016/j.hlc.2013.07.016. https:/doi.org/10.1016/j.hlc.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 15.Ascione R, Lloyd CT, Underwood MJ, Lotto AA, Pitsis AA, Angelini GD. Inflammatory response after coronary revascularization with or without cardiopulmonary bypass. Ann Thorac Surg. 2000;69(4):1198–204. doi: 10.1016/s0003-4975(00)01152-8. https:/doi.org/10.1016/S0003-4975(00)01152-8. [DOI] [PubMed] [Google Scholar]
- 16.Heijmans JH, Liem KS, Damoiseaux GM, Maessen JG, Roekaerts PM. Pulmonary function and inflammatory markers in patients undergoing coronary revascularisation with or without cardiopulmonary bypass. Anaesthesia. 2007;62(12):1233–40. doi: 10.1111/j.1365-2044.2007.05254.x. https:/doi.org/10.1111/j.1365-2044.2007.05254.x. [DOI] [PubMed] [Google Scholar]
- 17.Johansson-Synnergren M, Nilsson F, Bengtsson A, Jeppsson A, Wiklund L. Off-pump CABG reduces complement activation but does not significantly affect peripheral endothelial function: A prospective randomized study. Scand Cardiovasc J. 2004;38(38):53–8. doi: 10.1080/14017430410024847. https:/doi.org/10.1080/14017430410024847. [DOI] [PubMed] [Google Scholar]
- 18.Karu I, Taal G, Zilmer K, Pruunsild C, Starkopf J, Zilmer M. Inflammatory/oxidative stress during the first week after different types of cardiac surgery. Scand Cardiovasc J. 2010;44(2):119–24. doi: 10.3109/14017430903490981. https:/doi.org/10.3109/14017430903490981. [DOI] [PubMed] [Google Scholar]
- 19.Caputo M, Yeatman M, Narayan P, Marchetto G, Ascione R, Reeves BC, et al. Effect of off-pump coronary surgery with right ventricular assist device on organ function and inflammatory response: A randomized controlled trial. Ann Thorac Surg. 2002;74(6):2088–95. doi: 10.1016/s0003-4975(02)04025-0. https:/doi.org/10.1016/S0003-4975(02)04025-0. [DOI] [PubMed] [Google Scholar]
- 20.Massoudy P, Wagner S, Thielmann M, Herold U, Kottenberg-Assenmacher E, Marggraf G, et al. Coronary artery bypass surgery and acute kidney injury –Impact of the off-pump technique. Nephrol Dial Transplant. 2008;23(9):2853–60. doi: 10.1093/ndt/gfn153. https:/doi.org/10.1093/ndt/gfn153. [DOI] [PubMed] [Google Scholar]
- 21.Mazzone A, Gianetti J, Picano E, Bevilacqua S, Zucchelli G, Biagini A, et al. Correlation between inflammatory response and markers of neuronal damage in coronary revascularization with and without cardiopulmonary bypass. Perfusion. 2003;18(1):3–8. doi: 10.1191/0267659103pf622oa. DOI: 10.1191/0267659103pf622oa. [DOI] [PubMed] [Google Scholar]
- 22.Murakami T, Iwagaki H, Saito S, Ohtani S, Kuroki K, Kuinose M, et al. Equivalence of the acute cytokine surge and myocardial injury after coronary artery bypass grafting with and without a novel extracorporeal circulation system. J Int Med Res. 2005;33(2):133–49. doi: 10.1177/147323000503300201. https:/doi.org/10.1177/147323000503300201. [DOI] [PubMed] [Google Scholar]
- 23.Okubo N, Hatori N, Ochi M, Tanaka S. Comparison of m-RNA expression for inflammatory mediators in leukocytes between on-pump and off-pump coronary artery bypass grafting. Ann Thorac Cardiovasc Surg. 2003;9(1):43–9. [PubMed] [Google Scholar]
- 24.Parolari A, Camera M, Alamanni F, Naliato M, Polvani GL, Agrifoglio M, et al. Systemic inflammation after on-pump and off-pump coronary bypass surgery: A one-month follow-up. Ann Thorac Surg. 2007;84(3):823–8. doi: 10.1016/j.athoracsur.2007.04.048. https:/doi.org/10.1016/j.athoracsur.2007.04.048. [DOI] [PubMed] [Google Scholar]
- 25.Philippidis P, Athanasiou T, Nadra I, Ashrafian H, Haskard DO, Landis RC, et al. Anti-inflammatory haemoglobin scavenging monocytes are induced following coronary artery bypass surgery. Eur J Cardiothorac Surg. 2010;37(6):1360–6. doi: 10.1016/j.ejcts.2009.12.043. https:/doi.org/10.1016/j.ejcts.2009.12.043. [DOI] [PubMed] [Google Scholar]
- 26.Quaniers JM, Leruth J, Albert A, Limet RR, Defraigne JO. Comparison of inflammatory responses after off-pump and on-pump coronary surgery using surface modifying additives circuit. Ann Thorac Surg. 2006;81(5):1683–90. doi: 10.1016/j.athoracsur.2005.11.059. https:/doi.org/10.1016/j.athoracsur.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 27.Rasmussen BS, Laugesen H, Sollid J, Grønlund J, Rees SE, Toft E, et al. Oxygenation and release of inflammatory mediators after off-pump compared with after on-pump coronary artery bypass surgery. Acta Anaesthesiol Scand. 2007;51(9):1202–10. doi: 10.1111/j.1399-6576.2007.01426.x. https:/doi.org/10.1111/j.1399-6576.2007.01426.x. [DOI] [PubMed] [Google Scholar]
- 28.Schulze C, Conrad N, Schütz A, Egi K, Reichenspurner H, Reichart B, et al. Reduced expression of systemic proinflammatory cytokines after off-pump versus conventional coronary artery bypass grafting. Thorac Cardiovasc Surg. 2000;48(6):364–9. doi: 10.1055/s-2000-8352. https:/doi.org/10.1055/s-2000-8352. [DOI] [PubMed] [Google Scholar]
- 29.Serrano CV, Jr, Souza JA, Lopes NH, Fernandes JL, Nicolau JC, Blotta MH, et al. Reduced expression of systemic proinflammatory and myocardial biomarkers after off-pump versus on-pump coronary artery bypass surgery: A prospective randomized study. J Crit Care. 2010;25(2):305–12. doi: 10.1016/j.jcrc.2009.06.009. https:/doi.org/10.1016/j.jcrc.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 30.Al-Ruzzeh S, Hoare G, Marczin N, Asimakopoulos G, George S, Taylor K, et al. Off-pump coronary artery bypass surgery is associated with reduced neutrophil activation as measured by the expression of CD11b: A prospective randomized study. Heart Surg Forum. 2003;6(2):89–93. doi: 10.1532/hsf.1205. https:/doi.org/10.1532/hsf.1205. [DOI] [PubMed] [Google Scholar]
- 31.Szerafin T, Brunner M, Horváth A, Szentgyörgyi L, Moser B, Boltz-Nitulescu G, et al. Soluble ST2 protein in cardiac surgery: A possible negative feedback loop to prevent uncontrolled inflammatory reactions. Clin Lab. 2005;51(11-12):657–63. [PubMed] [Google Scholar]
- 32.Untch BR, Jeske WP, Schwartz J, Botkin S, Prechel M, Walenga JM, et al. Inflammatory and hemostatic activation in patients undergoing off-pump coronary artery bypass grafting. Clin Appl Thromb Hemost. 2008;14(2):141–8. doi: 10.1177/1076029607308869. https:/doi.org/10.1177/1076029607308869. [DOI] [PubMed] [Google Scholar]
- 33.Vallely MP, Bannon PG, Bayfield MS, Hughes CF, Kritharides L. Endothelial activation after coronary artery bypass surgery: comparison between on-pump and off-pump techniques. Heart Lung Circ. 2010;19(8):445–52. doi: 10.1016/j.hlc.2010.03.006. https:/doi.org/10.1016/j.hlc.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 34.Wippermann J, Albes JM, Hartrumpf M, Kaluza M, Vollandt R, Bruhin R, et al. Comparison of minimally invasive closed circuit extracorporeal circulation with conventional cardiopulmonary bypass and with off-pump technique in CABG patients: selected parameters of coagulation and inflammatory system. Eur J Cardiothorac Surg. 2005;28(1):127–32. doi: 10.1016/j.ejcts.2005.03.032. https:/doi.org/10.1016/j.ejcts.2005.03.032. [DOI] [PubMed] [Google Scholar]
- 35.Yamaguchi A, Endo H, Kawahito K, Adachi H, Ino T. Off-pump coronary artery bypass grafting attenuates proinflammatory markers. Jpn J Thorac Cardiovasc Surg. 2005;53(3):127–32. doi: 10.1007/s11748-005-0017-7. https:/doi.org/10.1007/s11748-005-0017-7. [DOI] [PubMed] [Google Scholar]
- 36.Mei YQ, Ji Q, Liu H, Wang X, Feng J, Long C, et al. Study on the relationship of APACHE III and levels of cytokines in patients with systemic inflammatory response syndrome after coronary artery bypass grafting. Biol Pharm Bull. 2007;30(3):410–4. doi: 10.1248/bpb.30.410. https:/doi.org/10.1248/bpb.30.410. [DOI] [PubMed] [Google Scholar]
- 37.Karu I, Starkopf J, Zilmer K, Zilmer M. Growth factors serum levels in coronary artery disease patients scheduled for bypass surgery: Perioperative dynamics and comparisons with healthy volunteers. Biomed Res Int. 2013;2013:985404. doi: 10.1155/2013/985404. https:/doi.org/10.1155/2013/985404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shi C, Zhu L, Chen X, Gu N, Chen L, Zhu L, et al. IL-6 and TNF-a induced obesity-related inflammatory response through transcriptional regulation of miR-146b. J Interferon Cytokine Res. 2014;34(5):342–8. doi: 10.1089/jir.2013.0078. https:/doi.org/10.1089/jir.2013.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pickup JC, Mattock MB, Chusney GD, Burt D. NIDDM as a disease of the innate immune system: Association of acute-phase reactants and interleukin-6 with metabolic syndrome X. Diabetologia. 1997;40(11):1286–92. doi: 10.1007/s001250050822. https:/doi.org/10.1007/s001250050822. [DOI] [PubMed] [Google Scholar]
- 40.Phillips CM, Perry IJ. Does inflammation determine metabolic health status in obese and nonobese adults? J Clin Endocrinol Metab. 2013;98(10):E1610–9. doi: 10.1210/jc.2013-2038. https:/doi.org/10.1210/jc.2013-2038. [DOI] [PubMed] [Google Scholar]
- 41.Vozarova B, Weyer C, Lindsay RS, Pratley RE, Bogardus C, Tataranni PA. High white blood cell count is associated with a worsening of insulin sensitivity and predicts the development of Type 2 diabetes. Diabetes. 2002;51(2):455–61. doi: 10.2337/diabetes.51.2.455. https:/doi.org/10.2337/diabetes.51.2.455. [DOI] [PubMed] [Google Scholar]


